Beruflich Dokumente
Kultur Dokumente
Standardized Balance Tests for Fall Risk Assessment
Hochgeladen von
Alvin Ong0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
194 Ansichten8 Seitenguideline tips
Originaltitel
Assessment Protocols for Standardized Balance Tests Modified
Copyright
© © All Rights Reserved
Verfügbare Formate
PDF, TXT oder online auf Scribd lesen
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenguideline tips
Copyright:
© All Rights Reserved
Verfügbare Formate
Als PDF, TXT herunterladen oder online auf Scribd lesen
0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
194 Ansichten8 SeitenStandardized Balance Tests for Fall Risk Assessment
Hochgeladen von
Alvin Ongguideline tips
Copyright:
© All Rights Reserved
Verfügbare Formate
Als PDF, TXT herunterladen oder online auf Scribd lesen
Sie sind auf Seite 1von 8
1
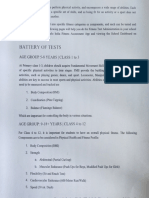
Assessment Protocols for Standardized Balance Tests
These are selected tests that are simple and quick yet are good indicators of falls risk and
are good outcome measures. The first three tests are for static and dynamic balance, and
leg strength that are good to use for brief performance screens. These take less than 5
minutes. All the balance measures can be used for measuring change in balance and
have good psychometric properties. We include the test protocols, normative values, or
risk cut points and a list of references.
GOOD BRIEF FALL SCREENING TESTS
1. TIMED UP AND GO TEST
2. SINGLE LEG STAND
3. SINGLE CHAIR RISE
OTHER BALANCE MEASURES USEFUL FOR ASSESSMENTS AND/OR OUTCOMES
4. TIMED CHAIR RISE x 5
5. CHAIR RISE # in 30 SEC
6. TANDEM STAND
7. 360
o
TURN PROTOCOL
8. FOUR SQUARE STEP TEST
9. ALTERNATE STEP TEST
10. TANDEM WALK TEST
2
PHYSICAL PERFORMANCE ASSESSMENTS FOR BALANCE AND FUNCTION
You will need a stop watch and masking tape. It is best to tell the client what the test measures,
give instructions, and demonstrate each test. You may need to repeat if it is obviously they do not
understand or were not giving it their best effort. These are all good tests for fall risk but
performance is also influenced by pain, cognitive ability, and other medical conditions. You will
need to interpret the results accordingly.
BRIEF FALL SCREENING TESTS
1. TIMED UP AND GO TEST
Description: The timed "Up & Go" test was developed as a brief screen for mobility and falls risk. It
has good test-retest reliability and sensitivity and specificity for falls. The timed "Up & Go" test
measures, in seconds, the time it takes for an individual to stand up from a standard arm chair
(approximate seat height of 46 cm, arm height 65 cm), walk a distance of 3 meters (9.84 feet), turn,
walk back to the chair, and sit down again. The participant wears his/her regular footwear and
uses his customary walking aid (none, cane, or walker). No physical assistance is given.
Instruction:
Participants start with their back against the chair, their arms resting on the armrests, and their
walking aid at hand if needed.
Instruction: When I say "go" Id like you to stand up and walk as quickly as safely as
possible to that line on the floor, turn, return to the chair, and sit down again.
Have the participant practice one trial to be sure they understand the procedure.
Start timing when you say go and stop when the participant sits down.
Use a stop-watch to time the performance and observe balance closely, especially at the turn.
If the participant does not perform the test correctly the first time (e.g., stops at the turn, does not
sit down right away, or does not walk all of the way to the 3 meter mark) repeat the test.
Record time in seconds to tenths of a second and which assistive device was used, if any.
Cut Points for this test vary depending on population studied, but generally accepted as 14 sec
2. SINGLE LEG STANCE
Description: Balance ability during a single leg stance. Measures static standing ability (balance
with feet fixed)
Instruction:
This test helps us to assess your standing balance. I want you to stand on one leg for as
long as you can, or until I say stop. Watch while I demonstrate. (Demonstrate using
chair/table/counter for initial support.)
You may choose either foot to stand on. You may hold you foot anywhere, but you may not
brace your free leg on the standing leg. Place your arm by your sides and try not to move
your feet or grab a support unless you need to gain your balance. Hold this position until I
say stop. When you are ready, pick up one of your feet from the floor and hold it as long as
you can.
Start timing when hand leaves the chair/table (if you are not using a support, start when the foot is
lifted). Stop timing when their free foot touches the ground, their hand contacts the chair/table,
their foot moved, or 30 seconds has passed.
Make sure you are close enough to guard the participant and they understand that they should put
their foot down before they fall.
Record the time to a tenth of a second.
3
Cut point Less than 10 sec indicated balance impairment and less than 5 sec fall risk.
3. SINGLE CHAIR RISE
Description: Measures the ability of person to rise from a chair. Chair rise is a complex test
requiring lower limb strength, range of motion, balance and is included in several risk assessment
scales.
Equipment: Stop watch and standard height chair.
Tester Notes: Have the participant sit erect in a standard height chair with the chair back against
the wall. You can use a chair with or without arms but the participants should not use their arms.
Instructions: Id like you to fold your arms across your chest and stand up one time.
Record Yes or No, is able or not. If the participant was NOT able to get up without using arms do
not perform the Repeated Chair Rise.
Cut Point = unable
OTHER BALANCE MEASURES USEFUL FOR ASSESSMENTS AND/OR OUTCOMES
4. TIMED REPEATED CHAIR RISE x 5 (SIT-to-STAND)
Description: Measures the ability of person to rise from a chair repeatedly. Repeated chair rise
test requires lower limb strength, range of motion, balance, and endurance. For the sit-to-stand
test with five repetitions subjects are asked to rise from a standard height (43 cm) chair without
armrests, five times, as quickly as possible with their arms folded across their chest.
Equipment: Stopwatch and standard height chair.
Tester Notes: Check that the client can successful perform a single chair rise before you test
repeated chair rise.
Instructions: Id like you to fold your arms across your chest and when I say go, I want
you to stand up and sit down as quickly as you can five times in row.
Record the time from the command go until the participant is in the final seated position,
and the number of completed chair rises (0-5)
Cut point Greater than 15 sec indicator for fall risk
5. 30 SECOND CHAIR RISE - ALTERNATIVE TEST
Description: This chair rise test is a functional measure of lower body strength. This is an item
from The Senior Fitness Test (Rikli and Jones 1999). The scores are compared to norms values
for gender and age. This is a good test to performance as a group. Each person counts their
stands while you time.
Instruction:
When I say go, I want you to stand up and sit down as quickly as you can until I tell you to
stop. You dont have to sit back in the chair completely, but you do have to make
sure your buttocks contacts the chair. I am going to count how many times you can up in
30 seconds.
Record the number of stands completed in 30 seconds from go command
Cut Point Generally less than 10 is an indication of poor leg strength. As yet there is no fall risk for
this test.
4
6. TANDEM STANCE
Description: Assesses static balance narrow base of support. For clients who cannot perform the
single leg stance, use the TS test for an outcome measure. It is a very responsive measure.
Tester Information: Participants s should wear tennis shoes or shoes with low or no heels.
Describe the stance to the resident as you demonstrate it. Stress that if the resident feels it
would be unsafe to try, to tell you. If the activity is not being done properly, demonstrate it again
or repeat instructions. Guard the participant for balance loss.
Stand next to the client to help him/her into the position. Make sure you have a table or chair
that the client can use for support. Supply just enough support to the clients arm to prevent loss
of balance. Start timing when support is released. Stop after 30 seconds or when the participant
steps out of position.
Instructions: This test will help us assess your balance during standing.
First I will show you the movement then I want you to try it. 'I would like you to stand with the
heel of one foot in front of and touching the toes of the other foot for 30 seconds. Keep you arms
by your sides and try not to shift your feet. Hold this position until I say stop.'
Record the time held to the nearest tenth of a second. If clients refuse, mark 0 time and indicate
they refused.
Cut point unable to TS for 10 sec is fall risk indicator
7. 360
o
TURN PROTOCOL
Description: A measure of dynamic balance. The participant turns in a complete circle 360
degrees. You can test to either direction but each trial is only one complete turn. The 360
and walking speed are highly correlated so you can which to use for dynamic balance.
Tester Notes:
Place a piece of masking tape on the floor for a starting position.
The participant stands with arms at his/her side and feet comfortably apart and pointing
straight ahead at the tape.
Start timing from the word GO and stop when the participants shoulders are square facing
you again. Have the participant do two trials. The participant may turn in either direction.
Instructions:
When I say go, I want you to turn around at your normal pace making sure to go in a
complete circle and take steps as you turn. Make sure you end up facing me.
Ill show you (demonstrate the turn). You choose which direction you want to turn.
When I say 'go' start turning. Ready, go.
Record the time for both trials to the nearest tenth of a second
Cut Point >3.8 sec is indicator of fall risk
5
8. FOUR SQUARE STEP TEST
Description: A higher order complex task assessing dynamic balance. This is a good test for
more advance balance skills and has a strong cognitive component.
Tester Notes:
1. Place four canes (1/2 inch pvc pipe, 35 inch length with a 4-way connector works
well) on the ground to form four squares.
2. Participants start in square one facing square two. Participants step forward into
square two, sideways to square three, backwards to square four, sideways into one,
and then reverse the sequence - sideways into four, forward, sideways, and
backwards to one. The sequence is 1,2,3,4,1,4,3,2,1.
3. Instructions are to complete the sequence as fast as possible without touching the
canes, both feet must make contact with the floor in each square, and to try to stay
facing forward during the entire sequence.
4. The sequence is demonstrated and participants are allowed one practice trial then
time two trials. The best time is recorded. Participants wear their usual shoes and
are allowed to turn their body to negotiate the canes if necessary, but should try to
face forward at all times. Mistrials occur if the participant cannot complete the
sequence, loses balance or steps on a cane. One mistrial is allowed.
Special Instructions: Participants may lose balance, make sure you are guarding. You can
cue the participants through the practice, but they should do the subsequent trials without
cueing. The most common error is not reversing the sequence at box one.
Participant Instructions: We are going to do a stepping test to check your balance. This
is what I want you to do: Demonstrate sequence and verbalize sequence while you are
demonstrating. Try to complete the sequence as fast as possible without touching the
sticks. Both your feet should make contact with the floor in each square. If possible,
face forward during the entire sequence. First I would like you practice one time. One
practice trial is completed to ensure the subject knows the sequence.
Record time from when the first foot contacts the floor in square 2 to when the last foot
comes back to touch the floor in square1. Two FSST are completed with the best time taken
as the score.
Cut point for falls risk >15sec
9. ALTERNATE STEP TEST
Description: The alternate-step test (AST) is a modified version of the Berg Balance Test stool-
stepping task. It involves weight shifting and provides a measure of lateral stability. This test
involves alternatively placing the entire left and right feet (shoes removed) as fast as possible onto
a step 18 cm high and 40 cm deep.
Instruction: I want you to place you feet on this step alternating R and L feet. Ill show you
(demonstrate).
Record: The time taken to complete eight steps, alternating between the left and right feet.
Cut point 10s RR =2.3 (CI 1.4, 3.5) LR =1.57, Sensitivity/specificity, 69/56.
Alternative is to count the number of steps in 10 sec
2 3
1 4
6
10. TANDEM WALK TEST
Description: Tandem gait is a high demand activity requiring careful control of both center of mass
movement (head, trunk, pelvis) and the successive re-establishment of a stable, narrow base of
support. Compared to normal gait, the tandem walk test tends to be more specific to impairments
affecting balance.
Instruction: There are two ways of conducting this test and evidence for clear cut points for falls
risk are not well established. Clients are required to walk heel to toe along a 10-foot line as quickly
as possible without errors. Errors included not walking heel to toe, stepping off the gait line, and
losing balance. I want you to walk along this line heel to toe without stepping off the line as
quickly as possible, its like a sobriety test.
Record: You can measure performance time and number of errors for three trials and average
across trials. Counting errors is tricky and not very reliable. An alternative is to ask clients to take 4
steps and score it as able or unable.
REFERENCES
Timed Up and Go Test
Podsiadlo D, Richardson S. The Timed Up & Go: A test of basic functional mobility for frail elderly
persons. J Am Geriatr Soc. 1991;39:142-148.
Shumway-Cook A, Brauer S, Woollacott M. Predicting the probability for falls in community-
dwelling older adults using the Timed Up & Go Test. Phys Ther. 2000;80:896-903.
Bohannon RW. Reference values for the timed up and go test: a descriptive meta-analysis. J
Geriatr Phys Ther. 2006;29(2):64-68.
Isles RC, Low Choy NL, Steer M, Nitz JC. Normal Values of Balance Tests in Women Aged
2080 J Am Geriatr Soc 52:13671372, 2004
Gunter KB, White KN, Hayes WC, et al. Functional mobility discriminates nonfallers from one-time
and frequent fallers. J Gerontol A Biol
Sci Med Sci 2000;55:M6726.
Timed Chair Stands
Guralnik JM, Simonsick EM, Ferucci L, et al. A short physical performance battery
assessing lower extremity function: association with self-reported disability and prediction of
mortality and nursing home admission. J Gerontol. 1994;49:M85-M94.
Guralnik JM, Ferucci L, Simonsick EM, et al. Lower extremity function in persons over the
age of 70 as a predictor of subsequent disability. N Engl J Med. 1995;332:556-561.
Whitney SL, Wrisley DM, Marchetti GF, et al. Clinical measurement of sit-to-stand
performance in people with balance disorders: validity of data for the Five-Times-Sit-to-
Stand Test. Phys Ther. 2005;85:1034 1045
30 sec Chair Stand
Rikli R, Jones J. Development and validation of a functional fitness test for community-
residing older adults. Journal of Aging and Physical Activity 1999a;7:129-161
Rikli R, Jones J. Functional fitness normative scores for community-residing older adults,
ages 60-94. Journal of Aging and Physical Activity 1999b;7:162-181
Single Limb Stand
7
Bohannon R, Larkin P, Cook A, Singer J. 1984. Decrease in timed balance test scores with
aging. Phys Ther 64:1067-1070
Vellas BJ, Wayne SJ, Romero L, Baumgartner RN, Rubenstein LZ, Garry PJ. One-leg
stance is an important predictor of injurious falls in older persons. J Am Geriatr Soc.
1997;45(6): 735-8.
Tandem and Semi-Tandem Stance
Guralnik JM. Ferrucci L. Simonsick EM. Salive ME. Wallace RB. Lower-extremity function in
persons over the age of 70 years as a predictor of subsequent disability. New England
Journal of Medicine. 1995;332(9):556-61.
Guralnik JM. Simonsick EM. Ferrucci L. Glynn RJ. Berkman LF. Blazer DG. Scherr PA.
Wallace RB. A short physical performance battery assessing lower extremity function:
association with self-reported disability and prediction of mortality and nursing home
admission. Journal of Gerontology. 1994;49(2):M85-94.
Walking Speed
Ferucci L, Guralnik JM, Salive ME, Fried LP, Bandeen-Roche K, Brock DB, Simonsick EM,
Corti MC, Zeger SL. Effect of age and severity of disability on short-term variation in walking
speed: the Womens Health and Aging Study. J Clinical Epidemiology. 1996;49(10):1089-
1096.
Guralnik JM, Ferrucci L, Pieper CF, Leveille SG, Markides KS, Ostir GV, Studenski S,
Berkman LF, Wallace RB. Lower extremity function and subsequent disability: consistency
across studies, predictive models, and value of gait speed alone compared with the short
physical performance battery. Gerontol A Biol Sci Med Sci. 2000;55(4):M221-31.
Harada N, Chiu V, Damron-Rodrigues J, et al. Screening for balance and mobility
impairment in elderly individuals living in residential care facilties. Phys Ther. 1995:75:462-
469.
Studenski S, Perera S, Wallace D, Chandler JM, Duncan PW, Rooney E, Fox M, Guralnik
JM. Physical performance measures in the clinical setting. J Am Geriatr Soc.
2003;51(3):314-22.
Van Swearingen JM, Paschal KA, Bonino P, Chen T. Assessing recurrent fall risk of
community dwelling, frail older veterans using specific tests of mobility and the Physical
Performance Test of function. J Gerontol A Biol Sci Med Sci. 1998;53:M457-M464.
360 Degree Turn
Gill TM, Williams CS, Mendes de Leon CF, Tinetti ME. The role of change in physical
performance in determining risk for dependence in activities of daily living among
nondisabled community-living elderly persons. Journal of Clinical Epidemiology.
1997;50(7):765-772.
Berg KO, Wood-Dauphinee SL, Williams JI, Maki BE. Measuring balance in the elderly:
validation of an instrument. Can J Public Health. 1992;83(suppl 2):S7-S11.
Van Swearingen JM, Paschal KA, Bonino P, Chen T. Assessing recurrent fall risk of
community dwelling, frail older veterans using specific tests of mobility and the Physical
Performance Test of function. J Gerontol A Biol Sci Med Sci. 1998;53:M457-M464.
Reuben DB, Siu AL. An objective measure of physical function of elderly outpatients: The
Physical Performance Test. J Am Geriatr Soc. 1990;38:1105-1112.
Four Square Step Test
Dite W, Temple VA. A clinical test of stepping and change of direction to identify multiple
falling older adults. Arch Phys Med Rehabil. 2002;83:1566-1571.
8
Alternate Step Test
Tiedemann A, Shimada H, Sherrington C, Murray C, Lord S. The comparative ability of eight
functional mobility tests for predicting falls in community-dwelling older people. Age and Ageing
2008; 37: 430435
Berg KO, Wood-Dauphinee SL, Williams JI, Maki BE. Measuring balance in the elderly:
validation of an instrument. Can J Public Health. 1992;83(suppl 2):S7-S11.
Hill K, Bernhardt J, McGann D et al. A new test of dynamic standing balance for stroke patients:
Reliability, validity and comparison with healthy elderly. Physiother Can 1996;48:257262.
Das könnte Ihnen auch gefallen
- CH-6 C - Test and Measurement in SportsDokument13 SeitenCH-6 C - Test and Measurement in SportsAkankshaNoch keine Bewertungen
- Euro Fit Fitness TestingDokument10 SeitenEuro Fit Fitness TestingAlisa CorobeaNoch keine Bewertungen
- Riks Jones TestDokument4 SeitenRiks Jones Testsachin pathakNoch keine Bewertungen
- Sit and Reach Flexibility TestDokument5 SeitenSit and Reach Flexibility TestJethro Enriquez100% (1)
- Test&Measurement GR 12Dokument8 SeitenTest&Measurement GR 12umamahfarooq75Noch keine Bewertungen
- Motor Fitness TestDokument23 SeitenMotor Fitness Testdharmendra jhaNoch keine Bewertungen
- Physical Education For Written in Lab ManualDokument24 SeitenPhysical Education For Written in Lab ManualAnirudh PratapNoch keine Bewertungen
- Assignment: Name: Class: XII Board Roll Number: Session: 2019-20Dokument31 SeitenAssignment: Name: Class: XII Board Roll Number: Session: 2019-20Biswarup NahaNoch keine Bewertungen
- Exercise Movement Activities To Test Balance, Muscle Endurance & Strength, Flexibility, Speed and AgilityDokument36 SeitenExercise Movement Activities To Test Balance, Muscle Endurance & Strength, Flexibility, Speed and AgilityJohn Michael FornelozaNoch keine Bewertungen
- Physical Fitness Test BatteryDokument10 SeitenPhysical Fitness Test Batteryyy_ssNoch keine Bewertungen
- P-E Physical Fitness Test BatteryDokument9 SeitenP-E Physical Fitness Test BatteryAl Brelzhiv SarsalejoNoch keine Bewertungen
- PE Chapter - 6Dokument72 SeitenPE Chapter - 6Punjabi Bass BoostedNoch keine Bewertungen
- Class: XII Topic: Subject: Physical Education: 1.50 Meter DashDokument8 SeitenClass: XII Topic: Subject: Physical Education: 1.50 Meter DashKunwar Devang Pratap SinghNoch keine Bewertungen
- 6 Test and Measurement-1Dokument10 Seiten6 Test and Measurement-1YashNoch keine Bewertungen
- Physical Education Class 12 (Chapter 7, 5 Marks) QuestionsDokument5 SeitenPhysical Education Class 12 (Chapter 7, 5 Marks) QuestionsTarget MyurNoch keine Bewertungen
- PE Project gr12Dokument15 SeitenPE Project gr12Daivik NagarajNoch keine Bewertungen
- UNIT - 6: Test & Measurement in Sports..!! Along-With Important QuestionsDokument68 SeitenUNIT - 6: Test & Measurement in Sports..!! Along-With Important QuestionsMahima Famous100% (1)
- Ped001 StationsDokument36 SeitenPed001 StationsAngelNoch keine Bewertungen
- PFT Manual 2021 2022Dokument10 SeitenPFT Manual 2021 2022L Y N N A HNoch keine Bewertungen
- Lab2 HowfitareyouDokument6 SeitenLab2 Howfitareyouapi-500185788Noch keine Bewertungen
- Short Physical Performance Battery Tests Balance, Walking SpeedDokument3 SeitenShort Physical Performance Battery Tests Balance, Walking SpeedLydia MartínNoch keine Bewertungen
- Fitness Test and MeasurementDokument10 SeitenFitness Test and MeasurementSAFDAR Hafiz100% (1)
- Fitness Test ProceduresDokument5 SeitenFitness Test ProceduresFelicity CabreraNoch keine Bewertungen
- CLASS 12 PracticalDokument10 SeitenCLASS 12 PracticalWORLD HISTORYNoch keine Bewertungen
- Fitness Assessment Tools and ProceduresDokument3 SeitenFitness Assessment Tools and ProceduresLowell SantuaNoch keine Bewertungen
- Senior Fitness TestsDokument29 SeitenSenior Fitness TestsRitik Chaudhary100% (7)
- Lesson 1Dokument17 SeitenLesson 1Chitsu ChanNoch keine Bewertungen
- Stork Balance Test: One-Leg Balance AssessmentDokument6 SeitenStork Balance Test: One-Leg Balance AssessmentUrikache LeyoungNoch keine Bewertungen
- Chapter 6 (Class XII)Dokument21 SeitenChapter 6 (Class XII)Ʀù D ƦåNoch keine Bewertungen
- Athletic Testing For Basketball PlayersDokument12 SeitenAthletic Testing For Basketball Playerseretria100% (1)
- Skill Related Fitness: Learning Activity Sheet (SHS) Physical Education and Health 1Dokument7 SeitenSkill Related Fitness: Learning Activity Sheet (SHS) Physical Education and Health 1Mark Allen LabasanNoch keine Bewertungen
- DocumentDokument14 SeitenDocumentSeema TeotiaNoch keine Bewertungen
- Chapter - 7 (Test and Measurement inDokument41 SeitenChapter - 7 (Test and Measurement inrm2006bwcNoch keine Bewertungen
- Student Fitness RecordDokument5 SeitenStudent Fitness RecordIan Hasheem O. DaniNoch keine Bewertungen
- Taguig City University Lesson on Physical Fitness TestsDokument13 SeitenTaguig City University Lesson on Physical Fitness TestsDom RejanoNoch keine Bewertungen
- Khelo India Test 2023Dokument12 SeitenKhelo India Test 2023asi795856Noch keine Bewertungen
- Q1 W4 M1 PeDokument3 SeitenQ1 W4 M1 PeChristian Don VelasquezNoch keine Bewertungen
- Fitness Tests SummaryDokument61 SeitenFitness Tests SummaryOm ZaveriNoch keine Bewertungen
- Unit ContentsDokument61 SeitenUnit ContentsOm ZaveriNoch keine Bewertungen
- Physical Education Class 12 Chapter 6 NotesDokument11 SeitenPhysical Education Class 12 Chapter 6 NotesAanchal PandeyNoch keine Bewertungen
- Yoga Class 12Dokument13 SeitenYoga Class 12Vandan KNoch keine Bewertungen
- Physical Fitness TestsDokument13 SeitenPhysical Fitness TestsJanzen Delos SantosNoch keine Bewertungen
- Physical Fitness Test BatteryDokument2 SeitenPhysical Fitness Test Batterymarla7368Noch keine Bewertungen
- Please Include This in All Learning Activity SheetsDokument14 SeitenPlease Include This in All Learning Activity SheetsApolonio Jr Punzalan EspirituNoch keine Bewertungen
- Activity 4Dokument3 SeitenActivity 4Princess Jonna BoiserNoch keine Bewertungen
- Lesson 1-Admistration of Physical Fitness TestDokument5 SeitenLesson 1-Admistration of Physical Fitness TestENSANO, RHYNS G.Noch keine Bewertungen
- The Physical Fitness TestsDokument61 SeitenThe Physical Fitness TestsMark John DomingoNoch keine Bewertungen
- Elearning Fitness Tests HOW TO TEST InformationDokument6 SeitenElearning Fitness Tests HOW TO TEST InformationCarson LoefflerNoch keine Bewertungen
- Sai Khelo IndiaDokument10 SeitenSai Khelo Indiaswayamprasadb0Noch keine Bewertungen
- Rikli and Jones TestDokument5 SeitenRikli and Jones TestNimisha Dhakad100% (2)
- Week 1-2 PathfitDokument11 SeitenWeek 1-2 PathfitRenelyn Repol RebloraNoch keine Bewertungen
- PHYSICAL-FITNESS-ASSESSMENT-lesson-1Dokument8 SeitenPHYSICAL-FITNESS-ASSESSMENT-lesson-1Glia QuillanoraNoch keine Bewertungen
- The Physical Fitness TestsDokument62 SeitenThe Physical Fitness TestsglennbondocNoch keine Bewertungen
- Physical Fitness Testing SheetDokument4 SeitenPhysical Fitness Testing SheetyujinanNoch keine Bewertungen
- Ampputee Mobility PredictorDokument2 SeitenAmpputee Mobility PredictorEldar SulejmanovicNoch keine Bewertungen
- Fitness Testing Methods & ReasonsDokument6 SeitenFitness Testing Methods & ReasonsKasam ANoch keine Bewertungen
- Pat Testing ResultsDokument2 SeitenPat Testing Resultsapi-314189740Noch keine Bewertungen
- Fitness Assessment Tools and Procedures Guide - Measure Your Physical Fitness LevelsDokument53 SeitenFitness Assessment Tools and Procedures Guide - Measure Your Physical Fitness LevelsVince AmarillaNoch keine Bewertungen
- A Princess of Mars Part 3Dokument4 SeitenA Princess of Mars Part 3Sheila Inca100% (1)
- Objective Mech II - IES 2009 Question PaperDokument28 SeitenObjective Mech II - IES 2009 Question Paperaditya_kumar_meNoch keine Bewertungen
- Assembly ModelingDokument222 SeitenAssembly ModelingjdfdfererNoch keine Bewertungen
- Masteringphys 14Dokument20 SeitenMasteringphys 14CarlosGomez0% (3)
- Anti Jamming of CdmaDokument10 SeitenAnti Jamming of CdmaVishnupriya_Ma_4804Noch keine Bewertungen
- Propoxur PMRADokument2 SeitenPropoxur PMRAuncleadolphNoch keine Bewertungen
- Get Oracle Order DetailsDokument4 SeitenGet Oracle Order Detailssiva_lordNoch keine Bewertungen
- EC GATE 2017 Set I Key SolutionDokument21 SeitenEC GATE 2017 Set I Key SolutionJeevan Sai MaddiNoch keine Bewertungen
- Chapter 4 DeterminantsDokument3 SeitenChapter 4 Determinantssraj68Noch keine Bewertungen
- Efaverenz p1Dokument4 SeitenEfaverenz p1Pragat KumarNoch keine Bewertungen
- Lab StoryDokument21 SeitenLab StoryAbdul QadirNoch keine Bewertungen
- WindSonic GPA Manual Issue 20Dokument31 SeitenWindSonic GPA Manual Issue 20stuartNoch keine Bewertungen
- Link Ratio MethodDokument18 SeitenLink Ratio MethodLuis ChioNoch keine Bewertungen
- France Winckler Final Rev 1Dokument14 SeitenFrance Winckler Final Rev 1Luciano Junior100% (1)
- Strategies For StartupDokument16 SeitenStrategies For StartupRoshankumar BalasubramanianNoch keine Bewertungen
- Unr Ece R046Dokument74 SeitenUnr Ece R046rianteri1125Noch keine Bewertungen
- Methods to estimate stakeholder views of sustainabilityDokument7 SeitenMethods to estimate stakeholder views of sustainabilityAlireza FatemiNoch keine Bewertungen
- Baobab MenuDokument4 SeitenBaobab Menuperseverence mahlamvanaNoch keine Bewertungen
- Test Bank For Fundamental Financial Accounting Concepts 10th by EdmondsDokument18 SeitenTest Bank For Fundamental Financial Accounting Concepts 10th by Edmondsooezoapunitory.xkgyo4100% (47)
- How To Text A Girl - A Girls Chase Guide (Girls Chase Guides) (PDFDrive) - 31-61Dokument31 SeitenHow To Text A Girl - A Girls Chase Guide (Girls Chase Guides) (PDFDrive) - 31-61Myster HighNoch keine Bewertungen
- Condition Based Monitoring System Using IoTDokument5 SeitenCondition Based Monitoring System Using IoTKaranMuvvalaRaoNoch keine Bewertungen
- SEC QPP Coop TrainingDokument62 SeitenSEC QPP Coop TrainingAbdalelah BagajateNoch keine Bewertungen
- Weone ProfileDokument10 SeitenWeone ProfileOmair FarooqNoch keine Bewertungen
- KPUPDokument38 SeitenKPUPRoda ES Jimbert50% (2)
- WWW - Commonsensemedia - OrgDokument3 SeitenWWW - Commonsensemedia - Orgkbeik001Noch keine Bewertungen
- 1st SemDokument3 Seiten1st SemARUPARNA MAITYNoch keine Bewertungen
- Staffing Process and Job AnalysisDokument8 SeitenStaffing Process and Job AnalysisRuben Rosendal De Asis100% (1)
- A Database of Chromatographic Properties and Mass Spectra of Fatty Acid Methyl Esters From Omega-3 ProductsDokument9 SeitenA Database of Chromatographic Properties and Mass Spectra of Fatty Acid Methyl Esters From Omega-3 ProductsmisaelNoch keine Bewertungen
- PHY210 Mechanism Ii and Thermal Physics Lab Report: Faculty of Applied Sciences Uitm Pahang (Jengka Campus)Dokument13 SeitenPHY210 Mechanism Ii and Thermal Physics Lab Report: Faculty of Applied Sciences Uitm Pahang (Jengka Campus)Arissa SyaminaNoch keine Bewertungen
- Galaxy Owners Manual Dx98vhpDokument10 SeitenGalaxy Owners Manual Dx98vhpbellscbNoch keine Bewertungen
- Why We Die: The New Science of Aging and the Quest for ImmortalityVon EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityBewertung: 3.5 von 5 Sternen3.5/5 (2)
- 10% Human: How Your Body's Microbes Hold the Key to Health and HappinessVon Everand10% Human: How Your Body's Microbes Hold the Key to Health and HappinessBewertung: 4 von 5 Sternen4/5 (33)
- The Molecule of More: How a Single Chemical in Your Brain Drives Love, Sex, and Creativity--and Will Determine the Fate of the Human RaceVon EverandThe Molecule of More: How a Single Chemical in Your Brain Drives Love, Sex, and Creativity--and Will Determine the Fate of the Human RaceBewertung: 4.5 von 5 Sternen4.5/5 (515)
- Masterminds: Genius, DNA, and the Quest to Rewrite LifeVon EverandMasterminds: Genius, DNA, and the Quest to Rewrite LifeNoch keine Bewertungen
- The Consciousness Instinct: Unraveling the Mystery of How the Brain Makes the MindVon EverandThe Consciousness Instinct: Unraveling the Mystery of How the Brain Makes the MindBewertung: 4.5 von 5 Sternen4.5/5 (93)
- Crypt: Life, Death and Disease in the Middle Ages and BeyondVon EverandCrypt: Life, Death and Disease in the Middle Ages and BeyondBewertung: 4 von 5 Sternen4/5 (3)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisVon EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisBewertung: 3.5 von 5 Sternen3.5/5 (2)
- This Is Your Brain On Parasites: How Tiny Creatures Manipulate Our Behavior and Shape SocietyVon EverandThis Is Your Brain On Parasites: How Tiny Creatures Manipulate Our Behavior and Shape SocietyBewertung: 3.5 von 5 Sternen3.5/5 (31)
- The Ancestor's Tale: A Pilgrimage to the Dawn of EvolutionVon EverandThe Ancestor's Tale: A Pilgrimage to the Dawn of EvolutionBewertung: 4 von 5 Sternen4/5 (811)
- All That Remains: A Renowned Forensic Scientist on Death, Mortality, and Solving CrimesVon EverandAll That Remains: A Renowned Forensic Scientist on Death, Mortality, and Solving CrimesBewertung: 4.5 von 5 Sternen4.5/5 (397)
- The Other Side of Normal: How Biology Is Providing the Clues to Unlock the Secrets of Normal and Abnormal BehaviorVon EverandThe Other Side of Normal: How Biology Is Providing the Clues to Unlock the Secrets of Normal and Abnormal BehaviorNoch keine Bewertungen
- Wayfinding: The Science and Mystery of How Humans Navigate the WorldVon EverandWayfinding: The Science and Mystery of How Humans Navigate the WorldBewertung: 4.5 von 5 Sternen4.5/5 (18)
- Undeniable: How Biology Confirms Our Intuition That Life Is DesignedVon EverandUndeniable: How Biology Confirms Our Intuition That Life Is DesignedBewertung: 4 von 5 Sternen4/5 (11)
- The Lives of Bees: The Untold Story of the Honey Bee in the WildVon EverandThe Lives of Bees: The Untold Story of the Honey Bee in the WildBewertung: 4.5 von 5 Sternen4.5/5 (44)
- The Second Brain: A Groundbreaking New Understanding of Nervous Disorders of the Stomach and IntestineVon EverandThe Second Brain: A Groundbreaking New Understanding of Nervous Disorders of the Stomach and IntestineBewertung: 4 von 5 Sternen4/5 (17)
- Eels: An Exploration, from New Zealand to the Sargasso, of the World's Most Mysterious FishVon EverandEels: An Exploration, from New Zealand to the Sargasso, of the World's Most Mysterious FishBewertung: 4 von 5 Sternen4/5 (30)
- Summary of Robert M. Sapolsky's DeterminedVon EverandSummary of Robert M. Sapolsky's DeterminedBewertung: 5 von 5 Sternen5/5 (2)
- A Brief History of Intelligence: Evolution, AI, and the Five Breakthroughs That Made Our BrainsVon EverandA Brief History of Intelligence: Evolution, AI, and the Five Breakthroughs That Made Our BrainsBewertung: 4.5 von 5 Sternen4.5/5 (4)
- Human Errors: A Panorama of Our Glitches, from Pointless Bones to Broken GenesVon EverandHuman Errors: A Panorama of Our Glitches, from Pointless Bones to Broken GenesBewertung: 3.5 von 5 Sternen3.5/5 (56)
- The Mind & The Brain: Neuroplasticity and the Power of Mental ForceVon EverandThe Mind & The Brain: Neuroplasticity and the Power of Mental ForceNoch keine Bewertungen
- Gathering Moss: A Natural and Cultural History of MossesVon EverandGathering Moss: A Natural and Cultural History of MossesBewertung: 4.5 von 5 Sternen4.5/5 (347)
- The Dog Who Couldn't Stop Loving: How Dogs Have Captured Our Hearts for Thousands of YearsVon EverandThe Dog Who Couldn't Stop Loving: How Dogs Have Captured Our Hearts for Thousands of YearsNoch keine Bewertungen
- Younger for Life: Feel Great and Look Your Best with the New Science of AutojuvenationVon EverandYounger for Life: Feel Great and Look Your Best with the New Science of AutojuvenationBewertung: 4 von 5 Sternen4/5 (1)
- Darwin's Dangerous Idea: Evolution and the Meaning of LifeVon EverandDarwin's Dangerous Idea: Evolution and the Meaning of LifeBewertung: 4 von 5 Sternen4/5 (523)
- Superlative: The Biology of ExtremesVon EverandSuperlative: The Biology of ExtremesBewertung: 4.5 von 5 Sternen4.5/5 (51)
- Why We Sleep: Unlocking the Power of Sleep and DreamsVon EverandWhy We Sleep: Unlocking the Power of Sleep and DreamsBewertung: 4.5 von 5 Sternen4.5/5 (2083)
- Lymph & Longevity: The Untapped Secret to HealthVon EverandLymph & Longevity: The Untapped Secret to HealthBewertung: 4.5 von 5 Sternen4.5/5 (13)