Beruflich Dokumente
Kultur Dokumente
Neuromediatorii in Ochiul Uscat
Hochgeladen von
Diana Elena0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
32 Ansichten6 SeitenNerve growth factor tear levels were significantly increased in participants with dry eye disease. CGRP and NPY but not NGF were changed in autoimmune dry eye diseases.
Originalbeschreibung:
Copyright
© © All Rights Reserved
Verfügbare Formate
PDF, TXT oder online auf Scribd lesen
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenNerve growth factor tear levels were significantly increased in participants with dry eye disease. CGRP and NPY but not NGF were changed in autoimmune dry eye diseases.
Copyright:
© All Rights Reserved
Verfügbare Formate
Als PDF, TXT herunterladen oder online auf Scribd lesen
0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
32 Ansichten6 SeitenNeuromediatorii in Ochiul Uscat
Hochgeladen von
Diana ElenaNerve growth factor tear levels were significantly increased in participants with dry eye disease. CGRP and NPY but not NGF were changed in autoimmune dry eye diseases.
Copyright:
© All Rights Reserved
Verfügbare Formate
Als PDF, TXT herunterladen oder online auf Scribd lesen
Sie sind auf Seite 1von 6
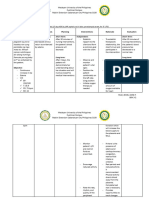
CLINICAL SCIENCES
Alterations of Tear Neuromediators
in Dry Eye Disease
Alessandro Lambiase, MD, PhD; Alessandra Micera, PhD; Marta Sacchetti, MD, PhD;
Magdalena Cortes, MD; Flavio Mantelli, MD; Stefano Bonini, MD
Objectives: To evaluate tear levels of neuromediators
in patients with dry eye disease and to identify statisti-
cal correlations with the clinical findings.
Methods: Nineteenpatients withdry eye disease (Sjo gren
syndrome, n=5 patients; nonSjo gren syndrome, n=10;
and ocular cicatricial pemphigoid, n=4) and 12 healthy
volunteers were enrolled. The eyes of all participants were
evaluated by slitlamp examination, Schirmer testing, fluo-
rescein staining, and tear filmbreak-up time. Grading of
dry eye severity was recorded. Tear samples were col-
lected, and substance P, calcitonin generelated peptide
(CGRP), neuropeptide Y(NPY), vasoactive intestinal pep-
tide, and nerve growth factor (NGF) concentrations were
evaluated by enzyme-linked immunoassay and corre-
lated with the clinical findings.
Results: Nerve growth factor tear levels were signifi-
cantly increasedinparticipants withdry eye disease; CGRP
andNPYconcentrations were significantly decreasedwhen
compared with those in healthy participants. Dry eye se-
verity showed a direct correlation with NGF and an in-
verse correlation with CGRP and NPY tear levels. Nerve
growth factor tear levels showed a direct correlation with
conjunctival hyperemia and fluorescein staining results,
CGRPdirectlycorrelatedwithSchirmer test values, andNPY
inversely correlated with tear film break-up time. Sub-
group analysis showed that CGRP and NPY but not NGF
were changed in autoimmune (ie, Sjo gren syndrome and
ocular cicatricial pemphigoid) dry eye disease.
Conclusions: The decreased tear levels of NPYand CGRP
in dry eye disease are related to impaired lacrimal func-
tion, and tear levels of NGF are more closely related to
corneal epithelial damage. Our findings suggest that NPY,
CGRP, and NGF could become useful markers of dry eye
severity.
Arch Ophthalmol. 2011;129(8):981-986
T
HE OCULAR SURFACE IS EX-
tensively supplied by sen-
sory and autonomic nerve
fibers that play a crucial role
in maintaining healthy epi-
thelia and represent the main sources of
neurogenic inflammation.
1- 3
Cross-
communication between the nervous and
immune systems is shown by the release
and binding of common neuromediators
and cytokines.
4-6
Specifically, substance P
(SP), calcitonin generelated peptide
(CGRP), vasoactive intestinal peptide
(VIP), and neuropeptide Y (NPY) are re-
leased fromocular surface epithelial cells,
lacrimal gland tissues, and nerve endings
at inflammatory sites, modulating the in-
filtration and activation of the immune
cells andtriggering the reflexof tearing and
ocular discomfort.
7,8
Evidence suggests that neuromedia-
tors are involved in chronic ocular sur-
face diseases such as dry eye. Dry eye is a
complex disease characterized by changes
in the ocular surface related to reduced
quality and/or quantity of tears, inflam-
matory reaction, and impairment of ocu-
lar surface sensitivity.
9,10
Lacrimal gland
function is regulated by the nervous sys-
tem, with autonomic and sensory nerves
being capable of influencing acinar gland
secretion and inflammatory reactions
through the release of neuromedia-
tors.
8,11,12
Substance P and CGRP pro-
mote local inflammationby inducing blood
vessel dilatation, leukocyte extravasa-
tion, immune cell activation, and synthe-
sis and release of several cytokines.
8,13-15
Vasoactive intestinal peptide and NPY ex-
ert anti-inflammatory actions by inhibit-
ing T-cell proliferation and helper T-cell
type 1 response and modulating the re-
lease of cytokines, chemokines, and ni-
tric oxide.
16-20
This neuroimmune cross-
communication is capable of modulating
local inflammation by enhancing sensory
nerve excitability and triggering the acti-
vation of different immune cell types.
Changes in circulating levels of neuro-
peptides and neurotrophins, as well as the
Author Affiliations:
Department of Ophthalmology,
Campus Bio-Medico, University
of Rome (Drs Lambiase, Micera,
Sacchetti, Cortes, Mantelli, and
Bonini), and Istituto di
Recovero e Cura a Carattere
Scientifico G. B. Bietti Eye
Foundation (Dr Micera),
Rome, Italy.
ARCH OPHTHALMOL/ VOL 129 (NO. 8), AUG 2011 WWW.ARCHOPHTHALMOL.COM
981
2011 American Medical Association. All rights reserved.
Downloaded From: http://archopht.jamanetwork.com/ on 12/04/2013
impairment of salivary gland innervation in patients with
Sjo gren syndrome, have been demonstrated.
21-24
These
changes are hypothesizedtobe a cause of salivary fluidflow
decrease during Sjo gren syndrome. In fact, a remarkable
discrepancy canbe observedbetweenthe inflammatory in-
volvement of the glands andthe decrease influidflow. One
possible explanationis that this autoimmune disease and/or
local inflammationmay cause vasoneural dysregulationof
and injury to the peripheral nerves, leading to decreased
fluid flowand atrophy of the acinar cells.
25,26
Patients with
autoimmune diseases are known to have a decrease in cir-
culating levels of NPY, and the salivary glands of patients
withSjo grensyndrome have reducedNPY-containingnerve
terminals.
25
Of interest, an increase in nerve growth factor
(NGF) tear levels also has been reported in patients with
dry eye disease.
27
Nerve growth factor is a neurotrophin
exerting a pleiotropic action on the ocular surface, modu-
lating immune reaction, sensitivity, corneal and conjunc-
tival epithelia proliferation, and differentiation and stimu-
lation of mucin production by goblet cells.
28
The aim of this study was to measure the tear con-
tent of VIP, NPY, CGRP, SP, and NGF in patients af-
fected by Sjo gren syndrome and nonSjo gren syndrome
dry eye disease compared with that of healthy volun-
teers. Potential correlations with the clinical character-
istics of the patients also were evaluated.
METHODS
PARTICIPANTS AND
TEAR SAMPLE COLLECTION
The study was performed in accordance with the Declaration
of Helsinki for research involving humans, and the Intramural
Ethics Committee approved the project. Informed consent waiv-
ers were signed by each participant.
Participants included 12 healthy individuals (8 men and 4
women; mean [SD] age, 41 [21] years) and 19 patients (4 men
and 15 women; 68 [13] years) with dry eye disease due to
Sjo gren syndrome (n=5), nonSjo gren syndrome (n=10), or
ocular cicatricial pemphigoid (n=4), with no history of other
ocular diseases.
The diagnosis of dry eye disease was based on clinical his-
tory and the results of slitlamp examination, Schirmer testing,
ocular surface fluorescein staining, and tear filmbreak-up time.
Conjunctival hyperemia was gradedas follows: 0, absent; 1, mild;
2, moderate; and 3, severe. Corneal staining was recorded and
graded according to the Oxford scheme. Dry eye severity grad-
ing from 1 to 4 was recorded according to the Dry Eye Work-
Shop classification.
29,30
Evaluation by an immunologist and bio-
chemical investigations were performed to identify systemic
autoimmune diseases.
Tear samples were collected without anesthetic from all
participants using dry microsponges (Sharp-tip Micro-
sponges; Alcon Laboratory Inc, Fort Worth, Texas) inserted
simultaneously in the inferior conjunctival fornix of both
eyes, removed after 60 seconds, and then immediately im-
mersed in a 1.5-mL Eppendorf vial containing 50 L of tissue
protein extractor solution (T-PER; Thermo Scientific Pierce
Protein Research Products, Rockford, Illinois) with 10 g/mL
of aprotinin and 1 mMof phenyl methyl sulfonyl fluoride. Mi-
crosponges were then centrifuged to dryness at 13 000 rpm
for 3 minutes to recover tears. The amount of fluid recovered
was determined, as previously described.
31
Briefly, it was ob-
tained by weighing the sponge and the tube after the absorp-
tion and centrifugation steps. The protein profile of the tears
was then recorded (A280 program of a NanoDrop ND-1000
UV-Vis Spectrophotometer; NanoDrop Technologies Inc,
Wilmington, Delaware).
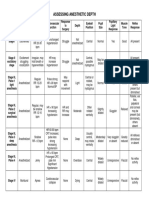
Table 1. Characteristics of Participants
With Dry Eye Disease
Characteristic Value
Patients, No. 19
Sex, No.
Male 4
Female 15
Age, y
Range 45-82
Mean (SD) 68 (13)
Dry eye type, No.
NonSjogren syndrome 10
Sjogren syndrome 5
Ocular cicatricial pemphigoid 4
Conjunctival hyperemia score
Median (range) 1 (0-2)
Mean (SD) 0.9 (0.7)
Schirmer test, mm/5 min
Median (range) 4 (1-10)
Mean (SD) 4.4 (3.1)
Tear film break-up time, s
Median (range) 4.0 (3.0-5.0)
Mean (SD) 3.7 (1.3)
Oxford score
Median (range) 3 (0-5)
Mean (SD) 1.8 (1.6)
9.0
7.0
8.0
6.0
3.0
2.0
1.0
5.0
4.0
0
SP
N
P
Y
T
e
a
r
L
e
v
e
l
,
n
g
/
m
L
A
Healthy
Dry eye
Healthy
Dry eye
CGRP NPY VIP
250.0
150.0
100.0
200.0
50.0
0
T
e
a
r
L
e
v
e
l
,
p
g
/
m
L
B
NGF
Figure 1. Changes in tear levels in patients with dry eye disease compared
with healthy participants. A, Significant decrease in tear levels of calcitonin
generelated peptide (CGRP) (P=.001) and neuropeptide Y (NPY) (P=.01),
but not of substance P (SP) and vasoactive intestinal peptide (VIP) in
patients with dry eye. B, Nerve growth factor (NGF) tear concentration
significantly increased in patients with dry eye (P=.02).
ARCH OPHTHALMOL/ VOL 129 (NO. 8), AUG 2011 WWW.ARCHOPHTHALMOL.COM
982
2011 American Medical Association. All rights reserved.
Downloaded From: http://archopht.jamanetwork.com/ on 12/04/2013
NEUROPEPTIDES
AND NGF DETERMINATION
Specific enzyme-linked immunoassay was performed on ex-
tracted proteins to quantify the amount of neuropeptides in
tear samples, using specific commercially available kits and
following the manufacturers instructions (Phoenix Pharma-
ceuticals Inc, Burlingame, California; detection limits: NPY,
0.09 ng/mL; SP, 0.07 ng/mL; CGRP, 0.28 ng/mL; and VIP,
0.12 ng/mL).
To evaluate NGF concentration in the tear samples, we
performed a 2-site NGF enzyme-linked immunoassay (sensi-
tivity, 0.5 pg/mL).
32
In brief, 96-well Maxisorp enzyme-linked
immunoassay plates were precoated with monoclonal anti-
human NGF antibodies (0.4 g/mL; MAB256; R&D Systems
Inc, Minneapolis, Minnesota). Standards (0.15 pg/mL to 1
ng/mL NGF; Alomone Labs, Jerusalem, Israel) and samples
were incubated at 4C for 18 hours. Enzyme-linked immuno-
assay was developed by using polyclonal biotinylated anti-
human NGF antibodies (0.15 g/mL, 500-P85Bt; PeproTech,
Milan, Italy), horseradish peroxidase streptavidin (R&D Sys-
tems) (1:300; DY998, RD), and the ready-to-use 3,3,5,5-
tetramethylbenzidine substrate (Zymed Laboratories, San
Francisco, California).
Optical density was measured at 450 to 550 by a micro-
plate enzyme-linked immunoassay reader (Sunrise; Tecan Sys-
tems Inc, San Jose, California). All samples were evaluated in
duplicate. Data are expressed as neuropeptide concentration
per milliliter.
STATISTICAL ANALYSIS
Data are presented as mean(SD), median, minimum, and maxi-
mumvalues. The nonparametric Mann-Whitney test was used
to compare tear levels of neuropeptides between patients with
dry eye disease and healthy participants and between patients
in different dry eye subgroups (Sjo gren syndrome, non
Sjo gren syndrome, and ocular cicatricial pemphigoid). Spear-
man correlation analysis was performed to identify relation-
ships between clinical variables and neuromediator tear levels
(SPSS 15.0; SPSS Inc, Chicago, Illinois). P.05 was consid-
ered statistically significant.
RESULTS
Nineteen patients with dry eye disease were included in
the study. According to the etiology of the disease, pa-
tients were further divided: nonSjo gren syndrome
(n=10); Sjo gren syndrome (n=5), and ocular cicatricial
pemphigoid (n=4) (Table 1).
Compared with healthy participants, patients with dry
eye disease showed a significant decrease in tear levels of
CGRP (mean [SD], 3.6 [2.3] ng/mL; median, 3.0 [range,
0.2-9.3] ng/mL vs mean, 6.0 [2.2] ng/mL; median, 5.8
[range, 2.5-10.5] ng/mL; P=.01) andNPY(mean, 3.1 [3.3]
ng/mL; median, 1.6 (range, 0.2-9.6) ng/mL vs mean, 4.3
[1.9] ng/mL; median, 4.3[range, 1.6-33.1] ng/mL; P=.011),
but not of SP and VIP (Figure 1A). Figure 1B shows that
NGF tear concentration was significantly increased in
patients with dry eye disease (mean, 137.7 [79.4] pg/mL;
median, 150 [range, 22-327] pg/mL vs mean, 64.7 [48.0]
pg/mL; median, 64.7 [range, 7.3-135.2] pg/mL; P=.02).
Neuromediators tear levels showed significant corre-
lations with clinical variables and dry eye severity grade.
Dry eye severity grading was inversely correlated with
CGRP and NPY (P.001 and P=.049, respectively) and
directly with NGF (P=.009) tear levels (Table 2).
Conjunctival hyperemia was directly correlated with
NGF tear levels (P=.01); the Oxford score showed an in-
verse correlation with CGRP and NPYtear levels (P=.001
and P=.005, respectively) and a direct correlation with
NGF tear concentration (P=.006). Schirmer test values
showed a direct correlation with CGRP (P=.003), and
tear film break-up time values were inversely correlated
with NPY tear levels (P=.006).
Also, CGRP tear levels were significantly decreased in
patients with dry eye disease who had severe reduction
in Schirmer test values (mean, 2.2 [1.3] ng/mL) when
compared with those of patients with moderate reduc-
tion (mean, 4.0 [1.7] ng/mL; P=.03) (Figure 2A). Neu-
ropeptide Y tear levels were significantly increased in pa-
tients with dry eye disease who had lower tear film
break-up time values (mean 7.6 [3.0] ng/mL) when com-
pared with patients with moderate reduction (mean, 2.2
[2.4] ng/mL; P=.02) (Figure 2B).
Different neuromediator patterns were observed in the
3 dry eye disease subgroups when compared with the
healthy participants (Table 3 and Figure 3). Specifi-
cally, in nonSjo gren syndrome, CGRP was signifi-
cantly decreased (P.001) and NGF was significantly
increased (P=.002). In ocular cicatricial pemphigoid,
CGRP was significantly decreased (P.001). In Sjo gren
syndrome, only NPYwas significantly decreased(P=.006).
These findings in neuromediator tear levels in the dry
eye disease subgroups were not related to any difference
in clinical severity; clinical signs (ie, conjunctival hyper-
emia and Oxford score) and tear film variables (ie,
Table 2. Correlation of Neuropeptide Tear Levels With Clinical Variables
Characteristic
Spearman Correlation
SP CGRP NPY VIP NGF
Conjunctival hyperemia P = .29 P = .07 P = .54 P = .90 P = .01; R = 0.489
Schirmer test P = .97 P = .003; R = 0.574 P = .19 P = .61 P = .34
BUT P = .45 P = .20 P = .006; R = 0.741 P = .73 P = .58
Oxford score P = .87 P .001; R = 0.629 P = .005; R = 0.526 P = .24 P = .006; R = 0.513
Dry eye severity grade P = .59 P .001; R = 0.674 P = .049; R = 0.515 P = .80 P = .009; R = 0.495
Abbreviations: BUT, tear film break-up time; CGRP, calcitonin generelated peptide; NGF, nerve growth factor; NPY, neuropeptide Y; SP, substance P;
VIP, vasoactive intestinal peptide.
ARCH OPHTHALMOL/ VOL 129 (NO. 8), AUG 2011 WWW.ARCHOPHTHALMOL.COM
983
2011 American Medical Association. All rights reserved.
Downloaded From: http://archopht.jamanetwork.com/ on 12/04/2013
Schirmer test and break-up time values) were not sig-
nificantly different between subgroups (Table 4).
COMMENT
Dry eye is a multifactorial disease characterized by de-
creased tear flow, conjunctival inflammation, impairment
of corneal sensitivity, decrease in goblet cell density, epi-
thelial metaplasia, and corneal damage, frequently lead-
ing to visual impairment.
9
It is well known
33
that normal
tear flow is regulated by a fine balance between the para-
sympathetic, sympathetic, and sensory nerves. In fact, the
autonomic and sensory nerves locally release several me-
diators that are able to influence acinar gland secretion as
well as the inflammatory reactionat the lacrimal glandand
the conjunctiva.
1
The main causes of this neurogenic in-
flammation are considered to be SP and CGRP, both re-
leased by the sensory nerves. In this study, we demon-
strateda significant decrease inCGRPinthe tears of patients
affected by dry eye; although not significant, a trend of de-
crease inSPalsowas observedinpatients withdryeye. Also,
inthose patients, we observeda significant decrease inNPY
and a significant increase in NGF; changes in VIP levels
were not significant. These results suggest that at least
CGRP, NPY, andNGFare involvedindryeye disease. How-
ever, because the source of these factors was not estab-
lished in this study, it is unclear whether these alterations
in the tears of patients with dry eye represent a patho-
genic mechanism of the disease or whether they may re-
sult fromchanges inthe ocular surface of dryeyes. We hope
that these aspects will be investigated in studies aimed at
6.0
4.0
3.0
5.0
1.0
2.0
0
T
e
a
r
L
e
v
e
l
,
n
g
/
m
L
A
= 5 mm/5 min
Schirmer Test Values
BUT Values
NPY
CGRP
<5 mm/ 5 m
12.0
8.0
6.0
10.0
2.0
4.0
0
T
e
a
r
L
e
v
e
l
,
n
g
/
m
L
B
= 4 s <4 s
Figure 2. Tear levels as evaluated by clinical tests. A, Calcitonin generelated
peptide (CGRP) tear levels are significantly lower in patients with severe
aqueous deficiency (ie, Schirmer test values 5 mm/5 min). B, Neuropeptide
Y (NPY) tear levels are significantly higher in patients with severe evaporative
dry eye disease (ie, tear film break-up time [BUT], 4 s).
Table 3. Tear Neuromediator Levels in Dry Eye Disease
Subgroups Compared With Healthy Participants
Variable CGRP, ng/mL NPY, ng/mL NGF, pg/mL
Healthy
Mean (SD) 6.0 (2.2) 4.3 (1.9) 64.7 (48.0)
Median (range) 5.8 (2.5-10.5) 4.3 (1.6-32.0) 64.7 (7.3-135.2)
Total dry eye
Mean (SD) 3.6 (2.3) 3.1 (3.3) 137.7 (79.4)
Median (range) 3.0 (0.2-9.3)
a
1.6 (0.2-9.6)
b
150.0 (22.0-328.0)
b
Sjogren syndrome
Mean (SD) 6.0 (2.4) 1.5 (0.3) 54.5 (61.8)
Median ( range) 6.3 (2.6-9.3) 1.4 (1.1-1.9)
b
28.9 (22.0-179.0)
NonSjogren
syndrome
Mean (SD) 3.0 (1.7) 4.6 (3.9) 186.5 (64.8)
Median (range) 3.0 (0.2-6.3)
a
3.2 (0.6-9.6) 167.6 (118.4-328.0)
a
OCP
Mean (SD) 2.3 (1.2) 1.5 (2.0) 120.8 (53.3)
Median (range) 2.3 (0.6-4.4)
a
0.5 (0.2-3.9) 144.2 (39.9-169.6)
Abbreviations: CGRP, calcitonin generelated peptide; NGF, nerve growth
factor; NPY, neuropeptide Y; OCP, ocular cicatricial pemphigoid.
a
P.01.
b
P.05.
9.0
7.0
8.0
6.0
3.0
2.0
1.0
5.0
4.0
0
T
e
a
r
L
e
v
e
l
,
n
g
/
m
L
B
Healthy Non-SS SS OCP
Healthy Non-SS
NGF
NPY
CGRP
SS OCP
300.0
150.0
100.0
200.0
250.0
50.0
0
T
e
a
r
L
e
v
e
l
,
p
g
/
m
L
C
9.0
7.0
8.0
6.0
3.0
2.0
1.0
5.0
4.0
0
T
e
a
r
L
e
v
e
l
,
n
g
/
m
L
A
Healthy Non-SS SS OCP
Figure 3. Changes in neuromediator tear levels in Sjogren syndrome (SS),
non-SS, and ocular cicatricial pemphigoid (OCP). A, Calcitonin generelated
peptide (CGRP) was significantly decreased (P.001) in non-SS and in OCP
(P.001). B. Neuropeptide Y (NPY) was significantly decreased in SS
(P=.006). C, Nerve growth factor (NGF) was increased in patients without SS
(P=.002). *Indicates a statistically significant difference.
ARCH OPHTHALMOL/ VOL 129 (NO. 8), AUG 2011 WWW.ARCHOPHTHALMOL.COM
984
2011 American Medical Association. All rights reserved.
Downloaded From: http://archopht.jamanetwork.com/ on 12/04/2013
addressing the clinical implications of our results; how-
ever, several hypotheses may be created based on our re-
sults. The decreased levels of CGRP and NPY may be re-
lated to changes in lacrimal gland function. In fact, both
of these neuromediators are present in the lacrimal gland,
and changes in their concentration have been demon-
strated in the salivary glands of patients with Sjo gren syn-
drome.
21
A decrease in the circulating levels of NPY also
has beendescribedinpatients affectedby autoimmune dis-
eases, which is in line with the anti-inflammatory role of
this neuropeptide.
18,25
In fact, NPY treatment is known
19
to inhibit experimental autoimmune encephalomyelitis, a
model of helper T-cell type 1driven disease, by inhibit-
ing helper T-cell type 1driven inflammatory responses.
The explanation of the decrease in CGRP in dry eye
disease is more complex. Apparently in contrast with our
results, this neuropeptide is considered to be a major
source of neurogenic inflammation. Specifically, CGRP
is known
13
to dilate blood vessels, to stimulate leuko-
cyte extravasation, and to induce the synthesis of sev-
eral cytokines (eg, interleukin8) by corneal epithelial cells.
However, recent evidence also suggests a more complex
role of CGRP in modulating inflammatory reactions: in
the epidermis, release of CGRP fromsensory nerves can
inhibit antigen presentation by Langerhan cells and im-
pair contact hypersensitivity by triggering mast cell re-
lease of tumor necrosis factor.
15,20
Moreover, to our knowl-
edge, no published evidence exists of a well-defined
proinflammatory or anti-inflammatory role of CGRP at
the ocular surface; the decrease in ocular surface sensi-
tivity demonstrated in patients with dry eye may be the
origin of the decreased tear concentration of this sen-
sory neuropeptide.
34
One could also speculate that the
decrease in CGRP in the tears partly may be responsible
for reduced mucin secretion by goblet cells, which is a
characteristic of dry eye disease.
35
Of interest, CGRP and NPY tear levels showed oppo-
site changes compared with NGF; our results suggest
that these neuromediators play a different role in the
pathophysiologic mechanisms of dry eye disease. Our
data showing an increase in NGF tear levels in patients
with dry eye are in line with the well-known neural sen-
sitizing role of this neuromediator and with the obser-
vations published by Lee et al.
27
However, our results
also showed a direct correlation between NGF tear lev-
els and the severity of corneal damage (as assessed by
the Oxford test), as well as with conjunctival hyper-
emia. These observations suggest that NGF may be in-
volved more with local tissue damage than with the dis-
ease pathogenesis. To support this hypothesis, when
splitting our results in the different dry eye disease sub-
groups, NGF tear levels are increased only in patients
with nonSjo gren syndrome dry eye. Moreover, it has
been widely demonstrated that NGF exerts a potent ac-
tion on corneal healing in physiologic and pathologic
conditions, and it has been shown in several animal
models that corneal injuries induce an increase in local
NGF and NGF receptors capable of stimulating epithe-
lial healing.
32
However, the increase in NGF tear levels
that we observed in dry eye also could be the result of
an increased release by the lacrimal gland because, in
animals and humans, lacrimal glands are known to pro-
duce, release, and be responsive to NGF.
36
The findings of this study provide evidence of an im-
balance of neuromediators in the tear film of patients
with dry eye disease. Although further studies will be
needed to demonstrate the source of each altered neuro-
mediator in patients with dry eye, it is possible to specu-
late that changes in neuromediators tear levels may con-
tribute to the disease pathogenesis rather than being a
mere epiphenomenon. In fact, locally released neuropep-
tides are crucial to conserving the homeostasis of the
ocular surface by acting on the epithelia, blood vessels,
and immune cells infiltrating the conjunctiva, as well as
by modulating inflammatory responses, epithelial cell
differentiation and proliferation, and conjunctival mucin
secretion.
1
Although several studies highlighted the cru-
cial role of neuropeptides on lacrimal gland inflamma-
tion in dry eye, only NGF was shown
27
to be increased in
the tears of patients with the disease. Our data suggest
that this increase in NGF probably is not related to the
pathogenesis of dry eye but is the result of ocular surface
damage. Moreover, our study shows that NPY and CGRP
tear levels correlate with dry eye severity, opening ven-
ues to further investigation regarding their potential use
as therapeutic targets and diagnostic markers.
Submitted for Publication: September 29, 2010; final re-
vision received December 12, 2010; accepted December
13, 2010.
Correspondence: Stefano Bonini, MD, Department of
Ophthalmology, University of Rome, Campus Bio-
Table 4. Clinical Characteristics of Dry Eye Disease Subgroups
Characteristic
Conjunctival
Hyperemia Schirmer Test BUT Oxford Score
Dry Eye
Severity Grade
Sjogren syndrome (n = 5)
Mean (SD) 1.0 (0.9) 5.6 (3.6) 4.3 (0.5) 2.1 (1.8) 2.2 (1.2)
Median (range) 1.0 (0-2.0) 5.0 (2.0-10.0) 4.0 (4.0-5.0) 3.0 (0-4.0) 2.0 (1.0-4.0)
NonSjogren syndrome (n = 10)
Mean (SD) 1.0 (0.5) 3.9 (2.0) 3.7 (0.6) 2.8 (1.0) 3.0 (1.0)
Median (range) 1.0 (0-2.0) 3.5 (1.0-7.0) 4.0 (3.0-5.0) 3.0 (2.0-5.0) 3.0 (1.0-4.0)
Ocular cicatricial pemphigoid (n = 4)
Mean (SD) 0.9 (0.7) 4.5 (3.3) 3.3 (1.7) 2.3 (1.5) 2.5 (1.2)
Median (range) 1.0 (0-1.0) 3.5 (0-13.0) 2.5 (0-5.0) 2.5 (1.0-3.0) 1.0 (1.0-3.0)
Abbreviation: BUT, tear film break-up time.
ARCH OPHTHALMOL/ VOL 129 (NO. 8), AUG 2011 WWW.ARCHOPHTHALMOL.COM
985
2011 American Medical Association. All rights reserved.
Downloaded From: http://archopht.jamanetwork.com/ on 12/04/2013
Medico, Via Alvaro del Portillo 200, 00128 Rome, Italy
(s.bonini@unicampus.it).
Financial Disclosure: None reported.
REFERENCES
1. Beuerman RW, Stern ME. Neurogenic inflammation: a first line of defense for
the ocular surface. Ocul Surf. 2005;3(4)(suppl):S203-S206.
2. Goetzl EJ, Sreedharan SP. Mediators of communication and adaptation in the
neuroendocrine and immune systems. FASEB J. 1992;6(9):2646-2652.
3. Lambrecht BN. Immunologists getting nervous: neuropeptides, dendritic cells
and T cell activation. Respir Res. 2001;2(3):133-138.
4. De Swert KO, Joos GF. Extending the understanding of sensory neuropeptides.
Eur J Pharmacol. 2006;533(1-3):171-181.
5. Melik-Parsadaniantz S, Rostne W. Chemokines and neuromodulation.
J Neuroimmunol. 2008;198(1):62-68.
6. Eskandari F, Webster JI, Sternberg EM. Neural immune pathways and their con-
nection to inflammatory diseases. Arthritis Res Ther. 2003;5(6):251-265.
7. Dartt DA, Kessler TL, Chung E-H, Zieske JD. Vasoactive intestinal peptide-
stimulated glycoconjugate secretion fromconjunctival goblet cells. Exp Eye Res.
1996;63(1):27-34.
8. Kovacs I, Ludany A, Koszegi T, et al. Substance P released from sensory nerve
endings influences tear secretion and goblet cell function in the rat. Neuropeptides.
2005;39(4):395-402.
9. The definition and classification of dry eye disease: report of the Definition and
Classification Subcommittee of the International Dry Eye WorkShop (2007). Ocul
Surf. 2007;5(2):75-92.
10. Lemp MA. Report of the National Eye Institute/Industry workshop on Clinical Trials
in Dry Eyes. CLAO J. 1995;21(4):221-232.
11. Dartt DA. Regulation of lacrimal gland secretion by neurotransmitters and the
EGF family of growth factors. Exp Eye Res. 2001;73(6):741-752.
12. Chung CW, Tigges M, Stone RA. Peptidergic innervation of the primate meibo-
mian gland. Invest Ophthalmol Vis Sci. 1996;37(1):238-245.
13. Springer J, Geppetti P, Fischer A, Groneberg DA. Calcitonin gene-related pep-
tide as inflammatory mediator. Pulm Pharmacol Ther. 2003;16(3):121-130.
14. OConnor TM, OConnell J, OBrien DI, Goode T, Bredin CP, Shanahan F. The role
of substance P in inflammatory disease. J Cell Physiol. 2004;201(2):167-180.
15. Hosoi J, Murphy GF, Egan CL, et al. Regulation of Langerhans cell function by
nerves containing calcitonin gene-related peptide. Nature. 1993;363(6425):
159-163.
16. Pozo D, Gonzalez-Rey E, Chorny A, Anderson P, Varela N, Delgado M. Tuning
immune tolerance with vasoactive intestinal peptide: a new therapeutic ap-
proach for immune disorders. Peptides. 2007;28(9):1833-1846.
17. Wheway J, Mackay CR, Newton RA, et al. A fundamental bimodal role for neu-
ropeptide Y1 receptor in the immune system. J Exp Med. 2005;202(11):1527-
1538.
18. Groneberg DA, Folkerts G, Peiser C, Chung KF, Fischer A. Neuropeptide Y (NPY).
Pulm Pharmacol Ther. 2004;17(4):173-180.
19. Bedoui S, Miyake S, Lin Y, et al. Neuropeptide Y (NPY) suppresses experimental
autoimmune encephalomyelitis: NPY
1
receptor-specific inhibition of autoreac-
tive Th1 responses in vivo. J Immunol. 2003;171(7):3451-3458.
20. Kodali S, Ding W, Huang J, Seiffert K, Wagner JA, Granstein RD. Vasoactive in-
testinal peptide modulates Langerhans cell immune function. J Immunol. 2004;
173(10):6082-6088.
21. Batbayar B, Nagy G, Kovesi G, Zelles T, Feher E. Morphological basis of sensory
neuropathy and neuroimmunomodulation in minor salivary glands of patients
with Sjogrens syndrome. Arch Oral Biol. 2004;49(7):529-538.
22. EkstromJ, Ekman R, Ha kanson R, Sjogren S, Sundler F. Calcitonin gene-related
peptide in rat salivary glands: neuronal localization, depletion upon nerve stimu-
lation, and effects on salivation in relation to substance P. Neuroscience. 1988;
26(3):933-949.
23. Lodde BM, Mineshiba F, Wang J, et al. Effect of human vasoactive intestinal pep-
tide gene transfer in a murine model of Sjogrens syndrome. Ann Rheum Dis.
2006;65(2):195-200.
24. Konttinen YT, Hukkanen M, Kemppinen P, et al. Peptide-containing nerves in la-
bial salivary glands in Sjogrens syndrome. Arthritis Rheum. 1992;35(7):815-
820.
25. Santavirta N, Konttinen YT, Tornwall J, et al. Neuropeptides of the autonomic
nervous system in Sjogrens syndrome. Ann Rheum Dis. 1997;56(12):737-
740.
26. Feher E, Zelles T, Nagy G. Immunocytochemical localisation of neuropep-
tide-containing nerve fibres in human labial glands. Arch Oral Biol. 1999;44
(suppl 1):S33-S37.
27. Lee HK, Lee KS, Kim HC, Lee SH, Kim EK. Nerve growth factor concentration
and implications in photorefractive keratectomy vs laser in situ keratomileusis.
Am J Ophthalmol. 2005;139(6):965-971.
28. Lambiase A, Micera A, Pellegrini G, et al. In vitro evidence of nerve growth fac-
tor effects on human conjunctival epithelial cell differentiation and mucin gene
expression. Invest Ophthalmol Vis Sci. 2009;50(10):4622-4630.
29. Methodologies to diagnose and monitor dry eye disease: report of the Diagnos-
tic Methodology Subcommittee of the International Dry Eye WorkShop (2007).
Ocul Surf. 2007;5(2):108-152.
30. Management andtherapy of dry eye disease: report of the Management andTherapy
Subcommittee of the International Dry Eye WorkShop (2007). Ocul Surf. 2007;
5(2):163-178.
31. Mantelli F, Tiberi E, Micera A, Lambiase A, Visintini F, Bonini S. MUC5AC over-
expression in tear film of neonates. Graefes Arch Clin Exp Ophthalmol. 2007;
245(9):1377-1381.
32. Lambiase A, Manni L, Bonini S, Rama P, Micera A, Aloe L. Nerve growth factor
promotes corneal healing: structural, biochemical, and molecular analyses of rat
and human corneas. Invest Ophthalmol Vis Sci. 2000;41(5):1063-1069.
33. Stern ME, Gao J, Siemasko KF, Beuerman RW, Pflugfelder SC. The role of the
lacrimal functional unit in the pathophysiology of dry eye. Exp Eye Res. 2004;
78(3):409-416.
34. Ben tez-del-Castillo JM, Acosta MC, Wassfi MA, et al. Relation between corneal
innervation with confocal microscopy and corneal sensitivity with noncontact es-
thesiometry in patients with dry eye. Invest Ophthalmol Vis Sci. 2007;48(1):
173-181.
35. Mantelli F, Argueso P. Functions of ocular surface mucins in health and disease.
Curr Opin Allergy Clin Immunol. 2008;8(5):477-483.
36. Nguyen DH, Beuerman RW, Thompson HW, DiLoreto DA. Growth factor and neu-
rotrophic factor mRNA in human lacrimal gland. Cornea. 1997;16(2):192-199.
ARCH OPHTHALMOL/ VOL 129 (NO. 8), AUG 2011 WWW.ARCHOPHTHALMOL.COM
986
2011 American Medical Association. All rights reserved.
Downloaded From: http://archopht.jamanetwork.com/ on 12/04/2013
Das könnte Ihnen auch gefallen
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- r145274208 Isabella Fonseca CUR145274208Dokument1 Seiter145274208 Isabella Fonseca CUR145274208Isabella FonsecaNoch keine Bewertungen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Surgical Management of Gastroesophageal Reflux in Adults - UpToDateDokument22 SeitenSurgical Management of Gastroesophageal Reflux in Adults - UpToDateJuan InsignaresNoch keine Bewertungen
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- 2020 Anaphylaxis JACI 2020Dokument42 Seiten2020 Anaphylaxis JACI 2020Peter Albeiro Falla CortesNoch keine Bewertungen
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Pedia Nursing Resource Unit - FinalDokument69 SeitenPedia Nursing Resource Unit - FinalDaryl Adrian RecaidoNoch keine Bewertungen
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- SupradynDokument5 SeitenSupradynashrayagrawalNoch keine Bewertungen
- Classification of Tongue Cancer Resection and Treatment AlgorithmDokument8 SeitenClassification of Tongue Cancer Resection and Treatment AlgorithmRahma WatiNoch keine Bewertungen
- Jamaophthalmology Biswas 2016 Oi 160055Dokument8 SeitenJamaophthalmology Biswas 2016 Oi 160055Ghalia HayetNoch keine Bewertungen
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- KSPCB BIOMEDICAL POSTER 1aDokument1 SeiteKSPCB BIOMEDICAL POSTER 1armulmadgiNoch keine Bewertungen
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Anesthesia-Assessing Depth PDFDokument1 SeiteAnesthesia-Assessing Depth PDFAvinash Technical ServiceNoch keine Bewertungen
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Manual of Bone Densitometry Measurements - An Aid To The Interpretation of Bone Densitometry Measurements in A Clinical Setting PDFDokument229 SeitenManual of Bone Densitometry Measurements - An Aid To The Interpretation of Bone Densitometry Measurements in A Clinical Setting PDFsesjrsNoch keine Bewertungen
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Case Study On Acute PyelonephritisDokument85 SeitenCase Study On Acute Pyelonephritissanutulsi100% (23)
- Preeclampsia Nursing Care PlanDokument5 SeitenPreeclampsia Nursing Care PlanBSN 3-2 RUIZ, Jewel Anne F.Noch keine Bewertungen
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Basic Surgical Skills FinalDokument62 SeitenBasic Surgical Skills Finalamel015Noch keine Bewertungen
- 1.0 Thrombocytes SCDokument10 Seiten1.0 Thrombocytes SC西矢椛Noch keine Bewertungen
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- XXXXXX 121Dokument11 SeitenXXXXXX 121AndriantkNoch keine Bewertungen
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- Bacteria Found in UrineDokument7 SeitenBacteria Found in UrineAria DomingoNoch keine Bewertungen
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- TORCHDokument32 SeitenTORCHJafar NoryNoch keine Bewertungen
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- TramadolDokument2 SeitenTramadolJordanne EtisNoch keine Bewertungen
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- PediatricsDokument312 SeitenPediatricsمحمد ابو مناضل الافينش100% (1)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Obstetrics Midterms Rationale 2nd Sem 2018 2019Dokument21 SeitenObstetrics Midterms Rationale 2nd Sem 2018 2019Gene Paulo UyNoch keine Bewertungen
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Apolinario Mabini Syphilis Rumors and Late 19th Century Philippine Power PlayDokument15 SeitenThe Apolinario Mabini Syphilis Rumors and Late 19th Century Philippine Power PlayHaneul KImNoch keine Bewertungen
- Massage Techniques and Effects PresentationDokument35 SeitenMassage Techniques and Effects Presentationama00Noch keine Bewertungen
- Pe 11 Quarter 3 Lesson 1Dokument17 SeitenPe 11 Quarter 3 Lesson 1Donah Kate AlbaNoch keine Bewertungen
- Icru 89 (229-260)Dokument32 SeitenIcru 89 (229-260)Christian Ordoñez100% (1)
- E341 FullDokument7 SeitenE341 FullwaribisalaNoch keine Bewertungen
- Celiac DiseaseDokument35 SeitenCeliac DiseaseRye HanaNoch keine Bewertungen
- Radiotherapy in Prostate Cancer Innovative Techniques and Current ControversiesDokument288 SeitenRadiotherapy in Prostate Cancer Innovative Techniques and Current ControversiesStirNoch keine Bewertungen
- Pathophysiology of InflammationDokument50 SeitenPathophysiology of InflammationElla Jones0% (1)
- HOPE 1 Quarter 1 Module 1 New S.Y 2021 22Dokument30 SeitenHOPE 1 Quarter 1 Module 1 New S.Y 2021 22Sarah Samon100% (1)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)