Beruflich Dokumente
Kultur Dokumente
Nrrheum 2010 118
Hochgeladen von
Siti Harwati DesrimelinaOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Nrrheum 2010 118
Hochgeladen von
Siti Harwati DesrimelinaCopyright:
Verfügbare Formate
NATURE REVIEWS | RHEUMATOLOGY VOLUME 6 | SEPTEMBER 2010 | 529
Department of
Pathophysiology,
Medical School,
National University of
Athens, 75 Mikras
Asias Street, 11527
Athens, Greece
(M. Voulgarelis,
A. G. Tzioufas).
Correspondence to:
M. Voulgarelis
mvoulgar@med.uoa.gr
Pathogenetic mechanisms in the initiation
and perpetuation of Sjgrens syndrome
Michael Voulgarelis and Athanasios G. Tzioufas
Abstract | Sjgrens syndrome (SS), a chronic autoimmune disorder, particularly compromises the function
of exocrine glands. The involvement of these glands is characterized by focal, mononuclear cell infiltrates
that surround the ducts and replace the secretory units. The pathogenetic mechanisms of this autoimmune
exocrinopathy have not been fully elucidated. Immunologically-activated or apoptotic glandular epithelial
cells that expose autoantigens in genetically predisposed individuals might drive autoimmune-mediated
tissue injury. Alterations in several immune mediators, such as upregulation of type I interferon-regulated
genes, abnormal expression of B-cell-activating factor and activation of the interleukin-23type 17 T-helper
cell pathway, have been reported. Extension of the pathological process that affects the exocrine glands into
periepithelial and extraepithelial tissue can cause a considerable percentage of patients to exhibit systemic
findings that involve the lungs, liver or kidneys. These manifestations develop as a result of lymphocytic
invasion or an immune-complex-mediated process, or both, and present as skin vasculitis coupled with
peripheral neuropathy or glomerulonephritis (or both). Patients with systemic extraepithelial manifestations
display low serum levels of the complement component C4 and mixed type II cryoglobulins, and show an
increased risk of developing non-Hodgkin lymphoma, thereby reflecting an overall worse prognosis with higher
mortality rates than those without extraepithelial manifestations.
Voulgarelis, M. & Tzioufas, A. G. Nat. Rev. Rheumatol. 6, 529537 (2010); published online 3 August 2010; doi:10.1038/nrrheum.2010.118
Introduction
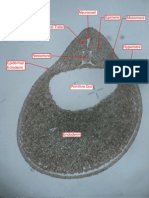
Sjgrens syndrome (SS) is a chronic inflammatory disease
that affects the exocrine glands, particularly the salivary
glands. Focal, mononuclear cell infiltrates surround the
ducts and replace the secretory units (Figure 1). Primary
SS is a common systemic auto immune disorder, affecting
approximately 0.10.4% of the general population with a
female to male ratio of 9:1, a prevalence that is comparable
to that of rheumatoid arthritis.
16
Although the patho-
genetic mechanisms of this autoimmune exocrino pathy
are not yet fully known, SS ariseseither as the primary
disease or occurring secondary to other autoimmune
rheumatic diseasesas a result of infiltration of the func-
tional glandular epithelium by autoreactive lymphocytes.
7
During the past 15 years, the importance of the epi thelial
cell in the pathogenesis and evolution of SS has been
highlighted and has prompted the use of the term auto-
immune epithelitis as an alternative name for the disease.
8
In its early stages, SS can also affect other organs, leading
to extraglandular manifestations, including interstitial
nephritis, liver disease and obstructive bronchitis.
911
Although the disease is limited to the exocrine glands
in the majority of patients, clinical and prognostic cri teria
demand that these patients be distinguished from the
approximately 10% of those who develop extra epithelial
manifestations secondary to the deposition of immune
complexes at extraglandular sites, including small or
medium-sized vessels, renal glomeruli and peripheral
nerve microvessels.
1214
A number of studies have docu-
mented an ongoing B-cell hyperactivity in SS, which
might be associated with an increased incidence of lym-
phoid malignancies in the presence of palpable purpura,
glomerulonephritis and peripheral neuro pathy.
1517
Such
serious immune-complex-mediated manifesta tions,
which usually present later in the course of the disease,
define a distinct group of SS patients who show an
increased risk of mortality owing to lymphoproliferative
hematologic malignancies.
15,17,18
In this Review, we aim to
describe important pathogenetic mechanisms involved in
the initiation and perpetuation of SS.
Pathogenesis of SS
As previously mentioned, the pathogenetic mecha-
nisms responsible for SS are not yet fully known, but in
the presence of a susceptible genetic background, both
environmental and hormonal factors are thought to be
capable of triggering this autoimmune exocrinopathy.
Salivary, lacrimal, and other exocrine glands become
infiltrated with CD4
+
T cells, but substantial numbers
of B cells and plasma cells are also present in inflamed
tissues. Moreover, glandular alteration in cell migration
can also lead to the formation of germinal center-like
structures that contain follicular dendritic cells (DCs)
and proliferating B cells.
19,20
Competing interests
The authors declare no competing interests.
REVIEWS
nrrheum_118_SEP10.indd 529 11/08/2010 16:03:38
20 Macmillan Publishers Limited. All rights reserved 10
530 | SEPTEMBER 2010 | VOLUME 6 www.nature.com/nrrheum
Genetic factors
The observed aggregation of autoimmune diseases in
families of SS patients is supportive for a genetic pre-
disposition to the disease. Alleles within the major
histo compatibility complex (MHC) class II gene region,
mainly HLA-DR and HLA-DQ, are involved in the
pathogenesis of SS. Patients of different ethnic origin
carry different HLA susceptibility alleles. By way of
illustration, white patients from Northern and Western
Europe and from North America show a high prevalence
of B8, DRw52 and DR3 genes, whereas Scandinavian and
Greek patients with SS display strong linkages to the DR2
and DR5 genes.
21
However, it has been shown that HLA
class II alleles are associated with the presence of specific
subsets of autoantibodies, rather than with the disease
itself.
22,23
For example, the production of anti-Ro52
autoantibodies is linked with the presence of the MHC
class II alleles DRB1*0301, DRB3*0101, DQA1*0501 and
DQB1*0201. A genome-wide association study has con-
firmed the genetic association of the interferon (IFN)
regulatory factor 5 (IRF5) rs2004640 T allele with a pre-
disposition to the development of SS (odds ratio, or OR,
1.93 [95% CI 1.153.42]).
24
Another study has revealed
a correlation between polymorphisms in IRF5 (CGGGG
indel, SNP rs10488631) and STAT4 (SNP rs7582694),
genes that encode transcription factors involved in
IFN signaling, and SS development in a Swedish and
Norwegian cohort.
25
Interestingly, the OR for SS in car-
riers with two risk alleles was 1.43, whereas those with
three risk alleles had an OR of 6.78. These findings indi-
cate that a genetic susceptibility conferring an increased
IFN response to different innate stimuli could promote
disease progression.
Hormonal factors
Sex hormones seem to influence humoral and cell-
mediated immune responses, and estrogen is considered
to be one of the factors responsible for gender immuno-
logic dimorphism. Apart from the predominance of
SS in postmenopausal women compared with men,
the results from several experiments in animal models
have indicated a role for estrogen deficiency in SS.
Key points
At the molecular and cellular levels, epithelial cells have an important role in the
initiation and perpetuation of autoimmune lesions in Sjgrens syndrome (SS)
Antigen presentation, apoptosis, chemokine production or germinal center
formation lie at the center of SS pathogenesis; epithelial cells have a key role
in all these processes
Alterations in a number of immune mediators contribute to chronic immune
dysregulation
These changes include: upregulation of type I-interferon-regulated genes;
abnormal expression of B-cell-activating factor; and activation of the
interleukin-23T-helper type 17 cell pathway
Among autoimmune diseases, SS displays the highest incidence of malignant
lymphoproliferative disorders
Severe involvement of exocrine glands, vasculitis, low C4 levels and
cryoglobulinemia at diagnosis identify specific SS patients with a high risk of
lymphoma development and therefore high mortality rates
Mice that lack aromatase (and therefore have an estro-
gen deficiency) develop a lymphoproliferative disease
that resembles SS; the disease is characterized by B-cell
infiltration of the kidney and the spleen.
26
In another
SS mouse model, overexpression in the exocrine glands
of retinoblastoma- associated protein 48 (also known
as histone-binding protein RBBP4), which induces
estrogen-deficiency-dependent apoptosis, caused an
age-dependent SS-like autoimmune exocrinopathy.
27
The sali vary epithelial cells of retinoblastoma- associated
protein 48 transgenic mice functioned as antigen-
presenting cells that directly upregulated the expression
of MHC class II molecules, secreted IFN- and inter-
leukin (IL)-18 and led to the activation of CD4
+
T cells
and glandular inflammation.
27
These findings strongly
suggest that estrogen deficiency stimulates
salivary epi-
thelial cells, via the upregulation
of RBBP4, to present an
autoantigen to the CD4
+
T cells, which
induces lesions in
the salivary glands that resemble
those of
human SS.
Environmental factors
Environmental factors, such as glandular viral infec-
tion, could prompt epithelial cells to activate the HLA-
independent innate immune system through Toll-like
receptors (TLRs); TLRs recognize conserved molecu-
lar patterns shared by large groups of micro-organisms
and products of apoptosis, and induce signaling path-
ways that lead to the production of inflammatory cyto-
kines and upregulation of co-stimulatory and adhesion
mol ecules.
28
Although a number of infectious agents
have been implicated in the pathogenesis of SS, such
as EpsteinBarr virus (EBV), human T-lymphotropic
virus type 1 and hepatitis C virus, their association with
SS appears weak.
29,30
Despite the association between SS
and viral infections being unclear, a high incidence of
EBV reactivation in SS patients has been reported; this
reactivation could contribute to the initiation or per-
petuation of an immune response in target organs.
3134
Interestingly, EBV is a common virus that infects both
salivary epi thelial cells and B cells.
35
Nonetheless, it
remains to be clarified exactly how reactivation of EBV
is induced in lesions of patients with SS, and which speci-
fic molecular mechanisms are involved in the process of
viral reactivation.
Evidence that the coxsackievirus might infect minor
salivary gland cells has also been reported in Greek
patients.
36
Furthermore, epithelial cells of SS patients
have been reported to show high constitutive expression
of several TLRs, which implicates innate immunity in the
autoimmune dysregulation.
37
These findings suggest that,
through an as yet unknown mechanism, the presence of
enteroviral RNA (in the form of the coxsackievirus) that
persistently escapes immune surveillance, activates the
epithelia and leads to chronic immune dysregulation.
However, another study failed to confirm this finding
in French patients.
38
Variations in the genetic poly-
morphisms of virus receptors and HLA among the two
study populations, as well as differences in the prevalence
of enteroviral infections in Greece compared to other
European countries could explain the discrepancy.
REVIEWS
nrrheum_118_SEP10.indd 530 11/08/2010 16:03:38
20 Macmillan Publishers Limited. All rights reserved 10
NATURE REVIEWS | RHEUMATOLOGY VOLUME 6 | SEPTEMBER 2010 | 531
Mild lesion
T cell infltrates B cell infltrates
Severe lesion
Altered glandular homeostasis
Salivary glands of the nonobese diabetic mouse model of
SS are characterized by abnormalities of glandular epi-
thelial cells that occur before infiltration by auto reactive
lymphocytes. Such abnormalities include disturbed cell
proliferation at birth, increased apoptosis of acinar tissue,
breakdown of secreted proteins and increased expression
of IFN-.
39
Altered glandular homeo stasis has also
been
reported in patients with SS. Biopsy samples from patients
with SS, compared to normal controls, showed a notable
increase in the expression of laminin messenger RNA and
protein before
lymphocytic infiltration, suggesting that
altered synthesis of the basement membrane of glandu-
lar epithelial cells is an early event that is associated with
salivary gland pathology in
SS.
40
Furthermore, acinar
and ductal cells from the salivary glands of patients with
SS have a molecular repertoire that is likely to confer an
increased capacity to dis organize their extracellular matrix
environment.
41
The increased gelatinolytic activity medi-
ated by matrix metallo proteinases of acinar and ductal
cells in the salivary glands of SS patients could allow the
subsequent invasion of cytotoxic T lymphocytes.
42,43
Although these findings suggest a primary intrinsic
homeostatic problem in the glands of SS patients, it is not
yet clear whether or not such a defect is an initial event in
the pathogenesis of SS. A special focus on early changes
in this disease could help the understanding of the specif ic
biologic events that lead to clinical signs of SS.
Perpetuation of inflammation
Critical to the initiation and perpetuation of SS patho-
genesis are the upregulation of adhesion molecules and
the production of chemokines and cytokines, which
together promote the migration of lymphocytes and
DCs into the glands, maintaining their cycle of homing
(Figure 2).
The role of epithelial cells
Despite the fact that endothelial cells in the salivary
glands of SS patients express adhesion molecules and
are morphologically similar to high endothelial venules
that might draw lymphocytes and DCs into the glands,
their role in mediating the local immune response has
not been clearly defined.
44
By contrast, evidence exists
that epithelial cells in SS lesions are active participants
in the induction and perpetuation of the inflamma-
tory process.
45
Although salivary gland epithelial cells
have never been directly shown to function as antigen-
presenting cells, they possess all the features needed to
do so.
4649
Their capacity to show enhanced expression
of CD40 and adhesion molecules, as well as to produce
lymphoid chemokines, cytokines and B-cell-activating
factor (BAFF, also known as BLyS and tumor necro-
sis factor ligand superfamily member 13b), indicates
their potential role in the accumulation of DCs, T cells
and B cells in the inflamed salivary glands and in the
formati on of lymphoid tissue.
45,5053
Figure 1 | Lesions in the salivary glands of patients with Sjgrens syndrome. The histopathological hallmark of SS is
periductal cellular infiltration of the salivary glands. In mild lesions, activated T cells predominate, whereas B cells prevail
in severe histologic lesions. Immunohistochemical analysis of minor salivary gland tissue from patients with SS; rabbit-
polyclonal antibodies to human CD3 and mouse-monoclonal antibodies to human CD20 were used to analyze the presence
of T and B cells respectively, original magnification 200. Abbreviation: SS, Sjgrens syndrome.
REVIEWS
nrrheum_118_SEP10.indd 531 11/08/2010 16:03:41
20 Macmillan Publishers Limited. All rights reserved 10
532 | SEPTEMBER 2010 | VOLUME 6 www.nature.com/nrrheum
The fact that the activation status of epithelial cells
derived from patients with SS remains unaltered
in vitro for a long period of time prompts the hypo-
thesis that they become activated intrinsically.
54
After
their migration to the glands, lymphocytes interact with
epithelial cells.
55
The latter are further activated by pro-
inflammatory cytokines such as IL-1, IFN- and tumor
necrosis factor (TNF) produced by neighboring T cells
and DCs.
56
Studies have shown that SS salivary acinar
epithelial cells express elevated apoptosis regulator BAX
and undergo apoptosis, which causes dysregulation of
the hosting organ.
57
By contrast, infiltrating lympho-
cytes express elevated apoptosis regulator Bcl-2 and are
resistant to apoptosis, which prolongs their survival.
Furthermore, through apoptosis and the formation of
membrane-bound vesicles known as exosomes, epi-
thelial cells present intracellular autoantigens, a process
that contributes to the breakdown of immune tolerance.
58
Ro/SSA and La/SSB are translocated from the nucleus
to apoptotic blebs, where they trigger the production,
by infiltrating B cells, of autoantibodies against these
autoantigens. Given that BAFF can be secreted by human
salivary gland epithelial cells following stimulation by
type I IFN and that viral infection directly induces
BAFF secretion by epithelial cells, it has been suggested
that epithelial cells might not only express and present
autoantigens but also concomitantly activate B cells by
the local secretion of BAFF.
59,60
The role of DCs
Interestingly, the action of type I IFN could orchestrate
all of the above described autoimmune mechanisms,
thereby linking the innate and adaptive immune systems
in SS. In this regard, analysis of minor salivary gland
tissue from patients with SS revealed enhanced levels
of IFN-inducible gene expression;
61,62
plasmacytoid
DCs were detected in the human SS salivary glands
by immuno histochemistry, indicating that the persis-
tence of the type I IFN signature could be related to an
inflammatory cycle that is associated with an inappro-
priate maturation of DCs, stimulation of autoreactive
T cells, production of autoantibodies and increased
production of endogenous IFN-.
61,62
The early appear-
ance of DCs in the salivary glands and the produc-
tion by these cells of type I IFNs could be important,
as they can cause abnormal retention and subsequent
activation of lympho cytes in these tissues, also result-
ing in increased metalloproteinase activity.
63
It has been
hypothesized that viral infections or RNA-containing
immune complexes acting through TLRs are responsible
for the activation of plasmacytoid DCs.
61
Interestingly,
a 2009 study demon strated that when NZB/W F1
mice were repeatedly injected with the TLR3 ligand
polyinosiniccytidylic acid, a rapid induction of type I
IFN and proinflammatory cytokines within the salivary
glands was observed, resulting in a considerable and
rapid loss of glandular function.
64
It has been suggested
that the salivary epithelial cells activated by TLR3 ligand
are the major source of type I IFNs within the gland.
64
This study further reinforces the notion that glandu-
lar epithelial cells have an important and active role in
the pathogenesis of SS and, moreover, that chronic viral
infection of salivary epithelial cells confers the potential
for initiation of salivary gland inflammation.
Resting epithelium Deregulated epithelium
BAFF
Type I IFNs
IL-1, IFN-, TNF
Effector T-cell cytotoxicity
Viral infection
Genetic predisposition
Estrogen defciency
Lymphoid chemokine production
Upregulation of adhesive molecules
Properties of antigen-presenting cells
Increased apoptosis and autoantigens expression
BAFF production
Activation of self reactive T cells
Aberrant homing
Breakdown of B-cell tolerance
Local production of autoantibodies
Production
T cell
B cell
pDCs
Figure 2 | Cellular and molecular pathways implicated in the pathogenesis of Sjgrens syndrome. Environmental (viral
infection) and hormonal factors (estrogen deficiency), in concert with an appropriate genetic background, are believed to
trigger SS, which dysregulates epithelial cells and allows the aberrant homing and activation of DCs, T cells and B cells.
Following the migration of lymphocytes into the glands in response to chemokines and specific adhesion molecules, T cells
interact with epithelial cells. Epithelial cells are further activated by proinflammatory cytokines (IL-1, IFN- and TNF), which
are produced by adjacent T cells. The early accumulation of pDCs in the target tissues, which produce high levels of type I
IFNs, seems to be important, as these cells can further dysregulate the immune response through abnormal retention of
lymphocytes in the tissues and their subsequent activation. IFN- is a powerful stimulator of the production of BAFF by
epithelial cells, DCs and T cells. BAFF stimulates aberrant B-cell maturation, leading to the emergence of self-reactive
B cells, which locally produce autoantibodies. Abbreviations: BAFF, B-cell-activating factor; DCs, dendritic cells; IFN,
interferon; IL-1, interleukin 1; pDCs, plasmacytoid DCs; SS, Sjgrens syndrome; TNF, tumor necrosis factor.
REVIEWS
nrrheum_118_SEP10.indd 532 11/08/2010 16:03:42
20 Macmillan Publishers Limited. All rights reserved 10
NATURE REVIEWS | RHEUMATOLOGY VOLUME 6 | SEPTEMBER 2010 | 533
The role of cytokines
Both proinflammatory and anti-inflammatory pathways
could be driven by this immune response. The inability to
suppress inflammation can lead to chronic tissue damage
and impaired salivary gland function. On examination of
cytokine mRNA expression in the salivary glands of SS
patients and animal models of the disease, an increase in
proinflammatory cytokines, including IL-1, IL-6, IL-7,
IL-10, IFN- and TNF, was noted.
6567
Cytokines pro-
duced by type 2 T-helper (T
H
) cells (T
H
2 cytokines) have
been found to dominate the early phase of SS, whereas
T
H
1 cytokines are associated with a later stage of the
disease.
68
Although such observations suggest that func-
tions associated with T
H
1 and T
H
2 cells are implicated in
the pathogenesis of clinical disease, CD4
+
T
H
17 memory
cells have also been reported within the lymphocytic
foci of the salivary and lacrimal glands of SS-susceptible
C57BL/6.NOD-Aec1Aec2 mice, indicating that the issue
is more complicated than previously thought.
69
In C57BL/6.NOD-Aec1Aec2 mice, the impairment of
exocrine gland tissue resulting from the autoimmune
attack is characterized by the reduced function of regula-
tory CD4
+
cells (T
REG
1 cells) and IL-27-producing DCs,
which would normally downregulate CD4
+
T
H
17 cells,
thus inducing their aberrant activation.
70
The involve-
ment of the IL-23T
H
17 pathway in the pathogenesis of
SS has been supported by data from studies of mice that
lack Ro52, an E3 ubiquitin ligase that is likely to regulate
the levels of several IRFs by ubiquitinyla ion. Ro52
/
mice
develop systemic autoimmunity that is characterized by
the enhanced production of pro inflammatory cytokines
regulated by IRFs, including cytokines involved in the
IL-23T
H
17 pathway.
71
Interestingly, loss of IL-23 and
IL-17 by genetic deletion of the p19 subunit of IL-23
in the Ro52
/
mice conferred protection from systemic
autoimmunity, suggesting that a defect in Ro52 func-
tion can lead to tissue inflammation and systemic auto-
immunity through the IL-23T
H
17 pathway. Likewise,
increased serum levels of IL-17 in SS patients, along with
increased levels of T
H
17 cells and related cytokines, are
dominant in salivary glands and strongly correlate with
the histological focus score.
72
Although compensatory
control of T
REG
1 cells against T
H
17 cell expansion seems
to occur in early and moderate infiltrations, in advanced
lesions T
REG
1 cells fail to control immune-mediated
tissue injury.
73,74
Dysregulation of B cells
As the lymphoid infiltration in the salivary glands is
established, CD4
+
T cells and DCs locally produce B-cell
targeted cytokines and other survival factors, including
BAFF and APRIL (a proliferation-inducing ligand, also
known as TNF ligand superfamily member 13).
52,56
B-cell
dysregulation in SS patients (Figure 3) can be demon-
strated by the presence of circulating immune complexes,
hypergammaglobulinemia, alterations in sub populations
of peripheral B cells, oligoclonal B-cell expansion and
a well-described increased risk of developing non-
Hodgkin lymphoma (NHL).
75,76
An ectopic germinal-
center-like structure found in one-fifth of patients with
SS represents the histologic hallmark of this abnormal
B-cell proliferation.
76
Ectopic germinal centers
Newly formed ectopic germinal centers have been
proposed to be sites of autoantibody production as
well as being involved in lymphomagenesis in patients
with SS.
77
Ectopic germinal centers represent a micro-
environment in the salivary glands in which B cells that
have bypassed the peripheral checkpoint against auto-
reactivity proceed to proliferation and incomplete dif-
ferentiation through T-cell-dependent pathways into
memory B cells and plasma cells.
78
Interestingly, the
formation of germinal centers in salivary glands of SS
patients correlates with increased glandular inflamma-
tion, elevated titers of rheuma toid factor (RF), increased
Risk of non-Hodgkin lymphoma
B-cell hyperactivity and monoclonality
Ectopic lymphoid tissue formation
Circulating immune complexes
Impaired censoring
Disturbed selection
Persistence of RF-expressing B cells
Oligoclonal B-cell expansion
p53 mutations
Malignant transformation
B-cell dysregulation
Perpetuation of SS pathogenesis
Figure 3 | B-cell hyperactivity, monoclonality and lymphomagenesis. The transition from a lymphoepithelial sialadenitis to
malignant lymphoma is a multistep process that is poorly understood. Chronic antigenic stimulation has an essential role
in the development of SS-associated lymphoproliferation by driving the proliferation of specific B cells and by increasing the
frequency of their transformation. B cells expressing cell surface RF are frequently detected in the salivary glands, which
suggests that clonal expansion in these glands might arise from antigen selection of RF-expressing B cells. Large amounts
of IgG produced in the salivary glands of SS patients could result in uncontrolled antigenic stimulation of RF-expressing
B cell clones in the ectopic germinal centers. Additional molecular oncogenic events, such as microsatellite instability, loss
of B-cell cycle control, inactivation of tumor suppressor genes and the forced overproduction of specific biological
stimulators of B cells (such as BAFF) seem to contribute to the emergence and progression of the malignant overgrowth.
Abbreviations: BAFF, B-cell activating factor; RF, rheumatoid factor; SS, Sjgrens syndrome.
REVIEWS
nrrheum_118_SEP10.indd 533 11/08/2010 16:03:43
20 Macmillan Publishers Limited. All rights reserved 10
534 | SEPTEMBER 2010 | VOLUME 6 www.nature.com/nrrheum
levels of auto antibodies and increased IgG levels com-
pared with SS patients without germinal centers.
79,80
These findings suggest that local selection and pro-
liferation of autoreactive B cells occur in ectopic germi-
nal centers. Additionally, increased levels of circulating
auto antibodies might reflect local autoantibody produc-
tion in the salivary glands. Szodoray et al.
81
identified
reliable biomarkers that detected the presence of germi-
nal centers in SS patients, among which CC-chemokine
ligand (CCL)-11, BAFF and IFN- have the strongest
discriminatory capacity.
81
The role of BAFF
Accumulating evidence has identified BAFF as an impor-
tant mediator in the neogenesis of germinal centers in
SS patients. BAFF can be secreted not only by salivary
epithelial cells but also directly by B cells, which high-
lights the important effect of this factor in the initiation
and perpetuation of B-cell dysregulation in SS.
82
The
reduced level of apoptosis among BAFF-expressing cells
in the salivary glands from SS patients potentially leads
to abundant BAFF expression, thereby amplifying B-cell
signal ing, promoting the regional proliferation of B cells
and their differentiation into autoantibody-producing
plasma cells.
83,84
Plasma levels of BAFF in SS patients are
strongly associated with autoantibody titers, including
those of RF and anti-Ro/SSA.
84
BAFF-transgenic mice
develop a disease that resembles human systemic lupus
erythematosus (SLE), and subsequently show infiltration
of salivary glands predominantly by activated B cells.
The occurrence of SS-like disease in BAFF-transgenic
mice could feasibly be explained by the excessive sur-
vival signals that are received by autoreactive B cells,
causing these cells to bypass the critical tolerance check-
point while maturing in the spleen.
85
In addition, it has
been suggested that the role of BAFF overexpression in
the impairment of self-tolerance in this animal model
further relies on the suppression of the protective effects
of DCs against the emergence of autoreactive T cells.
85
In
the salivary glands of patients with SS, the combination
of apoptotic bodies from epithelial cells and anti-Ro/
SSA antibodies could induce the production of IFN-
by infiltrating cells, which, in turn, could induce BAFF
expression by epithelial cells, leading to the stimulation
of autoreactive B cells.
5961
Interestingly, high levels of
infiltration by macrophages have been related to type II
cryoglobulinemia, parenchymal-organ involvement,
glandular inflammation and, most importantly, NHL,
suggesting the potential involvement of these cells in
disease severity and NHL development.
20
Together,
these data suggest that the sustained survival of auto-
reactive B cells, production of autoantibodies or later
development of NHL could be attributed to local BAFF
expression.
78
B-cell transformation
Patients with SS display severe B cell abnormalities com-
pared to that observed in other autoimmune diseases
such as SLE, with an increased concentration of serum
levels of BAFF.
86,87
The numbers of CD19
+
CD27
naive
B cells are decreased and the numbers of CD19
+
CD27
+
memory B cells are increased in patients
with active SLE,
in contrast with patients with SS, who display a consider-
able reduction in the number of peripheral CD27
+
memory B cells as a result of their migration from periph-
eral blood to the inflamed salivary glands.
88,89
The lym-
phoid population acquired secondary to the autoimmune
process (known as the mucosa-associated lymphoid
tissue [MALT] component) surrounds and infiltrates the
salivary ducts, and represents the substrate from which
B-cell lympho matous proliferation occurs.
90
The transition of reactive lymphoepithelial sialadeni-
tis from monoclonality to monoclonal lymphoma is
generally considered to represent a multistep process,
yet is poorly understood. Speculation exists that
chronic stimulation by exoantigens or autoantigens has
an essential role in the development of these tumors,
by driving the pro liferation of specific B cells and by
increasing the frequency of their transformation.
91
In
view of the intense modification of immunoglobulin
genes during immune responses, a number of criti-
cal transforming events, such as the inactivation of
tumor suppressor genes (for example, p53 mutations)
or chromosomal rearrangements, might result from the
intense cellular activity occurring within ectopic germi-
nal centers in SS.
92
Accordingly, SS patients who have
a high risk of developing NHL exhibit splenomegaly,
lymphadeno pathy,
type II cryoglobulinemia and parotid
swelling, all of which are indicators of extensive lympho-
proliferation.
17,9294
In addition, the occurrence of type II
cryoglobulinemia is thought to represent the transition
from polyclonal B-cell hyperactivity, a hallmark of SS,
to monoclonal expansion of B cells producing an IgMk
immunoglobulin with RF activity, suggesting that some
SS-derived NHLs originate from precursors that bear a
functional autoreactive B-cell receptor.
95
The persistence
of self-reactive RF-expressing B cells in SS might reflect
abnormal antigen selection, altered stimulation and
compromised censoringall mechanisms that magnify
the risk of malignant B-cell transformation.
78
Disease outcome and mortality
Published studies on the survival of SS patients are
limited in varied respects, most probably owing to rela-
tively small sample sizes (Table 1). However, results from
a number of studies indicate that, compared to other
autoimmune diseases, SS is associated with a notably
Table 1 | Studies of mortality in patients with Sjgrens syndrome
Study No. of
patients
Overall deaths
(lymphoma-related)
Standard
mortality ratio
Skopouli et al. (2000)
15
261 11 (3) 2.07
Ioannidis et al. (2002)
18
723 39 (7) 1.15
Petrovara et al. (2001)
106
110 17 (2) 1.20
Theander et al. (2006)
99
484 34 (6) 1.17
Alamanos et al. (2006)
102
422 47 (3) 1.02
Brito-Zern et al. (2007)
103
266 25 (2) 1.22
REVIEWS
nrrheum_118_SEP10.indd 534 11/08/2010 16:03:43
20 Macmillan Publishers Limited. All rights reserved 10
NATURE REVIEWS | RHEUMATOLOGY VOLUME 6 | SEPTEMBER 2010 | 535
high incidence of malignant NHL.
16,75,93,96100
A severe
involvement of the exocrine glands, and the presence of
vasculitis, low C4 levels and cryoglobulinemia at diag-
nosis can be used to identify patients with SS who are at
a high risk of developing lymphoma.
15,18,101104
Apart from this notably higher incidence of malignant
NHL, SS patients typically show only modest or clini-
cally insignificant deterioration in specific organ-related
symptomatology and function, which, together with the
low frequency of systemic effects, is likely to provide
an explanation for why mortality rates are only slightly
increased in patients with SS in comparison with the
remainder of the population.
105,106
This slight increase
in mortality rates in SS patients are mainly because of
the increased incidence of lymphoproliferative disease.
These largely unaffected mortality rates also contrast
with those of other connective tissue diseases such as
rheumatoid arthritis, scleroderma and SLE, which are
increased, mainly owing to cardiovascular disease.
107
Comorbidities have the capacity to influence the
prognosis of primary disease; the greater the number of
comorbidities, the greater the risk of patient hospitaliza-
tion and mortality. Comorbidities might be associated
with SS itself (for example, nephritis, interstitial lung
disease and peripheral neuropathy) or with its treatment
(such as immunosuppressive therapy). Unfortunately,
no published data on the incidence of these comorbidi-
ties and their mortality risk among SS patients exists.
Published data on the risk of accelerated athero sclerosis,
another comorbidity in SS, are lacking. Subclinical
athero sclerosis (intimamedia thickening of the large
vessels) was reported in about 50% of a cohort of young
women with SS.
108
Interestingly, these vascular changes
were not associated with the presence of cardiovascular
risk factors or any drug-induced effect, suggesting that
certain immune system characteristics of the disease
trigger early atherosclerosis. However, the presence of
early subclinical atherosclerosis does not always correlate
with an increased risk of cardiovascular-related death.
Consequently, further studies are needed to determine
the risk of atherosclerosis and cardiovascular-related
mortality among patients with SS.
Conclusions
The etiology and pathogenesis of SS are not clearly
understood. The hallmark of this disease is an immuno-
logically mediated inflammatory exocrinopathy that
is initially characterized by periductal infiltration of
the salivary tissue by lymphocytes and plasma cells.
The auto immune response in SS could ultimately be
driven by cellular proteins acting as autoantigens follow-
ing epi thelial cell apoptosis. In this context, it is feasible
to consider the epithelium as the main orchestrator of
the pathogenesis of SS. Dysregulation of sex hormones,
abnormalities in glandular homeostasis, deficiency in
T
REG
1 cells and dysregulation of plasmacytoid DCs con-
tribute to the disruption of peripheral tolerance and the
stimulation of autoreactive immune cells. Eventually,
these lymphocytes promote autoantibody
production
and damage the epithelium through their cytotoxicity.
SS is characterized by a slightly increased mortality
rate compared to the general population. However, the
develop ment of NHL is associated with an increased
overall disease mortality. The transition of reactive
lympho epithelial sialadenitis to malignant NHL is gen-
erally considered to be a multistep process. Chronic
antigenic stimulation, abnormal B-cell activation in the
inflamed tissues, somatic hypermutations and onco-
genic events in germinal centers are usually implicated
in malignant transformation. Severe involvement of the
exocrine glands, vasculitis, hypo complementemia and
cryoglobulinemia, which characterize a high-risk popu-
lation of patients, all highlight the paramount importance
of closer monitoring, as well as the need for tailored and
robust therapeutic management.
Review criteria
We searched for original articles published between
1968 and 2010 focusing on pathogenesis and mortality
in Sjgrens syndrome using MEDLINE and PubMed.
The search terms we used were Sjgrens syndrome,
mortality, pathogenesis and autoimmune
epithelitis. All papers identified were English-language,
full text papers. We also searched the reference lists of
identified articles for further papers.
1. Anaya, J. M. & Talal, N. In Arthritis and Allied
Conditions: a Textbook of Rheumatology 13
th
edn
(ed. Koopman, W. J.) 15611580 (Williams &
Wilkins, Baltimore, 1997).
2. Alamanos, Y. et al. Epidemiology of primary
Sjgrens syndrome in north-west Greece,
19822003. Rheumatology (Oxford) 45,
187191 (2006).
3. Trontzas, P. I. & Andrianakos, A. A. Sjogrens
syndrome: a population based study of
prevalence in Greece. The ESORDIG study. Ann.
Rheum. Dis. 64, 12401241 (2005).
4. Bowman, S. J., Ibrahim, G. H., Holmes, G.,
Hamburger, J. & Ainsworth, J. R. Estimating the
prevalence among Caucasian women of primary
Sjgrens syndrome in two general practices in
Birmingham, UK. Scand. J. Rheumatol. 33,
3943 (2004).
5. Delaleu, N., Jonsson, M. V., Appel, S. &
Jonsson, R. New concepts in the pathogenesis
of Sjgrens syndrome. Rheum. Dis. Clin. North
Am. 34, 833845 (2008).
6. Venables, P. J. Sjgrens syndrome. Best Pract.
Res. Clin. Rheumatol. 18, 313329 (2004).
7. Ramos-Casals, M. et al. SS-HCV Study Group.
Sjgren syndrome associated with hepatitis C
virus: a multicenter analysis of 137 cases.
Medicine (Baltimore) 84, 8189 (2005).
8. Moutsopoulos, H. M. Sjgrens syndrome:
autoimmune epithelitis. Clin. Immunol.
Immunopathol. 72, 162165 (1994).
9. Papiris, S. A. et al. Lung involvement in primary
Sjgrens syndrome is mainly related to the
small airway disease. Ann. Rheum. Dis. 58,
6164 (1999).
10. Tu, W. H., Shearn, M. A., Lee, J. C. & Hopper, J. Jr.
Interstitial nephritis in Sjgrens syndrome. Ann.
Intern. Med. 69, 11631170 (1968).
11. Skopouli, F. N., Barbatis, C. &
Moutsopoulos, H. M. Liver involvement in
primary Sjgrens syndrome. Br. J. Rheumatol.
33, 745748 (1994).
12. Ramos-Casals, M. et al. Cutaneous vasculitis in
primary Sjgren syndrome: classification and
clinical significance of 52 patients. Medicine
(Baltimore) 83, 96106 (2004).
13. Talal, N., Zisman, E. & Schur, P. H. Renal tubular
acidosis, glomerulonephritis and immunologic
factors in Sjgrens syndrome. Arthritis Rheum.
11, 774786 (1968).
14. Tsokos, M., Lazarou, S. A. & Moutsopoulos, H. M.
Vasculitis in primary Sjgrens syndrome.
Histologic classification and clinical
presentation. Am. J. Clin. Pathol. 88, 2631
(1987).
15. Skopouli, F. N., Dafni, U., Ioannidis, J. P. &
Moutsopoulos, H. M. Clinical evolution, and
morbidity and mortality of primary Sjogrens
syndrome. Semin. Arthritis Rheum. 29, 296304
(2000).
16. Voulgarelis, M., Dafni, U. G., Isenberg, D. A. &
Moutsopoulos, H. M. Malignant lymphoma in
primary Sjgrens syndrome: a multicenter,
retrospective, clinical study by the European
Concerted Action on Sjgrens Syndrome.
Arthritis Rheum. 42, 17651772 (1999).
REVIEWS
nrrheum_118_SEP10.indd 535 11/08/2010 16:03:43
20 Macmillan Publishers Limited. All rights reserved 10
536 | SEPTEMBER 2010 | VOLUME 6 www.nature.com/nrrheum
17. Tzioufas, A. G., Boumba, D. S., Skopouli, F. N. &
Moutsopoulos, H. M. Mixed monoclonal
cryoglobulinemia and monoclonal rheumatoid
factor cross-reactive idiotypes as predictive
factors for the development of lymphoma in
primary Sjgrens syndrome. Arthritis Rheum.
39, 767772 (1996).
18. Ioannidis, J. P., Vassiliou, V. A. &
Moutsopoulos, H. M. Long-term risk of mortality
and lymphoproliferative disease and predictive
classification of primary Sjogrens syndrome.
Arthritis Rheum. 46, 741747 (2002).
19. Katsifis, G. E., Moutsopoulos, N. M. &
Wahl, S. M. T lymphocytes in Sjgrens
syndrome: contributors to and regulators of
pathophysiology. Clin. Rev. Allergy Immunol. 32,
252264 (2007).
20. Manoussakis, M. N. et al. Rates of infiltration by
macrophages and dendritic cells and expression
of interleukin-18 and interleukin-12 in the
chronic inflammatory lesions of Sjgrens
syndrome: correlation with certain features of
immune hyperactivity and factors associated
with high risk of lymphoma development.
Arthritis Rheum. 56, 39773988 (2007).
21. Bolstad, A. I. & Jonsson, R. Genetic aspects of
Sjgrens syndrome. Arthritis Res. 4, 353359
(2002).
22. Gottenberg, J. E. et al. In primary Sjgrens
syndrome, HLA class II is associated exclusively
with autoantibody production and spreading of
the autoimmune response. Arthritis Rheum. 48,
22402245 (2003).
23. Miyagawa, S. et al. Polymorphisms of HLA
class II genes and autoimmune responses to
Ro/SS-ALa/SS-B among Japanese subjects.
Arthritis Rheum. 41, 927934 (1998).
24. Miceli-Richard, C. et al. Association of an IRF5
gene functional polymorphism with Sjgrens
syndrome. Arthritis Rheum. 56, 39893994
(2007).
25. Nordmark, G. et al. Additive effects of the major
risk alleles of IRF5 and STAT4 in primary Sjgrens
syndrome. Genes Immun. 10, 6876 (2009).
26. Shim, G. J. et al. Aromatase-deficient mice
spontaneously develop a lymphoproliferative
autoimmune disease resembling Sjogrens
syndrome. Proc. Natl Acad. Sci. USA 101,
1262812633 (2004).
27. Ishimaru, N. et al. Expression of the
retinoblastoma protein RbAp48 in exocrine
glands leads to Sjgrens syndrome-like
autoimmune exocrinopathy. J. Exp. Med. 205,
29152927 (2008).
28. Takeda, K., Kaisho, T. & Akira, S. Toll-like
receptors. Annu. Rev. Immunol. 21, 335376
(2003).
29. Pflugfelder, S. C. et al. EpsteinBarr virus and the
lacrimal gland pathology of Sjgrens syndrome.
Am. J. Pathol. 143, 4964 (1993).
30. Green, J. E., Hinrichs, S. H., Vogel, J. & Jay, G.
Exocrinopathy resembling Sjgrens syndrome in
HTLV-1 tax transgenic mice. Nature 341, 7274
(1989).
31. Saito, I., Servenius, B., Compton, T. & Fox, R. I.
Detection of EpsteinBarr virus DNA by
polymerase chain reaction in blood and tissue
biopsies from patients with Sjgrens syndrome.
J. Exp. Med. 169, 21912198 (1989).
32. Mariette, X., Gozlan, J., Clerc, D., Bisson, M. &
Morinet, F. Detection of EpsteinBarr virus DNA
by in situ hybridization and polymerase chain
reaction in salivary gland biopsy specimens from
patients with Sjgrens syndrome. Am. J. Med.
90, 286294 (1991).
33. Inoue, H. et al. Possible involvement of EBV-
mediated alpha-fodrin cleavage for organ-specific
autoantigen in Sjgrens syndrome. J. Immunol.
166, 58015809 (2001).
34. Nagata, Y. et al. Activation of EpsteinBarr virus
by saliva from Sjgrens syndrome patients.
Immunology 111, 223229 (2004).
35. Yamaoka, K., Miyasaka, N. & Yamamoto, K.
Possible involvement of EpsteinBarr virus in
polyclonal B cell activation in Sjgrens
syndrome. Arthritis Rheum. 31, 10141021
(1988).
36. Triantafyllopoulou, A., Tapinos, N. &
Moutsopoulos, H. M. Evidence for coxsackievirus
infection in primary Sjgrens syndrome. Arthritis
Rheum. 50, 28972902 (2004).
37. Spachidou, M. P. et al. Expression of functional
Toll-like receptors by salivary gland epithelial
cells: increased mRNA expression in cells
derived from patients with primary Sjgrens
syndrome. Clin. Exp. Immunol. 147, 497503
(2007).
38. Gottenberg, J. E. et al. Failure to confirm
coxsackievirus infection in primary Sjgrens
syndrome. Arthritis Rheum. 54, 20262028
(2006).
39. Cha, S., Peck, A. B. & Humphreys-Beher, M. G.
Progress in understanding autoimmune
exocrinopathy using the non-obese diabetic
mouse: an update. Crit. Rev. Oral Biol. Med. 13,
516 (2002).
40. McArthur, C. P., Daniels, P. J., Kragel, P.,
Howard, P. F. & Julian, L. Sjgrens syndrome
salivary gland immunopathology: increased
laminin expression precedes lymphocytic
infiltration. J. Autoimmun. 10, 5965 (1997).
41. Goicovich, E. et al. Enhanced degradation of
proteins of the basal lamina and stroma by
matrix metalloproteinases from the salivary
glands of Sjgrens syndrome patients:
correlation with reduced structural integrity of
acini and ducts. Arthritis Rheum. 48,
25732584 (2003).
42. Molina, C. et al. Basal lamina disorganisation of
the acini and ducts of labial salivary glands from
patients with Sjgrens syndrome: association
with mononuclear cell infiltration. Ann. Rheum.
Dis. 65, 178183 (2006).
43. Prez, P. et al. Differential expression of matrix
metalloproteinases in labial salivary glands of
patients with primary Sjgrens syndrome.
Arthritis Rheum. 43, 28072817 (2000).
44. Aziz, K. E., McCluskey, P. J., Montanaro, A. &
Wakefield, D. Vascular endothelium and
lymphocyte adhesion molecules in minor
salivary glands of patients with Sjgrens
syndrome. J. Clin. Lab. Immunol. 37, 3949
(1992).
45. Xanthou, G. et al. Lymphoid chemokine
messenger RNA expression by epithelial cells in
the chronic inflammatory lesion of the salivary
glands of Sjgrens syndrome patients: possible
participation in lymphoid structure formation.
Arthritis Rheum. 44, 408418 (2001).
46. Moutsopoulos, H. M. et al. HLA-DR expression by
labial minor salivary gland tissues in Sjgrens
syndrome. Ann. Rheum. Dis. 45, 677683
(1986).
47. Manoussakis, M. N. et al. Expression of B7
costimulatory molecules by salivary gland
epithelial cells in patients with Sjgrens
syndrome. Arthritis Rheum. 42, 229239
(1999).
48. Matsumura, R. et al. Glandular and
extraglandular expression of costimulatory
molecules in patients with Sjgrens syndrome.
Ann. Rheum. Dis. 60, 473482 (2001).
49. Manoussakis, M. N. & Kapsogeorgou, E. K. The
role of epithelial cells in the pathogenesis of
Sjgrens syndrome. Clin. Rev. Allergy Immunol.
32, 225230 (2007).
50. Tsunawaki, S. et al. Possible function of salivary
gland epithelial cells as nonprofessional antigen-
presenting cells in the development of Sjgrens
syndrome. J. Rheumatol. 29, 18841896
(2002).
51. Dimitriou, I. D., Kapsogeorgou, E. K.,
Moutsopoulos, H. M. & Manoussakis, M. N.
CD40 on salivary gland epithelial cells: high
constitutive expression by cultured cells from
Sjgrens syndrome patients indicating their
intrinsic activation. Clin. Exp. Immunol. 127,
386392 (2002).
52. Lavie, F. et al. Expression of BAFF (BLyS) in
T cells infiltrating labial salivary glands from
patients with Sjgrens syndrome. J. Pathol. 202,
496502 (2004).
53. Ohlsson, M., Szodoray, P., Loro, L. L.,
Johannessen, A. C. & Jonsson, R. CD40, CD154,
Bax and Bcl-2 expression in Sjgrens syndrome
salivary glands: a putative anti-apoptotic role
during its effector phases. Scand. J. Immunol.
56, 561571 (2002).
54. Mitsias, D. I., Kapsogeorgou, E. K. &
Moutsopoulos, H. M. The role of epithelial cells
in the initiation and perpetuation of autoimmune
lesions: lessons from Sjgrens syndrome
(autoimmune epithelitis). Lupus 15, 255261
(2006).
55. Jonsson, R., Gordon, T. P. & Konttinen, Y. T.
Recent advances in understanding molecular
mechanisms in the pathogenesis and antibody
profile of Sjgrens syndrome. Curr. Rheumatol.
Rep. 5, 311316 (2003).
56. Vogelsang, P., Jonsson, M. V., Dalvin, S. T. &
Appel, S. Role of dendritic cells in Sjgrens
syndrome. Scand. J. Immunol. 64, 219226
(2006).
57. Kong, L. et al. Bcl-2 family expression in salivary
glands from patients with primary Sjgrens
syndrome: involvement of Bax in salivary gland
destruction. Clin. Immunol. Immunopathol. 88,
133141 (1998).
58. Kapsogeorgou, E. K., Abu-Helu, R. F.,
Moutsopoulos, H. M. & Manoussakis, M. N.
Salivary gland epithelial cell exosomes: A source
of autoantigenic ribonucleoproteins. Arthritis
Rheum. 52, 15171521 (2005).
59. Ittah, M. et al. B-cell-activating factor of the
tumor necrosis factor family (BAFF) is expressed
under stimulation by interferon in salivary gland
epithelial cells in primary Sjgrens syndrome.
Arthritis Res. Ther. 8, R51 (2006).
60. Ittah, M. et al. B-cell-activating factor
expressions in salivary epithelial cells after
dsRNA virus infection depends on RNA-activated
protein kinase activation. Eur. J. Immunol. 39,
12711279 (2009).
61. Bve, U. et al. Activation of the type I interferon
system in primary Sjgrens syndrome:
a possible etiopathogenic mechanism. Arthritis
Rheum. 52, 11851195 (2005).
62. Gottenberg, J. E. et al. Activation of IFN pathways
and plasmacytoid dendritic cell recruitment in
target organs of primary Sjgrens syndrome. Proc.
Natl Acad. Sci. USA 103, 27702775 (2006).
63. Ma-Krupa, W. et al. Activation of arterial wall
dendritic cells and breakdown of self-tolerance
in giant cell arteritis. J. Exp. Med. 199, 173183
(2004).
64. Deshmukh, U. S., Nandula, S. R.,
Thimmalapura, P. R., Scindia, Y. M. & Bagavant, H.
Activation of innate immune responses through
Toll-like receptor 3 causes a rapid loss of salivary
gland function. J. Oral Pathol. Med. 38, 4247
(2009).
REVIEWS
nrrheum_118_SEP10.indd 536 11/08/2010 16:03:44
20 Macmillan Publishers Limited. All rights reserved 10
NATURE REVIEWS | RHEUMATOLOGY VOLUME 6 | SEPTEMBER 2010 | 537
65. Robinson, C. P. et al. Characterization of the
changing lymphocyte populations and cytokine
expression in the exocrine tissues of
autoimmune NOD mice. Autoimmunity 27,
2944 (1998).
66. Robinson, C. P. et al. Infiltrating lymphocyte
populations and cytokine production in the
salivary and lacrimal glands of autoimmune NOD
mice. Adv. Exp. Med. Biol. 438, 493497 (1998).
67. Kolkowski, E. C. et al. T
H
1 predominance and
perforin expression in minor salivary glands from
patients with primary Sjgrens syndrome.
J. Autoimmun. 13, 155162 (1999).
68. Mitsias, D. I. et al. The T
H
1/T
H
2 cytokine balance
changes with the progress of the
immunopathological lesion of Sjogrens
syndrome. Clin. Exp. Immunol. 128, 562568
(2002).
69. Nguyen, C. Q., Hu, M. H., Li, Y., Stewart, C. &
Peck, A. B. Salivary gland tissue expression of
interleukin-23 and interleukin-17 in Sjgrens
syndrome: findings in humans and mice.
Arthritis Rheum. 58, 734743 (2008).
70. Bettelli, E., Korn, T., Oukka, M. & Kuchroo, V. K.
Induction and effector functions of T
H
17 cells.
Nature 453, 10511057 (2008).
71. Espinosa, A. et al. Loss of the lupus autoantigen
Ro52/Trim21 induces tissue inflammation and
systemic autoimmunity by disregulating the
IL-23T
H
17 pathway. J. Exp. Med. 206,
16611671 (2009).
72. Katsifis, G. E., Rekka, S., Moutsopoulos, N. M.,
Pillemer, S. & Wahl, S. M. Systemic and local
interleukin 17 and linked cytokines associated
with Sjgrens syndrome immunopathogenesis.
Am. J. Pathol. 175, 11671177 (2009).
73. Christodoulou, M. I., Kapsogeorgou, E. K.,
Moutsopoulos, N. M. & Moutsopoulos, H. M.
Foxp3
+
T-regulatory cells in Sjgrens syndrome:
correlation with the grade of the autoimmune
lesion and certain adverse prognostic factors.
Am. J. Pathol. 173, 13891396 (2008).
74. Christodoulou, M. I., Kapsogeorgou, E. K. &
Moutsopoulos, H. M. Characteristics of the
minor salivary gland infiltrates in Sjgrens
syndrome. J. Autoimmun. 34, 400407 (2010).
75. Zintzaras, E., Voulgarelis, M. &
Moutsopoulos, H. M. The risk of lymphoma
development in autoimmune diseases: a meta-
analysis. Arch. Intern. Med. 165, 23372344
(2005).
76. Fox, R. I. Sjgrens syndrome. Lancet 366,
321331 (2005).
77. Salomonsson, S. et al. Cellular basis of ectopic
germinal center formation and autoantibody
production in the target organ of patients with
Sjgrens syndrome. Arthritis Rheum. 48,
31873201 (2003).
78. Hansen, A., Lipsky, P. E. & Drner, T. B cells in
Sjgrens syndrome: indications for disturbed
selection and differentiation in ectopic lymphoid
tissue. Arthritis Res. Ther. 9, 218 (2007).
79. Jonsson, M. V., Skarstein, K., Jonsson, R. &
Brun, J. G. Serological implications of germinal
center-like structures in primary Sjgrens
syndrome. J. Rheumatol. 34, 20442049
(2007).
80. Le Pottier, L. et al. Ectopic germinal centers are
rare in Sjgrens syndrome salivary glands and
do not exclude autoreactive B cells. J. Immunol.
182, 35403547 (2009).
81. Szodoray, P. et al. Distinct profiles of Sjgrens
syndrome patients with ectopic salivary gland
germinal centers revealed by serum cytokines
and BAFF. Clin. Immunol. 117, 168176 (2005).
82. Daridon, C. et al. Aberrant expression of BAFF by
B lymphocytes infiltrating the salivary glands of
patients with primary Sjgrens syndrome.
Arthritis Rheum. 56, 11341144 (2007).
83. Sutherland, A. P., Mackay, F. & Mackay, C. R.
Targeting BAFF: immunomodulation for
autoimmune diseases and lymphomas.
Pharmacol. Ther. 112, 774786 (2006).
84. Mariette, X. et al. The level of BLyS (BAFF)
correlates with the titre of autoantibodies in
human Sjgrens syndrome. Ann. Rheum. Dis.
62, 168171 (2003).
85. Groom, J. et al. Association of BAFF/BLyS
overexpression and altered B cell differentiation
with Sjgrens syndrome. J. Clin. Invest. 109,
5968 (2002).
86. Cheema, G. S., Roschke, V., Hilbert, D. M. &
Stohl, W. Elevated serum B lymphocyte
stimulator levels in patients with systemic
immune-based rheumatic diseases. Arthritis
Rheum. 44, 13131319 (2001).
87. Sellam, J. et al. Decreased B cell activating
factor receptor expression on peripheral
lymphocytes associated with increased disease
activity in primary Sjgrens syndrome and
systemic lupus erythematosus. Ann. Rheum. Dis.
66, 790797 (2007).
88. Jacobi, A. M. et al. Correlation between
circulating CD27
high
plasma cells and disease
activity in patients with systemic lupus
erythematosus. Arthritis Rheum. 48,
13321342 (2003).
89. Hansen, A. et al. Diminished peripheral blood
memory B cells and accumulation of memory
B cells in the salivary glands of patients with
Sjgrens syndrome. Arthritis Rheum. 46,
21602171 (2002).
90. DiGiuseppe, J. A., Corio, R. L. & Westra, W. H.
Lymphoid infiltrates of the salivary glands:
pathology, biology and clinical significance. Curr.
Opin. Oncol. 8, 232237 (1996).
91. Hansen, A., Lipsky, P. E. & Drner, T. B-cell
lymphoproliferation in chronic inflammatory
rheumatic diseases. Nat. Clin. Pract. Rheumatol.
3, 561569 (2007).
92. Tapinos, N. I., Polihronis, M. &
Moutsopoulos, H. M. Lymphoma development
in Sjgrens syndrome: novel p53 mutations.
Arthritis Rheum. 42, 14661472 (1999).
93. Kassan, S. S. et al. Increased risk of lymphoma
in sicca syndrome. Ann. Inter. Med. 89, 888892
(1978).
94. Baimpa, E., Dahabreh, I. J., Voulgarelis, M. &
Moutsopoulos, H. M. Hematologic
manifestations and predictors of lymphoma
development in primary Sjgren syndrome:
clinical and pathophysiologic aspects. Medicine
(Baltimore) 88, 284293 (2009).
95. Mariette, X. Lymphomas complicating Sjgrens
syndrome and hepatitis C virus infection may
share a common pathogenesis: chronic
stimulation of rheumatoid factor B cells. Ann.
Rheum. Dis. 60, 10071010 (2001).
96. Anderson, L. G. & Talal, N. The spectrum of
benign to malignant lymphoproliferation in
Sjogrens syndrome. Clin. Exp. Immunol. 10,
199221 (1972).
97. Anaya, J. M., McGuff, H. S., Banks, P. M. &
Talal, N. Clinicopathological factors relating
malignant lymphoma with Sjogrens syndrome.
Semin. Arthritis Rheum. 25, 337346 (1996).
98. Valesini, G. et al. Differential risk of non-
Hodgkins lymphoma in Italian patients with
primary Sjogrens syndrome. J. Rheumatol. 24,
23762380 (1997).
99. Theander, E. et al. Lymphoma and other
malignancies in primary Sjogrens syndrome:
A cohort study on cancer incidence and
lymphoma predictors. Ann. Rheum. Dis. 65,
796803 (2006).
100. Voulgarelis, M., Tzioufas, A. G. &
Moutsopoulos, H. M. Mortality in Sjgrens
syndrome. Clin. Exp. Rheumatol. 26
(5 Suppl. 51), S66S71 (2008).
101. Theander, E., Manthorpe, R. & Jacobsson, L. T.
Mortality and causes of death in primary
Sjgrens syndrome: a prospective cohort study.
Arthritis Rheum. 50, 12621269 (2004).
102. Alamanos, Y. et al. Epidemiology of primary
Sjgrens syndrome in north-west Greece,
19822003. Rheumatology (Oxford) 45,
187191 (2006).
103. Brito-Zern, P., Ramos-Casals, M., Bove, A.,
Sentis, J. & Font, J. Predicting adverse outcomes
in primary Sjogrens syndrome: identification of
prognostic factors. Rheumatology (Oxford) 46,
13591362 (2007).
104. Ramos-Casals, M. et al. Hypocomplementaemia
as an immunological marker of morbidity and
mortality in patients with primary Sjogrens
syndrome. Rheumatology (Oxford) 44, 8994
(2005).
105. Martens, P. B., Pillemer, S. R., Jacobsson, L. T.,
OFallon, W. M. & Matteson, E. L. Survivorship in
a population based cohort of patients with
Sjgrens syndrome, 19761992. J. Rheumatol.
26, 12961300 (1999).
106. Pertovaara, M., Pukkala, E., Laippala, P.,
Miettinen, A. & Pasternack, A. A longitudinal
cohort study of Finnish patients with primary
Sjgrens syndrome: clinical, immunological, and
epidemiological aspects. Ann. Rheum. Dis. 60,
467472 (2001).
107. Scalzi, L. V., Ballou, S. P., Park, J. Y., Redline, S. &
Kirchner, H. L. Cardiovascular disease risk
awareness in systemic lupus erythematosus
patients. Arthritis Rheum. 58, 14581464
(2008).
108. Vaudo, G. et al. Precocious intimamedia
thickening in patients with primary Sjgrens
syndrome. Arthritis Rheum. 52, 38903897
(2005).
Acknowledgments
We would like to thank Professor H. M. Moutsopoulos
for his inspiration and guidance.
Author contributions
M. Voulgarelis researched the data for the article,
provided a substantial contribution to the discussion of
content and wrote the article. A. G. Tzioufas reviewed
and edited the manuscript before submission.
REVIEWS
nrrheum_118_SEP10.indd 537 11/08/2010 16:03:44
20 Macmillan Publishers Limited. All rights reserved 10
Das könnte Ihnen auch gefallen
- Sindrome de SjogrenDokument8 SeitenSindrome de SjogrenDaniel IparraguirreNoch keine Bewertungen
- Semana 9 - Lupus PDFDokument12 SeitenSemana 9 - Lupus PDFSheyla Osorio RamosNoch keine Bewertungen
- Semana 9 - Lupus PDFDokument12 SeitenSemana 9 - Lupus PDFSheyla Osorio RamosNoch keine Bewertungen
- Lecture-3.3.6-Systemic Autoimmune Diseases With Examples-2Dokument3 SeitenLecture-3.3.6-Systemic Autoimmune Diseases With Examples-2aditya sahuNoch keine Bewertungen
- 2020-Autoimmunity and Organ Damage in SLEDokument24 Seiten2020-Autoimmunity and Organ Damage in SLECinantya Meyta SariNoch keine Bewertungen
- Sjögren's Syndrome: The Proteomic ApproachesDokument21 SeitenSjögren's Syndrome: The Proteomic Approacheskj185Noch keine Bewertungen
- Infections in SLEDokument19 SeitenInfections in SLEvincentmarinasNoch keine Bewertungen
- ANA TestDokument9 SeitenANA TestNena_mileyNoch keine Bewertungen
- Streptococcus Group A InfectionsDokument13 SeitenStreptococcus Group A InfectionsLidia GotoYourhappyplaceNoch keine Bewertungen
- NEL243403R03 Karasek Lewinski WRDokument6 SeitenNEL243403R03 Karasek Lewinski WRdebby claudiNoch keine Bewertungen
- Viral Genome MutationsDokument4 SeitenViral Genome Mutationsanindhita anestyaNoch keine Bewertungen
- Expression of Estrogen and Progesterone Receptors and Ki-67 Antigen in Graves' Disease and Nodular GoiterDokument6 SeitenExpression of Estrogen and Progesterone Receptors and Ki-67 Antigen in Graves' Disease and Nodular Goiteryenny handayani sihiteNoch keine Bewertungen
- Negrini2021 Article SjögrenSSyndromeASystemicAutoiDokument17 SeitenNegrini2021 Article SjögrenSSyndromeASystemicAutoiSahanaNoch keine Bewertungen
- Sle 3Dokument8 SeitenSle 3Dianu GutiérrezNoch keine Bewertungen
- BAYETTO Et Al, 2010Dokument9 SeitenBAYETTO Et Al, 2010DouglasNoch keine Bewertungen
- Patogenesis Del Síndrome de SjogrenDokument8 SeitenPatogenesis Del Síndrome de SjogrenRivera Cervantes Osiris MargaritaNoch keine Bewertungen
- Lymphohistiocytosis: Continuing Education ActivityDokument7 SeitenLymphohistiocytosis: Continuing Education ActivitySyeda F AmbreenNoch keine Bewertungen
- Final Hoo Gen MsDokument21 SeitenFinal Hoo Gen MsbadrusharryNoch keine Bewertungen
- Peran Pola Hidup Dan Faktor Lingkungan Dalam Patogenesis Penyakit AutoimunDokument7 SeitenPeran Pola Hidup Dan Faktor Lingkungan Dalam Patogenesis Penyakit AutoimunShevamykolayovychshevchenko MilaniztyonlymilanelloNoch keine Bewertungen
- Eosinophilia in Rheumatologic Vascular Disorders CNADokument24 SeitenEosinophilia in Rheumatologic Vascular Disorders CNAReyner LeonNoch keine Bewertungen
- Lupus FisiopatoDokument9 SeitenLupus FisiopatoFernando Re TaNoch keine Bewertungen
- Influence of AgingDokument16 SeitenInfluence of AgingSCIH HFCPNoch keine Bewertungen
- High Prevalence of Altered Immunological Biomarkers in A TransgenderDokument5 SeitenHigh Prevalence of Altered Immunological Biomarkers in A TransgenderVallejo Romo Alberto CristianNoch keine Bewertungen
- Eda JurnalDokument13 SeitenEda JurnalekalapaleloNoch keine Bewertungen
- Peran Imunitas Humoral Pada Penyakit Systemic LupuDokument12 SeitenPeran Imunitas Humoral Pada Penyakit Systemic LupukyoriellstudioNoch keine Bewertungen
- Harrus 1999Dokument5 SeitenHarrus 1999Paula Andrea Castro MartinezNoch keine Bewertungen
- An Update On Diet and Nutritional Factors in Systemic Lupus Erythematosus ManagementDokument20 SeitenAn Update On Diet and Nutritional Factors in Systemic Lupus Erythematosus ManagementnellieauthorNoch keine Bewertungen
- Pathogenesis Psoriasis Update 2017Dokument2 SeitenPathogenesis Psoriasis Update 2017eby_3tamaNoch keine Bewertungen
- Gotsch F, Sindrome de Respuesta Inflamatoria Fetal, COG 2007 PDFDokument32 SeitenGotsch F, Sindrome de Respuesta Inflamatoria Fetal, COG 2007 PDFVictor AyalaNoch keine Bewertungen
- Harrison SLEDokument11 SeitenHarrison SLEpazucenaNoch keine Bewertungen
- J Clin Pathol 2003 Mok 481 90Dokument11 SeitenJ Clin Pathol 2003 Mok 481 90Divika ShilvanaNoch keine Bewertungen
- 1 s2.0 S0749070421001019 MainDokument17 Seiten1 s2.0 S0749070421001019 MainEliseu AmaralNoch keine Bewertungen
- J Immunol 2011 Villanueva 538 52Dokument16 SeitenJ Immunol 2011 Villanueva 538 52Wayan Nico Fajar GNoch keine Bewertungen
- Sex-Based Differences AutoinmunityDokument8 SeitenSex-Based Differences AutoinmunityVallejo Romo Alberto CristianNoch keine Bewertungen
- Inducible Proteopathies: Lary C. Walker, Harry Levine Iii, Mark P. Mattson and Mathias JuckerDokument6 SeitenInducible Proteopathies: Lary C. Walker, Harry Levine Iii, Mark P. Mattson and Mathias JuckerFatima Herranz TrilloNoch keine Bewertungen
- The Pathogenesis of Graves' Disease: Bryan Mciver, MBCHB, and John C. MorrisDokument17 SeitenThe Pathogenesis of Graves' Disease: Bryan Mciver, MBCHB, and John C. MorrisSOPHIASTIA KUSBIANTI MHS 2017Noch keine Bewertungen
- Infection-Genetics Relationship in Systemic Lupus ErythematosusDokument8 SeitenInfection-Genetics Relationship in Systemic Lupus ErythematosusegonzalesrnNoch keine Bewertungen
- Multiple Sclerosis: Genetic Factors, Risk and PrevalenceDokument3 SeitenMultiple Sclerosis: Genetic Factors, Risk and PrevalenceGusti TettaNoch keine Bewertungen
- Arch Dis Child 1998 Ladhani 85 8Dokument5 SeitenArch Dis Child 1998 Ladhani 85 8Dian Ayu Permata SandiNoch keine Bewertungen
- An Update On Diet and Nutritional Factors in Systemic Lupus Erythematosus ManagementDokument20 SeitenAn Update On Diet and Nutritional Factors in Systemic Lupus Erythematosus ManagementDaniela Constanta SirbuNoch keine Bewertungen
- Sex Differences in Immune ResponsesDokument3 SeitenSex Differences in Immune ResponsestriNoch keine Bewertungen
- Pathogenesis of Systemic Lupus Erythematosus: ReviewDokument11 SeitenPathogenesis of Systemic Lupus Erythematosus: ReviewDaniela HernándezNoch keine Bewertungen
- 37 Aup EtalDokument8 Seiten37 Aup EtaleditorijmrhsNoch keine Bewertungen
- Infeccion y Lupus 2015Dokument13 SeitenInfeccion y Lupus 2015Vico EdieNoch keine Bewertungen
- Virulens Factor of S PyogenesDokument8 SeitenVirulens Factor of S Pyogeneszanetamanda20Noch keine Bewertungen
- Cryoglobulinemia: Dr. Luthfi Ahmad Dr. Suriani Alimudin, SP - PD, K-AIDokument16 SeitenCryoglobulinemia: Dr. Luthfi Ahmad Dr. Suriani Alimudin, SP - PD, K-AILuthfi Ziad AhmadNoch keine Bewertungen
- Raith Julia Mef Diplomski Rad 2021Dokument37 SeitenRaith Julia Mef Diplomski Rad 2021s.ullah janNoch keine Bewertungen
- REFERAT Sindrom NefrotikDokument39 SeitenREFERAT Sindrom Nefrotikwinda ameliaNoch keine Bewertungen
- Sle Clinical CaseDokument3 SeitenSle Clinical Caselina pinedaNoch keine Bewertungen
- Pathogenesis of Dengue Haemorrhagic Fever and Its Impact On Case ManagementDokument7 SeitenPathogenesis of Dengue Haemorrhagic Fever and Its Impact On Case ManagementMank BayuNoch keine Bewertungen
- Epidemiology and Clinical Features of Multiple Sclerosis in Adults Uptodate3Dokument11 SeitenEpidemiology and Clinical Features of Multiple Sclerosis in Adults Uptodate3Régulo RafaelNoch keine Bewertungen
- Sepsis: Definition, Epidemiology, and Diagnosis: Clinical ReviewDokument5 SeitenSepsis: Definition, Epidemiology, and Diagnosis: Clinical ReviewhfathiardiNoch keine Bewertungen
- Advances in Understanding The Pathogenesis of HLH: ReviewDokument14 SeitenAdvances in Understanding The Pathogenesis of HLH: Reviewizwan taufikNoch keine Bewertungen
- Rheumatoid Arthritis: Andrew P. CopeDokument15 SeitenRheumatoid Arthritis: Andrew P. CopesamNoch keine Bewertungen
- Eosinofilia en Trastornos Reumatologicos VascularesDokument24 SeitenEosinofilia en Trastornos Reumatologicos VascularesSaidNoch keine Bewertungen
- Lupus Research PaperDokument5 SeitenLupus Research Paperttdqgsbnd100% (3)
- Staphylococcus Aureus and Hyper-IgE SyndromeDokument12 SeitenStaphylococcus Aureus and Hyper-IgE SyndromeWalid AissaNoch keine Bewertungen
- Discipline: B. Tech (Biotech) Module: BT 501 IV Semester: VDokument6 SeitenDiscipline: B. Tech (Biotech) Module: BT 501 IV Semester: VsauravsarkarNoch keine Bewertungen
- Diagnosis and Management of Autoimmune Hepatitis: A Clinical GuideVon EverandDiagnosis and Management of Autoimmune Hepatitis: A Clinical GuideMark W. RussoNoch keine Bewertungen
- Auto-Inflammatory Syndromes: Pathophysiology, Diagnosis, and ManagementVon EverandAuto-Inflammatory Syndromes: Pathophysiology, Diagnosis, and ManagementPetros EfthimiouNoch keine Bewertungen
- Mechanisms of Salivary Gland Secretory Dysfunction in Sjögren's SyndromeDokument23 SeitenMechanisms of Salivary Gland Secretory Dysfunction in Sjögren's SyndromeSiti Harwati DesrimelinaNoch keine Bewertungen
- 3Dokument7 Seiten3Siti Harwati DesrimelinaNoch keine Bewertungen
- Hpodontia Maloklusi 2Dokument7 SeitenHpodontia Maloklusi 2Siti Harwati DesrimelinaNoch keine Bewertungen
- Black and Green Tea: How Do They Differ?Dokument9 SeitenBlack and Green Tea: How Do They Differ?Siti Harwati DesrimelinaNoch keine Bewertungen
- Hipodontia Maloklusi 3Dokument4 SeitenHipodontia Maloklusi 3Siti Harwati DesrimelinaNoch keine Bewertungen
- KlasifikasiDokument3 SeitenKlasifikasiSiti Harwati DesrimelinaNoch keine Bewertungen
- 1 PBDokument5 Seiten1 PBSiti Harwati DesrimelinaNoch keine Bewertungen
- Oral Health EGCG Acid ProductionDokument6 SeitenOral Health EGCG Acid ProductionHamid OkNoch keine Bewertungen
- Kelainan Kelenjar Air LudahDokument8 SeitenKelainan Kelenjar Air LudahPRHSTNoch keine Bewertungen
- Artigo EndoxDokument6 SeitenArtigo EndoxSiti Harwati DesrimelinaNoch keine Bewertungen
- Black and Green Tea: How Do They Differ?Dokument9 SeitenBlack and Green Tea: How Do They Differ?Siti Harwati DesrimelinaNoch keine Bewertungen
- Jurnal Periodonsia Merokok Terhadap Tanggalnya GigiDokument15 SeitenJurnal Periodonsia Merokok Terhadap Tanggalnya GigiSiti Harwati DesrimelinaNoch keine Bewertungen
- Immunological Differences and Similarities Between Chronic Periodontitis and Aggressive PeriodontitisDokument13 SeitenImmunological Differences and Similarities Between Chronic Periodontitis and Aggressive PeriodontitisSiti Harwati DesrimelinaNoch keine Bewertungen
- 1Dokument7 Seiten1Siti Harwati DesrimelinaNoch keine Bewertungen
- Piper NingrumDokument5 SeitenPiper NingrumSiti Harwati DesrimelinaNoch keine Bewertungen
- Immunological Differences and Similarities Between Chronic Periodontitis and Aggressive PeriodontitisDokument13 SeitenImmunological Differences and Similarities Between Chronic Periodontitis and Aggressive PeriodontitisSiti Harwati DesrimelinaNoch keine Bewertungen
- Siti Harwati Desrimelina 04121004017Dokument5 SeitenSiti Harwati Desrimelina 04121004017Siti Harwati DesrimelinaNoch keine Bewertungen
- Daun Kaca PiringDokument5 SeitenDaun Kaca PiringSiti Harwati DesrimelinaNoch keine Bewertungen
- 127Dokument8 Seiten127Siti Harwati DesrimelinaNoch keine Bewertungen
- NederiDokument5 SeitenNederiBramita Beta ArnandaNoch keine Bewertungen
- Antibacterial Activity of Glycyrrhiza Glabra Against Oral Pathogens: An in Vitro StudyDokument7 SeitenAntibacterial Activity of Glycyrrhiza Glabra Against Oral Pathogens: An in Vitro StudyNadya PurwantyNoch keine Bewertungen
- Elements Released From Dental Casting Alloys and Their Cytotoxic EffectsDokument6 SeitenElements Released From Dental Casting Alloys and Their Cytotoxic EffectsSiti Harwati DesrimelinaNoch keine Bewertungen
- (2004 Jan) Evaluation of Antiplaque Activity of Azadirachta Indica Leaf Extract Gel - A 6-Week Clinical Study - JEP, 90 (1), 99-103Dokument5 Seiten(2004 Jan) Evaluation of Antiplaque Activity of Azadirachta Indica Leaf Extract Gel - A 6-Week Clinical Study - JEP, 90 (1), 99-103Siti Harwati DesrimelinaNoch keine Bewertungen
- 58 347 1 PBDokument4 Seiten58 347 1 PBSiti Harwati DesrimelinaNoch keine Bewertungen
- ITMKGDokument5 SeitenITMKGSiti Harwati DesrimelinaNoch keine Bewertungen
- ITMKGDokument5 SeitenITMKGSiti Harwati DesrimelinaNoch keine Bewertungen
- Siti Harwati Desrimelina 04121004017Dokument5 SeitenSiti Harwati Desrimelina 04121004017Siti Harwati DesrimelinaNoch keine Bewertungen
- Sengketa Medik Dan Konflik EtikolegalDokument23 SeitenSengketa Medik Dan Konflik EtikolegalYuda LutfiadiNoch keine Bewertungen
- Critical Thinking 1Dokument15 SeitenCritical Thinking 1Siti Harwati DesrimelinaNoch keine Bewertungen
- Easypep-A New Simplified and Optimized Workflow For Ms Sample PreparationDokument1 SeiteEasypep-A New Simplified and Optimized Workflow For Ms Sample PreparationkarthikNoch keine Bewertungen
- 9th Grade Biology SyllabusDokument4 Seiten9th Grade Biology Syllabusapi-265724193Noch keine Bewertungen
- Graviola1 Triamazon, AntiCancer, InglesDokument2 SeitenGraviola1 Triamazon, AntiCancer, InglesManuel SierraNoch keine Bewertungen
- Mycobacteria Protocols 2021 PDFDokument734 SeitenMycobacteria Protocols 2021 PDFSunny JNoch keine Bewertungen
- Tutorial PDFDokument339 SeitenTutorial PDFJeanneth MosqueraNoch keine Bewertungen
- TellmeGen Interpretation ManualDokument22 SeitenTellmeGen Interpretation Manualhello goodbyeNoch keine Bewertungen
- J. Cumagun Plant PathologyDokument374 SeitenJ. Cumagun Plant PathologyCarlos Mauricio Rivera Lozano100% (1)
- Student Exploration: Digestive SystemDokument4 SeitenStudent Exploration: Digestive SystemNO POGGEGRNoch keine Bewertungen
- NCM 112 MW NotesDokument6 SeitenNCM 112 MW NotesJames Kristopher RebayaNoch keine Bewertungen
- Virology SummaryDokument3 SeitenVirology SummaryvictorNoch keine Bewertungen
- Osmosis LabDokument12 SeitenOsmosis Labapi-319060025Noch keine Bewertungen
- Inbde Knowledge Gen DentistDokument12 SeitenInbde Knowledge Gen DentistMubashir SheriffNoch keine Bewertungen
- Hynes 2016Dokument30 SeitenHynes 2016Ester LopezNoch keine Bewertungen
- Restriction EnzymeDokument28 SeitenRestriction Enzymeanon_173640290Noch keine Bewertungen
- Full Download Test Bank For Biology of Humans Concepts Applications and Issues 5th Edition Goodenough PDF Full ChapterDokument36 SeitenFull Download Test Bank For Biology of Humans Concepts Applications and Issues 5th Edition Goodenough PDF Full Chapterplagate.fanega.872zlw100% (15)
- Biology Ncert Revision-BiomoleculesDokument12 SeitenBiology Ncert Revision-BiomoleculesRITANKAR dASNoch keine Bewertungen
- Neural TubeDokument4 SeitenNeural TubeRuth Danielle GasconNoch keine Bewertungen
- Fracture Healing: Fauziarti Azimah - 1940312128 Preceptor: Dr. Rizki Rahmadian, Sp. OT (K), M. KesDokument17 SeitenFracture Healing: Fauziarti Azimah - 1940312128 Preceptor: Dr. Rizki Rahmadian, Sp. OT (K), M. KesZakia AmeliaNoch keine Bewertungen
- Disinfectant Efficacy Study Final Amal AdelDokument47 SeitenDisinfectant Efficacy Study Final Amal AdelYUSSIF MOHAMED ABDELRAOUFNoch keine Bewertungen
- Malaria JournalDokument8 SeitenMalaria JournalArmaina TanjungNoch keine Bewertungen
- Parts of Prokaryotic & Eukaryotic CellsDokument7 SeitenParts of Prokaryotic & Eukaryotic CellsRose Yan JiNoch keine Bewertungen
- Annelid ADokument52 SeitenAnnelid AMohammad Sharifuddin SallehNoch keine Bewertungen
- Soil Microbiology PTTDokument35 SeitenSoil Microbiology PTTZainab RBNoch keine Bewertungen
- Plant Transport Multiple Choice Qs PDFDokument7 SeitenPlant Transport Multiple Choice Qs PDFMathula MuhundanNoch keine Bewertungen
- Crandall, B.C. (Ed.) - NanotechnologyDokument216 SeitenCrandall, B.C. (Ed.) - Nanotechnologyjacobi84Noch keine Bewertungen
- فطريات بشكل عامDokument149 Seitenفطريات بشكل عامdhurgham alfarrajiNoch keine Bewertungen
- In Vivo Stem Cell Based UrotherapyDokument18 SeitenIn Vivo Stem Cell Based UrotherapyMarkMadMunkiNoch keine Bewertungen
- JP Publication PDFDokument5 SeitenJP Publication PDFJayaprakashvelNoch keine Bewertungen
- Hea 1 PERSONAL AND COMMUNITY HEALTHDokument4 SeitenHea 1 PERSONAL AND COMMUNITY HEALTHvaneknekNoch keine Bewertungen
- 3 Agarose Gel Electrophoresis & Ames TestDokument4 Seiten3 Agarose Gel Electrophoresis & Ames TestNurulNoch keine Bewertungen