Beruflich Dokumente
Kultur Dokumente
RM MN PN 8 CHP 6
Hochgeladen von
adadan0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
50 Ansichten12 SeitenHIV is a retrovirus that attacks and causes destruction of T lymphocytes. It causes immunosuppression in clients. HIV is transmitted from mothers to the fetus perinatally through the placenta.
Originalbeschreibung:
Originaltitel
Rm Mn Pn 8 Chp 6
Copyright
© © All Rights Reserved
Verfügbare Formate
PDF, TXT oder online auf Scribd lesen
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenHIV is a retrovirus that attacks and causes destruction of T lymphocytes. It causes immunosuppression in clients. HIV is transmitted from mothers to the fetus perinatally through the placenta.
Copyright:
© All Rights Reserved
Verfügbare Formate
Als PDF, TXT herunterladen oder online auf Scribd lesen
0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
50 Ansichten12 SeitenRM MN PN 8 CHP 6
Hochgeladen von
adadanHIV is a retrovirus that attacks and causes destruction of T lymphocytes. It causes immunosuppression in clients. HIV is transmitted from mothers to the fetus perinatally through the placenta.
Copyright:
© All Rights Reserved
Verfügbare Formate
Als PDF, TXT herunterladen oder online auf Scribd lesen
Sie sind auf Seite 1von 12
chapter 6 INFECTIONS
PN MATERNAL NEWBORN NURSING 71
UNIT 1 ANTEPARTUM NURSING CARE
Section: Complications of Pregnancy
Chapter 6 Infections
Overview
Maternal infections during pregnancy require prompt identication and treatment.
Infections that may affect pregnant clients include HIV, TORCH infections, streptococcus
-hemolytic, Group B, chlamydia, gonorrhea, and Candida albicans.
HIV/AIDS
Overview
HIV is a retrovirus that attacks and causes destruction of T lymphocytes. It causes
immunosuppression in clients. HIV is transmitted from mothers to the fetus perinatally
through the placenta and postnatally to newborns through the breast milk.
Routine laboratory testing in the early prenatal period includes testing for HIV. Early
identication and treatment signicantly decreases the incidence of perinatal transmission.
Testing is also recommended in the third trimester for clients who are at an increased risk.
Use of internal fetal monitors, vacuum extraction, and forceps during labor should be
avoided in clients who are HIV positive because of the risk of fetal bleeding.
Injections and blood testing should not take place until the rst bath is given to newborns
of mothers who are HIV positive.
Data Collection
Risk Factors
IV drug use
Multiple sexual partners
Bisexuality
Maternal history of multiple STIs
Blood transfusion (rare occurrence)
INFECTIONS
72 PN MATERNAL NEWBORN NURSING
Subjective Data
Fatigue
Objective Data
Physical assessment ndings
Diarrhea
Weight loss
Anemia
Laboratory tests
Testing begins with an antibody screening test such as enzyme immunoassay.
Conrmation of positive results is conrmed by Western blot testing.
Screen clients for STIs such as gonorrhea, Chlamydia, syphilis, and
hepatitis B.
Obtain frequent viral load levels and CD4 cell counts throughout the pregnancy
of mothers who are HIV positive.
Collaborative Care
Nursing Care
Provide support prior to and after testing.
Use standard precautions.
Administer antiviral combination therapy as prescribed.
Medications
Retrovir (Zidovudine)
Antiretroviral agent
Nucleoside reverse transcriptase inhibitor
Nursing Considerations
Start administration of retrovir after the rst trimester and continue
throughout the pregnancy.
Administer retrovir to newborns following delivery and for 6 weeks
following.
Interdisciplinary care
Request referral for clients to a mental health counselor, legal assistance, and nancial
resources if indicated.
INFECTIONS
PN MATERNAL NEWBORN NURSING 73
Care After Discharge
Client education
Instruct clients not to breastfeed.
Discuss safe sexual relations with clients.
Client Outcomes
The client will remain free from injury during pregnancy.
TORCH INFECTIONS
Overview
TORCH is an acronym for a group of infections that can negatively affect women who are
pregnant. These infections can cross the placenta and have teratogenic affects on the fetus.
Data Collection
Risk Factors
Toxoplasmosis is caused by consumption of raw or undercooked meat or handling cat
feces.
Rubella (German measles) is transmitted by droplet transmission of nasopharyngeal
secretions of individuals who are infected. The virus is also present in blood, stool, and
urine.
Cytomegalovirus (member of herpes virus family) is transmitted by droplet
transmission and is found in semen, cervical and vaginal secretions, breast milk,
placental tissue, urine, feces, and blood. Latent virus may be reactivated and cause
disease to the fetus in utero or during passage through the birth canal.
Herpes simplex virus (HSV) is spread by direct contact with oral or genital lesions.
Transmission to the fetus is greatest during vaginal birth if the woman has active
lesions.
Subjective Data
Toxoplasmosis symptoms similar to inuenza or lymphadenopathy
Reports of malaise, muscle aches, (u-like symptoms)
Rubella
Reports of joint and muscle pain
Cytomegalovirus is usually asymptomatic.
Herpes simplex virus
Reports of dysuria, malaise, fever, chills and numerous painful genital lesions
INFECTIONS
74 PN MATERNAL NEWBORN NURSING
Objective Data
Physical assessment ndings
Signs of toxoplasmosis include fever and tender lymph nodes.
Signs of rubella include rash, mild lymphedema, fever, and fetal consequences,
which include miscarriage, congenital anomalies, and death.
Herpes simplex virus initially presents with macules and papules that progress to
purulent vesicles.
View Media Supplement: Herpes Simplex Type 2 (Image)
Laboratory tests
For herpes simplex, obtain cultures from women who have HSV or are at or near
term.
Diagnostic procedures
A TORCH screen is an immunologic survey that is used to identify the existence
of these infections in mothers (to identify fetal risks) or in newborns (detection of
antibodies against infections).
Collaborative Care
Nursing Care
Monitor fetal well-being.
Educate clients on prevention practices including good hand hygiene and cooking
meat properly.
Medications
Administer antibiotics as prescribed.
For toxoplasmosis treatment, include sulfonamides or a combination of
pyrimethamine and sulfadiazine (potentially harmful to the fetus, but parasitic
treatment essential).
Care After Discharge
Client education
Instruct pregnant clients with rubella to avoid groups of young children.
Encourage clients with low rubella titers to receive immunizations prior to their
next pregnancy (usually done prior to discharge from the hospital after delivery).
Clients need to wait 4 weeks after immunization to become pregnant.
Reinforce the need for clients to adhere to the complete prescribed treatment.
Provide clients with emotional support.
INFECTIONS
PN MATERNAL NEWBORN NURSING 75
Client Outcomes
Clients will be free of clinical ndings indicating viral complications are affecting the
pregnancy.
STREPTOCOCCUS BETA-HEMOLYTIC, GROUP B
Overview
Streptococcus -hemolytic, Group B (GBS) is a bacterial infection that can be passed to
newborns during labor and delivery.
Data Collection
Risk Factors
History of positive culture with previous pregnancy
Risk factors for neonatal GBS
Positive culture with pregnancy
Prolonged rupture of membranes
Preterm delivery
Objective Data
Physical assessment ndings
Positive GBS may have maternal and fetal effects including premature rupture
of membranes, preterm labor and delivery, chorioamnionitis, infections of the
urinary tract, and maternal sepsis.
Laboratory tests
Vaginal and rectal cultures are performed between 35 to 37 weeks of gestation.
Collaborative Care
Nursing Care
Administer prophylaxis antibiotics during labor.
Medications
Penicillin G or ampicillin (Principen) may be prescribed as intermittent IV bolus to
treat positive GBS.
Care After Discharge
Client education
Instruct clients to monitor for signs of infection and to report to the provider.
INFECTIONS
76 PN MATERNAL NEWBORN NURSING
Client Outcomes
The newborns blood culture is negative for GBS with no clinical signs of sepsis.
CHLAMYDIA
Overview
Chlamydia is a bacterial infection caused by Chlamydia trachomatis. It is the most
common STI. The infection is often difcult to diagnose because it is typically
asymptomatic. According to current guidelines from the Centers for Disease Control and
Prevention, all women and adolescents ages 20 to 25 who are sexually active should be
screened for STIs.
Data Collection
Risk Factors
Multiple sexual partners
Unprotected sexual practices
Subjective Data
Vaginal spotting
Vulvar itching
Objective Data
Physical assessment ndings
White, watery vaginal discharge
Laboratory tests
Endocervical culture
Collaborative Care
Nursing Care
Instruct clients to take the entire prescription as prescribed.
Identify and treat all sexual partners.
Retest clients who are pregnant in 3 weeks after completing the prescribed regimen.
Medications
Azithromycin (Zithromax), amoxicillin (Amoxil), and erythromycin (Ery-Tab) are
prescribed during pregnancy.
Broad-spectrum antibiotic
Bactericidal action
INFECTIONS
PN MATERNAL NEWBORN NURSING 77
Nursing Considerations
Administer 0.5% erythromycin ophthalmic ointment to all newborns
following delivery. This antibiotic is both bacteriostatic and bactericidal,
thus it provides prophylaxis against Neisseria gonorrhoeae and Chlamydia
trachomatis.
Care After Discharge
Client education
Instruct clients to take all prescription as prescribed.
Educate clients about the possibility of decreasing effectiveness of oral
contraceptives.
Client Outcomes
The client will be free of clinical ndings of infection.
GONORRHEA
Overview
Neisseria gonorrhoeae is the causative agent of gonorrhea. Gonorrhea is a bacterial
infection that is primarily spread by genital-to-genital contact. However, it can also be
spread by anal-to-genital contact or oral-to-genital contact. It can also be transmitted to a
neonate during delivery. Women are frequently asymptomatic.
Data Collection
Risk Factors
Multiple sexual partners
Unprotected sexual practices
Subjective Data (Male)
Urethral discharge
Painful urination
Frequency
Subjective Data (Female)
Lower abdominal pain
Dysmenorrhea
Objective Data Male/Female
Physical assessment ndings
Urethral discharge
Yellowish-green vaginal discharge
INFECTIONS
78 PN MATERNAL NEWBORN NURSING
Reddened vulva and vaginal walls
If gonorrhea is left untreated, it can cause pelvic inammatory disease, heart
disease, and arthritis.
Laboratory tests
Urethral and vaginal cultures
Urine culture
Collaborative Care
Nursing Care
Provide clients education regarding disease transmission.
Instruct clients to take the entire prescription as prescribed.
Identify and treat all sexual partners.
Medications
Ceftriaxone (Rocephin) IM or azithromycin (Zithromax) PO
Given for 7 days
Broad-spectrum antibiotic
Bactericidal action
Care After Discharge
Client education
Instruct clients to nish all prescribed medications.
Instruct clients to repeat the culture to assess for medication effectiveness.
Educate clients regarding safe-sex practices.
Client Outcomes
The client will be free of clinical ndings of infection.
CANDIDA ALBICANS
Overview
A fungal infection caused by Candida albicans.
Data Collection
Risk Factors
Diabetes mellitus
Oral contraceptives
Recent antibiotic treatment
INFECTIONS
PN MATERNAL NEWBORN NURSING 79
Subjective Data
Vulvar itching
Objective Data
Physical assessment ndings
Thick, creamy white vaginal discharge
Vulvar redness
White patches on vaginal walls
Gray-white patches on the tongue and gums (newborns)
Laboratory tests
Wet prep
Diagnostic procedures
Potassium hydroxide (KOH) prep
Presence of hyphae and pseudohyphae indicates positive ndings
Collaborative Care
Nursing Care
Medications
Over-the-counter treatments, such as clotrimazole (Gyne-Lotrimin) or miconazole
(Monistat), are available to treat candidiasis. However, it is important for the
provider to diagnosis candidiasis initially.
Care After Discharge
Client education
Administer medication as prescribed.
Client Outcomes
The client will be free of clinical ndings of infection.
INFECTIONS
80 PN MATERNAL NEWBORN NURSING
APPLICATION EXERCISES
1. A nurse is admitting a client in labor to the obstetrical unit. The client has a positive human
immunodeciency virus (HIV) status. Discuss the contraindications for this client.
2. A nurse in an antepartum clinic is providing care for a client. Which of the following clinical
ndings are suggestive of gonorrhea? (Select all that apply.)
Dysmenorrhea
Yellowish-green vaginal discharge
Reddened vulva
Malaise
Lower abdominal pain
3. A nurse is caring for a pregnant client diagnosed with chlamydia. Which of the following
medications does the nurse anticipate the provider will prescribe? (Select all that apply.)
Ceftriaxone (Rocephin)
Azithromycin (Zithromax)
Amoxicillin (Amoxil)
Metronidazole (Flagyl)
Erythromycin (Ery-Tab)
4. A nurse is caring for a pregnant client diagnosed with human immunodeciency virus (HIV).
Which of the following medications does the nurse anticipate the provider will prescribe?
A. Ceftriaxone (Rocephin)
B. Retrovir (Zidovudine)
C. Metronidazole (Flagyl)
D. Tetracycline (Sumycin)
5. A nurse in an antepartum clinic is reviewing the laboratory reports of several clients. The nurse
is aware that which of the following infections have medications that can be prescribed as
prophylactic treatment during labor or immediately following delivery? (Select all that apply.)
Gonorrhea
Chlamydia
HIV
Group B Strep
TORCH
INFECTIONS
PN MATERNAL NEWBORN NURSING 81
APPLICATION EXERCISES ANSWER KEY
1. A nurse is admitting a client in labor to the obstetrical unit. The client has a positive human
immunodeciency virus (HIV) status. Discuss the contraindications for this client.
Episiotomy is contraindicated for HIV-positive clients due to the risk of maternal blood
exposure. Additionally, the use of internal fetal monitors, vacuum extraction, and forceps
during labor should be avoided because of the risk of fetal bleeding.
NCLEX
Connection: Physiological Adaptation, Alterations in Body Systems
2. A nurse in an antepartum clinic is providing care for a client. Which of the following clinical
ndings are suggestive of gonorrhea? (Select all that apply.)
X
Dysmenorrhea
X
Yellowish-green vaginal discharge
X
Reddened vulva
Malaise
X
Lower abdominal pain
Symptoms of gonorrhea include reports of dysmenorrhea and lower abdominal pain.
Objective ndings include yellowish-green vaginal discharge and reddened vulva and
vaginal walls. Malaise is not a clinical nding associated with gonorrhea.
NCLEX
Connection: Physiological Adaptation, Alterations in Body Systems
3. A nurse is caring for a pregnant client diagnosed with chlamydia. Which of the following
medications does the nurse anticipate the provider will prescribe? (Select all that apply.)
Ceftriaxone (Rocephin)
X
Azithromycin (Zithromax)
X
Amoxicillin (Amoxil)
Metronidazole (Flagyl)
X
Erythromycin (Ery-Tab)
Azithromycin, amoxicillin, and erythromycin are prescribed during pregnancy to treat
Chlamydia.
NCLEX
Connection: Pharmacological Therapies, Expected Actions/Outcomes
INFECTIONS
82 PN MATERNAL NEWBORN NURSING
4. A nurse is caring for a pregnant client diagnosed with human immunodeciency virus (HIV).
Which of the following medications does the nurse anticipate the provider will prescribe?
A. Ceftriaxone (Rocephin)
B. Retrovir (Zidovudine)
C. Metronidazole (Flagyl)
D. Tetracycline (Sumycin)
Retrovir (Zidovudine) is prescribed for the treatment of HIV. Start administration of
retrovir after the rst trimester and continue throughout the pregnancy. Additionally, it is
prescribed to the neonate following delivery and for 6 weeks. Ceftriaxone (Rocephin) IM is
prescribed for the treatment of gonorrhea. Metronidazole (Flagyl) is used in the treatment
of bacterial vaginosis and trichomoniasis. Tetracycline (Sumycin) is used to treat syphilis.
NCLEX
Connection: Physiological Adaptation, Alterations in Body Systems
5. A nurse in an antepartum clinic is reviewing the laboratory reports of several clients. The nurse
is aware that which of the following infections have medications that can be prescribed as
prophylactic treatment during labor or immediately following delivery? (Select all that apply.)
X
Gonorrhea
X
Chlamydia
X
HIV
X
Group B Strep
TORCH
Erythromycin is the medication of choice for ophthalmia neonatorum. This antibiotic
is both bacteriostatic and bactericidal, thus providing prophylaxis against Neisseria
gonorrhoeae and Chlamydia trachomatis. It is administrated to the neonate immediately
following delivery. Retrovir (Zidovudine) is prescribed to the client in labor who is
HIV positive. It is also administered to the newborn following delivery and for 6 weeks
thereafter. Penicillin G or ampicillin may be prescribed to treat positive GBS.
NCLEX
Connection: Physiological Adaptation, Alterations in Body Systems
Das könnte Ihnen auch gefallen
- PublicHealthEmerging IssuesDokument13 SeitenPublicHealthEmerging IssuesadadanNoch keine Bewertungen
- Acc 3121Dokument8 SeitenAcc 3121adadanNoch keine Bewertungen
- Acetaminphen Overdose Treatment InfoDokument19 SeitenAcetaminphen Overdose Treatment InfoadadanNoch keine Bewertungen
- Crash Assessment For Field Triage: "Rules and Exceptions"Dokument99 SeitenCrash Assessment For Field Triage: "Rules and Exceptions"adadanNoch keine Bewertungen
- Central Venous Access DevicesDokument3 SeitenCentral Venous Access DevicesadadanNoch keine Bewertungen
- Crash Assessment For Field Triage: "Rules and Exceptions"Dokument99 SeitenCrash Assessment For Field Triage: "Rules and Exceptions"adadanNoch keine Bewertungen
- DoffingBiologicalPPE EbolaPatients 8.5x11 CC v1.01Dokument6 SeitenDoffingBiologicalPPE EbolaPatients 8.5x11 CC v1.01adadanNoch keine Bewertungen
- Nurse Practice ActDokument85 SeitenNurse Practice Actadadan100% (1)
- Hurst Review Services - Live Review ScheduleDokument2 SeitenHurst Review Services - Live Review Scheduleadadan100% (1)
- 21 Day Bikini BodyDokument4 Seiten21 Day Bikini BodydocumentexchangeonlyNoch keine Bewertungen
- Web QsenDokument2 SeitenWeb QsenadadanNoch keine Bewertungen
- SchizophreniaDokument5 SeitenSchizophreniaadadanNoch keine Bewertungen
- Lab ValuesDokument8 SeitenLab Valuesjdub4yaNoch keine Bewertungen
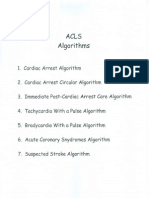
- Acls AlgorithmsDokument8 SeitenAcls Algorithmsdydy_7193Noch keine Bewertungen
- RespiratoryDokument34 SeitenRespiratoryadadan100% (1)
- ADN Student HandbookDokument101 SeitenADN Student HandbookadadanNoch keine Bewertungen
- Nursing Report Sheet TemplateDokument1 SeiteNursing Report Sheet TemplateadadanNoch keine Bewertungen
- Shaken Baby Syndrome (SBS)Dokument18 SeitenShaken Baby Syndrome (SBS)adadanNoch keine Bewertungen
- P 527Dokument10 SeitenP 527adadanNoch keine Bewertungen
- Hepatobiliary DisordersDokument11 SeitenHepatobiliary DisordersadadanNoch keine Bewertungen
- Exceptional Dentistry: Beverly Rose D.M.D.Dokument1 SeiteExceptional Dentistry: Beverly Rose D.M.D.adadanNoch keine Bewertungen
- NLN Pharmacology Study Guide Final 6-3-2013Dokument65 SeitenNLN Pharmacology Study Guide Final 6-3-2013الأغا محمد زكارنة100% (2)
- Clinical Pathway Acute Psych BehavioralDokument3 SeitenClinical Pathway Acute Psych Behavioraladadan100% (2)
- DoffingBiologicalPPE EbolaPatients 8.5x11 CC v1.01Dokument6 SeitenDoffingBiologicalPPE EbolaPatients 8.5x11 CC v1.01adadanNoch keine Bewertungen
- Chapter 057Dokument2 SeitenChapter 057adadanNoch keine Bewertungen
- Parkinson Professional GuideDokument172 SeitenParkinson Professional GuideGibran Ilham100% (2)
- BA MA ComparisonDokument32 SeitenBA MA ComparisonadadanNoch keine Bewertungen
- Connections: Nursing Practice ApplicationDokument3 SeitenConnections: Nursing Practice ApplicationadadanNoch keine Bewertungen
- Biographical InformationDokument1 SeiteBiographical InformationadadanNoch keine Bewertungen
- Lab ReferencesDokument8 SeitenLab ReferencesadadanNoch keine Bewertungen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- History of AutismDokument3 SeitenHistory of AutismTasy BvNoch keine Bewertungen
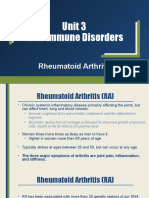
- Unit 3 Part 2 Rheumatoid ArthritisDokument10 SeitenUnit 3 Part 2 Rheumatoid ArthritisReman AlingasaNoch keine Bewertungen
- Chronic Hepatitis BDokument5 SeitenChronic Hepatitis BMurat HessesNoch keine Bewertungen
- Plastic SurgeryDokument5 SeitenPlastic Surgeryhasif21Noch keine Bewertungen
- Immunology Lab Worksheet StudentDokument6 SeitenImmunology Lab Worksheet StudentBNoch keine Bewertungen
- 1 - Mattu, Amal ECGsDokument68 Seiten1 - Mattu, Amal ECGsKhan A Reh50% (2)
- Dnb-General Surgery: Competency Based Training ProgrammeDokument49 SeitenDnb-General Surgery: Competency Based Training ProgrammeLakshmi Mounica Grandhi100% (1)
- 4 EL Husseinys Essentials of Cardiovascular System @eduwaves360Dokument236 Seiten4 EL Husseinys Essentials of Cardiovascular System @eduwaves360ahmed_abu_alrobNoch keine Bewertungen
- Hayashi Reiki ManualDokument14 SeitenHayashi Reiki Manualboomerb100% (4)
- Dengue Infection During Pregnancy andDokument7 SeitenDengue Infection During Pregnancy andAlia SalviraNoch keine Bewertungen
- Modul Normal Delivery 2016Dokument8 SeitenModul Normal Delivery 2016Alvin FarhanNoch keine Bewertungen
- Level 2 (Complete) Ppe Donning-Doffing ChecklistDokument2 SeitenLevel 2 (Complete) Ppe Donning-Doffing ChecklistALIMBOYOGUEN RexorNoch keine Bewertungen
- PEH 3 Lesson 2Dokument3 SeitenPEH 3 Lesson 2ShaineMaiko MarigocioNoch keine Bewertungen
- Procedimento Implante Dura IIDokument6 SeitenProcedimento Implante Dura IIapi-3762376Noch keine Bewertungen
- Cardiovascular Physiology MCQDokument11 SeitenCardiovascular Physiology MCQJessi ObibiNoch keine Bewertungen
- Newborn Care: A Newborn Baby or Animal Is One That Has Just Been BornDokument26 SeitenNewborn Care: A Newborn Baby or Animal Is One That Has Just Been BornJenny-Vi Tegelan LandayanNoch keine Bewertungen
- Vaginal MicrobiomeDokument9 SeitenVaginal MicrobiomeRika Yulizah GobelNoch keine Bewertungen
- Submental Abscess After Deoxycholic Acid Injection: ReferenceDokument1 SeiteSubmental Abscess After Deoxycholic Acid Injection: Referencechash75Noch keine Bewertungen
- Anatomy & Physiology: For Health Professions: An Interactive JourneyDokument60 SeitenAnatomy & Physiology: For Health Professions: An Interactive JourneyEllani A RoldanNoch keine Bewertungen
- Starting Intravenous LinesDokument7 SeitenStarting Intravenous LinesPhillip CharlesNoch keine Bewertungen
- Nursing Care Plan: Valiente, Ana Ambianca S. Maristela, Aony Jamaine Y. Tabora, Elyza M. Quitlong, Jennifer N. BSN 2BDokument6 SeitenNursing Care Plan: Valiente, Ana Ambianca S. Maristela, Aony Jamaine Y. Tabora, Elyza M. Quitlong, Jennifer N. BSN 2BAmbianca ValienteNoch keine Bewertungen
- Ankle SprainDokument3 SeitenAnkle SpraindrakbarbabNoch keine Bewertungen
- This Is It NCD Case PresentationDokument31 SeitenThis Is It NCD Case PresentationEli BolusaNoch keine Bewertungen
- McCracken Diseno Actual de PPRDokument9 SeitenMcCracken Diseno Actual de PPRRania LVNoch keine Bewertungen
- Eye & Ear IrrigationDokument34 SeitenEye & Ear IrrigationdaisyNoch keine Bewertungen
- Crowns and Other Extra-Coronal RestorationDokument116 SeitenCrowns and Other Extra-Coronal RestorationDennis La Torre Zea100% (4)
- The Hospital TeamsDokument8 SeitenThe Hospital Teamsجميلة المعافيةNoch keine Bewertungen
- Anxiety Disorder: College of NursingDokument10 SeitenAnxiety Disorder: College of NursingAyr MasenasNoch keine Bewertungen
- Acutebrainfailure: Pathophysiology, Diagnosis, Management, and Sequelae of DeliriumDokument59 SeitenAcutebrainfailure: Pathophysiology, Diagnosis, Management, and Sequelae of DeliriumdarlingcarvajalduqueNoch keine Bewertungen
- No. Nama Alat Satuan Jumlah ReagenDokument2 SeitenNo. Nama Alat Satuan Jumlah ReagenferinaNoch keine Bewertungen