Beruflich Dokumente
Kultur Dokumente
Treating Facial Acne in Adolescents and Young Adults With Auriculoacupuncture and Auriculotherapy
Hochgeladen von
Pedro MaiaOriginalbeschreibung:
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Treating Facial Acne in Adolescents and Young Adults With Auriculoacupuncture and Auriculotherapy
Hochgeladen von
Pedro MaiaCopyright:
Verfügbare Formate
Medical Acupuncture. Vol. 16, No.
1
Treating Facial Acne In Adolescents And Young Adults With
Auriculoacupuncture And Auriculotherapy: A Pilot Study
Denise McKee, MD, Kay Oring, PhD, Immaculada Aban, PhD, Marcia Lu, MD,
Kathleen Peele, RN, Barbara Scott, mph
ABSTRACT
Background Potential advantages of using auriculoacupuncture or
auriculotherapy to treat facial acne vulgaris include reduced cost of therapy, lack of
significant adverse effects, and better patient adherence and acceptance.
Objective To examine the efficacy of using auriculoacupuncture and
auriculotherapy for 20 weeks to treat acne in teenagers and young adults.
Design, Setting, and Patients Male and female volunteers (aged 13-25 years)
with grade I or II mild to moderate nonscarring facial acne were randomized to 1 of
4 groups: treatment needle (TN), control needle (CN), treatment electrical (TE), or
control electrical (CE). Bilateral auricular points used for the 2 treatment groups
(TN and TE) were Face Point, Skin Disorder Point F, Genital Control Point, Lung 1,
Lung 2, Point Zero, Shen Men, Allergy Point, and Endocrine Point. Nine sham
points on the fleshy portion of the auricular ridge were used for CN and CE groups.
Main Outcome Measure Papule count change from baseline.
Results On average, baseline papule counts of males (range, 32-50) were larger
than those of females (range,12-18). The mean changes in papules for males were
relatively greater. For females, the CN group had the highest mean baseline count
and showed worsening over time as evidenced by an increase in the mean count
over time, and mean change values generally below zero, i.e., counts were more
than baseline. The other 3 groups continuously improved as shown by the
downward trend in the mean papule counts, with the TN group showing the most
improvement followed by the CE group. For males, all treatment groups showed
improvement over time. The CE and TN groups had the highest baseline counts,
but the CE group showed more improvement than did the TN. The CN group had
the lowest mean count at the end of the study, but it also had the lowest baseline
count. The TE group had a baseline count slightly lower than that of CE and TN,
but finished with the most improvement.
Conclusions Both auriculoacupuncture and auriculotherapy appear to provide
some promising therapeutic results in the treatment of adolescent mild to moderate
acne vulgaris. Differences observed in therapeutic effect of the electrical
stimulation vs needle stimulation may result from differences in the amount of
energy delivered. Further study of this alternate treatment for acne is warranted.
KEY WORDS
Acupuncture, Electrical Stimulation, Alternative Medicine, Acne
INTRODUCTION
Acne vulgaris is one of the most common dermatological diseases. The prevalence
may be as high as 83%-95% in adolescents. While acne affects similar numbers
of males and females, males tend to have greater degrees of severity. A
substantial percentage of adults are also affected, either as a continuation of their
teenage acne or its first appearance in the 3rd or 4th decade. Acne is a disease of
the pilosebaceous unit, consisting of sebaceous glands and small hair follicles, and
is caused by obstruction of the pilosebaceous canal. The factors leading to acne
include sebum overproduction and bacterial infection from Propionibacterium
acnes, the organism active in inflammatory acne. Acne varies in severity from mild
(few comedones and papules) to severe (scarring, highly inflamed pustules,
nodules, i.e., acne conglobata).1-3 Acne is often dismissed as an affliction the
patient will outgrow, resulting in the postponement of treatment.
While it is true that most cases of acne subside and involute spontaneously and
completely within a few years of onset, a small percentage remains active. Acne
carries significant psychosocial implications and may cause considerable
temporary emotional distress during the acute phase of active outbreak as well as
permanent distress when facial scarring results. The psychosocial impact on
teenagers may be especially devastating. Low self-esteem, affected personal
appearance, peer taunting, and ridicule all demoralize the teen plagued with acne,
creating embarrassment and frustration. As acne is successfully treated, peer
acceptance improves, resulting in patients feeling less socially isolated.4
Accepted Western medical treatment of acne includes tretinoin, topical or oral
antibiotics, benzoyl peroxide, salicylic acid, sulfur preparations, azelaic acid,
adapalene, tazarotene, birth control pills in women, antiandrogen therapy (low-
dose corticosteroids, spironolactone), and isotretinoin as a last resort.5 While
effective in clearing acne, many of these treatments have significant adverse
effects. Tretinoin may cause photosensitivity, excessive skin dryness and cracking,
and is contraindicated in pregnancy.
Adverse effects of antibiotics include vaginal yeast infections, allergic reactions,
diarrhea, anaphylaxis, and potential for development of antibiotic resistance. Birth
control pills may cause hypertension, nausea, weight gain, migraines, depression,
and blood clots. Isotretinoin is particularly dangerous and expensive; the adverse
effects include elevated lipid profiles, hepatotoxicity, and fetal teratogenicity, thus
limiting its use in sexually active females of childbearing age. In addition, the cost
for drug therapy may be daunting, ranging from $10 per month for tetracycline to
$210 per month for isotretinoin.1,2
Given these problems with traditional treatments, patients with acne could benefit
from new therapies.6 Several studies have reported positive therapeutic effects of
auriculoacupuncture and auriculotherapy in the treatment of mild to moderate facial
acne vulgaris.7-15 The potential advantages of using auriculoacupuncture and
auriculotherapy to treat facial acne vulgaris include reduced cost of therapy, lack of
significant adverse effects, and better patient adherence and acceptance.
According to the principles of Traditional Chinese Medicine (TCM), acne vulgaris is
treated by stimulating ear points that clear heat, dispel wind and damp, cool blood,
and reduce stagnation. Metaphorical Chinese medical acupuncture logic indicates
how systemic disease can be reflected in the external ear as a self-contained
microsystem that affects the whole body.
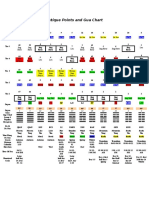
Figure 1. Treatment and Sham Points and Frequencies Used
There is now an accumulation of scientific studies examining electrophysiological
data obtained from animals and humans that provide neurohumeral support for
these clinical findings.16 Both forms of ear stimulation do not simply reduce pain or
temporarily "cure" the problem but, rather, facilitate the natural bodily healing
processes and affect deeper physiologic changes. Starwynn states that the human
body generates electrical energy that can migrate long distances through
semiconduction. Imbalances in ionic positive and negative charges are associated
with pain and injury. Thus the therapeutic effects of acupuncture are due to its
ability to discharge (locally and distally) these ionic charges.17 In traditional
Chinese therapy, skin is under the domain of influence of the Lung meridian and
therefore, auricular Lung points are logical to use in the treatment of acne vulgaris.
There are other logical reasons in selection of all the rest of the ear points in the
treatment of acne vulgaris.7 Research demonstrating release of endorphins by
stimulation of auricular acupuncture points provides a neurohumeral basis for the
clinical actions of auricular acupuncture.18
This pilot study was designed to examine the efficacy of alternative approaches to
treat mild to moderate acne in teens and young adults, using auriculoacupuncture
and auriculotherapy. Specifically, we sought to determine whether stimulation of
ear points by needles or by electrical microcurrent would be effective in 20 weekly
sessions. Specific outcomes examined included changes in number and severity of
lesions, presence of adverse effects, and duration of treatment needed to achieve
therapeutic success.
METHODS
Male and female volunteers between the ages of 13 and 25 years with mild to
moderate facial acne were recruited using a variety of methods, including fliers
posted around campus, articles in campus and local newspapers, letters and fliers
sent to community physicians, word-of-mouth, and television coverage. The
majority of subjects were recruited as a result of coverage by local print and
television media.
Criteria for inclusion in the study were grade I and II mild to moderate nonscarring
facial acne vulgaris as determined by a dermatologist blinded to the study.
Exclusion criteria were severe acne grades III and IV or any systemic acne therapy
(antibiotics, isotretinoin) or retinoid topical treatments (tretinoin) for 1 month prior to
the beginning of the study. Different acne grading systems have been used in
clinical studies for evaluation of acne treatment. For the purpose of this study, an
acne grading system using photographic standards was used in which overall acne
was evaluated on a 0 to 8 scale anchored to photographic standards that illustrate
grades 0, 2, 6, and 8. Experience with use of this system in large-scale clinical
trials has shown to be useful and reliable.20
The study was reviewed and approved by the institutional review board of the
University of Nevada, Reno. Potential study volunteers who were younger than 18
years were required to have a parent or guardian present during the orientation to
the study and review of the study protocol, risks, and benefits. Parents/guardians
were required to sign the informed consent for these younger volunteers, and the
teenager was required to sign a "teen" assent form. Volunteers between 18-25
years of age signed their own consent forms.
Subjects were informed that they would be required to present to the Family
Medicine Center once weekly for 20 weeks for about 30 minutes each time to
receive their treatment, discuss any concerns with the physician, and have 3
photographs (front and each side) taken of their face. Possible adverse effects or
risks to the patient of auriculoacupuncture and auriculotherapy (tenderness,
inflammation, bleeding, or infection in the ear, feelings of drowsiness, euphoria,
relaxation or sedation after a treatment period) were reviewed with each potential
volunteer. Rotchford's "Clinical Strategies for Reducing Adverse Events" were
followed.19 (For this study, the most expected adverse effect of drowsiness was
addressed by having the subjects wait 30 minutes after the 1st treatment before
driving a car, and advising them to be driven to the 1st treatment. Any subject who
experienced drowsiness after the 1st treatment was monitored thereafter at every
visit.). If, at the end of the study, control group participants desired to have
conventional or alternative therapy, it was provided free of charge for up to 20
weekly sessions.
After giving written informed consent, each subject was randomized to 1 of 4
groups and not informed of the assignment to treatment or control group:
1. treatment needle (TN) (auriculoacupuncture)
2. control needle (CN) (auriculoacupuncture)
3. treatment electrical (TE) (auriculotherapy)
4. control electrical (CE) (auriculotherapy).
Prior to beginning the study, the physicians (McKee and Lu) met with each
volunteer to take a health history and perform a limited physical examination. Initial
numbers of facial lesions were scored by an objective grading method using
photographic standards.20 Participants were asked not to use conventional
therapies such as tretinoin, isotretinoin, or antibiotics while enrolled in this study.
Women taking oral contraceptive pills were allowed to be in the study with the
understanding that they neither stop nor start oral contraceptives during the study.
A list of standard therapies was given to subjects, in the event they chose to drop
out of the study or not adhere to the study protocol. Use of non-prescription topical
treatments was monitored during the study.
Treatment
Nine bilateral auricular points from Oleson's Auricular Therapy manual16 used for
the 2 treatment groups (needle and electric) were: Shen Men, Allergy Point, Skin
Disorder Point F, Point Zero, Lung 1, Lung 2, Endocrine Point, Genital Control
Point, and Face Point. (Treatment points are shown by the solid black dot in Figure
1). Nine sham points (shown by the gray dot in Figure 1) were selected for the 2
control groups (needle and electric) to have no therapeutic effect.
These were located on the fleshy portion of the auricular ridge along the helix rim
of the ear, stopping before Darwin's tubercule and avoiding the allergy point. For
the needle groups, Tai Ji Acupuncture disposable needles gauge 36 were used.
For the control groups, the Electro Medical Stim Flex 400, an FDA-approved
device for auricular stimulation with ability to control noise and identify exact point
location, was used. Threshold levels in ohms and time current delivery were exact
and automatically controlled. Frequencies (also shown in Figure 1) were varied as
described by Oleson.
All 4 groups received 20-minute treatments in 20 weekly sessions as follows:
TN group received auriculoacupuncture in the 9 treatment points listed above,
and shown by the black dot in Figure 1.
CN group received sham acupuncture, the needling at the 9 points described
above, and shown by the gray dot in Figure 1.
TE group received auricular electrotherapy with microcurrent stimulation at
each treatment ear point as follows:
Treatment Ear Point 1 2 3 4 5 6 7 8 9
Duration, sec 16 8 8 8 8 8 8 8 16
Frequency, Hz 10 10 40 5 5 5 20 20 80
CE received auriculotherapy with microcurrent stimulation with electricity
applied at each sham point for the same duration and at the same
frequencies as those used for the corresponding treatment point for the TE
group (e.g., sham point #1: duration = 16 sec, frequency = 10 Hz; sham
point #2: duration = 8 sec, frequency = 10 Hz; sham point #3: duration = 8
sec, frequency = 40 Hz).
Three medical quality photographs (front, left, and right sides) were taken at each
visit with a digital camera to create a permanent record of each subject's clinical
status throughout the course of treatment that could then be re-evaluated by a
second dermatologist later if necessary. A dermatologist who was blinded to each
subject's treatment group assignment and week of treatment counted the number
of papules (small, circumscribed solid elevation of the skin) and pustules (small
elevation of the skin filled with pus), and these numbers were entered into a
database using Microsoft Excel (Microsoft, Redmond, WA).
Figure 2. Mean Papule Count and Mean Change in Papule Counts by Sex
Statistical Analysis
To test our hypotheses, the changes in the number (baseline count minus current
count) of papules and pustules were modelled, separately, over time using
repeated measures analyses. Results and conclusions of the analyses were
obtained using SAS PROC MIXED (SAS Institute Inc, Cary, NC) with an
unstructured covariance based on 5% significance level.There were several
missing values in the 1st few weeks of treatment due to missing or unreadable
photos. Some subjects did not have initial assessment photos, some subjects had
missing photos of the 1st or 2nd treatment week, and 2 of the 29 subjects had their
1st available photo only on the 3rd week of treatment. As a consequence,
"baseline count" for each subject was obtained by taking the average of all
available readings up to the 3rd treatment week. Because some subjects were
unable to appear every week and some subjects withdrew from the study before
the last treatment, these resulted in more missing data values. In order to
maximize the use of available information, "current count" for each subject was
obtained by taking the average of available data values of 2 consecutive treatment
weeks. A "time index" for the modified data that was used in the analyses was
defined to represent sequential time periods as follows:
Time Index 0 1 2 3 4 5 6 7 8 9
Treatment Week 0-3 4-5 6-7 8-9
10-
11
12-
13
14-
15
16-
17
18-
19
20
The predictor variables in the model were sex, treatment, time index (1-9), and all
2- and 3-factor interaction terms of these variables. Baseline count (i.e., count at
time index 0) was included in the model as a covariate. Time index was treated as
a categorical variable instead of a continuous variable to avoid assuming a
particular form of the mathematical relationship between mean change in counts
and time. The decision was made to use this modeling strategy even though
degrees of freedom were lost and the power of the statistical tests was lowered in
order to avoid the possibility of obtaining misleading results due to fitting an
inappropriate model.
RESULTS
A total of 29 subjects participated in the study (15 female and 14 male); 60% of the
females and 79.6% of males completed all 20 weeks of treatment. Table 1
summarizes the distribution of the subjects by their last week of treatment, sex,
and treatment group. The means and SDs of subjects' ages are shown in Table 2.
Male subjects were significantly younger on average than female subjects. We
noted that, on the average, subjects assigned to the TN group tended to be
younger relative to subjects in the other treatment groups, particularly among
females.
To better assess the possible therapeutic effects of the treatments, graphs of the
mean counts, and mean change in counts of papules and pustules per sex and
treatment group over time are presented; Figure 2 illustrates the mean and mean
change in papule counts.
On the average, baseline papule counts of male subjects (range, 32-50) were
larger than those of female subjects (range, 12-18). Consequently, the mean
changes in papules for males were relatively larger. Also, papule counts of
female subjects were less variable than those of the male subjects as indicated
by smoother curves for females.
For female subjects, the CN group had the highest mean baseline count and
showed worsening condition over time as supported by an increase in the
mean count over time, and mean change values generally below zero, i.e.,
counts were more than baseline. The other 3 groups continuously improved as
shown by the downward trend in the mean papule counts, with the TN group
showing the most improvement, since it had the highest mean change curve
over time, followed by the CE group.
For male subjects, all treatment groups showed improvement over time. The
CE and TN groups had the highest baseline counts, but the CE group showed
more improvement than did the TN group. The CN group had the lowest mean
count at the end of the study, but it also had the lowest baseline. The TE group
had a baseline count slightly lower than that of the CE and TN groups, but
finished with the most improvement as evidenced by the largest mean change
at the end of the study.
Figure 3 displays graphs of mean and mean change in pustule counts.
As in papule counts, male subjects had significantly higher baseline counts,
more variable curves, and larger changes in pustule counts on average than
did female subjects.
For females, the CN group worsened over time as shown by mean change
values below zero, although there is evidence of some improvement at Time
Index 1 and 2. The TN and CE groups worsened at first, but showed
improvement past time index 4, with the CE group showing the most
improvement, especially since it started with a relatively high mean baseline
pustule count. The TE group showed marked improvement (large positive
mean changes) early on, but decreased over time as indicated by smaller
positive mean changes and a below-zero value (i.e., worse condition relative to
baseline count) at Time Index 20.
For males, the TE group improved the most because it had the highest baseline
count and ended up with the largest mean change at the end of the study. The
CN group, which had the lowest baseline count, also improved over time. The
CE group improved early in the study but worsened toward the end, while the
TN group showed only moderate improvement over time.
Modeling the change in counts as described
in the previous section is a way to
determine if the above observations are
statistically significant or are simply due to
chance. Since baseline count could
possibly affect the amount of change in the
papule and pustule counts, this was
included as a covariate in the modeling.
Results showed significant 3-factor "sex-
treatment-time" interaction for papules
(P<.001) and pustules (P=.003). Hence,
there were significant therapeutic effects,
but these effects depended jointly on
treatment, sex, and time. As expected, it
was also found that the baseline count was
a significant covariate (P<.001). The
treatment groups were then compared with
each other to determine which group
differed from another after adjusting for the
baseline count for each time index.
Table 3 summarizes the results of these
comparisons of the treatment groups by sex
and time after adjusting for baseline counts.
No significant differences among the
treatment groups for female subjects were
observed until the 18th week of treatment.
As seen in Figure 2, the significant results
were mainly due to the CN group getting
worse while the other groups continued to
improve, particularly the CE and TN groups.
For male subjects, significant differences
were observed in the early part of the
treatment period, where the TE and CN
groups both showed significant
improvement over the CE and TN groups.
However, at the 20th week of the treatment
period, only the TE and TN groups were significantly different from each other, with
the TE subjects improving significantly compared with the TN group. The CE and
CN groups also showed improvement at the end of the treatment period as seen in
Figure 2, but these improvements were not significantly different from those of the
TN or TE groups.
On pustule counts, the CN group was significantly worse than the other groups for
females as early as treatment week 14 and continued until the end of treatment.
Conversely, there was an increasing trend in the mean change in pustule counts
for males and hence, evidence of improvement for both the CN and TE groups.
From Table 3, the improvement in the TE group was significantly higher than that
of the TN and CE groups, but not with the CN group.
The CN female group significantly worsened (papule and pustule) while the other 3
treatment groups improved. TE and CN groups appeared to indicate some positive
therapeutic effects on papule and pustule counts.
DISCUSSION
The design of this study was sound and statistical modeling was well-conducted.
Even though the sample size was small, some significant results were obtained.
Electroacupuncture using the points described appeared to provide some
promising positive therapeutic results in the treatment of adolescent mild to
moderate acne vulgaris. Differences observed in therapeutic effect of the electrical
stimulation vs needle stimulation may result from differences in amount of energy
delivered and may also warrant further investigation.
CONCLUSION
We concluded that there was positive improvement of facial acne vulgaris by
auriculoacupuncture and auriculotherapy. The results of this pilot study appear
promising, suggesting that further study of this alternate treatment for acne is
warranted. Apparent sex differences as-sociated with time to treatment
effectiveness may affect subject retention and point to a shorter time frame needed
to treat males. Although the improvement in facial acne did not always reach
statistical significance for the treatment groups, there was improvement that may
indicate clinical efficacy.
Many lessons were learned from this pilot study in this rapidly evolving field. Based
on our lessons and on advances in the field of auriculotherapy, we recommend
that future studies consider:
Recruiting a larger number of subjects
Including funds for recruitment and subject remuneration in budget request
Broadening inclusion criteria to include participants with severe acne vulgaris
Controlling more rigorously for cofactors or potential confounders such as diet
and exercise
Limiting intervention to only 1 type of treatment (electrical stimulation or
acupuncture) at a time
Considering acne in all 3 phases; and
Treating the selected active points with a multifrequency probe to allow each
point to maximally utilize the appropriate frequency for its stage.
This study used a recipe approach to point selection and took into account only 1
phase of disease process as reflected in the external ear. When disease is
considered in all 3 phases of energetic expression, this necessitates changes in
point selection and frequency of optimal electricity delivered to the ear. A
multisequence probe would deliver all frequencies to the ear in auriculotherapy,
allowing each point to only absorb the frequency that corresponded to its energetic
phase. Furthermore, because each subject has unique reasons and energetic
imbalances responsible for physical disease expression, a more individualized
study design would seem prudent if it could be adequately controlled. For example,
more accurate point scanning for electrically active points prior to needling or
probe placement to individualize the treatment may result in better outcomes, with
some points producing a specific localized effect and others producing a more
systemic effect.
Table 1. Distribution of Subjects by Last Week of
Treatment, Sex, and Treatment Group
Treatment Sex Last Week of Treatment Total
6 7 8 12 13 16 20
CN F 2 2
M 1 3 4
TN F 1 1 2 4
M 2 2
CE F 3 3
M 3 3
TE F 1 1 1 1 2 6
M 1 1 3 5
Total 1 2 3 1 1 1 20 29
Abbreviations: TN, treatment needle (auriculoacupuncture);
CN, control needle (auriculoacupuncture); TE, treatment
electrical (auriculotherapy); CE, control electrical
(auriculotherapy).
Table 2. Subjects's Ages
Age, Mean, (SD), y Treatment
Group
Female Male
CN 19(4.2) 17(1.9)
TN 16(2.1) 15(.7)
CE 21(1.5) 15(1.2)
TE 21(3.4) 16(3.6)
Table 3. Results of Comparing Treatment Groups *
Papules Pustules
Time Female Male Female Male
1 (weeks 4-5)
TE>TN (P=.04)
TE>CE (P=.01)
CN>TN (P=.02)
CN>CE (P=.005)
5 (weeks 12-13)
CN>TN (P=.02)
CN>TE (P=.04)
TE>CE (P=.03)
6 (weeks 14-15)
TE>CN (P=.01)
TN>CN (P=.02)
CE>CN(P=.01)
TE>TN (P=.03)
TE>CE (P=.001)
CN>CE (P=.02)
7 (weeks 16-17)
TE>CN (P=.001)
TN>CN (P=.003)
CE>CN (P=.002)
8 (weeks 18-19)
TE>CN (P=.04)
TN>CN (P=.03)
CE>CN (P=.03)
TE>CN (P=.04)
TN>CN (P=.03)
CE>CN (P=.03)
CN>TN (P=.008)
CN>CE (P=.008)
9 (week 20)
TE>CN (P=.02)
TN>CN (P=.003)
CE>CN (P=.009)
TE>TN (P=.04)
TE>CN (P=.008)
TN>CN (P=.003)
CE>CN (P=.001)
TE>TN (P=.02)
TE>CE (P=.002)
CN>CE (P=.01)
*Only comparisons with P<.05 were included in this table.
Further investigation is needed to determine if differences in therapeutic effect
between electrical and needle stimulation result from higher energetic input from
electrical stimulation. More studies are also needed to better understand the
apparent effectiveness of sham therapy from both electrical and needle sham
therapy. One possibility is that there may be a strong placebo effect, while it is also
possible that the points selected to be sham may actually have therapeutic effects.
On a more holistic level, this study addressed solely physical symptom
manifestation even though our being is much more complex, encompassing
spiritual, mental, emotional, and energetic parts of our vital force. We believe that
all these other aspects of our being affect the root of the disease process. It is
possible that a more complex treatment protocol taking these issues into account
would yield better results.
FUNDING/SUPPORT
We acknowledge the support of the Department of Family and Community
Medicine, and funding for a Family Medicine Clinical Research Initiative (grant
5D32HP10250-03) from the Bureau of Health Professions (HHS, HRSA).
ACKNOWLEDGEMENTS
We thank Franz Stadler, MD, for his invaluable assistance in evaluating the photos
to score the number and type of lesions; Richard Niemtzow, MD, for his expertise
and invaluable guidance in the development of the protocol for this study; and
Adrian Gammon and Heather Rainford, research assistants, for their assistance in
every aspect of the study.
REFERENCES
1. Russel J. Topical Therapy for acne. Am Fam Physician. 2000;61:357-366.
2. Habif T. A Color Guide to Diagnosis and Therapy Clinical Dermatology. St.
Louis, MO: MOsby. 1996:148-153.
3. Rossen MH, Roed-Petersen J. Acne vulgaris. Ugeskr Laeger.
1993;155:775-778.
4. Krowchuk DP, Stancin T, et al. The psychosocial effects of acne on
adolescents. Pediatr Dermatol. 1991;8:332-338.
5. Thiboutot DM. Acne: an overview of clinical research findings. Dermatol
Clin. 1997;15:97-109.
6. Helms JM. Acupuncture Energetics: A Clinical Approach for Physicians.
Berkeley, CA: Medical Acupuncture Publishers; 1995.
7. Dai G. Advances in the acupuncture treatment of acne. J Tradit Chin Med.
1997;17:65-72.
8. Huang ZM. A survey on the treatment of acne. Chung Kuo Chung Hsi I
Chieh Ho Tsa Chih. 1995;15:379-381.
9. Liu J. Treatment of adolescent acne with acupuncture. J Tradit Chin Med.
1993; 3;187-188.
10. Chen D, Jiang N, Cong X. 47 Cases of acne treated by prick-bloodletting
plus cupping. J Tradit Chin Med. 1993;3:185-186.
11. Chen K, Zhou S, Zheng Y. Clinical application of traditional auriculoacupoint
therapy. J Tradit Chin Med. 1993;13:152-154.
12. Xu Y. Treatment of facial skin diseases with acupuncture: a report of 129
cases. J Tradit Chin Med. 1990;10:22-25.
13. Xu YH. Treatment of acne with ear acupuncture: a clinical observation of 80
cases. J Tradit Chin Med. 1989;9:238-239.
14. Ding LN. 50 Cases of acne treated by puncturing acupoint Dazhui
incombination with cupping. J Tradit Chin Med. 1985;5:128.
15. Chen H. Recent studies on auriculoacupuncture and its mechanisms. J
Tradit Chin Med. 1993;13:129-143.
16. Oleson T. Auriculotherapy Manual: Chinese and Western Systems of Ear
Acupuncture. 2nd ed. Los Angeles, CA: Health Care Alternatives; 1996.
17. Starwynn D. Electrophysiology and the acupuncture system. Medical
Acupuncture. 1999/2000;11(2):25-31.
18. Oleson T. Electrophysiological research on the differential localization of
auricular acupoints. Medical Acupuncture. 1999/2000;11(2):25-31.
19. Rotchford JK. Overview: adverse effects of acupuncture. Medical
Acupuncture. 1999/2000;11(2):32-35.
20. Cook CH, Centner RL, Michaels SE. An acne grading method using
photgraphic standards. Arch Dermatol. 1979;115:571-575.
AUTHORS' INFORMATION
Dr Denise McKee is a full-time faculty member at the University of Nevada in the
Department of Family Medicine in Reno, Nevada. Dr McKee integrates medical
acupuncture with allopathic medicine, and has additional areas of special interest
in wilderness medicine and spirituality in medicine.
Denise McKee, MD*
Associate Professor
University of Nevada, Reno
School of Medicine, Dept of Family and Community Medicine
Brigham Bldg/316
Reno, NV 89557-0046
Phone: 775-747-0920 Fax: 775-327-2102 Email: mckee@med.unr.edu
Kay Oring, PhD, recently retired from clinical nutrition practice and teaching. At the
time of the study reported above, she was Associate Professor and Director of
Clinical Research in the Department of Family Medicine. Dr Oring has a special
interest in adolescent eating disorders.
Kay Oring, PhD, RD
Adjunct Professor
University of Nevada, Reno
School of Medicine, Dept of Family and Community Medicine
Brigham Bldg/316
Reno, NV 89557-0046
Phone: 775-784-6180 Fax: 775-327-2102 Email: koring@med.unr.edu
Inmaculada Aban, PhD, has been teaching mathematics and statistics at the
University of Nevada since 1995. She also provides statistical consulting services
to the faculty and students at the University of Nevada and to other agencies in
northern Nevada.
Inmaculada Aban, PhD
Associate Professor
University of Nevada, Reno
Dept of Mathematics and Statistics (084)
Reno, NV 89557
Phone: 775-784-6720 Fax: 775-784-6378 Email: aban@unr.edu
Dr Marcia Lu is a faculty member in the Department of Family Medicine, and is
Director of Medical Student Education. Dr Lu's special areas of interest are
medical education, preventive health care, gynecology, and dermatology.
Marcia Lu, MD
Assistant Professor
University of Nevada, Reno
School of Medicine, Dept of Family and Community Medicine
Brigham Bldg/316
Reno, NV 89557-0046
Phone: 775-784-6180 Fax: 775-327-2102
Email: stadlerlu@earthlink.net
Kathleen Peele, RN, is a Pediatric Nurse Practitioner who specializes in child
sexual abuse and adolescent medicine. She has a strong interest in
complementary medicine, has studied acupuncture, and is currently a student of
Homeopathy.
Kathleen Peele, RN, C-PNP
Associate Professor
University of Nevada, Reno
School of Medicine, Dept of Pediatrics/333
Reno, NV 89557-0046
Phone: 775-784-6178 Fax: 775-784-4828 Email: peele@med.unr.edu
Barbara Scott, MPH, is a Clinical Nutritionist and faculty member with a joint
appointment in Family Medicine and Pediatrics. Her areas of specialty include
adolescent nutrition, children with special needs, Ayurvedic nutrition, and
HIV/AIDS.
Barbara Scott, MPH, RD
Associate Professor, Director of Clinical Research
University of Nevada, Reno
School of Medicine, Dept of Family and Community Medicine
Brigham Bldg/316
Reno, NV 89557-0046
Phone: 775-784-6180 Fax: 775-327-2102 Email: scottbj@med.unr.edu
*Correspondence and reprint requests
http://www.medicalacupuncture.org/aama_marf/journal/vol16_1/article6.html
Das könnte Ihnen auch gefallen
- Tennis Elbow GetDokument20 SeitenTennis Elbow GetHeri DwiantoNoch keine Bewertungen
- Foot AcupunctureDokument0 SeitenFoot Acupuncturerasputin22Noch keine Bewertungen
- AuriculotherapyDokument14 SeitenAuriculotherapyapi-3769566100% (3)
- The Crossing Method of Point Selection: by DR Zhou Yu YanDokument3 SeitenThe Crossing Method of Point Selection: by DR Zhou Yu YanJose Gregorio ParraNoch keine Bewertungen
- Using Acupuncture Points To Eliminate Jet LagDokument5 SeitenUsing Acupuncture Points To Eliminate Jet Lagsale18100% (1)
- Home About Us Order Info FAQ Distributors Suppliers Feedback Contact Us View CartDokument5 SeitenHome About Us Order Info FAQ Distributors Suppliers Feedback Contact Us View CartdpscribdzoneNoch keine Bewertungen
- Test II-3.indd PDFDokument1 SeiteTest II-3.indd PDFKika HadjNoch keine Bewertungen
- (Fu Ke) Acupuncture PointDokument2 Seiten(Fu Ke) Acupuncture PointWafaa Abdel AzizNoch keine Bewertungen
- TCM Imassager Instruction Manual 2011.6Dokument24 SeitenTCM Imassager Instruction Manual 2011.6drfaizal100% (1)
- The Leg Three Miles Acupuncture PointDokument5 SeitenThe Leg Three Miles Acupuncture Pointdoktormin106Noch keine Bewertungen
- Auriculotherapy Certification in UtahDokument1 SeiteAuriculotherapy Certification in UtahricafelNoch keine Bewertungen
- Instruments: Number of Item Item Unit Price in EURODokument2 SeitenInstruments: Number of Item Item Unit Price in EUROkudum33Noch keine Bewertungen
- 15 00h Usichenko TarasDokument18 Seiten15 00h Usichenko TarasGraziele GuimaraesNoch keine Bewertungen
- WHO Standard Nomenclature of AcupunctureDokument36 SeitenWHO Standard Nomenclature of AcupunctureTiffanny Anastasy100% (1)
- 7.1 Petermann PCLACDokument11 Seiten7.1 Petermann PCLACbob marley100% (1)
- Acupuncture For The Treatment of Chronic Painful Peripheral Diabetic Neuropathy: A Long-Term StudyDokument7 SeitenAcupuncture For The Treatment of Chronic Painful Peripheral Diabetic Neuropathy: A Long-Term StudyFernanda GiulianoNoch keine Bewertungen
- A Study of The Sa-Ahm Five Element Acupuncture Theory: December 2009Dokument13 SeitenA Study of The Sa-Ahm Five Element Acupuncture Theory: December 2009dtncorreoNoch keine Bewertungen
- Cranio em InglesDokument39 SeitenCranio em InglesbrunamontenegrooNoch keine Bewertungen
- The Effect of Microcurrents On Facial WrinklesDokument9 SeitenThe Effect of Microcurrents On Facial WrinklesSofia RivaNoch keine Bewertungen
- Cheng AcupunctureforWomenwithObesity PDFDokument13 SeitenCheng AcupunctureforWomenwithObesity PDFAshari Fisio180% (1)
- 08152011-Article 0 PDFDokument2 Seiten08152011-Article 0 PDFЕвгений ТополовскийNoch keine Bewertungen
- Balance Method RevBalance Method Revolutionizes Acupunctureolutionizes AcupunctureDokument3 SeitenBalance Method RevBalance Method Revolutionizes Acupunctureolutionizes Acupuncturedrtommy75Noch keine Bewertungen
- Abdominal PalpationDokument11 SeitenAbdominal PalpationDoctora SantanaNoch keine Bewertungen
- Acupuncture Relieves Asthma AttacksDokument4 SeitenAcupuncture Relieves Asthma AttacksriezzzadityaNoch keine Bewertungen
- A Skeptical Look at The AcuGraphDokument4 SeitenA Skeptical Look at The AcuGraphhjsassoNoch keine Bewertungen
- Microsystem AcupunctureDokument3 SeitenMicrosystem AcupunctureZulfa MayiruliNoch keine Bewertungen
- PPM May08 Kneebone LaserAcupunctureDokument4 SeitenPPM May08 Kneebone LaserAcupuncturejoseNoch keine Bewertungen
- Alchemical Facial Acupuncture Protocols, Part 3: by Mary Elizabeth Wakefield, Lac, Dipl. Ac., MS, MMDokument3 SeitenAlchemical Facial Acupuncture Protocols, Part 3: by Mary Elizabeth Wakefield, Lac, Dipl. Ac., MS, MMHaryono zhuNoch keine Bewertungen
- M.E.a.D. Report ComparisonsDokument1 SeiteM.E.a.D. Report ComparisonsFaisal MadjidNoch keine Bewertungen
- Acupuncture On The Cutting Edg@Dokument10 SeitenAcupuncture On The Cutting Edg@Fra LanNoch keine Bewertungen
- Menopausal Syndrome FootDokument0 SeitenMenopausal Syndrome Footrasputin22100% (1)
- The Acupuncture Prescription:: A Holistic Approach to HealthVon EverandThe Acupuncture Prescription:: A Holistic Approach to HealthNoch keine Bewertungen
- Cutaneous Regions of the 14 Meridians MapDokument4 SeitenCutaneous Regions of the 14 Meridians MapjjseguinNoch keine Bewertungen
- Byol Meridian NewDokument2 SeitenByol Meridian NewRahulKumar0% (1)
- Auricular PointsDokument6 SeitenAuricular PointsDrnarendra KumarNoch keine Bewertungen
- Course C Basic Theories of Acupuncture and MoxibustionDokument36 SeitenCourse C Basic Theories of Acupuncture and MoxibustionGermey HoongNoch keine Bewertungen
- What Is AcupunctureDokument3 SeitenWhat Is AcupunctureSreedhar PulipatiNoch keine Bewertungen
- Babu's Notes On AcupunctureDokument14 SeitenBabu's Notes On Acupuncturemailbabu100% (1)
- Escalpo Acupuntura HemorragiaDokument9 SeitenEscalpo Acupuntura HemorragiaGraziele GuimaraesNoch keine Bewertungen
- An Acupuncture Approach to Improved Breast HealthDokument1 SeiteAn Acupuncture Approach to Improved Breast HealthmnaturaisNoch keine Bewertungen
- Tugas Farmakologi ToksikologiDokument55 SeitenTugas Farmakologi ToksikologilucyanaNoch keine Bewertungen
- Acupressure & Meridian Therapy: by Walter LastDokument10 SeitenAcupressure & Meridian Therapy: by Walter LastEstela BenegildoNoch keine Bewertungen
- Greek Acupuncture Meridians Points HippocratesDokument9 SeitenGreek Acupuncture Meridians Points Hippocrateskaravi schiniasNoch keine Bewertungen
- Peripheral Neuropathy TreatmentDokument3 SeitenPeripheral Neuropathy TreatmentSantiago HerreraNoch keine Bewertungen
- Premio 20 DTDokument35 SeitenPremio 20 DThyakueNoch keine Bewertungen
- 10 Denmark DVM Earacupuncture WebDokument10 Seiten10 Denmark DVM Earacupuncture WebDaniel Mendes NettoNoch keine Bewertungen
- Acupoint Stimulation Effective for AcneDokument22 SeitenAcupoint Stimulation Effective for AcneCristian SauraNoch keine Bewertungen
- Respiratory Examination - Protected 1Dokument4 SeitenRespiratory Examination - Protected 1anirudh811100% (1)
- Towards A Spirit at Peace: Understanding The Treatment of Shen Disorders With Chinese MedicineDokument6 SeitenTowards A Spirit at Peace: Understanding The Treatment of Shen Disorders With Chinese MedicineMarcin SowNoch keine Bewertungen
- Cerebrolysin in Patients With Hemorrhagic StrokeDokument7 SeitenCerebrolysin in Patients With Hemorrhagic StrokeZeynep Emirhan ŞenyüzNoch keine Bewertungen
- Cmac Point LocationDokument23 SeitenCmac Point LocationvinayNoch keine Bewertungen
- Docid 3 873Dokument4 SeitenDocid 3 873Faith Acu CureNoch keine Bewertungen
- Acu DevicesDokument6 SeitenAcu Devicescksharma68Noch keine Bewertungen
- Autonomic Regulation 1Dokument5 SeitenAutonomic Regulation 1Darren StarwynnNoch keine Bewertungen
- Large Intestine LI 1Dokument11 SeitenLarge Intestine LI 1Renugadevi DinakaranNoch keine Bewertungen
- Discover Instant and Natural Ways To Relieve Arthritis PainVon EverandDiscover Instant and Natural Ways To Relieve Arthritis PainNoch keine Bewertungen
- Effects of Low - vs. High-Load Resistance Training On Muscle Strength and Hypertrophy in Well-Trained MenDokument2 SeitenEffects of Low - vs. High-Load Resistance Training On Muscle Strength and Hypertrophy in Well-Trained MenPedro MaiaNoch keine Bewertungen
- FLIR One Ios Android User GuideDokument11 SeitenFLIR One Ios Android User GuideAmol KhadkeNoch keine Bewertungen
- AkbarDokument2 SeitenAkbarvamshishashankNoch keine Bewertungen
- Bitcoin Manifesto - Satoshi NakamotoDokument9 SeitenBitcoin Manifesto - Satoshi NakamotoJessica Vu100% (1)
- Bitcoin Manifesto - Satoshi NakamotoDokument9 SeitenBitcoin Manifesto - Satoshi NakamotoJessica Vu100% (1)
- Study of Acupuncture For Low Back Pain in Recent 20 Years: A Bibliometric Analysis Via CiteSpaceDokument14 SeitenStudy of Acupuncture For Low Back Pain in Recent 20 Years: A Bibliometric Analysis Via CiteSpacePedro MaiaNoch keine Bewertungen
- High-Intensity Versus Low-Intensity Physical Activity Orexercise in People With Hip or Knee Osteoarthritis (Review)Dokument65 SeitenHigh-Intensity Versus Low-Intensity Physical Activity Orexercise in People With Hip or Knee Osteoarthritis (Review)Pedro MaiaNoch keine Bewertungen
- Cartaz A4 MansionDokument1 SeiteCartaz A4 MansionPedro MaiaNoch keine Bewertungen
- High-Intensity Versus Low-Intensity Physical Activity or Exercise in People With Hip or Knee Osteoarthritis (Review)Dokument65 SeitenHigh-Intensity Versus Low-Intensity Physical Activity or Exercise in People With Hip or Knee Osteoarthritis (Review)Pedro MaiaNoch keine Bewertungen
- Dr. Tan - S Vessel Relationships ChartDokument2 SeitenDr. Tan - S Vessel Relationships ChartPedro Maia100% (3)
- Bwhisnant Introallergies LNDokument9 SeitenBwhisnant Introallergies LNPedro Maia100% (2)
- Brad Whisnant Five Element WebinarDokument27 SeitenBrad Whisnant Five Element WebinarRodrigo Bittencourt93% (15)
- Eran Even Autumn 2016Dokument8 SeitenEran Even Autumn 2016Pedro MaiaNoch keine Bewertungen
- TCM Medicated Diet Recipes for HealthDokument117 SeitenTCM Medicated Diet Recipes for Healthmayyrv67% (3)
- Anatomical Foundations of Chinese MedDokument29 SeitenAnatomical Foundations of Chinese Medanattā100% (1)
- Ancient Chinese Gua Chart and Organ PointsDokument1 SeiteAncient Chinese Gua Chart and Organ PointsPedro MaiaNoch keine Bewertungen
- Videos para VerDokument1 SeiteVideos para VerPedro MaiaNoch keine Bewertungen
- BL 47Dokument1 SeiteBL 47BDI92Noch keine Bewertungen
- Possible Lung and Respiratory IndicationsDokument5 SeitenPossible Lung and Respiratory IndicationsPedro Maia100% (2)
- Foot and Hand Meridian ChartDokument12 SeitenFoot and Hand Meridian ChartWilliam Tell100% (11)
- 9.26.15 Gmaciocia Tonguedx LNDokument34 Seiten9.26.15 Gmaciocia Tonguedx LNPedro Maia67% (3)
- Yao Chart RevB Oct 2010Dokument1 SeiteYao Chart RevB Oct 2010Pedro Maia100% (1)
- Stomach Channel GuideDokument1 SeiteStomach Channel GuidePedro MaiaNoch keine Bewertungen
- The Extraordinary ChannelsDokument28 SeitenThe Extraordinary Channelsaleman_gloria9842Noch keine Bewertungen
- Ren 2 PDFDokument1 SeiteRen 2 PDFPedro MaiaNoch keine Bewertungen
- L. Intestine Contents Guide for Eye DiseasesDokument1 SeiteL. Intestine Contents Guide for Eye Diseasesray72roNoch keine Bewertungen
- ScheidDokument12 SeitenScheidPedro MaiaNoch keine Bewertungen
- Balancing The 5 Senses For TaiwanDokument19 SeitenBalancing The 5 Senses For TaiwanPedro Maia100% (3)
- Yili Scroll 3Dokument62 SeitenYili Scroll 3Pedro Maia100% (1)
- Balance Notes NewDokument4 SeitenBalance Notes NewPedro Maia100% (30)
- Financial Assistance for Burial Expenses Due to Death of Chronic Kidney Disease PatientDokument2 SeitenFinancial Assistance for Burial Expenses Due to Death of Chronic Kidney Disease Patientrafael solam75% (8)
- Assessment of Insulin Injection Practice of Nurses Working inDokument7 SeitenAssessment of Insulin Injection Practice of Nurses Working inBheru LalNoch keine Bewertungen
- Exploring The Health Outcomes of Conditional Cash Transfer Program in Rural PhilippinesDokument16 SeitenExploring The Health Outcomes of Conditional Cash Transfer Program in Rural PhilippinesNadine VillaretNoch keine Bewertungen
- CONSENT FOR BIOPSY v2Dokument1 SeiteCONSENT FOR BIOPSY v2Bhumika SharmaNoch keine Bewertungen
- ICL-Coding Operative ReportDokument33 SeitenICL-Coding Operative ReportHIMOfficial100% (2)
- Jurnal2 JBI - Critical - Appraisal-Checklist - For - Analytical - Cross - Sectional - Studies2017Dokument8 SeitenJurnal2 JBI - Critical - Appraisal-Checklist - For - Analytical - Cross - Sectional - Studies2017Allysa safitriNoch keine Bewertungen
- Administering Intramuscular Injection StepsDokument3 SeitenAdministering Intramuscular Injection StepsJela Jane ArcalNoch keine Bewertungen
- HR 1701 - Commending Medical and Nursing Board TopnotchersDokument2 SeitenHR 1701 - Commending Medical and Nursing Board TopnotchersBayan Muna Party-listNoch keine Bewertungen
- Ethics in Midwifery PowerpointDokument24 SeitenEthics in Midwifery PowerpointEden NatividadNoch keine Bewertungen
- Directory of Avma Ecfvg® Listed Veterinary Colleges of The WorldDokument16 SeitenDirectory of Avma Ecfvg® Listed Veterinary Colleges of The Worldkaran kambojNoch keine Bewertungen
- Referat ObsgynDokument21 SeitenReferat ObsgynRoberto HutapeaNoch keine Bewertungen
- Leadership in Health Services: Article InformationDokument19 SeitenLeadership in Health Services: Article Informationumadevi.nagiahNoch keine Bewertungen
- Ksa and Uae 2020 AmroDokument131 SeitenKsa and Uae 2020 AmroamroNoch keine Bewertungen
- Infection Control and Safety MeasuresDokument29 SeitenInfection Control and Safety MeasuresAlma Susan100% (1)
- Pharmacy: Google Classroom, Google Hangout, Google Meet Google Classroom, Google Hangout, Google MeetDokument5 SeitenPharmacy: Google Classroom, Google Hangout, Google Meet Google Classroom, Google Hangout, Google MeetFelix John Paul BarquerosNoch keine Bewertungen
- Share FORM 10 - Workplace Application Evaluation ToolDokument3 SeitenShare FORM 10 - Workplace Application Evaluation ToolRocel Ann CarantoNoch keine Bewertungen
- NEW GUIDELINES - CDC Softens Opioid Prescribing Guidelines For DoctorsDokument100 SeitenNEW GUIDELINES - CDC Softens Opioid Prescribing Guidelines For DoctorsDan LehrNoch keine Bewertungen
- NCP Risk For BleedingDokument1 SeiteNCP Risk For BleedingJen Garzo75% (4)
- Ruba Naz Siddiqui Objective: Bachelor in PhysiotherapyDokument4 SeitenRuba Naz Siddiqui Objective: Bachelor in PhysiotherapyASHUMEHMOODNoch keine Bewertungen
- Myers CocktailDokument15 SeitenMyers CocktailViladosgirassois Couto PinonNoch keine Bewertungen
- Blount's Disease and Its Homeopathic Self Treatment Scheme - Bashir Mahmud ElliasDokument5 SeitenBlount's Disease and Its Homeopathic Self Treatment Scheme - Bashir Mahmud ElliasBashir Mahmud ElliasNoch keine Bewertungen
- Jacobson Progressive Muscle Relaxation TechniqueDokument3 SeitenJacobson Progressive Muscle Relaxation TechniqueAleena ThakurtaNoch keine Bewertungen
- Bair Paws Patient Satisfaction Case StudyDokument3 SeitenBair Paws Patient Satisfaction Case StudymochkurniawanNoch keine Bewertungen
- Lived Experience Leading The Way: Peer Support in Mental HealthDokument4 SeitenLived Experience Leading The Way: Peer Support in Mental HealthCarolyn AndersonNoch keine Bewertungen
- 1 - DS SATK Form - Initial Application of LTO 1.2Dokument4 Seiten1 - DS SATK Form - Initial Application of LTO 1.2Sophia TokieNoch keine Bewertungen
- Dispensing Medications During Off-Hours StrategiesDokument14 SeitenDispensing Medications During Off-Hours StrategiesHamza Ali100% (2)
- Patient Blood Group ReportDokument1 SeitePatient Blood Group Reportمرتجز حیدرNoch keine Bewertungen
- Standards For Good Pharmacy Practice - A Comparative AnalysisDokument6 SeitenStandards For Good Pharmacy Practice - A Comparative AnalysisClaudia NovăceanNoch keine Bewertungen
- Complimentary & Alternative System of MedicineDokument27 SeitenComplimentary & Alternative System of MedicineSANANoch keine Bewertungen
- Konsep Pasien Safety Dalam Keperawatan, DR AdibDokument32 SeitenKonsep Pasien Safety Dalam Keperawatan, DR Adibvhero handayaniNoch keine Bewertungen