Beruflich Dokumente
Kultur Dokumente
How To Strike Down Tuberculosis
Hochgeladen von
kyawswarpmOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
How To Strike Down Tuberculosis
Hochgeladen von
kyawswarpmCopyright:
Verfügbare Formate
H
o
w
t
o
p
in
d
o
w
n
T
u
b
e
r
c
u
lo
s
is
in
t
h
e
w
o
r
k
p
la
c
e
2
New cases of Tuberculosis or
TB are still being reported in Singapore.
Although the spread of TB is within
control, the community needs to be
aware of how TB is spread, what to do
and where to seek medical treatment
if they are infected.
TB is caused by bacteria that usually
attack the lungs. It can also
affect other parts of the body
such as the kidneys, spine
and brain. If not treated
properly, TB can be fatal.
Fortunately, TB can be cured as long
as it is promptly diagnosed and
treated. You are in a great position
to help your workforce should any
of them develop the disease.
This book can help you understand
how TB can be best managed in
the workplace. Read on to find
out exactly how to protect your
workforce and manage TB to
minimise disruptions to the
workflow and productivity of
your company.
3
W
h
a
t
i
s
T
B
a
n
d
h
o
w
d
o
e
s
i
t
s
p
r
e
a
d
?
P
r
o
t
e
c
t
i
n
g
y
o
u
r
s
t
a
f
f
f
r
o
m
T
B
t
r
a
n
s
m
i
s
s
i
o
n
M
anaging TB
in
the w
orkplace
T
r
e
a
t
i
n
g
a
n
d
c
u
r
i
n
g
T
B
4
TB is a disease caused by
bacteria called Mycobacterium
tuberculosis. It usually affects the
lungs (pulmonary tuberculosis),
but can also infect other parts
of the body (extrapulmonary
tuberculosis), such as the brain,
lymph nodes, kidneys, bones
and joints.
The general symptoms of TB
include feelings of sickness or
weakness, weight loss, fever,
and night sweats. The symptoms
of TB in the lungs also include an
ongoing cough, chest pain, and
coughing up blood.
Symptoms of TB in other parts
of the body depend on the
area affected.
What is TB and how
does it spread?
5
TB is an airborne infection. When someone with TB
coughs or sneezes, TB bacteria are released into the air
and can stay there for several hours. People nearby may
breathe in these bacteria and become infected.
In this way, an untreated person will pass TB on to
10 15 people each year. On average, one in 10 of those
people will develop active, contagious TB, while the
rest will not have any symptoms or be able to pass the
disease onto others.
TB transmission
Risk of getting TB
Active TB develops in about 10% of infected
people even if they have a healthy immune
system. However, if the persons immune system
is weakened, e.g. by other health conditions, the
chance of getting sick will be higher. Hence, the risk
of developing active TB is greater among:
Children, who have naturally weaker immune
systems
People in close contact with untreated infectious
TB cases
People with underlying medical conditions such
as HIV infection and diabetes
6
Transmission depends on
How many bacteria droplets
are in the air
How strong the type of bacteria is
The size of the room
The ventilation of the room
People with active TB are most
likely to spread the bacteria to
people they spend time with every
day, such as household and family
members, friends, co-workers
or schoolmates.
Factors that affect
transmission
7
In most parts of the world, especially
in developing countries, TB is a major
cause of death and disability. Untreated
TB can cause severe complications such
as bleeding in the lungs and respiratory
failure, and can be fatal.
However, with the right
and complete treatment
TB can be cured.
It is important to recognise the symptoms
of TB, as that is the first step towards
diagnosis and cure. The next chapter
outlines the early signs of disease, and the
appropriate measures to take.
Understanding
the risks
8
Protecting your staff
from TB transmission
Symptoms of TB
The single most effective way to
prevent TB transmission is to make
sure that the person with active TB is
diagnosed early and treated properly.
By knowing the signs and symptoms,
you can ensure that your workers get
the treatment and care they need.
Cough that lasts for more than 3 weeks
Weight loss
Fever
Night sweats
Loss of appetite
Coughing up blood
9
The most common symptom
of pulmonary TB (or TB that
affects the lungs) is an ongoing
cough for 3 weeks or more.
This is the key thing to remember anyone who has a
persistent cough may have TB in his or her lungs.
If someone on your workforce has had a cough for 3 or more
weeks, they should be referred to a medical practitioner
for assessment.
Someone who is diagnosed with TB will need to take medical
leave for the first 2 weeks of treatment, so arrangements will
need to be made to cover his or her duties.
After completion of the first 2 weeks of treatment, most
people are able to re-join the workforce, posing no risk of
transmission to others. However, they must continue treatment
for at least 6 months in order to be cured of the disease.
The best way to ensure that a TB patient is properly treated
and cured is for him or her to undergo supervised treatment
(Directly Observed Therapy or DOT, see page 13).
The most common
symptom of TB
Defending your workforce
10
A doctor who diagnoses a person
with TB is required by law to notify
the Ministry of Health (MOH) National TB
registry. The TB Control Unit (TBCU) then
follows a three-step procedure:
1. TBCU identifies people who may
have been put at risk anyone
who has had close and prolonged
contact with the person with
active TB.
2. These close contacts are given
a skin test* to find out whether they
have been infected. Results are
available 48 72 hrs after testing.
3. Preventive treatment may be offered to
those with a positive skin test.
People with a positive skin test but no
signs of active TB have dormant infection.
Contact tracing is carried out by the
TBCU free of charge for identified close
contacts of infectious TB patients under
the National TB Control Programme.
* Called a Mantoux test a safe TB extract is injected under
the skin and the skin reaction is measured.
If TB is diagnosed
11
If someone suspects that he or she
has been exposed to TB, there are a
few important things to remember:
You would have to breathe in TB
bacteria from someone with active
disease in order to become
infected yourself
The inhaled bacteria would have
to multiply in your body to cause
active TB
Exposure to TB
12
S M T
1
6 7 8
13 14 15
20 21 22
27 28 29
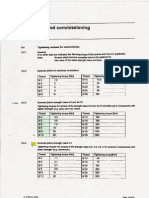
Once TB has been diagnosed it needs to be
treated so the patient can recover and the spread of
TB can be prevented or minimised. Most cases can be
treated on an outpatient basis. TB drugs are provided
free to patients treated under DOT (Directly-Observed
Treatment) by the TB Control Unit.
It is important that patients take the right combination of
drugs for the right length of time (6 9 months) in order
to make a full recovery. If the TB is not drug-resistant,
and the full course of treatment is taken, more than 95%
of all patients can be cured.*
*Source: www.moh.gov.sg
Treating and curing TB
It is vital that anyone with TB completes his or her full
course of medication. People often start to feel better
after the first few weeks of treatment, and may stop or
partially skip their treatment for the next few months.
Incomplete treatment is worse than no treatment at
all as the TB bacteria will grow resistant to the drugs
that are first used. When this happens, it becomes
necessary to use different drugs for a longer duration,
and it becomes more difficult to achieve a cure.
13
A full course of
medication is key
13
W T F S
2 3 4 5
9 10 11 12
16 17 18 19
23 24 25 26
30 31
16
DOT, or Directly Observed Treatment, involves taking
TB treatment under the supervision of a nurse or
other healthcare professional. This ensures that the
patient adheres to the treatment regimen, which
increases his or her chance of being cured.
Directly Observed
Treatment
Don't miss any treat ment doses.
14
The previous pages provide the information you need
to recognise the early signs of TB and support any
employee who becomes infected with the bacteria.
In addition, the following tips provide a guide to
offering the best response to TB within the workplace.
Managing TB in
the workplace
1. Recognise that TB is a workplace issue.
TB affects businesses as it increases labour costs and
reduces productivity you could help your company and your
employee by providing TB education.
2. Create awareness.
This booklet and accompanying materials can help you
educate your workforce about TB. Employees should
understand that anyone can be infected, but that treatment
is simple and effective. They should also know where to
seek more information, medical consultation and treatment.
3. Ensure non-discrimination.
No one should be discriminated against or penalised because
of his or her real or possible TB status. Fear of stigmatisation
makes people less likely to seek diagnosis, and therefore
makes it harder to stop the spread of this disease.
Employers should support TB patients by encouraging them
to adhere to and complete the treatment course, by allowing
them time to attend DOT where necessary.
15
4. Respect confidentiality.
Other members of your workforce do not need to know
about a co-workers TB status. Ensuring confidentially means
employees will place more trust in your managements
professionalism and your TB workplace health-promotion
programme, which will help it be more effective.
5. Facilitate maintenance of DOT.
Employees need to continue their DOT until they are
completely cured. Supervisors at work should exercise
empathy and concern for their employees and facilitate their
continuation of DOT at their nearest polyclinic.
For example, allow flexible working hours or time off to
receive DOT. Remember that in making these arrangements,
confidentiality on employees TB status should be maintained.
6. Develop a sustainable network of TB programme partners.
There are various healthcare organisations like SATA
CommHealth (Tel: 6244 6688; www.sata.com.sg) that can
provide long-term resources, support and information for
workplace TB programmes.
Copyright HPB B E 614-10
April 2010
For more information on TB,
please visit
www.hpb.gov.sg/infectiousdiseases
Health Promotion Board
3 Second Hospital Avenue, Singapore 168937
Das könnte Ihnen auch gefallen
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (120)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Laboratory Medicine Diagnosis of Disease in Clinical LaboratoryDokument513 SeitenLaboratory Medicine Diagnosis of Disease in Clinical Laboratorydahmer16100% (3)
- Clinician's Guide To ADHD Comorbidities in Children and Adolescents Case Studies 2019 PDFDokument148 SeitenClinician's Guide To ADHD Comorbidities in Children and Adolescents Case Studies 2019 PDFfadel bilondatu100% (3)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Pharmacotherapy DocToonPage PDFDokument307 SeitenPharmacotherapy DocToonPage PDFmukdad9Noch keine Bewertungen
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- Therapeutic Modalities Module 5Dokument4 SeitenTherapeutic Modalities Module 5johnpaulacosta100% (1)
- Baldor Motor Cowern Papers (PR2525)Dokument124 SeitenBaldor Motor Cowern Papers (PR2525)Jeff AyersmanNoch keine Bewertungen
- HV Switching ProcedureDokument6 SeitenHV Switching Procedurekyawswarpm100% (3)
- Evaluation of Reactances and Time Constants of Synchronous GeneratorDokument5 SeitenEvaluation of Reactances and Time Constants of Synchronous GeneratorInternational Journal of Research in Engineering and TechnologyNoch keine Bewertungen
- 1200 CFM or 2000 Cu - MTR Per HR Air Compressor (Datasheet)Dokument3 Seiten1200 CFM or 2000 Cu - MTR Per HR Air Compressor (Datasheet)kyawswarpmNoch keine Bewertungen
- Calc Drip Rates 2Dokument2 SeitenCalc Drip Rates 2Charisse Nicole DiazNoch keine Bewertungen
- Current Transformers Theory & SelectionDokument7 SeitenCurrent Transformers Theory & Selectionkyawswarpm100% (1)
- Assessing Dehydration in ChildrenDokument40 SeitenAssessing Dehydration in ChildrenDr. Jayesh PatidarNoch keine Bewertungen
- Short Circuit StudyDokument29 SeitenShort Circuit StudyPramod B.Wankhade100% (3)
- Solutions For Internal Arc Protection According To IEC 62271-200 in MV SwitchgearDokument5 SeitenSolutions For Internal Arc Protection According To IEC 62271-200 in MV Switchgearkyawswarpm100% (1)
- CP5 Amendment 1 27 Feb 2009 Fact SheetDokument4 SeitenCP5 Amendment 1 27 Feb 2009 Fact Sheetkyawswarpm100% (1)
- Battery Sizing CalculatorDokument6 SeitenBattery Sizing Calculatormfisol2000Noch keine Bewertungen
- The Controversy of Icu and IcsDokument2 SeitenThe Controversy of Icu and IcsUsama AhmedNoch keine Bewertungen
- Remotivation TherapyDokument2 SeitenRemotivation TherapyMelissa David100% (1)
- New International VersionDokument2 SeitenNew International VersionkyawswarpmNoch keine Bewertungen
- Population in Brief 2014Dokument26 SeitenPopulation in Brief 2014Hongwei GuanNoch keine Bewertungen
- Graduate Admissions: Service ObligationDokument3 SeitenGraduate Admissions: Service ObligationkyawswarpmNoch keine Bewertungen
- Att-4 LV Cable Epr Epr GSWB Shf-2Dokument7 SeitenAtt-4 LV Cable Epr Epr GSWB Shf-2kyawswarpmNoch keine Bewertungen
- 06 RadioactiveDokument4 Seiten06 RadioactiveWalid FattahNoch keine Bewertungen
- Electrical System Design EngineeringDokument3 SeitenElectrical System Design EngineeringsrsureshrajanNoch keine Bewertungen
- Report of 2013 From World Energy CouncilDokument48 SeitenReport of 2013 From World Energy CouncilkyawswarpmNoch keine Bewertungen
- Gamma Ray Level GaugeDokument1 SeiteGamma Ray Level GaugekyawswarpmNoch keine Bewertungen
- Advanced Diploma of E & IDokument33 SeitenAdvanced Diploma of E & IkyawswarpmNoch keine Bewertungen
- Topics From IELTS ReadingDokument22 SeitenTopics From IELTS ReadingkyawswarpmNoch keine Bewertungen
- 02 MSC (Power System and Energy Management, Singapore)Dokument8 Seiten02 MSC (Power System and Energy Management, Singapore)kyawswarpmNoch keine Bewertungen
- CEFR Levels DiagramDokument7 SeitenCEFR Levels DiagramkyawswarpmNoch keine Bewertungen
- Topics From IELTS ReadingDokument22 SeitenTopics From IELTS ReadingkyawswarpmNoch keine Bewertungen
- 2014 Global Peace Index REPORTDokument110 Seiten2014 Global Peace Index REPORTKashmir WatchNoch keine Bewertungen
- ITEE, UniSA 2014Dokument23 SeitenITEE, UniSA 2014kyawswarpmNoch keine Bewertungen
- The Universal Declaration of Human Rights in BurmeseDokument9 SeitenThe Universal Declaration of Human Rights in Burmesethanhtutaung100% (2)
- Christianity - VictoryDokument2 SeitenChristianity - VictorykyawswarpmNoch keine Bewertungen
- Torque Table (Electrical Connections)Dokument1 SeiteTorque Table (Electrical Connections)kyawswarpmNoch keine Bewertungen
- IELTS Writing Band Descriptors Task 1Dokument1 SeiteIELTS Writing Band Descriptors Task 1MasonAllisonNoch keine Bewertungen
- Torque Table (Electrical Connections)Dokument1 SeiteTorque Table (Electrical Connections)kyawswarpmNoch keine Bewertungen
- Lester Et Al Cognitive ErrorsDokument11 SeitenLester Et Al Cognitive ErrorsДоникаNoch keine Bewertungen
- Scabies-2017-The Journal of DermatologyDokument24 SeitenScabies-2017-The Journal of DermatologysirohNoch keine Bewertungen
- Adrenergic DrugsDokument2 SeitenAdrenergic DrugsSunshine_Bacla_4275Noch keine Bewertungen
- No Nama Obat Sediaan Dosis Indikasi Dewasa Anak: 2 Yr: 12 mg/kg/24Dokument6 SeitenNo Nama Obat Sediaan Dosis Indikasi Dewasa Anak: 2 Yr: 12 mg/kg/24JovitaNoch keine Bewertungen
- Ayurvedic & Unani Tibbia College, Delhi: National Institute of Unani MedicineDokument3 SeitenAyurvedic & Unani Tibbia College, Delhi: National Institute of Unani MedicineShashank JainNoch keine Bewertungen
- INVOICE 2-4 April 2023Dokument3 SeitenINVOICE 2-4 April 2023IwanAtassonggeNoch keine Bewertungen
- The Wick: The Magazine of Hartwick College - Summer 2011Dokument56 SeitenThe Wick: The Magazine of Hartwick College - Summer 2011Stephanie BrunettaNoch keine Bewertungen
- Kuliah 2 AccupunctureDokument40 SeitenKuliah 2 AccupunctureRizka PermanaNoch keine Bewertungen
- Julia H Bartlett ResumeDokument3 SeitenJulia H Bartlett Resumeapi-484975401Noch keine Bewertungen
- Positive End Expiratory PressureDokument5 SeitenPositive End Expiratory PressureIrving H Torres LopezNoch keine Bewertungen
- Panchakarma EXAM QUESTION PAPERDokument29 SeitenPanchakarma EXAM QUESTION PAPERNiramayam RmoNoch keine Bewertungen
- Aurobindo Pharma Receives USFDA Approval For Vancomycin Hydrochloride For Injection (Company Update)Dokument2 SeitenAurobindo Pharma Receives USFDA Approval For Vancomycin Hydrochloride For Injection (Company Update)Shyam SunderNoch keine Bewertungen
- Pulmonary Function TestDokument87 SeitenPulmonary Function TestRiry AmbarsaryNoch keine Bewertungen
- Aao Final Program2014 PDFDokument388 SeitenAao Final Program2014 PDFbrohussein1982100% (1)
- Pain Assessment and Management in Cancer Patients: Saint Louis University School of NursingDokument3 SeitenPain Assessment and Management in Cancer Patients: Saint Louis University School of NursingSoniaMarieBalanayNoch keine Bewertungen
- Resume - Mohammad AmaniDokument2 SeitenResume - Mohammad Amaniarian tejaratNoch keine Bewertungen
- Drug PepcidDokument2 SeitenDrug PepcidSrkocher0% (1)
- 1026 FullDokument5 Seiten1026 FullMuhammad Yufimar Rizza FadilahNoch keine Bewertungen
- Wolberg DefinitionDokument18 SeitenWolberg DefinitionSwati ThakurNoch keine Bewertungen
- Medicaid Waiver Guide 3-2013 - CDokument39 SeitenMedicaid Waiver Guide 3-2013 - CMelissa Simpson HouseNoch keine Bewertungen
- Red Flags of The Shoulder and NeckDokument5 SeitenRed Flags of The Shoulder and NecksugoimanNoch keine Bewertungen
- CRA 2010-Poster-PresentationsDokument236 SeitenCRA 2010-Poster-PresentationsJoe GassNoch keine Bewertungen
- Reflexology: Grinberg MethodDokument2 SeitenReflexology: Grinberg MethodHannah CheethamNoch keine Bewertungen