Beruflich Dokumente
Kultur Dokumente
PCA and Epidural Presentation Outline 2014
Hochgeladen von
sparticuslivesCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
PCA and Epidural Presentation Outline 2014
Hochgeladen von
sparticuslivesCopyright:
Verfügbare Formate
PCA & EPIDURAL ADMINISTRATION
RNURS-033
Required Reading
Skill 13.3: Patient-Controlled Analgesia
13.1: Epidural Analgesia
Objectives
In the classroom, clinical, and/or lab the student will:
Describe how PCA and epidural analgesics are administered and the
advantages and disadvantages of each.
Interpret orders and understand equipment to insure the correct dosage of
medication is administered.
Assess the client for pain control and side effects of medication.
Teach the client:
to assess own pain
how/when to use PCA
pain level management
of right to pain control
Document assessment, pain control, medication administered and any side
effects.
Why PCA & Epidural?
Research shows:
Better pain control
Earlier client ambulation
Higher client satisfaction
PCA:
Definition:
Uses:
Good Candidates:
Poor Candidates:
Commonly used medications:
Route:
Primarily IV, epidural, and SQ
Transdermal
Variations:
PCA Advantages:
More constant serum levels of opioid
Reduced opioid used when client controls when medication administered
Better pain relief
Fewer side effects from opiods
Decreased complications d/t earlier & easier ambulation
Eliminates need for IM analgesics
Allows client to sleep at night while minimizing daytime drowsiness
Allows for client independence
PCA Disadvantages:
Client Related Issues:
Pump Failure:
Operator Related Issues:
Key: careful, ongoing management
Assessments:
Check MD order
Client Allergies
Clients cognitive ability
Clients physical ability
Pain (PQRSTU)
Environment for factors that increase pain
Existing IV infusion line
Presence of Sleep Apnea
Check PCA Infusion Pump Settings at start of Shift by pressing HX Button=>
compare to MD order
Planning:
Expected Outcomes
Delegation Considerations
Narcan
Know dose; dilution; timing
Narcan
Mix 0.4 mg/ml (1 ml amp) in 9 ml of NS (10 ml total volume)
Administer 1 ml of diluted Narcan (0.04 mg/ml) IV stat
Give 1 ml diluted Narcan IV q30-60 sec up to a total of 20 ml (total Narcan dose
0.8 mg/2amps) until sedation level is 2 or respiratory rate is >10/min
Interpretation of MD Order
Loading Dose
Basal Infusion Rate
PCA Dose
Bolus Dose Administered by RN
1-4 Hour Dose Limit
Lockout Interval
Implementation: See Text
Client Education:
Medication
Purpose and Benefits
Side Effects and When to Notify RN
Goal for Pain Control
Demonstrate function of PCA
Lock-out and inability to Overdose
When to use PCA
Attach PCA pump to pole less than 10 inches above infusion site
Attach med syringe and Prime PCA tubing with Morphine or Dilaudid
Prime Primary IV line with NS and insert into IV pump
Connect tubing from PCA pump to Primary Line at Y site closest to patient
Set pump according to MD orders
2 RNs must Independently verify medication, dose & rate & cosign MAR
Medication
Basal infusion rate
PCA dose
1-4 hour lock-out
Lock-out interval
Must re-verify: q8hr; new med syringe, pump setting change
Changing Medication Syringe
Check MD orders
Obtain correct med syringe
Raise top bracket-remove old syringe
Uncap new syringe-place in chamber & slide down bracket
If changing to new medication => change tubing also
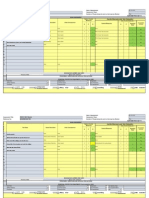
Assessment &
Documentation
15 min post Q 2 hr
& prn
Q4 hr
& prn
Q8 hr
RR
O
2
Saturation
Sedation Level
Concentration
Rate
Pump
1
st
24
hr
After 1
st
24 hr
Pain Intensity Administration of
supplemental
narcotics or
sedatives
IV site for s/s of
infection/infiltration
Medication &
Concentration
PCA Dose
Basal rate
1-4 hr Dose Limit
Lock-Out Interval
# of injections
# of attempts
Total narcotic
administered
(Pump
settings
only)
Sedation Scale
S = asleep
1 = Awake and alert
Action needed:
2 = Slightly drowsy
Action needed:
3 = Frequently drowsy, drifts off during conversation
Action needed:
4 = Somnolent, minimal or no response to physical stimulation
Action needed:
Actions for Sedation Level 3 @ JMCC
DC Continuous/Bolus rate if present
Decrease PCA dose by 50% if no Continuous/Bolus rate
Begin Respiratory Risk Precautions
Notify MD
Respiratory Risk Precautions
Check RR, SpO2, sedation level q 1 hr until scale 2
Call MD if SpO2 <92% & RR <8 and immediately give or increase O2 to max of
6L/min via NC to maintain SpO2>92%
If insufficient,
OxyMask or Non-Rebreather at 8-15 L/min
Notify RT
Notify Rapid Response Team
Notify MD
PCA ADMINISTRATION
Miscellaneous:
Meperidine (Demerol) NOT recommended for PCA
No additional IV/IM/PO narcotics are to be given unless ordered by MD initiating
PCA
Primary Infusion:
Currently infusing compatible fluid @ current rate or
D
5
NS @ 30 ml/hr
Other Meds
Commonly Ordered with PCA
Ondansetron (Zofran) prn nausea
Dephenhydramine (Benadryl) prn itching
Notify MD if itching unrelieved
Docusate sodium (Colace) PO daily
Hold for loose stools
Bisacodyl (Dulcolax) PO daily
Hold for loose stools
What do you do if client pain continues or worsens?
What do you do when the MD orders PCA to be Discontinued?
Even with the lock out factor clients can be overmedicated? Why?
What can you do when the client is overmedicated?
Should PCA be used to treat acute pain in addicted patients?
PCA: Pediatric & Geriatric Considerations
Pediatric:
Age 8-9
Understand concept
Geriatric:
Sensitive to analgesic properties an side effects of opioids
Slow opioid metabolism & excretion
Start low and go slow
What if becomes confused while taking?
EPIDURAL ADMINISTRATION
Definition:
Uses:
Eligible Clients:
Commonly Used Medications:
Opioids; local anesthetics; separately or in combination
Route: Epidural
Patient Controlled?
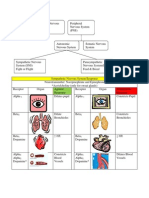
How does it work?
Analgesic is distributed via:
Diffusion through dura mater into CSF
Blood vessels in epidural space transport systemically
Absorption by fat in epidural space creating a depot for slow systemic
release
Analgesic acts by binding to opiate receptors in the dorsal horn of the spinal cord
blocking pain impulse transmission to cerebral cortex
Figure 13-4 Anatomical drawing of epidural space.
Epidural Space:
Space found just outside the dura mater, which is the outermost membrane
covering the spinal cord. There is no direct contact with cerebral spinal fluid in
the epidural space.
Figure 13-5 Placement of epidural catheter.
Advantages of Epidural Administration:
Lower total dose of opioid required to control pain d/t delivery close to site of action
(CNS)
Lower doses of opiods => fewer side effects
Client can ambulate earlier
Client less drowsy
EPIDURAL ADMINISTRATION
Pain Medication ordered by anesthesiologist ONLY
No other narcotics/sedatives except those ordered by anesthesiologist
Deliver MD ordered medication boluses by pump only
Disadvantages of Epidural Administration
Potential for respiratory depression
Potential for catheter migration into subarachnoid space resulting in dangerously
high levels of medication
Urinary retention
Respiratory depression
Motor or sensory changes d/t effect of analgesia on spinal cord transmission below
the level of catheter insertion
Requires frequent monitoring
Clients at Increased Risk for Respiratory Depression Include Those:
Greater than 70 years of age
Receiving concurrent CNS depressants
With renal, hepatic, and/or cardiac impairment
With pulmonary impairment such as sleep apnea, increased intracranial pressure,
COPD, asthma
With upper abdominal or thoracic surgery
With obesity
Respiratory Risk Precautions
Follow those on earlier slide
Common Medications Used
Opioids:
Morphine
Hydromorphone
Fentanyl
Sufentanil
Baseline Assessment
Check MD Order
Client Pain (PQRSTU)
Drug Allergies
Sedation level
Respiratory rate; pattern: depth
BP
Initial motor/sensory function
Insertion site; tubing (patent; secured)
Contraindications:
Use of anticoagulants; herbal meds; abnormal clotting studies; hx of multiple
abscesses; sepsis; skeletal or spinal abnormalities
Planning
Expected Outcomes
Delegation Considerations
Implementation
EQUIPMENT
Medication clearly labeled
Independent Verification: confirm medication, dose & pump settings with another
RN, initially and with any change in rate. 2nd RN cosigns MAR
Pump labeled Epidural ONLY
Tubing with no Y-ports
Pump settings
Dressing change & line removal by anesthesiologist only.
RN may reinforce dressing prn
Assessment/
Documentation
Contin-
uous
15 min. Post q1 hr
& prn
Q2hr
& prn
Q8 hr
&prn
SpO2
Until 12
hr p DC
Pain intensity
Sedation level
RR
SpO2
Concentration
Rate
Pump
1
st
24
hr
Until
12 hr
p DC
Catheter
insertion site
Motor/ sensory
function/CMST
of lower
extremities
BP; pulse
Temp
Med
Concentration
Diluent
Dose/Pump
Setting
Total narcotic
administered
Ongoing Assessment & Documentation
Side Effects:
Urinary retention/constipation
Is/Os; bladder distention
Nausea
Vomiting
Pruritis
Headache
Ongoing Assessment and Documentation
EPIDURAL ADMINISTRATION
Miscellaneous:
Have oxygen equipment, bag/valve/mask, & Narcan available to treat respiratory
depression
Patient located near nursing station for frequent assessment
Check orthostatic BP prior to ambulating for first 24 hr
When to call anesthesiologist
Changes in CMST
Confusion
Continued dizziness
Nausea
Increased heart rate or lightheadedness present with decrease in BP
Any problems with epidural line including catheter leak, disconnection, redness or
drainage at insertion site
Unexpected Outcomes
See Text
What to do if catheter becomes disconnected, or sterility is compromised?
Epidural: Pediatric & Geriatric Considerations
Pediatric
OK all age groups
Dosed per kg
Requires: Continuous cardiac, respiratory, O2 sat monitoring
Geriatric
Beware hypotension esp. in those taking antihypertensives
PCA & EPIDURAL ADMINISTRATION
Review:
Provide acute pain control
Administer correct medication dosage
Interpret orders
Know the equipment
Assess patient for pain and side effects
Teach patient
Documentation
Das könnte Ihnen auch gefallen
- Emergency DrugsDokument10 SeitenEmergency DrugsRoland Mark Rodel LagosNoch keine Bewertungen
- Heart of the Field "Refresher & Nha Certification Quick Notes"Von EverandHeart of the Field "Refresher & Nha Certification Quick Notes"Noch keine Bewertungen
- Dimensional Analysis For Nursing StudentsVon EverandDimensional Analysis For Nursing StudentsNoch keine Bewertungen
- Opioid Analgesics: T. Binder Department of PharmacologyDokument36 SeitenOpioid Analgesics: T. Binder Department of PharmacologywwwrgrobinNoch keine Bewertungen
- Haemodynamic Monitoring & Manipulation: an easy learning guideVon EverandHaemodynamic Monitoring & Manipulation: an easy learning guideNoch keine Bewertungen
- PMS-morphine clinical worksheetDokument1 SeitePMS-morphine clinical worksheetMichael Kuzbyt100% (1)
- Orthopedic Inpatient Protocols: A Guide to Orthopedic Inpatient RoundingVon EverandOrthopedic Inpatient Protocols: A Guide to Orthopedic Inpatient RoundingNoch keine Bewertungen
- Project On SamsungDokument39 SeitenProject On SamsungAbbas0% (1)
- Pain Management in Surgical PatientsDokument35 SeitenPain Management in Surgical Patientssuleman2009100% (1)
- FentanylDokument2 SeitenFentanylKatie McPeek63% (8)
- Line Sets in Oracle Order ManagementDokument9 SeitenLine Sets in Oracle Order ManagementS S PatelNoch keine Bewertungen
- Client Information Sheet (CIS)Dokument10 SeitenClient Information Sheet (CIS)Christine RombawaNoch keine Bewertungen
- Task Based Risk Assesment FormDokument2 SeitenTask Based Risk Assesment FormKolluri SrinivasNoch keine Bewertungen
- Proposed Construction of New Kutulo Airstrip - RetenderDokument112 SeitenProposed Construction of New Kutulo Airstrip - RetenderKenyaAirportsNoch keine Bewertungen
- Oxycodone Acetaminophen PercocetDokument1 SeiteOxycodone Acetaminophen PercocetENoch keine Bewertungen
- Drug MetoprololDokument1 SeiteDrug MetoprololSrkocher0% (1)
- DilaudidDokument2 SeitenDilaudidAdrianne Bazo100% (2)
- Tramadol Drug StudyDokument3 SeitenTramadol Drug StudyAnn Michelle Tarrobago100% (1)
- SEDATION and ANALGESIA in The PICU - Bijapur - Dr. Anand BhutadaDokument64 SeitenSEDATION and ANALGESIA in The PICU - Bijapur - Dr. Anand BhutadacrplzNoch keine Bewertungen
- 15 04 06 SCDokument30 Seiten15 04 06 SCSugarNoch keine Bewertungen
- TIVA - Copy (2) - Copy-1Dokument34 SeitenTIVA - Copy (2) - Copy-1Keerthikumar Parvatha100% (2)
- Employee Training and DevelopmentDokument33 SeitenEmployee Training and DevelopmentMoogii50% (2)
- Sedation in Critically IllDokument32 SeitenSedation in Critically IllSamantha Deshapriya100% (1)
- PCA For ICUDokument41 SeitenPCA For ICUMarina ShliginNoch keine Bewertungen
- Pca PP Revised 6 4 14 v6Dokument12 SeitenPca PP Revised 6 4 14 v6api-244230664Noch keine Bewertungen
- Postoperative AnalgesiaDokument38 SeitenPostoperative AnalgesiaKomella PrakasamNoch keine Bewertungen
- ICU Sedation and Analgesia GuideDokument10 SeitenICU Sedation and Analgesia GuideAvi CNoch keine Bewertungen
- Factors Influencing PainDokument81 SeitenFactors Influencing Painlorella_abejuelaNoch keine Bewertungen
- Patient Controlled AnalgesiaDokument35 SeitenPatient Controlled AnalgesiamochkurniawanNoch keine Bewertungen
- 5 Dosages, Solution & CalculationDokument50 Seiten5 Dosages, Solution & CalculationPrince Rener Velasco PeraNoch keine Bewertungen
- Patient Controlled AnalgesiaDokument26 SeitenPatient Controlled AnalgesiaSabah AlungalNoch keine Bewertungen
- COX-2 Inhibitors: Examples Parecoxib (Dynastat) Celecoxib (Celebrex) Etoricoxib (Arcoxia)Dokument31 SeitenCOX-2 Inhibitors: Examples Parecoxib (Dynastat) Celecoxib (Celebrex) Etoricoxib (Arcoxia)Ben Man JunNoch keine Bewertungen
- Spontaneous Awakening Trial PDFDokument1 SeiteSpontaneous Awakening Trial PDFyonoNoch keine Bewertungen
- Catapres Clonidine Drug CardDokument1 SeiteCatapres Clonidine Drug CardSheri490Noch keine Bewertungen
- Pca PP Revised 7 7 14 v7Dokument12 SeitenPca PP Revised 7 7 14 v7api-244230664Noch keine Bewertungen
- MEDICATION: Generic: Albuterol Trade: Proventil HFA, Ventolin DiskusDokument2 SeitenMEDICATION: Generic: Albuterol Trade: Proventil HFA, Ventolin Diskuszhulieta angovaNoch keine Bewertungen
- Phenergan (Promethazine)Dokument1 SeitePhenergan (Promethazine)E100% (1)
- Intro Anesthesia 2019 Drugs WebDokument38 SeitenIntro Anesthesia 2019 Drugs WebAbiNoch keine Bewertungen
- Nclex 3 With RationaleDokument13 SeitenNclex 3 With RationaleMsPocketbook HoarderNoch keine Bewertungen
- Patient Management Flow Chart: Appt W/ Bronchoscopist PFT/ P&H/StabilityDokument7 SeitenPatient Management Flow Chart: Appt W/ Bronchoscopist PFT/ P&H/StabilityKinnari PatelNoch keine Bewertungen
- Sedation and Analgesia ProtocolDokument5 SeitenSedation and Analgesia ProtocolBoston GunawanNoch keine Bewertungen
- NCP and RX StudyDokument13 SeitenNCP and RX StudyBinhafez Camlian DalhaniNoch keine Bewertungen
- XopenexDokument1 SeiteXopenexKatie McPeekNoch keine Bewertungen
- Ventilator Management ProtocolDokument15 SeitenVentilator Management Protocolihtisham1Noch keine Bewertungen
- Pain MXDokument7 SeitenPain MXRezaul KarimNoch keine Bewertungen
- Med Name: Mechanism of Action: Dosage: 10 MG Daily Priority Med Specific Patient TeachingDokument6 SeitenMed Name: Mechanism of Action: Dosage: 10 MG Daily Priority Med Specific Patient TeachingBrittany BennettNoch keine Bewertungen
- Managing pain with PercocetDokument2 SeitenManaging pain with PercocetKay TaylorNoch keine Bewertungen
- Patient Controlled AnalgesiaDokument129 SeitenPatient Controlled AnalgesiamehranerezvaniNoch keine Bewertungen
- DYSNEA ASSESSMENTDokument2 SeitenDYSNEA ASSESSMENTKang Opik TaufikNoch keine Bewertungen
- Med Template - Hydro Morph One Hydro Chloride (Hydromorphone Contin, Dilaudid)Dokument2 SeitenMed Template - Hydro Morph One Hydro Chloride (Hydromorphone Contin, Dilaudid)Ashlee KeeferNoch keine Bewertungen
- Practice - Exam - .Docx 8Dokument1 SeitePractice - Exam - .Docx 8jaloaliniskiNoch keine Bewertungen
- Naloxone (Narcan)Dokument2 SeitenNaloxone (Narcan)Adrianne BazoNoch keine Bewertungen
- Case Study 1Dokument3 SeitenCase Study 1Amberly BohackNoch keine Bewertungen
- DarvacetDokument1 SeiteDarvacetAdrianne BazoNoch keine Bewertungen
- NCP PROPER Pain and Decreased Cardiac OutputDokument3 SeitenNCP PROPER Pain and Decreased Cardiac OutputErienne Lae Manangan - CadalsoNoch keine Bewertungen
- JCI Accreditation Presentation 3Dokument77 SeitenJCI Accreditation Presentation 3Osama MarzoukNoch keine Bewertungen
- Ketamine Infusion For CRPS or Opioid Weaning GuidelineDokument14 SeitenKetamine Infusion For CRPS or Opioid Weaning GuidelineAlia SandoQaNoch keine Bewertungen
- Night Float VADokument9 SeitenNight Float VAkirNoch keine Bewertungen
- Drug Study: PART 1: To Be Completed Prior To Clinical ExperienceDokument5 SeitenDrug Study: PART 1: To Be Completed Prior To Clinical ExperienceFrozanSNoch keine Bewertungen
- Epidurals & PCAs: Understanding Pain Management OptionsDokument19 SeitenEpidurals & PCAs: Understanding Pain Management OptionsAdrian RodriguezNoch keine Bewertungen
- MEDICAL MANAGEMENTDokument12 SeitenMEDICAL MANAGEMENTMaricris Tubig LeritNoch keine Bewertungen
- DrugsDokument5 SeitenDrugsnurse_nurseNoch keine Bewertungen
- Symph A To Mimetic SDokument27 SeitenSymph A To Mimetic Sjl frusaNoch keine Bewertungen
- Neonatal Icu Skills ChecklistDokument5 SeitenNeonatal Icu Skills ChecklistsparticuslivesNoch keine Bewertungen
- Today 5Dokument1 SeiteToday 5sparticuslivesNoch keine Bewertungen
- CEN Brochure SAFH InformationDokument3 SeitenCEN Brochure SAFH InformationsparticuslivesNoch keine Bewertungen
- Expense Analysis WorksheetDokument2 SeitenExpense Analysis WorksheetsparticuslivesNoch keine Bewertungen
- Expense Analysis WorksheetDokument2 SeitenExpense Analysis WorksheetsparticuslivesNoch keine Bewertungen
- CEN Brochure SAFH InformationDokument3 SeitenCEN Brochure SAFH InformationsparticuslivesNoch keine Bewertungen
- Expense Analysis WorksheetDokument2 SeitenExpense Analysis WorksheetsparticuslivesNoch keine Bewertungen
- Expense Analysis WorksheetDokument2 SeitenExpense Analysis WorksheetsparticuslivesNoch keine Bewertungen
- Cardiovascular ReviewDokument8 SeitenCardiovascular ReviewsparticuslivesNoch keine Bewertungen
- EndocrineDokument2 SeitenEndocrinesparticuslivesNoch keine Bewertungen
- Expense Analysis WorksheetDokument2 SeitenExpense Analysis WorksheetsparticuslivesNoch keine Bewertungen
- Cardiovascular ReviewDokument8 SeitenCardiovascular ReviewsparticuslivesNoch keine Bewertungen
- EndocrineDokument2 SeitenEndocrinesparticuslivesNoch keine Bewertungen
- EndocrineDokument2 SeitenEndocrinesparticuslivesNoch keine Bewertungen
- EndocrineDokument2 SeitenEndocrinesparticuslivesNoch keine Bewertungen
- Criteria For INACTIVE MRSA StatusDokument2 SeitenCriteria For INACTIVE MRSA StatussparticuslivesNoch keine Bewertungen
- Cardiovascular ReviewDokument8 SeitenCardiovascular ReviewsparticuslivesNoch keine Bewertungen
- Cardiovascular ReviewDokument8 SeitenCardiovascular ReviewsparticuslivesNoch keine Bewertungen
- Explanation of AbbreviationsDokument1 SeiteExplanation of AbbreviationssparticuslivesNoch keine Bewertungen
- Vascular Disorders CH 38Dokument6 SeitenVascular Disorders CH 38sparticuslives100% (1)
- Vascular Disorders CH 38Dokument6 SeitenVascular Disorders CH 38sparticuslives100% (1)
- Explanation of AbbreviationsDokument1 SeiteExplanation of AbbreviationssparticuslivesNoch keine Bewertungen
- CNS PNS Autonomic Nervous Systems SNS PNS Receptors ResponsesDokument3 SeitenCNS PNS Autonomic Nervous Systems SNS PNS Receptors ResponsesKara Dawn MasonNoch keine Bewertungen
- Vascular Disorders CH 38Dokument6 SeitenVascular Disorders CH 38sparticuslives100% (1)
- ANS ChartDokument3 SeitenANS ChartsparticuslivesNoch keine Bewertungen
- CNS PNS Autonomic Nervous Systems SNS PNS Receptors ResponsesDokument3 SeitenCNS PNS Autonomic Nervous Systems SNS PNS Receptors ResponsesKara Dawn MasonNoch keine Bewertungen
- PCA and Epidural Presentation Outline 2014Dokument10 SeitenPCA and Epidural Presentation Outline 2014sparticuslives100% (1)
- Explanation of AbbreviationsDokument1 SeiteExplanation of AbbreviationssparticuslivesNoch keine Bewertungen
- Explanation of AbbreviationsDokument1 SeiteExplanation of AbbreviationssparticuslivesNoch keine Bewertungen
- Refractomax 521 Refractive Index Detector: FeaturesDokument2 SeitenRefractomax 521 Refractive Index Detector: FeaturestamiaNoch keine Bewertungen
- Chapter 4-Ohm's LawDokument12 SeitenChapter 4-Ohm's LawErin LoveNoch keine Bewertungen
- Mid Semester ExaminationDokument2 SeitenMid Semester ExaminationMOHAMMED RIHANNoch keine Bewertungen
- Piroxicam (Wikipedia)Dokument4 SeitenPiroxicam (Wikipedia)Adrian ArnasaputraNoch keine Bewertungen
- MCQ 14 Communication SystemsDokument21 SeitenMCQ 14 Communication SystemsXeverus RhodesNoch keine Bewertungen
- Daa M-4Dokument28 SeitenDaa M-4Vairavel ChenniyappanNoch keine Bewertungen
- GE's Two-Decade Transformation: Jack Welch's Leadership: Amanda Rodriguez Patricia Robledo Brittany Culberson Yue JiangDokument34 SeitenGE's Two-Decade Transformation: Jack Welch's Leadership: Amanda Rodriguez Patricia Robledo Brittany Culberson Yue JiangRishendra Singh RathourNoch keine Bewertungen
- OTA710C User ManualDokument32 SeitenOTA710C User ManualEver Daniel Barreto Rojas100% (2)
- 7 ways to improve energy efficiency of pumpsDokument1 Seite7 ways to improve energy efficiency of pumpsCharina Malolot VillalonNoch keine Bewertungen
- Lecture 2 Leader-Centred PerspectivesDokument24 SeitenLecture 2 Leader-Centred PerspectivesLIVINGSTONE CAESARNoch keine Bewertungen
- Project IGI 2 Cheat Codes, Hints, and HelpDokument4 SeitenProject IGI 2 Cheat Codes, Hints, and Helppadalakirankumar60% (5)
- What Is Propaganda DeviceDokument3 SeitenWhat Is Propaganda DeviceGino R. Monteloyola100% (1)
- Holmes 1993Dokument8 SeitenHolmes 1993Rumaisa KrubaNoch keine Bewertungen
- Smart Card PresentationDokument4 SeitenSmart Card PresentationNitika MithalNoch keine Bewertungen
- 2021 A Review of Image Based Pavement Crack Detection AlgorithmsDokument7 Seiten2021 A Review of Image Based Pavement Crack Detection Algorithmsgandhara11Noch keine Bewertungen
- Rural Perception of SUV CarsDokument29 SeitenRural Perception of SUV CarsritusinNoch keine Bewertungen
- Siemens ProjectDokument17 SeitenSiemens ProjectMayisha Alamgir100% (1)
- Indian companies involved in trade dispute caseDokument15 SeitenIndian companies involved in trade dispute caseakshay daymaNoch keine Bewertungen
- How To Block Facebook in Mikrotik Using L7 Protocols (Layer 7) - Lazy Geek - )Dokument11 SeitenHow To Block Facebook in Mikrotik Using L7 Protocols (Layer 7) - Lazy Geek - )oscar_198810Noch keine Bewertungen
- Dhabli - 1axis Tracker PVSYSTDokument5 SeitenDhabli - 1axis Tracker PVSYSTLakshmi NarayananNoch keine Bewertungen
- Rheomix 141Dokument5 SeitenRheomix 141Haresh BhavnaniNoch keine Bewertungen
- Understanding Nominal Pipe Sizes (NPS) and Pipe DimensionsDokument39 SeitenUnderstanding Nominal Pipe Sizes (NPS) and Pipe DimensionsprathikNoch keine Bewertungen
- Consumer Preference and Demand For Rice Grain QualityDokument38 SeitenConsumer Preference and Demand For Rice Grain QualityIRRI_SSDNoch keine Bewertungen
- Sys Admin Guide Xerox WorkCentre 7775Dokument185 SeitenSys Admin Guide Xerox WorkCentre 7775dankorzon1Noch keine Bewertungen