Beruflich Dokumente
Kultur Dokumente
Migraine PDF
Hochgeladen von
Daniel Bryant0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
126 Ansichten5 SeitenMigraine without aura is characterised over time by its evolution into chronic migraine. In MO patients the high frequency of migraine attacks, comorbidity with depression, and the tendency to develop arterial hypertension should require particular attention and careful management.
Originalbeschreibung:
Originaltitel
MIGRAINE.pdf
Copyright
© © All Rights Reserved
Verfügbare Formate
PDF, TXT oder online auf Scribd lesen
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenMigraine without aura is characterised over time by its evolution into chronic migraine. In MO patients the high frequency of migraine attacks, comorbidity with depression, and the tendency to develop arterial hypertension should require particular attention and careful management.
Copyright:
© All Rights Reserved
Verfügbare Formate
Als PDF, TXT herunterladen oder online auf Scribd lesen
0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
126 Ansichten5 SeitenMigraine PDF
Hochgeladen von
Daniel BryantMigraine without aura is characterised over time by its evolution into chronic migraine. In MO patients the high frequency of migraine attacks, comorbidity with depression, and the tendency to develop arterial hypertension should require particular attention and careful management.
Copyright:
© All Rights Reserved
Verfügbare Formate
Als PDF, TXT herunterladen oder online auf Scribd lesen
Sie sind auf Seite 1von 5
ORAL COMMUNI CATI ONS
Detection of possible factors favouring the evolution of migraine
without aura into chronic migraine
G. C. Manzoni
L. L. Lombardi
S. Lana
M. Maffezzoni
C. Camarda
P. Torelli
Springer-Verlag 2012
Abstract In a minority of cases, the natural history of
migraine without aura (MO) is characterised over time by its
evolution into a form of chronic migraine (CM). In order to
detect the possible factors predictingthis negative evolutionof
MO, we searched in our Headache Centre les for all clinical
records that met the following criteria: (a) rst visit between
1976and1998; (b) diagnosis of MOor of commonmigraine at
the rst observation, with or without association with other
primary headache types; (c)\15 days per month of migraine
at the rst observation; and (d) at least one follow-up visit at
least 10 years after the rst visit. The patients thus identied
were then divided into two groups based on a favourable/
steadyevolution(GroupA: n = 243, 195womenand48men)
or an unfavourable evolution (Group B: n = 72, 62 women
and 10 men) of their migraine over time. In the two groups, we
compared various clinical parameters that were present at the
rst observation or emerged at the subsequent follow-up vis-
its. The parameters that were statistically signicantly more
frequent in Group Band can therefore be considered pos-
sible negative prognostic factorswere: (a) C10 days per
month of migraine at the rst observation; (b) presence of
depressionat the rst visit inmales; and(c) onset of depression
or arterial hypertension after the rst observation but before
transformation to CM in females. Based on these ndings, in
MO patients the high frequency of migraine attacks, comor-
bidity with depression, and the tendency to develop arterial
hypertension should require particular attention and careful
management to prevent evolution into CM.
Keywords Migraine Migraine without aura Chronic
migraine Chronic daily headache Chronic headache
Introduction
Mean age at onset of migraine without aura (MO) is about
20 years. Onset may occur as early as in childhood, but
very rarely does over 50. Around this age, most patients see
that their migraine symptoms decrease and sometimes even
resolve completely. In contrast, in a minority, but not
negligible number, of patients, MO worsens over time,
changing some of its previous clinical features and espe-
cially increasing in frequency until there are no more free
intervals between attacks. Thus, MO is gradually trans-
formed from a typical attack-like headache to a so-called
chronic headache.
Several reports have been published on this subject in
the literature. However, there is still no consensus of
opinion on: (a) the type of headache that occurs in these
patients; and (b) the factors that may favour MO worsening
over time. We therefore tried to help clarify this issue by
performing a review of the broad case series of patients
followed over the years at our Headache Centre. We report
here the preliminary data of our study. The nal data will
be presented in a future publication.
Patients and methods
We accessed the University of Parma Headache Centre
les and took all clinical records of patients that met the
G. C. Manzoni (&) L. L. Lombardi S. Lana
M. Maffezzoni P. Torelli
Headache Centre, University of Parma, Via Gramsci, 14,
43100 Parma, Italy
e-mail: giancamillo.manzoni@unipr.it
C. Camarda
University of Palermo, Palermo, Italy
1 3
Neurol Sci (2012) 33 (Suppl 1):S165S167
DOI 10.1007/s10072-012-1075-0
following requirements: (a) rst visit between 1976 and
1998; (b) diagnosis of MO or of common migraine at the
rst observation, with or without association with other
primary headache types; (c) \15 days per month of
migraine at the rst observation; and (d) at least one fol-
low-up visit at least 10 years after the rst visit.
The 348 patients (286 women and 62 men) thus iden-
tied were divided into groups based on the diagnoses
made at the subsequent visits, and particularly the diag-
nosis made during the most recent visit at the Centre.
Diagnoses were established according to the criteria of the
International Classication of Headache Disorders, 2nd
Edition (ICHD-II) of 2004 [1] and its 2006 revision
(ICHD-IIR) [2].
The MO patterns that the 348 patients exhibited over the
years varied widely, not only from patient to patient, but
also within the same patient showing a course of alternat-
ing improvement and worsening. For that reason, in order
to compare patients with a steady or favourable evolution
of MO over time to patients with an unfavourable evolu-
tion, we excluded 33 patients (29 women and four men)
who over the years showed a cyclically uctuating
migraine pattern or developed a new form of headache that
might not necessary be interpreted as an evolution of their
original MO.
The remaining 315 patients (257 women and 58 men)
were divided into two groups based on a steady/favourable
evolution (Group A: n = 243, 195 women and 48 men) or
an unfavourable evolution (Group B: n = 72, 62 women
and 10 men) of their migraine over time. In each of the two
groups we compared not only the clinical features of MO
that were originally present at the rst visit, but also several
parameters related to the patients family, physiological,
past, and recent medical histories, both at the rst visit and
at the subsequent follow-up visits. Statistical analysis was
performed using Students t test and the v
2
test.
Results
Mean age at the rst observation of the 315 patients
included in the study was 32.0 11.2 years, with no sig-
nicant differences between the 257 women (32.1
11.1 years) and the 58 men (31.6 11.9 years). In the 72
patients with an unfavourable MO evolution, mean age at
the rst observation was older (Group B: 35.3 11.6
years), though in a non-statistically signicant way, than in
the 243 patients with a steady/favourable evolution (Group
A: 30.5 11.1 years). The difference was more marked in
men (38.7 8.8 vs. 30.1 11.8) than in women (34.8
11.9 vs. 30.6 10.9).
No statistically signicant differences were found
between Group A and Group B in age at the last
observation (46.0 11.5 and 52.2 12.5, respectively),
the number of years of observation (15.8 4.4 and
15.0 4.8), and the number of follow-up visits (3.8 3.6
and 5.0 4.8).
No signicant differences were found between the two
groups in age at onset of MO, family history of migraine,
pain location, and duration of attacks at the time of the rst
observation.
If we exclude three patients in Group A (two women and
one man) with a highly variable number of MO days per
month and 12 patientseight in Group A (seven women
and one man) and four in Group B (three women and one
man)with no certain data in their clinical records about
the number of MO days per month, the remaining 232
patients in Group A (186 women and 46 men) and the
remaining 68 patients in Group B (59 women and nine
men) showed a statistically signicant difference in the
number of MO days per month at the time of the rst
observation (Table 1).
In the patients medical histories reported at the rst
observation, depression was more statistically signicantly
present (p \0.05) in Group B men (6/9 corresponding to
66.7 %) than in Group A men (10/48 corresponding to
20.8 %).
Among the diseases that were reported at the subsequent
visits but occurred before MO chronication, Group B
versus Group A women showed a statistically signicantly
higher rate of depression (27/62 corresponding to 43.5 %
vs. 26/195 corresponding to 13.3 %, p \0.01) and arterial
hypertension (24/62 corresponding to 38.7 % vs. 35/195
corresponding to 17.9 %, p \0.01).
No statistically signicant differences were found
between the two groups in the presence of other diseases
(head injury, hypo- or hyper-thyroidism, colitis, allergy,
insomnia, anxiety, and panic attack disorder), either at the
time of the rst observation or later.
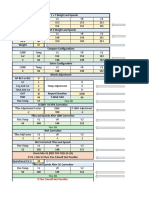
Table 1 Number of days of migraine per month at the rst visit
B5 days per
month
6 to 10 days per
month
11 to 15 days per
month
Group A
M 20 (41.7 %) 19 (39.6 %) 7 (14.6 %)
F 83 (42.6 %) 59 (30.3 %) 44 (22.6 %)
Total 103 (42.4 %) 78 (32.1 %) 51 (21.0 %)
Group B
M 1 (10.0 %) 3 (30.0 %) 5 (50.0 %)
F 20 (32.3 %) 15 (24.2 %) 24 (38.7 %)
Total 21 (29.2 %) 18 (25.0 %) 29 (40.3 %)
1115 days of MO per month versus B10 days of MO per month:
Group A versus Group B: p \0.01 for the total sample; p \0.05 for
both men and women
S166 Neurol Sci (2012) 33 (Suppl 1):S165S167
1 3
Conclusions
Our data analysis indicates that a high number of MO days
per month, comorbidity with depression and susceptibility
to arterial hypertension in women represent unfavourable
prognostic factors for a possible chronication of MO.
Therefore, it is extremely important that the presence of
these elements in all MO subjects be investigated with the
utmost care. If present, they should be managed in the most
appropriate way in order to prevent migraine from turning
chronic.
Conict of interest None.
References
1. Headache Classication Subcommittee of the International Head-
ache Society (2004) The International Classication of Headache
Disorders. Cephalalgia 24(suppl 1):1160
2. Olesen J, Bousser MG, Diener HC, Dodick D, First M, Goadsby
PJ, Goebel H, Lainez MJA, Lance JW, Lipton RB, Nappi G, Sakai
F, Schoenen J, Silberstein SD, Steiner TJ (2006) New appendix
criteria open for a broader concept of chronic migraine. Cepha-
lalgia 26:742746
Neurol Sci (2012) 33 (Suppl 1):S165S167 S167
1 3
Copyright of Neurological Sciences is the property of Springer Science & Business Media B.V. and its content
may not be copied or emailed to multiple sites or posted to a listserv without the copyright holder's express
written permission. However, users may print, download, or email articles for individual use.
Copyright of Neurological Sciences is the property of Springer Science & Business Media B.V. and its content
may not be copied or emailed to multiple sites or posted to a listserv without the copyright holder's express
written permission. However, users may print, download, or email articles for individual use.
Das könnte Ihnen auch gefallen
- Discapacidad y Calidad de Vida Pacientes MigrañaDokument8 SeitenDiscapacidad y Calidad de Vida Pacientes Migrañamaikol ramirezNoch keine Bewertungen
- ArticleDokument8 SeitenArticleDavidNoch keine Bewertungen
- Classification and Clinical Features of Headache Disorders in Pakistan: A Retrospective Review of Clinical DataDokument8 SeitenClassification and Clinical Features of Headache Disorders in Pakistan: A Retrospective Review of Clinical DatarikramNoch keine Bewertungen
- New Comprehensive Headache Quality of Life Questionnaire ValidatedDokument15 SeitenNew Comprehensive Headache Quality of Life Questionnaire ValidatedRicky HerdiantoNoch keine Bewertungen
- Bevilaqua-Grossi Et Al 2016 Arch Phys Med RehabilDokument9 SeitenBevilaqua-Grossi Et Al 2016 Arch Phys Med Rehabilcris.endo.ceNoch keine Bewertungen
- Associations Between Chronic Pain and Depressive SDokument7 SeitenAssociations Between Chronic Pain and Depressive SPati RamosNoch keine Bewertungen
- Epidemiology of headaches in BrazilDokument4 SeitenEpidemiology of headaches in BrazilVinicius SpazzapanNoch keine Bewertungen
- Chronic Scrotal Pain in Young Adults: BMC Research NotesDokument5 SeitenChronic Scrotal Pain in Young Adults: BMC Research NotesNoviTrianaNoch keine Bewertungen
- NeurologiaDokument216 SeitenNeurologiaPietro BracagliaNoch keine Bewertungen
- BMC Musculoskeletal Disorders: Fatigue in Osteoarthritis: A Qualitative StudyDokument8 SeitenBMC Musculoskeletal Disorders: Fatigue in Osteoarthritis: A Qualitative StudyElvis Ponce AbarcaNoch keine Bewertungen
- Italian Guideline of HeadacheDokument40 SeitenItalian Guideline of HeadachefadhilsyafeiNoch keine Bewertungen
- Depressive Spectrum Disorders in Cancer Prevalence Risk Factors and Screening For Depression: A Critical ReviewDokument11 SeitenDepressive Spectrum Disorders in Cancer Prevalence Risk Factors and Screening For Depression: A Critical ReviewppeixinhoNoch keine Bewertungen
- EBM Prognosis 2011Dokument47 SeitenEBM Prognosis 2011Astrid AviditaNoch keine Bewertungen
- P o S T - S T Roke Depression and Functional Outcome: A Cohort Study Investigating The Influence of Depression On Functional Recovery From StrokeDokument5 SeitenP o S T - S T Roke Depression and Functional Outcome: A Cohort Study Investigating The Influence of Depression On Functional Recovery From StrokeHasan KhawaldehNoch keine Bewertungen
- Chronische Mudigkeit 2020 Klinghardt MüdigkeitDokument99 SeitenChronische Mudigkeit 2020 Klinghardt Müdigkeitzim1dsgvo.ruNoch keine Bewertungen
- 1908 Clinical Characteristics and Prognosis of Polymyositis and Dermatomyositis Associated With Malignancy - A 25 Year Retrospective StudyDokument7 Seiten1908 Clinical Characteristics and Prognosis of Polymyositis and Dermatomyositis Associated With Malignancy - A 25 Year Retrospective StudyFlorian LamblinNoch keine Bewertungen
- Work Ability in Healthcare Workers (HCWS) After Breast Cancer: Preliminary Data of A Pilot StudyDokument9 SeitenWork Ability in Healthcare Workers (HCWS) After Breast Cancer: Preliminary Data of A Pilot StudyFirdaus BambooNoch keine Bewertungen
- 22 Masa Font2015Dokument9 Seiten22 Masa Font2015Sergio Machado NeurocientistaNoch keine Bewertungen
- Article PDFDokument8 SeitenArticle PDFFanel PutraNoch keine Bewertungen
- Persistence and Switching Patterns of Oral Migraine Prophylactic Medications Among Patients With Chronic Migraine: A Retrospective Claims AnalysisDokument16 SeitenPersistence and Switching Patterns of Oral Migraine Prophylactic Medications Among Patients With Chronic Migraine: A Retrospective Claims AnalysisAzam alausyNoch keine Bewertungen
- Psychosocial Support Groups For Patients With Multidrug Resistant Tuberculosis Five Years of ExperienceDokument15 SeitenPsychosocial Support Groups For Patients With Multidrug Resistant Tuberculosis Five Years of ExperienceLinh NguyenNoch keine Bewertungen
- Impact of Speed and Magnitude of Weight Loss On The Development of Brain Trophic Changes in Adolescents With Anorexia Nervosa: A Case Control StudyDokument4 SeitenImpact of Speed and Magnitude of Weight Loss On The Development of Brain Trophic Changes in Adolescents With Anorexia Nervosa: A Case Control StudyDhiafah Hera DarayaniNoch keine Bewertungen
- Chronic Lymphocytic Leukemia in Young (Comprehensive Analysis of Prognostic Factors and OutcomesDokument40 SeitenChronic Lymphocytic Leukemia in Young (Comprehensive Analysis of Prognostic Factors and OutcomesSanti Ayu SNoch keine Bewertungen
- Journal of Affective Disorders: Salma A. Ayis, Luis Ayerbe, Siobhan L. Crichton, Anthony G. Rudd, Charles D.A. WolfeDokument7 SeitenJournal of Affective Disorders: Salma A. Ayis, Luis Ayerbe, Siobhan L. Crichton, Anthony G. Rudd, Charles D.A. WolfeDafny C. AroneNoch keine Bewertungen
- Non-Specific Low Back PainDokument12 SeitenNon-Specific Low Back PainSarah Naura IrbahNoch keine Bewertungen
- Acm 2009 0376Dokument10 SeitenAcm 2009 0376Dr Tanu GogoiNoch keine Bewertungen
- Prevalen of DDokument8 SeitenPrevalen of DĐỗ Văn ĐứcNoch keine Bewertungen
- Ebm SeptemberDokument29 SeitenEbm SeptemberJulius OentarioNoch keine Bewertungen
- Anxiety and Depression After Cancer DiagnosisDokument26 SeitenAnxiety and Depression After Cancer DiagnosisMesias PatricioNoch keine Bewertungen
- Depression in Multiple Sclerosis PDFDokument11 SeitenDepression in Multiple Sclerosis PDFalejandro bustamanteNoch keine Bewertungen
- Assessing Chronic Illness Representations - The Implicit Models of Illness QuestionnaiDokument18 SeitenAssessing Chronic Illness Representations - The Implicit Models of Illness QuestionnaiiulianaNoch keine Bewertungen
- 7 FTPDokument6 Seiten7 FTPhaddig8Noch keine Bewertungen
- Depression Timing and Cardiac Outcomes in PatientsDokument43 SeitenDepression Timing and Cardiac Outcomes in PatientsMae MayugaNoch keine Bewertungen
- International Journal of LeprosyDokument9 SeitenInternational Journal of LeprosyAjie WitamaNoch keine Bewertungen
- Guide Diagnosis Treatment DecisionsDokument12 SeitenGuide Diagnosis Treatment DecisionsJehad Ali Al-ammariNoch keine Bewertungen
- Nonespecific Low BackpainDokument8 SeitenNonespecific Low BackpainleocmyNoch keine Bewertungen
- 10 1155@2019@7307198Dokument9 Seiten10 1155@2019@7307198Asti YumnaNoch keine Bewertungen
- HD Psychiatry 1Dokument6 SeitenHD Psychiatry 1annaNoch keine Bewertungen
- Journal 2Dokument12 SeitenJournal 2FieraNoch keine Bewertungen
- Prieto6 Roleofdepression Jco2005Dokument9 SeitenPrieto6 Roleofdepression Jco2005jesusprietusNoch keine Bewertungen
- Vulnerabilidade A Dor 2014Dokument9 SeitenVulnerabilidade A Dor 2014Ellen AmaralNoch keine Bewertungen
- Quality of Life in Episodic Cluster HeadacheDokument29 SeitenQuality of Life in Episodic Cluster HeadacheDrMorczNoch keine Bewertungen
- Gambriela 2019, ScopusDokument15 SeitenGambriela 2019, Scopusnirmala amirNoch keine Bewertungen
- Mal de DebarquementDokument10 SeitenMal de DebarquementFelipeAsenjoÁlvarezNoch keine Bewertungen
- Systematic Review Article: Section Editor: Angela EnrightDokument10 SeitenSystematic Review Article: Section Editor: Angela EnrightLuciana AraújoNoch keine Bewertungen
- VM FactorsDokument10 SeitenVM Factorssanti sidabalokNoch keine Bewertungen
- Chen 2015 Self-Report PDFDokument35 SeitenChen 2015 Self-Report PDFviolaarisanti6Noch keine Bewertungen
- 10 1002@msc 1498Dokument13 Seiten10 1002@msc 1498Ricardo PietrobonNoch keine Bewertungen
- Baizabal, J. Et Al (2023) Contrasting Features Between Tourette Syndrome and Secondary Tic...Dokument6 SeitenBaizabal, J. Et Al (2023) Contrasting Features Between Tourette Syndrome and Secondary Tic...cuautzinNoch keine Bewertungen
- Bladder Pain Syndrome/Interstitial Cystitis Is Associated With HyperthyroidismDokument5 SeitenBladder Pain Syndrome/Interstitial Cystitis Is Associated With HyperthyroidismAlbari PohanNoch keine Bewertungen
- DNB Vol33 NoSuppl 2 190Dokument2 SeitenDNB Vol33 NoSuppl 2 190Anel BrigićNoch keine Bewertungen
- Prevalence of Post Stroke Depression in Ambulatory PatientsDokument7 SeitenPrevalence of Post Stroke Depression in Ambulatory PatientsSitti Rosdiana YahyaNoch keine Bewertungen
- Articulo PsychoDokument8 SeitenArticulo PsychoLaura AlfaroNoch keine Bewertungen
- Stress y Alopecia AreataDokument10 SeitenStress y Alopecia AreataKaren MoctezumaNoch keine Bewertungen
- CDC Grand Rounds: Chronic Fatigue Syndrome - Advancing Research and Clinical EducationDokument5 SeitenCDC Grand Rounds: Chronic Fatigue Syndrome - Advancing Research and Clinical EducationMarcelita DuwiriNoch keine Bewertungen
- EBM - Critical Appraisal of Prognostic StudiesDokument24 SeitenEBM - Critical Appraisal of Prognostic StudiesNabilla Sophia Sofyan100% (2)
- Antidepressant-Associated Chronic Irritable Dysphoria (ACID) in STEP-BD PatientsDokument6 SeitenAntidepressant-Associated Chronic Irritable Dysphoria (ACID) in STEP-BD Patientseduardobar2000Noch keine Bewertungen
- 10.1016@S0140 67361160610 7Dokument10 Seiten10.1016@S0140 67361160610 7Agus PrimaNoch keine Bewertungen
- Critical Reviews in Oncology / HematologyDokument18 SeitenCritical Reviews in Oncology / HematologyLiterasi MedsosNoch keine Bewertungen
- Farm AkoooDokument2 SeitenFarm AkoooDaniel BryantNoch keine Bewertungen
- Far MakooooDokument1 SeiteFar MakooooDaniel BryantNoch keine Bewertungen
- Far MakoooDokument1 SeiteFar MakoooDaniel BryantNoch keine Bewertungen
- Untitled 1Dokument3 SeitenUntitled 1Daniel BryantNoch keine Bewertungen
- Book I Concerning DisciplineDokument1 SeiteBook I Concerning DisciplinelakshmiduraiNoch keine Bewertungen
- SSH TEXT Singapura 14 September 2015Dokument1 SeiteSSH TEXT Singapura 14 September 2015Daniel BryantNoch keine Bewertungen
- SN Photoshop Cs5Dokument5 SeitenSN Photoshop Cs5Daniel BryantNoch keine Bewertungen
- SN Photoshop Cs5Dokument1 SeiteSN Photoshop Cs5Daniel BryantNoch keine Bewertungen
- SN Photoshop Cs5Dokument1 SeiteSN Photoshop Cs5Daniel BryantNoch keine Bewertungen
- Friend ConnectDokument1 SeiteFriend ConnectDaniel BryantNoch keine Bewertungen
- CookieDokument1 SeiteCookieDaniel BryantNoch keine Bewertungen
- Book I Concerning DisciplineDokument1 SeiteBook I Concerning DisciplinelakshmiduraiNoch keine Bewertungen
- CorelDRAW Graphics Suite X6Dokument1 SeiteCorelDRAW Graphics Suite X6Daniel BryantNoch keine Bewertungen
- Cardiophysiology: by Sawiji Amani Mobile Phone: 081 328 028333 E-MailDokument8 SeitenCardiophysiology: by Sawiji Amani Mobile Phone: 081 328 028333 E-MailDaniel BryantNoch keine Bewertungen
- Cardiovascular and Lymphatic Systems: Tutorial Class SeriesDokument31 SeitenCardiovascular and Lymphatic Systems: Tutorial Class SeriesDaniel BryantNoch keine Bewertungen
- Keyboard Keys and Key Code Values in ActionScript 2.0Dokument4 SeitenKeyboard Keys and Key Code Values in ActionScript 2.0Sapath GuptaNoch keine Bewertungen
- Cardiovascular and Lymphatic Systems: Tutorial Class SeriesDokument31 SeitenCardiovascular and Lymphatic Systems: Tutorial Class SeriesDaniel BryantNoch keine Bewertungen
- Cardiovascular and Lymphatic Systems: Tutorial Class SeriesDokument31 SeitenCardiovascular and Lymphatic Systems: Tutorial Class SeriesDaniel BryantNoch keine Bewertungen
- Lingsir Wengi & Kusumaning AtiDokument1 SeiteLingsir Wengi & Kusumaning AtiDaniel BryantNoch keine Bewertungen
- 1Dokument17 Seiten1Daniel BryantNoch keine Bewertungen
- Assignment 5: Building More Complex Tasks: 1 BackgroundDokument3 SeitenAssignment 5: Building More Complex Tasks: 1 Backgroundt_hoffmannNoch keine Bewertungen
- A320 Flex CalculationDokument10 SeitenA320 Flex CalculationMansour TaoualiNoch keine Bewertungen
- Us00-000 831 01 02 02Dokument18 SeitenUs00-000 831 01 02 02Cristian Camilo0% (1)
- Assumptions of Indifference CurveDokument12 SeitenAssumptions of Indifference CurveAbhishek RavalNoch keine Bewertungen
- Grade-3-DLL MATHEMATICS-3 Q1 W4Dokument3 SeitenGrade-3-DLL MATHEMATICS-3 Q1 W4Jonathan Corveau IgayaNoch keine Bewertungen
- Murat Kenedy: Bu Içerik Tarafından HazırlanmıştırDokument2 SeitenMurat Kenedy: Bu Içerik Tarafından HazırlanmıştırChatorg. orgNoch keine Bewertungen
- Industrial Wire Cutting Machine: A Senior Capstone Design ProjectDokument17 SeitenIndustrial Wire Cutting Machine: A Senior Capstone Design ProjectTruta IonutNoch keine Bewertungen
- Automatic Helmet DetectDokument4 SeitenAutomatic Helmet Detectvasanth100% (1)
- Friction WedgesDokument7 SeitenFriction Wedgespericharla ravivarmaNoch keine Bewertungen
- Mental Health Stigma and Help SeekingDokument4 SeitenMental Health Stigma and Help SeekingJane Arian BerzabalNoch keine Bewertungen
- Organizational Structure and ProfilesDokument178 SeitenOrganizational Structure and ProfilesImran Khan NiaziNoch keine Bewertungen
- Sheet Metalworking 1 - Chapter 19Dokument99 SeitenSheet Metalworking 1 - Chapter 19xharpreetxNoch keine Bewertungen
- Four Ball EPDokument5 SeitenFour Ball EPu4sachinNoch keine Bewertungen
- Daily Dawn Newspaper Vocabulary with Urdu MeaningsDokument4 SeitenDaily Dawn Newspaper Vocabulary with Urdu MeaningsBahawal Khan JamaliNoch keine Bewertungen
- Slippery? Contradictory? Sociologically Untenable? The Copenhagen School RepliesDokument10 SeitenSlippery? Contradictory? Sociologically Untenable? The Copenhagen School RepliesDaniel CorrenteNoch keine Bewertungen
- 268US03 Oiltech Technical & Product Catalogue Letter WDokument48 Seiten268US03 Oiltech Technical & Product Catalogue Letter WMauricio CarestiaNoch keine Bewertungen
- ButeDokument89 SeitenButeNassime AmnNoch keine Bewertungen
- Final Koni FinalDokument124 SeitenFinal Koni FinalBinod BoharaNoch keine Bewertungen
- Project Equipment Load AnalysisDokument54 SeitenProject Equipment Load Analysisrajeshmk2002100% (6)
- Organizational Change & Development - VIL2021 - 22Dokument3 SeitenOrganizational Change & Development - VIL2021 - 22Rahul TRIPATHINoch keine Bewertungen
- Hydro Cyclone: Centripetal Force Fluid ResistanceDokument10 SeitenHydro Cyclone: Centripetal Force Fluid ResistanceMaxwell ToffahNoch keine Bewertungen
- POOJA TRADING CO. Price List for FRP Manhole CoversDokument1 SeitePOOJA TRADING CO. Price List for FRP Manhole Coversmitesh20281Noch keine Bewertungen
- 3 - Big Data CharacteristicsDokument32 Seiten3 - Big Data CharacteristicsWong pi wenNoch keine Bewertungen
- Microsoft Word - JOB DESCRIPTION Staff AccountantDokument2 SeitenMicrosoft Word - JOB DESCRIPTION Staff Accountantanon-634050100% (3)
- #C C C$ C%C& C' C (CDokument4 Seiten#C C C$ C%C& C' C (CThong Chee WheiNoch keine Bewertungen
- Public Dealing With UrduDokument5 SeitenPublic Dealing With UrduTariq Ghayyur86% (7)
- Accomplishment Report - English (Sy 2020-2021)Dokument7 SeitenAccomplishment Report - English (Sy 2020-2021)Erika Ikang WayawayNoch keine Bewertungen
- ETEEAP Application SummaryDokument9 SeitenETEEAP Application SummaryAlfred Ronuel AquinoNoch keine Bewertungen
- Format Question Bank RevisedDokument21 SeitenFormat Question Bank RevisedkhananuNoch keine Bewertungen
- Adss-Eke 150 (Mm12c) eDokument7 SeitenAdss-Eke 150 (Mm12c) eYuseidy Rguez PaezNoch keine Bewertungen