Beruflich Dokumente
Kultur Dokumente
Aguirre5Local Anesthetics
Hochgeladen von
achmaddani1317Originalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Aguirre5Local Anesthetics
Hochgeladen von
achmaddani1317Copyright:
Verfügbare Formate
Local anesthetics
James E. Heavner
Introduction
Local anesthetics are widely used to prevent or treat
acute pain; to treat inflammatory, cancer related, and
chronic pain; and for diagnostic and prognostic
purposes. Drugs classified as local anesthetics reversibly
bloc action potential propagation in a!ons by preventing
the sodium entry that produces the potentials "#$. %ther
actions of these drugs, however, such as anti&inflammatory
actions by interaction with '&protein receptors "($, are
also thought to be relevant to their use to prevent or
treat pain. )oth nociceptive and neuropathic pain are
targeted by this group of drugs. *ny part of the
nervous system, from the periphery to the brain, may be
where local anesthetics act to produce a desired
anesthetic or analgesic effect. * variety of formulations
of local anesthetics, routes of administration, and
methods of administration are used. +he drugs are
formulated commercially or by medical personnel
according to intended route of administration or to
address specific concerns or needs. In this article I
provide a concise review of the pharmacology of local
anesthetics with an emphasis on current concepts.
,urr %pin *naesthesiol (-.//0 1 /2(. (--3 Lippincott 4illiams 5 4ilins.
Department of *nesthesiology and 6hysiology, +e!as +echnology 7niversity
Health 8ciences ,enter, Lubboc, +e!as, 78*
,orrespondence to JE Heavner, D9:, 6hD, *nesthesiology, /0-# 2th 8treet,
++7H8,, Lubboc, +; 3<2/-, 78*
+el. =# >-0 32/ (<#0; fa!. =# >-0 32/ #?##; e&mail. @ames . heavnerAttuhsc.edu
,urrent %pinion in *naesthesiology (--3, (-.//0 1 /2(
(--3 Lippincott 4illiams 5 4ilins
-<?(&3<-3
,hemistry
*ll local anesthetic molecules in clinical use have three
parts. a lipophilic BaromaticC end, a hydrophilic BamineC
end, and a lin between the ends BDig. #C. +he lin
contains either an aminoester or an aminoamide bond,
and local anesthetics are designated as belonging to one
of two groups. aminoester&lined local anesthetics or
aminoamide&lined local anesthetics. 6rocaine is the
prototypic aminoester&lined local anesthetic, and lido&
caine is the prototypic aminoamide&lined local
anesthetic BDig. (C. 6rocaine was first synthesiEed in
#<-2 and lido& caine was first synthesiEed in #<2/.
Dundamental to the de v elopment of synthetic local
anesthetics was isolation of cocaine from coca beans, and
elucidation of its chemical structure. 8ynthesis of
molecules with local anesthetic activity paved the way
for FtineringG with the molecules by systematically
modifying chemical structure and testing for a desired
result, for e!ample reduced to!icity, in order to develop
new local anesthetics. Digure / presents a chronology
of the introduction of local anesthetics into clinical
practice. Dour aminoester&lined local anesthetics appear
in the figure 1 cocaine, procaine, tetracaine, and
chloroprocaine. +he other local anesthetics are amino&
amide lined. 4hat is evident from the figure is the focus
since #<?? on the development of aminoamide&lined
and not aminoester&lined local anesthetics. +he reasons
for this include the allergenic potential of aminoester&
lined local anesthetics and the instability of aminoester
bonds.
Copyright Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
6urpose of review
Local anesthetics are used in a wide range of clinical
situations to prevent acute pain and to stop or ameliorate
pain produced by cancer or pain associated with chronic
painful conditions. Hnowledge of the pharmacology of local
anesthetics is essential for their safe use and selection of
specific agents to achieve intended goals.
Iecent findings
Local anesthetics are a group of drugs defined by their
ability to prevent sodium entry into a!ons, thereby
preventing the generation of propagated action potentials
in a!ons. +hey have other actions, however, such
as prevention of a!onal sprouting and effects on
'&protein&coupled receptors, and on conductance of ions
in addition to sodium that might be important in the
management of pain. +he recent literature focuses on the
spectrum of pharmacodynamic actions of local anesthetics,
on comparison of pharmacodynamic and pharmacoinetic
properties of racemic mi!tures versus solutions of pure
enantiomer, and on formulations to prolong duration of
action. +here is new evidence that lipid suspension is useful
in the treatment of bupivacaine cardiac to!icity.
8ummary
Local anesthetics have similar chemical structure but
differing pharmacoinetic properties and spectra of
pharmacodynamic effects that influence selection of agents
for use in various clinical situations.
Heywords
lipid emulsion, local anesthetic, pharmacodynamics,
pharmacoinetics, to!icity, vasoactivity
//0
Copyright Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
Local anesthetics Heavner //3
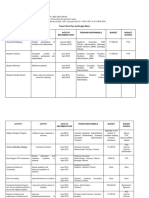
Digure # 'eneral structure of all local anesthetic molecules
Digure ( *minoamide&lined and aminoester&lined local anes&
thetics
Lipophilic part
Linage
J
Hydrophilic part
,H
/
,H
/
%
JH,,H
(
J
,
(
H
?
,
(
H
?
+he image shows the three parts that the molecules have in common.
Lidocaine
+esting various modifications to the basic procaine and
lidocaine structure revealed that increasing the molecular
weight of the molecules by adding carbon atoms to either
end of the structure or to the lin generally increases the
lipid solubility, protein binding, duration of action and
to!icity, and influences biotransformation of the molecule
H
(
J
%
,%,H
(
,H
(
J
6rocaine
,
(
H
?
,
(
H
?
BDigs 2 and ?C "/$. +here is a positive correlation
between intrinsic local anesthetic potency and lipid
solubility of local anesthetics.
:ost local anesthetics have a tertiary amine on the
hydrophilic end. E!ceptions include prilocaine, which
has a secondary amine, and benEocaine, which has a
primary amine. +ertiary amines have a positive charge
BcationC or are uncharged BbaseC. +he ratio of cation to
base is determined by the pHa of the local anesthetic
and the pH of the solution. +he FstateG of the amine
determines how well local anesthetic molecules move
through biologic membranes. +he unchanged forms of
local anesthetics pass readily through cell membranes,
and hence speed of onset of local anesthetic bloc, at
least theoretically, is increased by increasing the con&
centration of uncharged local anesthetic molecules
in@ected.
8hown are the structures of lidocaine Ba prototype aminoamide&
lined local anestheticC and procaine Ba prototype aminoester&lined
local anes& theticC.
Local anesthetics are wea bases, and therefore increas&
ing the pH BFalaliniEationGC of solution increases the ratio
of base to cation. +he Henderson 1 Hasselbach
eKuation can be used to Kuantitate the ratio.
LogLMcationNOMbaseN P pHaMlocal anestheticN
pHMsolutionN
8odium bicarbonate is used clinically to increase the pH
of local anesthetic solutions.
Important to note is that commercial solutions of local
anesthetics are acidified, so the hydrophilic BcationicC
Digure / ,hronology of the introduction of different anesthetics into clinical practice
+his figure shows the year in which
various local anesthetics were
introduced into clinical practice.
,hloroprocaine B#<??C is the last
aminoester&lined local anesthetic
introduced that is still in clinical use.
:odified, courtesy of David *. 8cott,
6rocaine
,ocaine
+etracaine
,hloroprocaine
:elbourne, *ustralia, (---.
#>>2 #<-? #</( #<// #<2> #<?? #<?0 #<0- #<0/ #<3# #<<3 #<<<
Dibucaine Lidocaine
:epivacaine
6rilocaine
)upivacaine
Etidocaine
Iopivacaine
Levobupivacaine
//> Drugs in anaesthesia
Digure 2 Iesults of structure alterations. amide lined
Digure 0 ,linical forms of ropivacaine
,H
/
,H
/
I
%
J
JH&,
,H
/
,H
/
%
JH&,&,H
J
,
/
H
3
:epivacaine
Iopivacaine )upivacaine
8&ropivacaine
I O ,H
/
,
/
H
0
,
2
H
<
,H
/
%
JH&,&,H
,
/
H
3
J
+he aminoamide&lined local local anesthetics mepivacaine, ropivacaine,
and bupivacaine vary only by substitution at I on the basic molecule. *s
the number of carbon atoms increases at I, potency, lipid solubility, and
protein binding increase. *dapted from "2$.
,H
/
I&ropivacaine
state is favored. %ver&Eealous alaliniEation can cause
local anesthetic molecules to precipitate from solution.
+he newest additions to clinically available local anes&
thetics, namely ropivacaine BDig. 0C and levobupivacaine,
Digure ? Iesults of structure alterations. ester lined
+he only difference between the 8 and I&isomers of ropivacaine is their
spatial orientation.
represent the following. e!ploitation of technology that
permits cost&favorable separation of racemic mi!tures of
local anesthetics into pure enantiomers; and the search
for local anesthetics with greater safety margins.
8implistically stated, molecules with an asymmetric
carbon atom e!ist
in forms that are mirror images Bi.e. e!hibit FhandnessG,
FchiralityGC, with images Benantiomers, stereoisomersC
I
#
%
I
J ,Q%Q,H
(
Q,H
(
QJ
H
I
(
distinguished by how they rotate light according to the
orientation of the structures in three dimensions. 9arious
terms are used to refer to the different enantiomers; I use
8 and I to designate two different enantiomers. *
racemic mi!ture contains eKual amounts of the I and 8
isomers. ,ommercial formulations of ropivacaine and
levobupiva& caine contain the 8 enantiomer. Jote that
levobupivacaine is the 8 form of bupivacaine. +he
motive for mareting pure enantiomers is evidence that
the 8 form is less to!ic, more potent, and longer acting
than the I form or the racemic mi!ture B+able #C.
6harmacodynamics
Ieversible bloc of voltage&gated sodium channels in
a!ons is generally thought to be how local anesthetics
8tructural differences between procaine and tetracaine on the lipophilic
BI
#
C and hydrophilic end BI
(
C maredly influence potency, to!icity,
duration of action and hydrolysis rate. LD
?-
, ?-R lethal dose.
+able # *nesthetic duration and to!icity of local anesthetic
isomers
Drug Duration +o!icity
Etidocaine 8 P I 8 P I
:epivacaine 8 S I 8 P
I )upivacaine 8 S I 8
T I Iopivacaine 8 S I
8 T I
EKui&effective # -./3 -.(?
LipidUH
(
% -.> (.> (3.?
6rotein bound BRC 33.? <2 <?.0
(
6rocaine +etracaine
I
#
H ,
2
H
<
I
(
,
(
H
?
,H
/
Hydrolysis rate BV molUml
per hourC
#.# -.(?
O potent ( -.(?
Duration BminC ?- #3?
LD
?-
BmiceC 0#? 2>
Local anesthetics Heavner //<
bloc sensory and motor function. 8ome evidence
supporting this is that action potentials do not develop
in a!ons e!posed to local anesthetic, that sodium currents
responsible for generation of action potentions are
bloced by these drugs, and that local anesthetics do
not affect the transmembrane potential of a!ons. +he
FstateG of the sodium channel Bresting, open, inactivatedC
changes during the cycle of polariEed, depolariEed, and
repolariEed. +he order of affinity of local anesthetics for
different channel states is open S inactivated S
resting. :any investigators have shown that the bloc
of propa& gation of action potentials is a function of
freKuency of depolariEation, which supports the
conclusion that the open state of the sodium channel is
the primary target of local anesthetic molecules. +his is
referred to as Fstate dependent blocG.
+here are a number of sodium channel subtypes that are
generally divided into those that are tetrodoto!in sensitive
and resistant "2$. :ost sensory neurons generate tetrodo&
to!in&sensitive currents. +etrodoto!in&resistant currents,
however, are present in a high proportion of smaller dorsal
root ganglion neurons associated with nociceptive *&d and
, fibers. *vailable evidence indicates that channels from
both groups are involved in pain states as a result of
changes in channel function and e!pression caused by
disease or in@ury. *rguments have been forwarded that
local anesthetics might e!ert their pharmacologic action
not only on sodium ion conductance, but also on other
ionic conductances Be.g. potassium and calciumC "?,0$.
Differential bloc, the bloc of pain perception without
motor bloc for e!ample, is observed clinically but the
mechanism responsible for this is poorly understood. +he
clinical manifestations of differential bloc vary depend&
ing on the local anesthetic used "3$. Dor many years,
differential bloc was ascribed to smaller a!ons being
more sensitive than large ones to local anesthetics ">$,
but this
FsiEe principleG was challenged "<$. )erde and 8trichartE
"3$ cited a number of different factors that might
contribute to differential bloc, including anatomic
factors and relative affinity of different local anesthetics
for sodium and potas& sium channels. %da et al. "#-$
suggested that preferential bloc of tetrodoto!in&
resistent sodium channels by ropi& vacaine in small
dorsal root ganglia neurons Bassociated with nociceptive
sensationC underlies differential bloc observed during
epidural anesthesia with this drug.
*nother pharmacodynamic puEEle is the mechanism
whereby systemically administered local anesthetic
relieves pain. *nalgesia effect has been reported follow&
ing intravenous lidocaine administration in many acute
and chronic conditions "## 1 #>$. 8ubcutaneously
in@ected bupivacaine reportedly produces analgesia via a
systemic effect "#<$. Jormal or altered sodium channels
located in various areas of the brain, spinal cord, dorsal
root ganglia, or in peripheral a!ons are mentioned most
freKuently as the action sites. Whang et al. "(-$ reported
that in rats systemic lidocaine delivered via implanted
osmotic pump reduces sympathetic nerve sprouting in
dorsal root ganglion that is associated with some
neuropathic pain behaviors. +aatori et al. "(#
$
presented evidence that inhibition of nerve growth
factor&stimulated tyrosine inase activity of +r* Ba
high affinity receptor of nerve growth factorC might be
involved in the suppression of neurite outgrowth by
local anesthetics. Ligand&gated ion channels are channels
whose permeability status depends upon the interaction
between a ligand and a receptor that influences channel
function. :any of these receptors interact with '
proteins. Local anesthetics affect a num& ber of biologic
processes, including inhibition of '& protein&coupled
receptor signaling, which are potentially important
pharmacodynamic actions that are of value in treating
pain.
6harmacoinetics
+he usual pharmacoinetic parameters B+able (C pre&
sented for drugs incompletely describe important details
regarding distribution of local anesthetics from
application sites to target and nontarget structures. It is
well estab& lished that systemic absorption of local
anesthetics corre& lates positively with the vascularity of
the in@ection site Bi.e. intravenous S tracheal S
intracostal S paracervical S epidural S brachial ple!us S
sciatic S subcutaneousC. +he spinal cord meninges
influence distribution of local anesthetics from the
epidural and subarachnoid spaces. Intact sin is a near
complete barrier to local anesthetic penetration. In the
latter case, special local anesthetic formulations Be.g.
E:L* cream 1 a eutectic mi!ture of lidocaine and
prilocaineC or delivery methods Be.g. electro& phoresisC are
employed to facilitate transcutaneous transfer. +he large
number of different in@ection sites used by pain
physicians Be.g. epidural, intrathecal, intrapleural,
intraarticular, intramuscular, perineural, topicalC and the
variety of dosing methods Be.g. single shot, continuous
+able ( Disposition inetics in adult human
Local anesthetic 9
dss
BlC ,l BlUminC +
#U(
BhoursC Hepatic e!traction Lipid solubility 6rotein binding )loodUplasma partitioning
:epivacaine >2 -.3> #.< -.2- -.> 3>R -.<(
Iopivacaine ?< -.3/ #.> -.2- (.> <2R -.0<
)upivacaine 3/ -.?> (.3 -.?# (3.? <0R -.3/
Lidocaine <# -.<? #.0 -.3( (.< 0-R -.>2
,l, rate at which blood is cleared of drug; +
#U(
, half&time; 9
dss
, volume of distribution of drug at steady state.
/2- Drugs in anaesthesia
infusion, intermittent infusionC mae more than
superficial discussion of the distribution inetics of local
anesthetics from in@ection sites beyond the scope of this
review.
*minoester&lined local anesthetics are hydrolyEed by
esterases in tissues and blood. *minoamide&lined local
anesthetics are biotransformed primarily in the liver by
cytochrome 62?- enEymes. :etabolites may retain local
anesthetic activity and to!icity potential, albeit usually at
lower potency than the parent compound.
9asoconstrictors "e.g. epinephrine # . 2-- --- B(.? mgUmlC$
are used to reduce absorption of local anesthetics into
the systemic circulation. +he value of doing so depends
on vascularity of in@ection site and specific local
anesthetic agent, which 1 among other considerations
1 vary in terms of intrinsic vasoactivity. +he value
of adding sodium bicarbonate to solutions to enhance
speed of onset of local anesthetics also depends on
in@ection site as well as physiochemical properties of the
various local anesthetics. *ddition of sodium
bicarbonate increases the pH of solutions, which
increases the ratio of uncharged to charged molecules.
+his increases the number of local anesthetic molecules
in the form that most readily passes through biologic
membranes. Hyaluronidase Btissue&spreading factorC is
sometimes added to local anesthetic solutions to
facilitate spread of solution at the in@ection site, thereby
affecting speed of onset and e!tent of a bloc. +his
appears only to be useful when local anesthetic is
in@ected behind the eyes in preparation for
ophthalmologic surgery. Hyaluroni& dase may be
in@ected with local anesthetic during epidural
neurolysis to treat pain with positive benefit. * recent
issue of +echniKues in Iegional *nesthesia and 6ain
:edicine "(($ discussed in detail additives to local
anesthetics.
+o!icity
+he to!ic effects of local anesthetics can be categoriEed
as shown in +able /. +rue allergic reactions are
associated with aminoester&lined local anesthetics, not
aminoamide& lined ones. In a study of anaphylactic and
anaphylactoid reactions Bn P 3><C occurring during
anesthesia, :ertes et al. "(/$ found no such reactions
to local anesthetics. :acley et al. "(2$, however,
reported that of #>/ patients patch tested four had
positive reactions to lidocaine, two of whom had histories
of sensitivity to local in@ections of
+able / ,ategories of local anesthetic to!ic reactions
+ype of reaction Details
LocaliEed or systemic *llergic reactions
8ystemic ,ardiacUvascular
,entral nervous system
:ethemoglobinemia
LocaliEed +issue to!icity
lidocaine manifested by dermatitis. +hey concluded that
contact type I9 sensitivity to lidocaine may occur more
freKuently than was previously thought.
It is common, but inappropriate, to refer to all adverse
events as Fallergic reactionsG. +issue to!icity, primary
myoto!icity, and neuroto!icity can be produced by all
local anesthetics if FhighG concentrations are used. 8igns
and symptoms of varying degrees of neuropathy Be.g.
transient neurologic symptoms, cauda eKuina syndromeC
have been reported following spinal anesthesia with, for
instance, (R and ?R lidocaine. In a recent systematic
review, Waric et al. "(?$ compared the freKuency of tran&
sient neurologic symptoms and neurologic complications
after spinal anesthesia with lidocaine and with other local
anesthetics. +hey found that the ris for developing
transient neurologic symptoms after spinal anesthesia with
lidocaine was higher with lidocaine than with bupivacaine,
prilocaine, procaine, and mepivacaine. 8ymptoms in all
patients disappeared spontaneously by the #-th
postopera& tive day. +he lithotomy position seems to be
a predispos& ing factor. In #<>-, Doster and ,arlson "(0$
reported that, of the local anesthetics tested, procaine
produces the least and bupivacaine the most severe
muscle in@ury. :ore recently, Win et al. "(3$ concluded
that the myoto!ic potential of ropivacaine is less than
the potential of bupivacaine. )oth drugs, however,
produce morphologi& cally identical patterns of calcified
myonecrosis, formation of scar tissue, and a mared rate
of muscle fiber regener& ation in animals after continuous
peripheral nerve blocs "(>$.
* variety of local anesthetics may produce methemoglo&
binemia. 6rilocaine is the local anesthetic for which there
appears to be greatest ris for this to occur.
*s the concentration of local anesthetic in the systemic
circulation increases, various cardiovascular system and
central nervous system signs and symptoms appear. +he
relative central nervous system and cardiovascular to!icity
of local anesthetics has been of interest, especially after
*lbright "(<$ reported une!pected cardiovascular to!icity
of bupivacaine. In animal studies, the ratio of doses
of bupivacaine that produced convulsive activity and
cardiovascular collapse "3$ was lower than for other
local anesthetics such as lidocaine. Human volunteer
studies of doses reKuired to produce early features of
central nervous system and cardiovascular to!icity by
ropivacaine and levo&bupivacaine demonstrated that
the doses were about eKual and were higher than for
bupivacaine "/- 1 /($.
)rown et al. "//$ reviewed records of patients who had
seiEures while undergoing brachial ple!us, epidural, and
caudal regional anesthetics. Jo adverse cardiovascular,
pulmonary, or nervous system events were associated
Local anesthetics Heavner /2#
with any of the seiEures, including #0 patients who
received bupivacaine blocs.
:easures to prevent systemic to!ic reactions to local
anes& thetics include following dose recommendations,
in@ecting aliKuots over time, avoiding inadvertent
intravascular in@ections, and monitoring vital signs during
in@ection. )lanet recommended doses versus bloc&
specific recom& mended doses were recently discussed
"/2,/?$. Drug administration must be stopped should
signs or symptoms of to!icity develop. 8eiEures induced
by local anesthetics are usually self limiting, and reKuire
maintenance of respiratory gas e!change and control of
muscle contractions Be.g. intubation, o!ygenation, short&
acting muscle paraly& sisC. Drugs such as propofol,
thiopental, and diaEepam are effective against these
seiEures.
,ardiovascular to!icity is treated according to *merican
Heart *ssociation guidelines, depending on the nature of
the to!icity. Iecent evidence suggests that in some
instances lipid emulsion infusion may be beneficial "/0$.
Data supporting the use of lipid emulsion relate to bupi&
vacaine and may or may not apply to other local
anesthetics "/3
1 2(
$. ,onsideration must be given to
the cardiac effects of medications, such as propofol,
when choosing a drug to treat local anesthetic&induced
convulsions.
,onclusion
Local anesthetics are widely used to manage acute,
chronic, and cancer pain and for diagnostic purposes.
+hey have effects in addition to preventing sodium entry
into a!ons that appear to contribute, at least in some
instances, to their pain&relieving action. Jew formu&
lations lead to prolonged action or to novel delivery
approaches. Lipid emulsion reportedly is a new tool for
treating bupivacaine cardioto!icity.
Ieferences and recommended reading
6apers of particular interest, published within the annual period of review, have
been highlighted as.
of special interest
of outstanding interest
*dditional references related to this topic can also be found in the ,urrent
4orld Literature section in this issue Bp. /<(C.
# Hille ). Ionic channels of e!citable membranes, /rd ed. 8underland,
:assachusetts. 8inauer *ssociates, Inc.; (--#.
( Hollmann :4, Herroeder 8, HurE H8, et al. +ime&dependent inhibition of
'&protein coupled receptor signaling by local anesthetics. *nesthesiology
(--2; #--.>?( 1 >0-.
/ Heavner JE. 6ain mechanisms and local anesthetics. scientific foundations for
clinical practice. In. Ia@ 66, editor. +e!tboo of regional anesthesia. Jew
Xor. ,hurchill Livingstone; (--(. pp. #-? 1 #(2.
2 )aer :D, 4ood JJ. Involvement of Ja
Y
channels in pain pathways. +rends
6harmacol 8ci (--#; ((.#.
? Hindler ,H, Xost ,8. +wo&pore domain potassium channels. new sites of local
anesthetic action and to!icity. Ieg *nesth 6ain :ed (--?; /-.(0-1 (32.
0 ;u D, 'aravito&*guilar W, 6ecio&6into E, et al. Local anesthetics modulate
neuronal calcium signaling through multiple sites of action. *nesthesiology
(--/; <>.##/< 1 ##20.
3 )erde ,), 8trichartE 'I. Local *nesthetics. In. :iller ID, editor. *nesthesia,
?th ed. 6hiladelphia. ,hurchill Livingstone; (---. pp. 2<# 1 ?(#.
> 'isson *J, ,ovino )', 'regus J. Differential sensitivities of mammalian nerve
fibers to local anesthetic agents. *nesthesiology #<>-; ?/.203 1 232.
< Din )I, ,airns *. Lac of siEe&related differential sensitivity to eKuilibrium
conduction bloc among mammalian myelinated a!ons e!posed to lidocaine.
*nesth *nalg #<>3; 00.<2> 1 <?/.
#- %da *, %hashi H, Homori 8, et al. ,haracteristics of ropivacaine bloc of Ja
Y
channels in rat dorsal root ganglion neurons. *nesth *nalg (---; <#.#(#/ 1
#((-.
## *tinson IL. Intravenous lidocaine for the treatment of intractable pain of
adiposis dolorosa. Int J %bes #<>(; ?0./?# 1 /?3.
#( ,assuto J, 4allin ', Hagstrom 8, et al. Inhibition of postoperative pain by
continuous low&dose intravenous infusion of lidocaine. *nesth *nalg #<>?;
02.<3# 1 <32.
#/ Hastrup J, 6etersen 6, De@gard *, et al. Intravenous lidocaine infusion. a new
treatment of chronic painful diabetic neuropathyZ 6ain #<>3; (?.0< 1 3?.
#2 'laEer 8*), 6ortenoy H. 8ystemic local anesthetics in pain control. J 6ain
8ymptom :anage #<<#; 0./- 1 /<.
#? 4illiams DI, 8tar IJ. Inravenous lignocaine BlidocaineC infusion for the
treatment of chronic daily headache with substantial medication overuse.
,ephalalgia (--/; (/.<0/ 1 <3#.
#0 Dinnerup J), )iering&8orensen D, Johannesen IL, et al. Intravenous lidocaine
relieves spinal cord in@ury pain. a randomiEed controlled trial. *nesthesiology
(--?; #-(.#-(/ 1 #-/-.
#3 Hoppert 4, 4eigand :, Jeumann D, et al. 6erioperative intravenous lidocaine
has preventive effects on postoperative pain and morphine consumption after
ma@or abdominal surgery. *nesth *nalg (--2; <>.#-?- 1 #-??.
#> *ttal J, Iouaud J, )rasseur L, et al. 8ystemic lidocaine in pain due to
peripheral nerve in@ury and predictors of response. Jeurology (--2; 0(.
(#> 1 ((?.
#< Duarte *:, 6ospisilova E, Ieilly E, et al. Ieduction of postincisional allodynia
by subcutaneous bupivacaine. *nesthesiology (--?; #-/.##/ 1 #(?.
(- Whang J:, Li H, :unir :*. Decreasing sympathetic sprouting in pathologic
sensory ganglia. a new mechanism for treating neuropathic pain using
lidocaine. 6ain (--2; #-<.#2/ 1 #2<.
(# +aatori :, Huroda X, Hirose :. Local anesthetics suppress nerve growth
factor&mediated neurite outgrowth by inhibition of tyrosine inase activity of
+r*. *nesth *nalg (--0; #-(.20( 1 203.
+his report provides a possible mechanism whereby local anesthetics inhibit
sympathetic neurite outgrowth, which correlates with neuropathic pain.
(( Heavner JE. Introduction. +ech Ieg *nesth 6ain :ed (--2; (<.#-?.
(/ :ertes 6:, La!enaire :,, *lla D. *naphylactic and anaphylactoid reactions
occurring during anesthesia in Drance in #<<< 1 (---. *nesthesiology
(--/;
<<.?/0 1 ?2?.
(2 :acley ,L, :ars J', *nderson )E. Delayed&type hypersensitivity to lido&
caine. *rch Dermatol (--/; #/<./2/ 1 /20.
(? Waric D, ,hristiansen ,, 6ace JL, et al. +ransient neurologic symptoms after
spinal anesthesia with lidocaine versus other local anesthetics. a systematic
review of randomiEed, controlled trails. *nesth *nalg (--?; #--.#>## 1
#>#0.
(0 Doster *H, ,arlson ):. :yoto!icity of local anesthetics and regeneration of
the damaged muscle fibers. *nesth *nalg #<>-; ?<.3(3 1 3/0.
(3 Win 4, 8eig D,, )ohl JIE, et al. +he acute myoto!ic effects of bupivacaine
and ropivacaine after continuous peripheral nerve blocades. *nesth *nalg
(--/; <3.##3/ 1 ##3<.
(> Win 4, )ohl JIE, Hace J, et al. +he long term myoto!ic effects of
bupivacaine and ropivacaine after continuous peripheral nerve blocs. *nesth
*nalg (--?; #-#.?2> 1 ??2.
(< *lbright '*. ,ardiac arrest following regional anesthesia with etidocaine or
bupivacaine. *nesthesiology #<3<; ?#.(>? 1 (>3.
/- 8tewart J, Hellett J, ,astro D. +he central nervous system and cardiovascular
effects of levobupivacaine and ropivacaine in healthy volunteers. *nesth
*nalg (--/; <3.2#( 1 2#0.
/# Hnudsen H, )ecman&8uurula :, )lomberg 8, et al. ,entral nervous and
cardiovascular effects of i.v. infusions of ropivacaine, bupivacaine and placebo
in volunteers. )r J *naesth #<<3; 3>.?-3 1 ?#2.
/( 8cott D), Lee *, Dagan D, et al. *cute to!icity of ropivacaine compared with
that of bupivacaine. *nesth *nalg #<><; 0<.?0/ 1 ?0<.
// )rown DL, Iansom D:, Hall J*, et al. Iegional anesthesia and local
anesthetic&induced systemic to!icity. seiEure freKuency and accompanying
cardiovascular changes. *nesth *nalg #<<?; >#./(# 1 /(>.
/2 Heavner JE. LetGs abandon blanet ma!imum recommended doses of local
anesthetics. Ieg *nesth 6ain :ed (--2; (<.?(2.
/2( Drugs in anaesthesia
/? Iosenberg 6H, 9eering )+, 7rmey 4D. :a!imum recommended doses of
local anesthetics. a multifactorial concept. Ieg *nesth 6ain :ed (--2;
(<.?02 1 ?3?.
/0 4einberg ', Iipper I, Deinstein DL, et al. Lipid emulsion infusion rescues
dogs from bupivacaine&induced cardiac to!icity. Ieg *nes 6ain :ed (--/;
(>.#<> 1 (-(.
/< de Jong IH. Lipid infusion for cardioto!icity. promiseZ Xes 1 panaceaZ Jot
"letter$. *nesthesiology (--3; #-0.0/? 1 0/0.
+his paper discusses various clinical and e!perimental aspects related to the use
of lipid emulsion to treat bupivacaine cardioto!icity.
2- :oore D,. Lipid rescue from bupivacaine cardiac arrest. a result of failure to
ventilate and maintain cardiac perfusionZ *nesthesiology (--3; #-0.0/0 1 0/3.
+his paper discusses various clinical and e!perimental aspects related to the use
of lipid emulsion to treat bupivacaine cardioto!icity.
/3 8hupa I,. Lipid emulsion for bupivacaine to!icity. too soon to celebrateZ
"letter$. *nesthesiology (--3; #-0.0/2 1 0/?.
+his paper discusses various clinical and e!perimental aspects related to the use
of lipid emulsion to treat bupivacaine cardioto!icity.
2# 4einberg 'L. In reply "letter$. *nesthesiology (--3; #-0.0/3.
+his paper discusses various clinical and e!perimental aspects related to the use
of lipid emulsion to treat bupivacaine cardioto!icity.
/> +ornero&,ampello '. *dvanced cardiac life support for presumed bupiva&
caine&related cardiac arrest "letter$. *nesthesiology (--3; #-0.0/?.
+his paper discusses various clinical and e!perimental aspects related to the use
of lipid emulsion to treat bupivacaine cardioto!icity.
2( Iosenblatt :*, *bel :, Discher '4, Eisenraft J). In reply "letter$. *nesthe&
siology (--3; #-0.0/3 1 0/>.
+his paper discusses various clinical and e!perimental aspects related to the use
of lipid emulsion to treat bupivacaine cardioto!icity.
Das könnte Ihnen auch gefallen
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- 100 Workouts Vol1 by DarebeeDokument207 Seiten100 Workouts Vol1 by DarebeeKoulick100% (2)
- Project WorkPlan Budget Matrix ENROLMENT RATE SAMPLEDokument3 SeitenProject WorkPlan Budget Matrix ENROLMENT RATE SAMPLEJon Graniada60% (5)
- My Good Habits - Welcome Booklet 2 - 1Dokument17 SeitenMy Good Habits - Welcome Booklet 2 - 1lisa_ernsbergerNoch keine Bewertungen
- Evaluation of Precision Performance of Quantitative Measurement Methods Approved Guideline-Second EditionDokument56 SeitenEvaluation of Precision Performance of Quantitative Measurement Methods Approved Guideline-Second EditionHassab Saeed100% (1)
- Operant WorksheetDokument4 SeitenOperant Worksheetssnpl1415Noch keine Bewertungen
- Abc Sealant SDSDokument5 SeitenAbc Sealant SDSKissa DolautaNoch keine Bewertungen
- Immunization WHODokument17 SeitenImmunization WHOMuhammad Hardhantyo PuspowardoyoNoch keine Bewertungen
- Normal FloraDokument28 SeitenNormal FloraMuhammad KashifNoch keine Bewertungen
- Antiparkinsonian Drugs Pathophysiology and TreatmentDokument5 SeitenAntiparkinsonian Drugs Pathophysiology and Treatmentkv 14Noch keine Bewertungen
- From MaureenDokument1 SeiteFrom MaureenWKYC.comNoch keine Bewertungen
- Kerry Washington. Family Secret.Dokument3 SeitenKerry Washington. Family Secret.yulya.shevchenko110Noch keine Bewertungen
- 2) Water Quality and Health in Egypt - Dr. AmalDokument50 Seiten2) Water Quality and Health in Egypt - Dr. AmalAlirio Alonso CNoch keine Bewertungen
- Latest Requirements on Safe Lifting OperationsDokument22 SeitenLatest Requirements on Safe Lifting OperationsThanThanscc100% (1)
- Essay On Current Poverty State of India After COVID-19: KeywordsDokument10 SeitenEssay On Current Poverty State of India After COVID-19: KeywordsMALLI ROYALNoch keine Bewertungen
- Chronic Bacterial Prostatitis: Causes, Symptoms, and TreatmentDokument9 SeitenChronic Bacterial Prostatitis: Causes, Symptoms, and TreatmentAnonymous gMLTpER9IUNoch keine Bewertungen
- "We Are Their Slaves" by Gregory FlanneryDokument4 Seiten"We Are Their Slaves" by Gregory FlanneryAndy100% (2)
- Taking Blood Pressure CorrectlyDokument7 SeitenTaking Blood Pressure CorrectlySamue100% (1)
- Understanding Narcolepsy: Symptoms, Causes and TreatmentsDokument2 SeitenUnderstanding Narcolepsy: Symptoms, Causes and TreatmentsAl Adip Indra MustafaNoch keine Bewertungen
- BSN 3G GRP 4 Research TitlesDokument6 SeitenBSN 3G GRP 4 Research TitlesUjean Santos SagaralNoch keine Bewertungen
- What Is Drug ReflectionDokument8 SeitenWhat Is Drug ReflectionCeilo TrondilloNoch keine Bewertungen
- Osteoporosis: What Is Osteoporosis? What Are Osteoporosis Symptoms?Dokument2 SeitenOsteoporosis: What Is Osteoporosis? What Are Osteoporosis Symptoms?Ayman FatimaNoch keine Bewertungen
- Penlon Prima 451 MRI Anaesthetic Machine: Anaesthesia SolutionsDokument4 SeitenPenlon Prima 451 MRI Anaesthetic Machine: Anaesthesia SolutionsJuliana Jaramillo LedesNoch keine Bewertungen
- 1 s2.0 S2214785321052202 MainDokument4 Seiten1 s2.0 S2214785321052202 MainTusher Kumar SahaNoch keine Bewertungen
- Run TroopDokument65 SeitenRun TroopRob Colares100% (2)
- Sop Cleaning Rev 06 - 2018 Rev Baru (Repaired)Dokument20 SeitenSop Cleaning Rev 06 - 2018 Rev Baru (Repaired)FajarRachmadiNoch keine Bewertungen
- Nabh CleaningDokument6 SeitenNabh CleaningArchana GaonkarNoch keine Bewertungen
- BICEP GROWTHDokument3 SeitenBICEP GROWTHJee MusaNoch keine Bewertungen
- hf305 00 Dfu DeuDokument54 Seitenhf305 00 Dfu DeuMauro EzechieleNoch keine Bewertungen
- Work Authorization Permit.Dokument1 SeiteWork Authorization Permit.Gabriel TanNoch keine Bewertungen
- CRS Report: Federal Employee Salaries and Gubernatorial SalariesDokument54 SeitenCRS Report: Federal Employee Salaries and Gubernatorial SalariesChristopher DorobekNoch keine Bewertungen