Beruflich Dokumente
Kultur Dokumente
Radiation Doses of Indirect and Direct Digital Cephalometric Radiography
Hochgeladen von
Marilyn Gonzales0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
28 Ansichten4 SeitenA pilot study was carried out to compare diagnostic image quality of indirect and direct digital cephalometric imaging. Organ doses were higher for direct digital imaging, except for the thyroid gland, where the organ doses are comparable.
Originalbeschreibung:
Originaltitel
4811532 A
Copyright
© © All Rights Reserved
Verfügbare Formate
PDF, TXT oder online auf Scribd lesen
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenA pilot study was carried out to compare diagnostic image quality of indirect and direct digital cephalometric imaging. Organ doses were higher for direct digital imaging, except for the thyroid gland, where the organ doses are comparable.
Copyright:
© All Rights Reserved
Verfügbare Formate
Als PDF, TXT herunterladen oder online auf Scribd lesen
0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
28 Ansichten4 SeitenRadiation Doses of Indirect and Direct Digital Cephalometric Radiography
Hochgeladen von
Marilyn GonzalesA pilot study was carried out to compare diagnostic image quality of indirect and direct digital cephalometric imaging. Organ doses were higher for direct digital imaging, except for the thyroid gland, where the organ doses are comparable.
Copyright:
© All Rights Reserved
Verfügbare Formate
Als PDF, TXT herunterladen oder online auf Scribd lesen
Sie sind auf Seite 1von 4
BRITISH DENTAL JOURNAL VOLUME 197 NO.
3 AUGUST 14 2004 149
Radiation doses of indirect and direct digital
cephalometric radiography
F. Gijbels,
1
G. Sanderink,
2
J. Wyatt,
3
J. Van Dam,
4
B. Nowak
5
and R. Jacobs
6
Aim The aim of this study was to measure organ doses and calculate
the effective dose for indirect and direct digital cephalometric
exposures.
Material and methods Indirect digital cephalometric exposures were
made of a Rando phantom head using a Cranex Tome multipurpose
unit with storage phosphor plates from Agfa and the direct digital (Charge
Coupled Device, CCD) exposures were made with a Proline Ceph CM unit.
Exposure settings were 70 kV and 4 mAs for indirect digital exposures.
Direct digital exposures were made with 70 kV, 10 mA and a total scanning
time of 23 s. TLD700 dosemeters were used to measure organ doses, and
the effective doses were calculated with (effective dose
sal
) and without
inclusion of the salivary glands. A pilot study was carried out to compare
diagnostic image quality of both imaging modalities.
Results Effective doses were 1.7 Sv for direct digital and 1.6 Sv for
indirect digital cephalometric imaging. When salivary glands were
included in the calculation, effective doses
sal
were 3.4 Sv and 2.2 Sv
respectively. Organ doses were higher for direct digital imaging, except
for the thyroid gland, where the organ doses were comparable.
Diagnostic image quality of indirect and direct digital cephalometric
images seemed comparable.
Conclusion Effective dose and effective dose
sal
were higher for direct
digital cephalometric exposure compared with indirect digital exposure.
Organ doses were higher for direct digital cephalography. From
preliminary data, it may be presumed that diagnostic image quality of
indirect and direct digital cephalometric images are comparable.
INTRODUCTION
Digital equipment for radiographic exposures was introduced to
dentistry in the late 1980s (RadioVisioGraphy, Trophy, Vin-
1
Postdoctoral Researcher,
3
Research Assistant in Paediatric Dentistry,
6*
Associate Professor,
Oral Imaging Centre, School of Dentistry, Oral Pathology and Maxillofacial Surgery,
Katholieke Universiteit Leuven, Belgium;
2
Associate Professor, Department of Oral
Radiology, Academic Centre for Dentistry, Amsterdam, The Netherlands;
4
Professor,
5
Postdoctoral Researcher, Department of Radiotherapy, Katholieke Universiteit Leuven,
Belgium.
*Correspondence to: Reinhilde Jacobs, Oral Imaging Centre, School of Dentistry, Oral
Pathology and Maxillofacial Surgery, Katholieke Universiteit Leuven, Kapucijnenvoer 7,
B-3000 Leuven, Belgium
E-mail: Reinhilde.Jacobs@uz.kuleuven.ac.be
Refereed Paper
doi:10.1038/sj.bdj.4811532
Received 27.01.03; Accepted 23.10.03
British Dental Journal 2004; 197: 149152
cennes, France). The first systems were based on the charge-
coupled device technology (CCD), which can also be found in cam-
era systems. With this technique, radiation is detected by the sen-
sor and converted into digital data, which are sent immediately to
a computer. The radiographic image is almost real time shown on
a computer monitor and is therefore also called direct digital radi-
ography. In the early 1990s, digital storage phosphor systems took
over from medical radiology. Storage phosphor plates (SPP) cap-
ture radiation energy for a certain period and can be read out by a
laser scanner, which converts radiation energy into light energy
that is measured and translated into digital data. Because of the
delay caused by the scanning procedure, the digital storage phos-
phor technique is also called indirect digital radiography.
A technical limitation of extra-oral direct digital radiography is
the very small active area of the CCD sensor. This is a minor prob-
lem for intra-oral digital radiography, where the active area of the
sensor remains somewhat smaller than a conventional intra-oral
film. For static extraoral radiography, such as anteroposterior and
cephalometric projections however, a linear scanning procedure is
usually applied to cover the whole area. This lengthens the expo-
sure time considerably.
Among other advantages, such as the possibility to digitally
manipulate the radiographic data, digital radiography can possibly
reduce radiation dose compared with conventional radiography.
Digital sensors (both direct and indirect) should be more sensitive
for radiation energy, which allows a lowering of radiation dose.
This is especially true for intra-oral radiography, where a signifi-
cant reduction of radiation dose has been reported.
15
For extrao-
ral digital radiography however, a smaller reduction can be
expected because of the already low dose thanks to the use of
intensifying screens and fast film-screen combinations in conven-
tional radiography. For digital panoramic radiography, different
amounts of dose reduction have been reported.
68
In a previous
report
9
, comparing conventional and indirect digital cephalomet-
ric radiography, it was found that image quality of digital and con-
ventional radiographs was not significantly different. However,
image quality of indirect digital radiographs was more stable for
variations in exposure parameters than conventional radiographs.
Because of the different exposure technique (linear scanning pro-
cedure) used in direct digital cephalometric radiography, a direct
comparison or interpolation of radiation doses is impossible. The
current study, therefore, was designed to measure organ doses for
This article aims to guide readers in taking the correct purchase/use decision of digital
radiographic equipment, based on scientific evidence, by achieving a proper balance
between diagnostic quality and radiation dose.
There is a lower radiation dose to the salivary gland when indirect digital rather than
direct cephalometric radiography is carried out.
Their image quality is comparable for both direct and indirect digital cephalometric
radiography.
I N BRI E F
RESEARCH
03p149-152.qxd 08/07/2004 13:52 Page 149
RESEARCH
150 BRITISH DENTAL JOURNAL VOLUME 197 NO. 3 AUGUST 14 2004
both direct and indirect digital exposure techniques for cephalo-
metric exposures. A pilot study was also performed to compare the
diagnostic image quality of the two digital imaging techniques.
MATERIAL AND METHODS
Exposures were made with storage phosphor plates (24 cm 30
cm, ADCC MD plate Agfa, Mortsel, Belgium) using the cephalo-
metric programme of the Cranex Tome multipurpose radiation
unit (Soredex, Helsinki, Finland). Exposure settings were 70 kV
and 4 mAs, considered as being the settings used for an average
person in daily practice. A custom-made lead collimator was
placed in front of the radiation tube to limit the exposure area
(Fig. 1). The lead collimator was constructed from a 3 mm thick
piece of lead and attached to the radiation unit in front of the radi-
ation source. In a previous study,
10
it was found that this collima-
tor could reduce the field size by 55% and the effective radiation
dose by almost 50%. The direct digital exposures were made with
the Proline Ceph CM unit (Planmeca, Helsinki, Finland) which has
a cephalometric exposure area of 18 cm 24 cm. The same lead
collimator was applied, taking care to collimate down to the same
region of the skull with both cephalometric units. Exposure set-
tings were 70 kV and 10 mA. The total exposure time for the linear
scanning procedure was 23 s. These are also the settings used for
an average person in daily practice.
A Rando phantom head (Alderson Research Laboratories, NY,
USA) (Fig. 2) representing an average man was exposed. The
Rando phantom head consisted of a human skull and vertebrae
surrounded and filled with tissue-equivalent material. It is a gener-
ally accepted method to measure absorbed radiation doses in dif-
ferent organs of the human body.
1117
The skull is cut into hori-
zontal slices and every slice contains holes that can be filled with
dosemeters. In the present study, dosemeters were put in the sub-
mandibular glands, parotid glands, bone marrow of the ascending
ramus, pituitary gland, corpus callosum, frontal brain lobe, cere-
bellum, thyroid gland, lenses of the eyes and skin. Two dosemeters
were used for each site and each exposure was repeated ten times.
The dosemeters were of the LiF:Mg,Ti TLD-700 type (Bicron NE,
Solon, USA) (containing only Li-7, without Li-6). They consisted of
ribbons of 3 3 0.15 mm
3
and have a standard deviation of 10%
(variability of the resulting doses after manipulation and reading
out procedures). They were read out with a fully-automated Har-
shaw 6600 reader (Bicron NE, Solon, USA) after correction for
atmospheric pressure, temperature and air humidity. The resulting
data were divided by 10 and averaged for the two dosemeters per
site. A number of dosemeters (five per session) underwent the same
procedure, except for the irradiation, to record the background
radiation (around 30 to 40 Gy). These values were subtracted
from the recorded data.
The data of the radiation doses absorbed by different organs
were then used for calculation of the effective radiation dose,
which is an indication of the impact of a certain radiation
exposure on the whole human body. The formula takes the vari-
ation in sensitivity towards radiation of the different organs
into account. Whereas absorbed radiation doses are expressed
in ()Gy, effective dose is expressed in ()Sv. The effective dose
was calculated using the formula: D
eff
= D
abs
.WF with D
eff
being the effective dose, D
abs
the absorbed organ doses and WF
the weighting factors as determined by ICRP60.
18
The effective
dose was calculated both with (effective dose
sal
) and without
(effective dose) inclusion of the salivary glands as part of the
remainder organs.
19
Following the ICRP regulations, salivary
glands are not considered as organs sensitive for the detrimen-
tal effects of radiation. A number of studies,
2023
however,
indicate a possible relationship between ionising radiation and
salivary gland cancers. A weighting factor of 0.05 was assigned
to the average of the remainder organs (pituitary gland, cere-
bellum, frontal brain lobe, corpus callosum and salivary
glands).
Because skin dose and bone marrow dose were only measured
locally, a formula described by Huda and Sandison
24
was used to
calculate the whole body skin and bone marrow doses. The bone
marrow dose was also used for the bone surface dose. For those
organs not measured in the present study, the absorbed dose was
assumed to be zero.
Fig. 1 The lead collimator limits the exposed area of the cephalometric
radiographs by 55%, which leads to a reduction in effective dose of 47% and
a reduction in effective dose
sal
of 41%.
10
Fig. 2 The Rando phantom head consists of a human skull surrounded and
filled with tissue equivalent material. The slices allow positioning of
dosemeters in pre-cut holes
03p149-152.qxd 08/07/2004 13:52 Page 150
RESEARCH
BRITISH DENTAL JOURNAL VOLUME 197 NO. 3 AUGUST 14 2004 151
When absorbed organ doses were considered, an overall
higher organ dose was found for direct digital cephalometry,
except for the dose to the thyroid gland, which was comparable.
For other organs, absorbed doses of up to 19 times higher (eye
lens tube side) could be found for direct digital imaging. This
has, however, not a large effect on the effective dose because the
doses to the lenses of the eyes are not included in the calculation
(deterministic effect, with threshold dose of 2 Gy
25
). Further-
more, the skin and bone marrow dose contribute only minimally
to the effective dose due to the use of the correction factors.
24
Thus, the organs most involved in the calculation of the effec-
tive dose are the thyroid gland, the brain tissue and, for the
effective dose
sal
, the salivary glands. This explains also the large
effect of the inclusion of the salivary gland tissue on the effec-
tive dose.
The difference in absorbed organ doses between indirect and
direct digital cephalometric exposures can probably be explained
by the different nature of the exposure technique. For the direct
digital imaging technique, a linear scanning procedure is used,
whereas a short exposure shot is used for the indirect digital tech-
nique. The longer time required by the scanning procedure also
implies a risk of movement artefacts, especially for children.
As a more general remark, it should be mentioned that differ-
ences in radiation dose could be due to individual anatomical vari-
ations. However, as the same phantom set-up was used for both
digital imaging techniques, at least a relative comparison between
both methods can be made.
Furthermore, a custom-made lead collimator was used for
cephalometric exposures, which means that higher doses will be
achieved in clinical practice where this collimator is not used.
A study by Visser et al. in 2001
26
on dosimetric measurements
for direct digital and conventional cephalometric radiography,
yielded an effective dose for direct digital cephalometric exposure
of 1.1 Sv, which is comparable to our result. A Siemens
Orthophos DS Ceph unit (Sirona Dental, Bietigheim-Bissingen)
was used. The exposure settings were 73 kV, 15 mA and 15.8 s.
Additional collimation was not used.
A preliminary evaluation of the diagnostic image quality of
both digital imaging systems was performed in a pilot study by
assessing the visibility of six cephalometric landmarks (nasion,
orbitale, A-point, B-point, pogonion, gonion). These landmarks
were selected because they are relatively independent of the pos-
sible superimposition of anatomical structures.
27
For both imag-
ing techniques, relatively high scores were assigned to nasion,
orbitale, B-point, pogonion and gonion. The A-point was scored
lower for both techniques. Previous studies already showed that
diagnostic image quality of cephalometric radiographs is not so
much dependent on physical properties but rather on observer
performance and pattern recognition.
28,29
A study by Liu et al.
30
showed that collimation of cephalometric radiographs leads to
improved contrast and diagnostic image quality. It should also be
kept in mind that a phantom head was used to evaluate the image
quality, which is not subject to possible movement artefacts due
to the almost 60 times longer exposure time for direct digital
exposures.
CONCLUSION
In conclusion, higher organ doses are found for direct digital
cephalometric radiography, except for the thyroid gland. Depend-
ing on the inclusion of the salivary gland tissue in the calculation
of the effective dose, effective doses for direct digital cephalomet-
ric imaging are 9% (1.7 Sv compared with 1.6 Sv) or 56% higher
(effective dose
sal
3.4 Sv compared with 2.2 Sv) than for indirect
digital cephalometric exposures. Furthermore, from preliminary
data, it seems that diagnostic image quality of both digital imaging
techniques is comparable.
In order to compare the diagnostic image quality of the indirect
and direct digital cephalometric radiographs, a pilot study was
performed by four observers. The visibility of six different
cephalometric landmarks (nasion, orbitale, A point, B point, pogo-
nion and gonion) was scored on a 5-point scale (1 = minimal visi-
bility, 5 = maximal visibility) for the two digital techniques. In
both cases, the radiographs taken from the phantom head were
shown on a computer monitor (17-inch screen, 24-bit colour
depth, resolution of 1024 768 pixels, dimmed ambient light). The
observers were blinded for the type of panoramic radiographs
(direct or indirect digital) and the radiographs were shown in ran-
dom order. The ratings were repeated with a 14-day interval. The
data were statistically analysed using the Kruskal-Wallis ANOVA
(Statistica, Tulsa, OK, USA) with observer and panoramic unit as
independent variables and cephalometric landmark and time of
assessment as dependent variables.
RESULTS
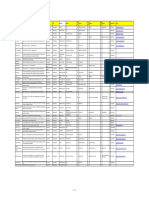
The results of the dose measurements and the resulting effective
dose are shown in Table 1. In the table, the results for ten repeated
exposures are divided by 10 after subtraction of the background
radiation (30 to 40 Gy). The effective doses are 1.6 Sv for indi-
rect digital cephalometric exposure and 1.7 for direct digital
cephalometric exposure. The corresponding effective doses
sal
are
2.2 Sv and 3.4 Sv respectively.
The diagnostic image quality of the two digital techniques were
comparable for the abovementioned cephalometric landmarks,
with good visibility (average score > 3) for nasion, orbitale,
B-point, pogonion and gonion, and poorer visibility (average score
of 2.81) for A-point. Inter- and intra-observer differences were
also not statistically significant.
DISCUSSION
The inclusion of the salivary gland tissue in the calculation of the
effective dose has a remarkable effect. Whereas the effective doses
of indirect and direct exposures are comparable (1.6 Sv vs 1.7 Sv
respectively, which is a difference of 9%) when the salivary tissue
is not included, the difference is larger when the salivary tissue is
included (2.2 Sv compared with 3.4 Sv, or 56%).
Table 1 Absorbed organ doses measured for indirect digital (SPP) and
direct digital (CCD) cephalometric exposures are expressed in Gy, the
effective dose is expressed in Sv
SPP CCD
Submandibular gland TS 45.4 112.2
Submandibular gland FS 14.0 52.8
Parotid gland TS 35.4 99.5
Parotid gland FS 6.3 9.5
Pituitary gland 3.2 39.5
Bone marrow TS 58.6 122.5
Bone marrow FS 8.7 18.7
Cerebellum 2.1 4.6
Frontal brain lobe 2.9 30.4
Corpus callosum 1.8 6.1
Eye lens TS 8.1 150.9
Eye lens FS 1.6 12.1
Skin TS 26.3 163.3
Skin FS 3.1 5.7
Thyroid gland 29.6 23.2
Effective dose (Sv) 1.6 1.7
Effective dose
sal
(Sv) 2.2 3.4
TS = tube side, FS = film side, effective dose
sal
= effective dose with salivary
glands as part of the remainder organs
03p149-152.qxd 08/07/2004 13:53 Page 151
RESEARCH
152 BRITISH DENTAL JOURNAL VOLUME 197 NO. 3 AUGUST 14 2004
Reinhilde Jacobs is a postdoctoral researcher of the Fund for Scientific Research
Flanders.
1. Brettle D S, Workman A, Ellwood R P, Launders J H, Horner K, Davies R M. The imaging
performance of a storage phosphor system for dental radiography. Br J Radiol 1996;
69: 256-261.
2. Lim K F, Loh E E-M, Hong Y H. Intra-oral computed radiography an in vitro
evaluation. J Dent 1996; 24: 359-364.
3. Velders X L, Sanderink G C H, van der Stelt P F. Dose reduction of two digital sensor
systems measuring file lengths. Oral Surg Oral Med Oral Pathol Oral Radiol Endod
1996; 81: 607-612.
4. Huysmans M C D, Hintze H, Wenzel A. Effect of exposure time on in vitro caries
diagnosis using the Digora system. Eur J Oral Sci 1997;105: 15-20.
5. Yoshiura K, Kawazu T, Chikui T, Tatsumi M, Tokumori K, Tanaka T, Kanda S. Assessment
of image quality in dental radiography, part 2: optimum exposure conditions for
detection of small mass changes in 6 intra-oral radiography systems. Oral Surg Oral
Med Oral Pathol Oral Radiol Endod 1999; 87: 123-129.
6. Dula K, Sanderink G, van der Stelt P F, Mini R, Buser D. Effects of dose reduction on the
detectability of standardized radiolucent lesions in digital panoramic radiography.
Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1998; 86: 227-233.
7. Farman T T, Farman A G, Kelly M S, Firriolo F J, Yancey J M, Stewart A V. Charge-
coupled device panoramic radiography: effect of beam energy on radiation exposure.
Dentomaxillofac Radiol 1998; 27: 36-40.
8. Dannewitz B, Hassfeld S, Eickholz P, Muhling J. Effect of dose reduction in digital dental
panoramic radiography on image quality. Dentomaxillofac Radiol 2002; 31: 50-55.
9. Gijbels F, Bou Serhal C, Willems G, Bosmans H, Sanderink G, Persoons M, Jacobs R.
Diagnostic yield of conventional and digital cephalometric images: a human cadaver
study. Dentomaxillofac Radiol 2001; 30: 101-105.
10. Gijbels F, Sanderink G, Wyatt J, Van Dam J, Nowak B, Jacobs R. Radiation doses of
collimated vs non-collimated cephalometric exposures. Dentomaxillofac Radiol 2003;
32: 128-133.
11. Wall B F, Fisher E S, Paynter R, Hudson A, Bird P D. Doses to patients from
pantomographic and conventional dental radiography. Br J Radiol 1979; 52:
727-734.
12. Velders X L, van Aken J, van der Stelt P F. Absorbed dose to organs in the head and
neck from bitewing radiography. Dentomaxillofac Radiol 1991; 20: 161-165.
13. Velders X L, van Aken J, van der Stelt P F. Risk assessment from bitewing radiography.
Dentomaxillofac Radiol 1991; 20: 209-213.
14. Gilda J E, Maillie H D. Dosimetry of absorbed radiation in radiographic cephalometry.
Oral Surg Oral Med Oral Pathol 1992; 73: 638-643.
15. Hayakawa Y, Fujimori H, Kuroyanagi K. Absorbed doses with intra-oral radiography.
Function of various technical parameters. Oral Surg Oral Med Oral Pathol 1993; 76:
519-524.
16. Farman T T, Farman A G, Kelly M S, Firriolo F J, Yancey J M, Stewart A V. Charge-
coupled device panoramic radiography; effect of beam energy on radiation exposure.
Dentomaxillofac Radiol 1998; 27: 36-40.
17. Bou Serhal C, Jacobs R, Gijbels F, Bosmans H, Hermans R, Quirynen M, van
Steenberghe D. Absorbed doses from spiral CT and conventional spiral tomography: a
phantom vs. cadaver study. Clin Oral Implants Res 2001; 12: 473-478.
18. International Commission on Radiological Protection. Recommendations of the
International Commission on Radiological Protection. ICRP Publication No. 60. Ann.
ICRP 1991; 21: 1-3.
19. Lecomber A R, Downes S L, Mokhtari M, Faulkner K. Optimisation of patient doses in
programmable dental panoramic radiography. Dentomaxillofac Radiol 2000; 29:
107-112.
20. Preston-Martin S, Henderson B E, Bernstein L. Medical and dental x rays as risk factors
for recently diagnosed tumors of the head. Natl Cancer Inst Monogr 1985; 69:
175-179.
21. Preston-Martin S, Thomas D C, White S C, Cohen D. Prior exposure to medical and
dental x-rays related to tumors of the parotid gland. J Natl Cancer Inst 1988; 80:
943-949.
22. Preston-Martin S, White S C. Brain and salivary gland tumors related to prior dental
radiography: implications for current practice. J Am Dent Assoc 1990; 120: 151-158.
23. Horn-Ross P L, Ljung B M, Morrow M. Environmental factors and the risk of salivary
gland cancer. Epidemiol 1997; 8: 414-419.
24. Huda W, Sandison G. Estimation of mean organ doses in diagnostic radiology from
Rando phantom measurements. Health Physics 1984; 47: 463-467.
25. ICRP Publication 41. Nonstochastic effects of ionizing radiation. Ann ICRP 1984; 14:
paragraph 3.
26. Visser H, Rdig T, Hermann K-P. Dose reduction by direct-digital cephalometric
radiography. Angle Orthod 2001; 71: 159-163.
27. Trpkova B, Major P, Prasad N, Nebbe B. Cephalometric landmarks identification and
reproducibility: A Meta Analysis. Am J Orthod Dentofac Orthoped 1997; 112:
165-170.
28. Nslund E-B, Kruger M, Petersson A, Hansen K. Analysis of low-dose digital lateral
cephalometric radiographs. Dentomaxillofac Radiol 1998; 27: 136-139.
29. Rossman K, Wiley B. The central problem in the study of radiographic image quality.
Radiol 1970; 96: 113-118.
30. Liu Y T, Gravely J F. The effect of beam collimation in lateral radiographic
cephalometry. Br J Orthod 1991; 18: 119-124.
In Volume 197, issue No. 12 of the BDJ (June 26, 2004), there was an error in
the first question on CPD Article 2.
Option C reads:
resin cements are more resistant to wear both in neutral and acidic conditions in
relation to other dental cement materials and always decrease the marginal gap
width.
Option C should have read:
resin cements are less resistant to wear both in neutral and acidic conditions in
relation to other dental cement materials and always decrease the marginal gap
width.
We apologise for any inconvenience this may have caused. For any further
queries please contact the Eastman at BDJ Eastman CPD, 123 Grays Inn Rd,
London, WC1X 8WD or e-mail support@bdjeastmancpd.com
CPD correction
03p149-152.qxd 08/07/2004 13:53 Page 152
Das könnte Ihnen auch gefallen
- Physical Assessment SampleDokument6 SeitenPhysical Assessment Samplecarlylove33% (3)
- Full Notes RadiographyDokument120 SeitenFull Notes RadiographyNishimwe Lambert100% (1)
- Radiation Doses of Indirect and Direct Digital CepDokument5 SeitenRadiation Doses of Indirect and Direct Digital CepdentureNoch keine Bewertungen
- BulganDokument10 SeitenBulganIkh nahia Ikh Nakhia PharmNoch keine Bewertungen
- Chan 2015Dokument10 SeitenChan 2015Innes AndrianiNoch keine Bewertungen
- Electron Beam Total Skin Irradiation PDFDokument1 SeiteElectron Beam Total Skin Irradiation PDFVictorM.LópezGuadalupeNoch keine Bewertungen
- Danne WitzDokument6 SeitenDanne WitzKhairniNoch keine Bewertungen
- Effect of CT Modality in Patient Doses and Image Quality in Pediatric CTDokument9 SeitenEffect of CT Modality in Patient Doses and Image Quality in Pediatric CTSoma SweetNoch keine Bewertungen
- Assesment of Entrance Skin Doses For Patients - Abdullah Medical CityDokument4 SeitenAssesment of Entrance Skin Doses For Patients - Abdullah Medical CityGeorgiana KokonaNoch keine Bewertungen
- Biij2007 Vol3 Issue2 Article6 JournalDokument14 SeitenBiij2007 Vol3 Issue2 Article6 JournalpritikachandNoch keine Bewertungen
- Sarti 2012Dokument12 SeitenSarti 2012mariaNoch keine Bewertungen
- Jurnal 2Dokument7 SeitenJurnal 2NOOR SYIFANoch keine Bewertungen
- Organ and Effective Dose Reduction in Adult Chest CT UsingDokument7 SeitenOrgan and Effective Dose Reduction in Adult Chest CT UsingIshani Anushika JayakodyNoch keine Bewertungen
- LawsonDokument7 SeitenLawsonrodolfo gorveñaNoch keine Bewertungen
- Laser Targeting With C-Arm FluorosDokument6 SeitenLaser Targeting With C-Arm Fluorosramankarnwal1971Noch keine Bewertungen
- Galileos CBCT Dosimetry ReportDokument12 SeitenGalileos CBCT Dosimetry ReportHả Nguyễn MỹNoch keine Bewertungen
- Image and Surgery-Related Costs Comparing Cone Beam CT and Panoramic Imaging Before Removal of Impacted Mandibular Third MolarsDokument7 SeitenImage and Surgery-Related Costs Comparing Cone Beam CT and Panoramic Imaging Before Removal of Impacted Mandibular Third MolarsSung Soon ChangNoch keine Bewertungen
- Literature Review of Uwb AntennaDokument7 SeitenLiterature Review of Uwb Antennac5ppm3e3100% (1)
- PR CBCT Minimum Dose For Maximum Safety ENDokument6 SeitenPR CBCT Minimum Dose For Maximum Safety ENSam Al AbabNoch keine Bewertungen
- A Paediatric X-Ray Exposure ChartDokument11 SeitenA Paediatric X-Ray Exposure Chartdddemourita9249Noch keine Bewertungen
- A Paediatric X-Ray Exposure ChartDokument11 SeitenA Paediatric X-Ray Exposure ChartMarco Jimenez HerreraNoch keine Bewertungen
- Geijer2003 Article DigitalRadiographyOfScoliosisWDokument9 SeitenGeijer2003 Article DigitalRadiographyOfScoliosisWbrian mgabiNoch keine Bewertungen
- Evaluation of Image Quality Parameters of Representative Intraoral Radiographic SystemsDokument10 SeitenEvaluation of Image Quality Parameters of Representative Intraoral Radiographic SystemsAlina RogojanuNoch keine Bewertungen
- Al-Okshi Et Al 2016Dokument11 SeitenAl-Okshi Et Al 2016Ayman AlOkshiNoch keine Bewertungen
- Dosimetric Evaluation of Radiation Dose Rate Effect inDokument5 SeitenDosimetric Evaluation of Radiation Dose Rate Effect inAlanaNoch keine Bewertungen
- Radiation Dose Modulation Techniques MDCTDokument10 SeitenRadiation Dose Modulation Techniques MDCTFelipe Gustavo Tercero Vega AbantoNoch keine Bewertungen
- Artigo - Hand Exposure in Diagnostic Nuc MedDokument6 SeitenArtigo - Hand Exposure in Diagnostic Nuc MedsamuelNoch keine Bewertungen
- CancerDokument9 SeitenCancerMARIA JOSE RIVERA AVILANoch keine Bewertungen
- Te 1667 WebDokument3 SeitenTe 1667 WebeguleamrNoch keine Bewertungen
- Development and Validation of A Low Dose Simulation Algorithm For Computed TomographyDokument9 SeitenDevelopment and Validation of A Low Dose Simulation Algorithm For Computed TomographyBrankica MitrovicNoch keine Bewertungen
- State-Of-The-Art On Cone Beam CT Imaging For Preoperative Planning of Implant PlacementDokument7 SeitenState-Of-The-Art On Cone Beam CT Imaging For Preoperative Planning of Implant Placementanimeilove3Noch keine Bewertungen
- Ciocca Et Al. - 2019 - Design and Commissioning of The Nondedicated Scanning Proton Beamline For Ocular Treatment at The SynchrotronDokument12 SeitenCiocca Et Al. - 2019 - Design and Commissioning of The Nondedicated Scanning Proton Beamline For Ocular Treatment at The SynchrotronKanit TanthanawigraiNoch keine Bewertungen
- J Ejmp 2020 02 017Dokument2 SeitenJ Ejmp 2020 02 017Camilo SotomayorNoch keine Bewertungen
- Quality ControlDokument4 SeitenQuality ControlDefi AndriyaniNoch keine Bewertungen
- Impact of Focal Spot Size On Radiologic Image Quality - A Visual Grading AnalysisDokument10 SeitenImpact of Focal Spot Size On Radiologic Image Quality - A Visual Grading AnalysisNurulazirah SalihNoch keine Bewertungen
- Radiation Dose Reduction Techniques For Chest CT Principles and Clinical ResultsDokument11 SeitenRadiation Dose Reduction Techniques For Chest CT Principles and Clinical ResultsSantiago TapiaNoch keine Bewertungen
- UntitledDokument12 SeitenUntitledapi-239502672Noch keine Bewertungen
- 08 0508182 Bindu ALTAMDokument21 Seiten08 0508182 Bindu ALTAMPriyansha KauravNoch keine Bewertungen
- Monitoring Tumor Motion by Real Time 2D-3D Registration During RadiotherapyDokument7 SeitenMonitoring Tumor Motion by Real Time 2D-3D Registration During RadiotherapyAsaduz ZamanNoch keine Bewertungen
- Thesis On Ultrasound ImagingDokument7 SeitenThesis On Ultrasound Imagingafknkzkkb100% (1)
- Hoff 2017Dokument1 SeiteHoff 2017Saadia BenhaloucheNoch keine Bewertungen
- Measurement of Scattered and Transmitted Xrays From Intraoral An 2018Dokument13 SeitenMeasurement of Scattered and Transmitted Xrays From Intraoral An 2018MahiraNoch keine Bewertungen
- Dose Evaluation For Skin and Organ in HepatocellulDokument11 SeitenDose Evaluation For Skin and Organ in HepatocellulAnne MbrkNoch keine Bewertungen
- AbdoDokument6 SeitenAbdosaifulmangopo123Noch keine Bewertungen
- Berger 2007Dokument9 SeitenBerger 2007Benfredj KhalilNoch keine Bewertungen
- DMF 41 011 PDFDokument7 SeitenDMF 41 011 PDFDenis KimNoch keine Bewertungen
- A Comparison of 18 Different X-Ray Detectors Currently UsedDokument5 SeitenA Comparison of 18 Different X-Ray Detectors Currently UsedpnogrlNoch keine Bewertungen
- Towards Cost-Effective and Lightweight Surface Plasmon Resonance Biosensing For H5N1 Avian Influenza Virus Detection - Integration of Novel Near-Infrared Organic Photodetectors - ScienceDirectDokument7 SeitenTowards Cost-Effective and Lightweight Surface Plasmon Resonance Biosensing For H5N1 Avian Influenza Virus Detection - Integration of Novel Near-Infrared Organic Photodetectors - ScienceDirectAna JuliaNoch keine Bewertungen
- 11 - Radiographic Parameters Biological Significance and Clinical Use - Periodontology 2000 - 2005 - BR Gger PDFDokument18 Seiten11 - Radiographic Parameters Biological Significance and Clinical Use - Periodontology 2000 - 2005 - BR Gger PDFm.castillo11Noch keine Bewertungen
- Image Processing and Visualization TopicsDokument16 SeitenImage Processing and Visualization TopicsBradda Derru Nesta MarleyNoch keine Bewertungen
- SPECT/CT Radiation DosimetryDokument13 SeitenSPECT/CT Radiation DosimetryMohamed Abd ElazizNoch keine Bewertungen
- What The General Dental Practitioner Should Know About Cone Beam Com-Puted Tomograph TechnologyDokument8 SeitenWhat The General Dental Practitioner Should Know About Cone Beam Com-Puted Tomograph TechnologydanmoviNoch keine Bewertungen
- Utilization Patterns of Multidetector Computed Tomography in Elective and Emergency Conditions: Indications, Exposure Risk, and Diagnostic GainDokument4 SeitenUtilization Patterns of Multidetector Computed Tomography in Elective and Emergency Conditions: Indications, Exposure Risk, and Diagnostic GainJorge RodriguezNoch keine Bewertungen
- The Unnecessary Dose Behind Cropped Radiographs: Radiography OpenDokument10 SeitenThe Unnecessary Dose Behind Cropped Radiographs: Radiography OpenVaishak JayaramNoch keine Bewertungen
- Marshall 2011Dokument22 SeitenMarshall 2011Ilham Bolqiah ZamerNoch keine Bewertungen
- The EOS 2D/3D X-Ray Imaging System: A Cost-Effectiveness Analysis Quantifying The Health Benefits From Reduced Radiation ExposureDokument27 SeitenThe EOS 2D/3D X-Ray Imaging System: A Cost-Effectiveness Analysis Quantifying The Health Benefits From Reduced Radiation Exposure979104025Noch keine Bewertungen
- CT Diagnostic Reference Levels: Are They Appropriately Computed?Dokument8 SeitenCT Diagnostic Reference Levels: Are They Appropriately Computed?EDISON FLOREZNoch keine Bewertungen
- Accuracy of Digital and Analogue Cephalometric Measurements Assessed With The Sandwich TechniqueDokument7 SeitenAccuracy of Digital and Analogue Cephalometric Measurements Assessed With The Sandwich TechniqueNurulArifahNoch keine Bewertungen
- Elgström - Sandborg - 2021 - Fluoro SNR - RPDDokument20 SeitenElgström - Sandborg - 2021 - Fluoro SNR - RPDmartuflashNoch keine Bewertungen
- Patient Shielding During Dentomaxillofacial RadiographyDokument12 SeitenPatient Shielding During Dentomaxillofacial RadiographyAainaa KhairuddinNoch keine Bewertungen
- Textbook of Urgent Care Management: Chapter 35, Urgent Care Imaging and InterpretationVon EverandTextbook of Urgent Care Management: Chapter 35, Urgent Care Imaging and InterpretationNoch keine Bewertungen
- FDI Dental Ethics ManualDokument136 SeitenFDI Dental Ethics Manualdocx1975100% (2)
- Journal of Endodontics 2013 Ball - Henrik - Skjerven - 11!06!2013Dokument10 SeitenJournal of Endodontics 2013 Ball - Henrik - Skjerven - 11!06!2013Marilyn GonzalesNoch keine Bewertungen
- Measles and Rubella: Learning A Lesson The Hard WayDokument2 SeitenMeasles and Rubella: Learning A Lesson The Hard WayMarilyn GonzalesNoch keine Bewertungen
- Measles (Rubeola) : Communicable Disease Management ProtocolDokument9 SeitenMeasles (Rubeola) : Communicable Disease Management ProtocolMarilyn GonzalesNoch keine Bewertungen
- Chakra Dancing Teacher Prospectus 2011 PDFDokument3 SeitenChakra Dancing Teacher Prospectus 2011 PDFGavin ElderNoch keine Bewertungen
- DSWD Guidelines For Residential FacilitiesDokument12 SeitenDSWD Guidelines For Residential FacilitiesCharlene Ordoñez Dela CruzNoch keine Bewertungen
- CertificateDokument1 SeiteCertificateSanskruti RautNoch keine Bewertungen
- Pest Control Risk Assessment Indoor and OutdoorDokument72 SeitenPest Control Risk Assessment Indoor and OutdoorarmkarthickNoch keine Bewertungen
- ECAM2015 324369 PDFDokument6 SeitenECAM2015 324369 PDFLuiz Otavio CostaNoch keine Bewertungen
- VP Hospital Nursing Executive in Atlanta GA Resume Margaret SterbenzDokument5 SeitenVP Hospital Nursing Executive in Atlanta GA Resume Margaret SterbenzMargaretSterbenzNoch keine Bewertungen
- Biocare GuidelinesDokument3 SeitenBiocare GuidelinesnsjunnarkarNoch keine Bewertungen
- York County Court Schedule For Aug. 20Dokument15 SeitenYork County Court Schedule For Aug. 20York Daily Record/Sunday NewsNoch keine Bewertungen
- Orthodontic Appliances: General Requirements of An Orthodontic ApplianceDokument20 SeitenOrthodontic Appliances: General Requirements of An Orthodontic ApplianceSafaa GhobNoch keine Bewertungen
- Name Clinic/Hosp/Med Name &address Area City Speciality SEWA01 Disc 01 SEWA02 DIS C02 SEWA03 Disc 03 SEWA04 DIS C04 Contact No. EmailDokument8 SeitenName Clinic/Hosp/Med Name &address Area City Speciality SEWA01 Disc 01 SEWA02 DIS C02 SEWA03 Disc 03 SEWA04 DIS C04 Contact No. EmailshrutiNoch keine Bewertungen
- Worksheet For Nervous Systems-KeyDokument5 SeitenWorksheet For Nervous Systems-KeyNazarine Torres100% (2)
- Surgery Shelf TopicsDokument2 SeitenSurgery Shelf TopicsSaulNoch keine Bewertungen
- Read The Text and Answer Questions 5 and 6.: Cookbook. New York: DK Publishing, 2007, P. 8Dokument1 SeiteRead The Text and Answer Questions 5 and 6.: Cookbook. New York: DK Publishing, 2007, P. 8matheus gonçalvesNoch keine Bewertungen
- Computer Addiction Power Point PresentationDokument24 SeitenComputer Addiction Power Point PresentationGee A50% (4)
- Myocardial InfarctionDokument4 SeitenMyocardial InfarctionLetecia MooreNoch keine Bewertungen
- Malaria Lesson Plan 1Dokument3 SeitenMalaria Lesson Plan 1Jayshree ParmarNoch keine Bewertungen
- Detailed Job Description - RaqsDokument3 SeitenDetailed Job Description - RaqsBarga John0% (1)
- A) Long-Term Follow-Up of Patients With Migrainous Infarction - Accepted and Final Publication From Elsevier1-s2.0-S030384671730344X-mainDokument3 SeitenA) Long-Term Follow-Up of Patients With Migrainous Infarction - Accepted and Final Publication From Elsevier1-s2.0-S030384671730344X-mainRodrigo Uribe PachecoNoch keine Bewertungen
- Sepsis en El Embarazo y PuerperioDokument9 SeitenSepsis en El Embarazo y PuerperioJoseTeodomiroQuispeRicciNoch keine Bewertungen
- Child Health ProgramDokument10 SeitenChild Health ProgramDrAshiq ANoch keine Bewertungen
- Olympus BF Channels-DesinfDokument1 SeiteOlympus BF Channels-DesinfEduardo ArreguinNoch keine Bewertungen
- NDOC-DOJ ComplianceDokument7 SeitenNDOC-DOJ ComplianceUnited Press InternationalNoch keine Bewertungen
- Osnove FarmakokinetikeDokument46 SeitenOsnove Farmakokinetikeapi-3814389Noch keine Bewertungen
- Mendiguchia 2012 Rectus Femoris Muscle Injuries in Football-A Clinically Relevant Review of Mechanisms of Injury, Risk Factors and Preventive Strategies PDFDokument11 SeitenMendiguchia 2012 Rectus Femoris Muscle Injuries in Football-A Clinically Relevant Review of Mechanisms of Injury, Risk Factors and Preventive Strategies PDFJuan PalomoNoch keine Bewertungen
- Author(s) : John Levine License:Unless Otherwise Noted, This Material Is Made Available Under The TermsDokument50 SeitenAuthor(s) : John Levine License:Unless Otherwise Noted, This Material Is Made Available Under The TermsMahda AzimahNoch keine Bewertungen
- Arya Maheswara - Stroke InfarkDokument17 SeitenArya Maheswara - Stroke InfarkdianarahimmNoch keine Bewertungen
- Movie ReviewDokument5 SeitenMovie ReviewVangeline MandiitNoch keine Bewertungen
- Note Regarding Retiring DoctorsDokument3 SeitenNote Regarding Retiring DoctorsnamankumaragrawalNoch keine Bewertungen
- Daftar Pustaka OaDokument2 SeitenDaftar Pustaka OaCut Naja SoviaNoch keine Bewertungen