Beruflich Dokumente
Kultur Dokumente
Respiratory Nursing #1
Hochgeladen von
shenric16100%(12)100% fanden dieses Dokument nützlich (12 Abstimmungen)
2K Ansichten19 Seitenms respiratory nursing
Copyright
© © All Rights Reserved
Verfügbare Formate
PDF, TXT oder online auf Scribd lesen
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenms respiratory nursing
Copyright:
© All Rights Reserved
Verfügbare Formate
Als PDF, TXT herunterladen oder online auf Scribd lesen
100%(12)100% fanden dieses Dokument nützlich (12 Abstimmungen)
2K Ansichten19 SeitenRespiratory Nursing #1
Hochgeladen von
shenric16ms respiratory nursing
Copyright:
© All Rights Reserved
Verfügbare Formate
Als PDF, TXT herunterladen oder online auf Scribd lesen
Sie sind auf Seite 1von 19
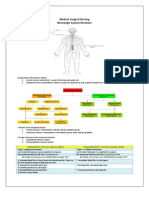
Medical and Surgical Nursing
Respiratory System Lecture Notes
Prepared by: Mark Fredderick R. Abejo RN,, MAN
MS Abejo 1
MEDICAL AND SURGICAL NURSING
Respiratory System
Lecturer: Mark Fredderick R. Abejo RN,MAN
Medical and Surgical Nursing
Respiratory System Lecture Notes
Prepared by: Mark Fredderick R. Abejo RN,, MAN
MS Abejo 2
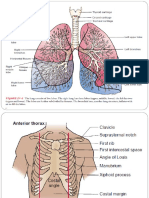
ANATOMY OF RESPIRATORY SYSTEM
OXYGENATON: the dynamic interaction of gases in the body for
the purpose of delivering adequate oxygen essential for cellular
survival
RESPIRATORY SYSTEM MAIN FUNCTION:
GAS EXCHANGE
I. Upper Respiratory Tract
A. Functions
1. Filtering
2. Warming and moistening
3. Humidification
B. Parts
1. Nose - made up of framework of cartilages; divided
into R and L by the nasal septum.
2. Paranasal Sinuses includes four pair of bony
cavities that are lined with nasal mucosa and ciliated
epithelium.
3. Tubernate Bones ( Conchae )
4. Pharynx muscular passageway for both food and
air
Nasopharynx
Oropharynx
Laryngopharynx
5. Tonsils and Adenoids
6. Larynx voice production, coughing reflex
Made up of framework of:
Epiglottis valve that covers the opening
to the larynx during swallowing.
Glottis opening between the vocal cords
Hyoid bone u shaped bone in neck
Cricoid cartilage
Thyroid cartilage, forms the Adams apple
Arythenoid cartilage
Speech production and cough reflex
Vocal cords
7. Trachea - consists of cartilaginous rings
Passageway of air
Site of tracheostomy (4
th
-6
th
tracheal ring)
II. Lower respiratory tract
A. Function: facilitates gas exchange
B. Parts
1. Lungs, are paired elastic structure enclosed in the
thoracic cage, which is an airtight chamber with
distensible walls.
Right 3 lobes, 10 segments
Left 2 lobes, 8 segments
Client post pneumonectomy affected side to promote expansion
Post lobectomy unaffected side to promote drainage
Pleural cavity
Parietal
Visceral
Pleural Fluid: prevents pleural friction rub
(as seen in pneumonia and pleural effusion)
2. Bronchi
Lobar Bronchi: 3 R and 2 L
Segmental Bronchi: 10 R and 8 L
Subsegmental Bronchi
3. Bronchioles
Terminal Bronchioles
Respiratory Bronchioles, considered to be
the transitional passageways between the
conducting airways and the gas exchange
4. Alveoli
- functional cellular units or gas-exchange
units of the lungs.
- O2 and CO2 exchange takes place
- Made up of about 300 million
TYPE 1 - provide structure to the alveoli
TYPE 2 - secrete SURFACTANT, reduces surface
tension; increases alveoli stability & prevents their
collapse
TYPE 3 alveolar cell macrophages, destroys
foreign material, such as bacteria
Lecithin
Sphingomyelin
L/S ratio indicates lung maturity
2:1 normal
1:2 immature lungs
PULMONARY CIRCULATION
- Provides for reoxygenation of blood and release of CO2
PULMONARY ARTERIES, carry blood from
the heart to the lungs.
PULMONARY VEINS, is a large blood vessel
of the circulatory system that carries blood
from the lungs to the left atrium of the heart.
RESPIRATORY MUSCLES
- PRIMARY: diaphragm and external intercostal muscles
- ACCESORY: sternocleidomastoid (elevated sternum),
the scalene muscles (anterior, middle and posterior
scalene) and the nasal alae
Medical and Surgical Nursing
Respiratory System Lecture Notes
Prepared by: Mark Fredderick R. Abejo RN,, MAN
MS Abejo 3
PHYSIOLOGY OF RESPIRATORY SYSTEM
VENTILATION: The movement of air in and out of the airways.
The thoracic cavity is an air tight chamber. the floor of
this chamber is the diaphragm.
Inspiration: contraction of the diaphragm (movement of
this chamber floor downward) and contraction of the
external intercostal muscles increases the space in this
chamber. lowered intrathoracic pressure causes air to
enter through the airways and inflate the lungs.
Expiration: with relaxation, the diaphragm moves up and
intrathoracic pressure increases. this increased pressure
pushes air out of the lungs. expiration requires the elastic
recoil of the lungs.
Inspiration normally is 1/3 of the respiratory cycle and
expiration is 2/3.
DRIVING FORCE FOR AIR FLOW
Airflow driven by the pressure difference between
atmosphere (barometric pressure) and inside the lungs
(intrapulmonary pressure).
AIRWAY RESISTANCE
Resistance is determined chiefly by the radius size of the
airway.
Causes of Increased Airway Resistance
1. Contraction of bronchial mucosa
2. Thickening of bronchial mucosa
3. Obstruction of the airway
4. Loss of lung elasticity
RESPIRATION
The process of gas exchange between atmospheric air
and the blood at the alveoli, and between the blood cells
and the cells of the body.
Exchange of gases occurs because of differences in
partial pressures.
Oxygen diffuses from the air into the blood at the alveoli
to be transported to the cells of the body.
Carbon dioxide diffuses from the blood into the air at the
alveoli to be removed from the body.
NEUROCHEMICAL CONTROL
MEDULLA OBLONGATA respiratory center
initiates each breath by sending messages to primary
respiratory muscles over the phrenic nerve
- has inspiration and expiration centers
PONS has 2 respiration centers that work with the
inspiration center to produce normal rate of breathing
1. PNEUMOTAXIC CENTER affects the inspiratory
effort by limiting the volume of air inspired
2. APNEUSTIC CENTER prolongs inhalation
NOTE: Chemoreceptors responds to changes in ph, increased
PaCO2 = increase RR
RESPIRATORY EXAMINATION AND
ASSESSMENT
Background information
A. Abnormal patterns of breathing
1. Sleep Apnea
cessation of airflow for more than 10 seconds more
than 10 times a night during sleep
causes: obstructive (e.g. obesity with upper narrowing,
enlarged tonsils, pharyngeal soft tissue changes in
acromegaly or hypothyroidism)
2. Cheyne-Stokes
periods of apnoea alternating with periods of
hyperpnoae
pathophysiology: delay in medullary chemoreceptor
response to blood gas changes
causes
left ventricular failure
brain damage (e.g. trauma, cerebral,
haemorrhage)
high altitude
3. Kussmaul's (air hunger)
deep rapid respiration due to stimulation of respiratory
centre
causes: metabolic acidosis (e.g. diabetes mellitus,
chronic renal failure)
4. Hyperventilation
complications: alkalosis and tetany
causes: anxiety
5. Ataxic (Biot)
irregular in timing and deep
causes: brainstem damage
6. Apneustic
post-inspiratory pause in breathing
causes: brain (pontine) damage
Medical and Surgical Nursing
Respiratory System Lecture Notes
Prepared by: Mark Fredderick R. Abejo RN,, MAN
MS Abejo 4
7. Paradoxical
the abdomen sucks with respiration (normally, it
pouches uotward due to diaphragmatic descent)
causes: diaphragmatic paralysis
B. Cyanosis
1. Refers to blue discoloration of skin and mucous
membranes , is due to presence of deoxygenated
haemoglobin in superficial blood vessels
2. Central cyanosis = abnromal amout of deoxygenated
haemoglobin in arteries and that blue discoloration is
present in parts of body with good circulation such as
tongue
3. Peripheral cyanosis = occurs when blood supply to a
certain part of body is reduced, and the tissue extracts
more oxygen from normal from the circulating blood, e.g.
lips in cold weather are often blue, but lips are spared
4. Causes of cyanosis
Central cyanosis
decreased arterial saturation
decreased concentration of inspired oxygen:
high altitude
lung disease: COPD with cor pulmoale,
massive pulmonary embolism
right to left cardiac shunt (cyanotic congenital
heart disease)
polycythaemia
haemoglobin abnromalities (rare):
methaemoglobinaemia, sulphaemoglobinaemia
Peripheral cyanosis
all causes of central cyanosis cause peripheral
cyanosis
exposure to cold
reduced cardiac output: left ventricular failure or
shock
arterial or venous obstruction
Position: patient sitting over edge of bed
General appearance
look for the following
Dyspnea
normal respiratory rate < 14 each minute
tachypnoea = rapid respiratory rate
are accessory muscles being used (sternomastoids,
platysma, strap muscles of neck) - characteristically,
the accessory muscles cause elevation of shoulders
with inspiration and aid respiration by increasing
chest expansion
Cyanosis
Character of cough
ask patient to cough several times
lack of usual explosive beginning may indicate
vocal cord paralysis (bovine cough)
muffled, wheezy ineffective cough suggests airflow
limitation
very loose productive cough suggests excessive
bronchial secretions due to:
- chronic bronchitis
- pneumonia
- bronchiectasis
dry irritating cough may occur with:
- chest infection
- asthma
- carcinoma of bronchus
- left ventricular failure
- interstitial lung disease
- ACE inhibitors
Sputum
volume
type (purulent, mucoid, mucopurulent)
presence or absence of blood?
Stridor
croaking noise loudest on inspiration
is a sign that requires urgent attention
causes: (obstruction of larynx, trachea or large
broncus)
- acute onset (minutes)
inhaled foreign body
acute epiglottitis
anaphylaxis
toxic gas inhalation
- gradual onset (days, weeks)
laryngeal and pharyngeal tumours
crico-arytenoid rheumatoid arthritis
bilateral vocal cord palsy
tracheal carcinoma
paratracheal compression by lymph nodes
post-tracheostomy or intubation
granulomata
Hoarseness
causes include:
- laryngitis
- laryngeal nerve palsy associated with
carcinoma of lung
- laryngeal carcinoma
The Hands
Clubbing
commonly cause by respiratory disease (but NOT
emphysema or chronic bronchitis)
occasionally, clubbing is associated with hypertrophic
pulmonary osteoarthropathy (HPO)
characterised by periosteal inflammation at distal ends
of long bones, wrists, ankles, metacarpals and
metatarsals
sweelling and tenderness over wrists and other
involved areas
Staining
staining of fingers - sign of cigarette smoking (caused by
tar, not nicotine)
Wasting and weakness
Pulse rate
Flapping tremor (asterixis) - unreliable sign
ask patient to dorsiflex wrists and spread out fingers, with
arms outstretched
flapping tremor may occur with severe carbon dioxide
retention (severe chronic airflow limitation)
Medical and Surgical Nursing
Respiratory System Lecture Notes
Prepared by: Mark Fredderick R. Abejo RN,, MAN
MS Abejo 5
The Face
Eyes
Horner's syndrome? (constricted pupil, partial ptosis and
loss of sweating which can be due to apical lung tumour
compressing sympathetic nerves in neck)
Nose
polpys? (associated with asthma)
engorged turbinates? (various allergic conditions)
deviated septum? (nasal obstruction)
Mouth and tongue
look for central cyanosis
evidence of upper respiratory tract infection (a reddened
pharynx and tonsillar enlargement with or without a
coating of pus)
broken tooth - may predispose to lung abscess or
pneumonia
sinusitis is indicated by tenderness over the sinuses on
palpation
some patients with obstructive sleep apnoea will be obese
with a receding chin, a small pharynx and a short thick neck
The Trachea
causes of tracheal displacement:
toward the side of the lung lesion
upper lobe collapse
upper lobe fibrosis
pneumonectomy
upper mediastinal masses, such as retrosternal goitre
tracheal tug (finger resting on trachea feels it move inferiorly
with each inspiration) is a sign of gross overexpansion of the
chest because of airflow obstruction
The Chest: inspection
Shape and symmetry of chest
Barrel shaped
anteroposterior (AP) diameter is increased compared
with lateral diameter
causes: hyperinflation due to asthma, emphysema
Pigeon chest (pectus carinatum)
localised prominence (outward bowing of sternum and
costal cartilages)
causes:
manifestation of chronic childhood illness (due to
repeated strong contractions of diaphragm while
thorax is still pliable)
rickets
Funnel chest (pectus excavatum)
developmental defect involving a localised depression
of lower end of sternum in severe cases, lung capacity
may be restricted
Harrison's sulcus
innar depression of lower ribs just above costal margins
at site of attachment of diaphragm
causes:
severe asthma in childhood
rickets
Kyphosis , exaggerated forward curvature of spine
Scoliosis , lateral bowing
Kyphoscoliosis: causes:
idiopathic (80%)
secondary to poliomyelitis (inflammation involving
grey matter of cord)
(note: severe thoracic kyphoscoliosis may reduce lung
capacity and increase work of breathing)
Lesions of chest wall
scars - previous thoracic operations or chest drains for a
previous pneumothorax or pleural effusion
thoracoplasty (was once performed to remove TB, but
no longer is because of effective antituberculosis
chemotherapy) invovled removal of large number of
ribs on one side to achieve permanent collapse of
affected lung
erythema and thickening of skin may occur in
radiotherapy; there is a sharp demarcation between
abnormal and normal skin
Diffuse swelling of chest wall and neck
pathophysiology: air tracking from the lungs
causes:
pneumothorax
rupture of oesopahagus
Prominent veins
cause: superior vena caval obstruction
Asymmetry of chest wall movements
assess this by inspecting from behind patient, looking
down the clavicles during moderate respiration -
diminished movement indicates underlying lung disease
the affected side will showed delayed or decreased
movement
causes of reduced chest wall movements on one side are
localised:
localised pulmonary fibrosis
consolidation
collapse
pleural effusion
pneumothroax
causes of bilateral reduced chest wall movements are
diffuse:
chronic airflow limitation
diffuse pulmonary fibrosis
Medical and Surgical Nursing
Respiratory System Lecture Notes
Prepared by: Mark Fredderick R. Abejo RN,, MAN
MS Abejo 6
The Chest: palpation
chest expansion
place hands firmly on chest wall with fingers extending
around sides of chest (fugyre 4.5)
as patient takes a big breath in, the thumbs should move
symmetrically apart about 5 cm
reduced expansion on one side indicates a lesion on that
side
note: lower lobe expansion is tested here; upper lobe is
tested for on inspection (as above)
apex beat
(discussed in cardiac section)
for respiratory diseases:
displacement toward site of lesion - can be caused by:
collapse of lower lobe
localised pulmonary fibrosis
displacement away from site of lesion - can be caused
by:
pleural effusion
tension pneumothorax
apex beat is often impalpable in a chest which is
hyperexpanded secondary to chronic airflow limitation
vocal fremitus
palpate chest wall with palm of hand while patient repeats
"99"
front and back of chest are each palpated in 2 comparable
positions with palms; in this way differences in vibration on
chest wall can be detected
causes of change in vocal fremitus are the same as those for
vocal resonance (see later)
ribs
gently compress chest wall anteroposteriorly and laterally
localised pain suggests a rib fracture (may be secondary to
trauma or spontaneous as a result of tumour deposition or
bone disease)
The Chest: percussion
with left hand on chest wall and fingers slightly separated and
aligned with ribs, the middle finger is pressed firmly against
the chest; pad of right middle finger is used to strike firmly the
middle phalanx of middle finger of left hand
percussion of symmetrical areas of:
anterior (chest)
posterior (back) (ask patient to move elbows forward
across the front of chest - this rotates the scapulae
anteriorly, i.e. moves it out of the way)
axillary region (side)
supraclavicular fossa
percussion over a solid structure (e.g. liver, consolidated lung)
produces a dull note
percusion over a fluid filled area (e.g. pleural effusion)
produces an extremely dull (stony dull) note
percussion over the normal lung produces a resonant note
percussion over a hollow structure (e.g. bowel, pneumothorax)
produces a hyperresonsant note
liver dullness:
upper level of liver dullness is determined by percussing
down the anterior cehst in mid-clavicular line
normally, upper level of liver dullness is 6th rib in right
mid-clavicular line
if chest is resonant below this level, it is a sign of
hyperinflation usually due to emphysema, asthma
cardiac dullness:
area of cardiac dullness is uaully present on left side of
chest
this may decrease in emphysema or asthma
The Chest: auscultation
breath sounds
introduction
one should use the diaphragm of stethoscope to listen
to breath sound in each area, comparing each side
remember to listen high up into the axillae
remember to use bell of stethoscope to listen to lung
from above the clavicles
quality of breath sounds
normal breat sounds
are heard with stethoscope over all parts of
chest, produced in airways rather than alveoli
(although once they had been thought to arise
from alveoli (vesicles) and are therefore called
vesicular sounds)
normal (vesicular) breath sounds are louder and
longer on inspiration than on expiration; and
there is no gap between the inspiratory and
expiratory sounds
bronchial breath sounds
turbulence in large airways is heard without
being filtered by the alveoli, and therefore
produce a different quality; they are heard over
the trachea normally, but not over the lungs
are audible throughout expiration, and often
there is a gap between inspiration and expiration
are heard over areas of consolidation since solid
lung conducts the sound of turbulence in main
airways to peripheral areas without filtering
causes include:
- lung consolidation (lobar pneumonia) -
common
- localised pulmonary fibrosis - uncommon
- pleural effusion (above the fluid) -
uncommon
- collapsed lung (e.g. adjacent to a pleural
effusion) - uncommon
amphoric sound = when breath sounds over a
large cavity have an exaggerated bronchial
quality)
intensity of breath sounds
causes of reduced breath sounds include:
chronic airflow limitation (especially
emphysema)
pleural effusion
pneumothorax
pneumonia
large neoplasm
pulmonary collapse
added (adventitious) sounds
two types of added sounds: continuous (wheezes) and
interrupted (crackles)
wheezes
may be heard in expiration or inspiration or both
pathophysiology of wheezes - airway narrowing
an inspiratory wheeze implies severe airway
narrowing
Medical and Surgical Nursing
Respiratory System Lecture Notes
Prepared by: Mark Fredderick R. Abejo RN,, MAN
MS Abejo 7
causes of wheezes include:
- asthma (often high pitched) - due to muscle
spasm, mucosal oedema, excessive
secretions
- chronic airflow diseases - due to mucosal
oedema and excessive secretions
- carcinoma causing bronchial obstruction -
tends to cause a localised wheeze which is
monophonic and does not clear with
coughing
crackles
some terms not to use include rales (low pitched
crackles) and creptitations (high pitched
crackles)
crackles are due to collapse of peripheral
airways on expiration and sudden opening on
inspiration
early inspiratory crackles
- suggests disease of small airways
- characteristic of chronic airflow limitation
- are only heard in early inspiration
late or paninspiratory crackles
- suggests disease confined to alveoli
- may be fine, medium or coarse
- fine crackles - typically caused by
pulmonary fibrosis
- medium crackles - typically caused by left
ventricular failure (due to presence of
alveolar fluid)
- coarse crackes - tend to change with
coughing; occur with any disease that leads
to retention of secretions; commonly occur
in bronchiectasis
pleural friction rub
when thickened, roughened pleural surfaces rub
together, a continuous or intermittent grating
sound may be heard
suggests pleurisy, which may be secondary to
pulmonary infarction or pnuemonia
vocal resonanance
gives information about lungs' ability to transmit sounds
consolidated lung tends to transmit high frequencies so
that speech heard through stethoscope takes a bleeting
quality (aegophony); when a patient with aegophony says
"bee" it sounds like "bay"
listen over each part of chest as patient says "99"; over
consolidated lung, the numbers will become clearly
audible; over normal lung, the sound is muffled
whispering pectoriloquy - vocal resonance is increased to
such an extent that whispered speech is distinctly heard
The Heart
lie patient at 45 degrees
measure jugular venous plse for right heart failure
examine preacordium; pay close attention to pulmonary
component of P2 (which is best heard at 2nd intercostal
space on left) and should not be louder than A2; if it is
louder, suspect pulmonary hypertension
cor pulmonale (also called pulmonary hypertensive heart
disease) may be due to:
chronic airflow limitation (emphysema)
pulmonary fibrosis
pulmonary thromboembolism
marked obesity
sleep apnoea
severe kyphoscoliosis
The Abdomen
palpate liver for enlargement due to secondary deposits of
tumour from lung, or right heart failure
Other
Permberton's sign
ask patient to lift arms over head
look for development of facial plethora, inspiratory
stridor, non-pulsatile elevation of jugular venous
pressure
occurs in vena caval obstruction
Feet
inspect for oedema or cyanosis (clues of cor
pulmonale)
look for evidence of deep vein thrombosisd
Respiratory rate on exercise and positioning
patients complaining of dyspnoea should have their
respiratory rate measured at rest, at maximal tolerated
exertion and supine
if dyspnoea is not accompanied by tachypnoea when
a patient climbs stairs, one should consider
malingering
look for paradoxical inward motion of abdomen
during inspiration when patient is uspine (indicating
diaphragmatic paralysis)
Temperature: fever may accompany any acute or chronic
chest infection
DIAGNOSTIC EVALUATION
1. Skin Test: Mantoux Test or Tuberculin Skin Test
This is used to determine if a person has been infected or
has been exposed to the TB bacillus.
This utilizes the PPD (Purified Protein Derivatives).
The PPD is injected intradermally usually in the inner
aspect of the lower forearm about 4 inches below the
elbow.
The test is read 48 to 72 hours after injection.
(+) Mantoux Test is induration of 10 mm or more.
But for HIV positive clients, induration of about 5 mm is
considered positive
Signifies exposure to Mycobacterium Tubercle bacilli
Medical and Surgical Nursing
Respiratory System Lecture Notes
Prepared by: Mark Fredderick R. Abejo RN,, MAN
MS Abejo 8
2. Pulse Oximeter
Non-invasive method of continuously monitoring he
oxygen saturation of hemoglobin
A probe or sensor is attached to the fingertip, forehead,
earlobe or bridge of the nose
Sensor detects changes in O2 sat levels by monitoring
light signals generated by the oximeter and reflected by
the blood pulsing through the tissue at the probe
Normal SpO2 = 95% - 100%
< 85% - tissues are not receiving enough O2
Results unreliable in:
Cardiac arrest
Shock
Use of dyes or
vasoconstrictors
Severe anemia
High carbon
monoxide Level
3. Chest X-ray
This is a NON-invasive procedure involving the use of x-
rays with minimal radiation.
The nurse instructs the patient to practice the on cue to
hold his breath and to do deep breathing
Instruct the client to remove metals from the chest.
Rule out pregnancy first.
5. Computed Tomography (CT Scan) and Magnetic Resonance
Imaging ( MRI )
The CT scan is a radiographic procedure that utilizes
x-ray machine.
The MRI uses magnetic field to record the H
+
density of
the tissue.
It does NOT involve the use of radiation.
The contraindications for this procedure are the
following: patients with implanted pacemaker,
patients with metallic hip prosthesis or other metal
implants in the body.
This chest CT scan shows a cross-section of a person
with bronchial cancer. The two dark areas are the lungs. The light
areas within the lungs represent the cancer.
Clear MRI images of lung airways during breathing.
6. Flouroscopy
Studies the lung and chest in motion
Involves the continuous observation of an image
reflected on a screen when exposed to radiation in the
manner of television screen that is activated by an
electrode beam.
Structures of different densities that intercept the X-ray
beam are visualized on the screen in silhouette
7. Indirect Bronchography
A radiopaque medium is instilled directly into the
trachea and the bronchi and the outline of the entire
bronchial tree or selected areas may be visualized
through x-ray.
It reveals anomalies of the bronchial tree and is
important in the diagnosis of bronchiectasis.
Nursing interventions BEFORE Bronchogram
Secure written consent
Check for allergies to sea foods or iodine or
anesthesia
NPO for 6 to 8 hours
Pre-op meds: atropine SO
4
and valium,
topical anesthesia sprayed; followed by local
anesthetic injected into larynx. The nurse must
have oxygen and anti spasmodic agents ready.
Nursing interventions AFTER Bronchogram
Side-lying position
NPO until cough and gag reflexes returned
Instruct the client to cough and deep breathe
client
8. Bronchoscopy
This is the direct inspection and observation of the
larynx, trachea and bronchi through a flexible or rigid
bronchoscope.
Passage of a lighted bronchoscope into the bronchial
tree for direct visualization of the trachea and the
tracheobronchial tree.
Diagnostic uses:
To examine tissues or collect secretions
To determine location or pathologic process
and collect specimen for biopsy
Medical and Surgical Nursing
Respiratory System Lecture Notes
Prepared by: Mark Fredderick R. Abejo RN,, MAN
MS Abejo 9
To evaluate bleeding sites
To determine if a tumor can be resected
surgically
Therapeutic uses
To Remove foreign objects from
tracheobronchial tree
To Excise lesions
To remove tenacious secretions obstructing the
tracheobronchial tree
To drain abscess
To treat post-operative atelectasis
Nursing interventions BEFORE Bronchoscopy
Informed consent/ permit needed
Explain procedure to the patient, tell him what
to expect, to help him cope with the unkown
Atropine (to diminish secretions) is
administered one hour before the procedure
About 30 minutes before bronchoscopy,
Valium is given to sedate patient and allay
anxiety.
Topical anesthesia is sprayed followed by
local anesthesia injected into the larynx
Instruct on NPO for 6-8 hours
Remove dentures, prostheses and contact lenses
The patient is placed supine with
hyperextended neck during the procedure
Nursing interventions AFTER Bronchoscopy
Put the patient on Side lying position
Tell patient that the throat may feel sore with .
Check for the return of cough and gag reflex.
Check vasovagal response.
Watch for cyanosis, hypotension, tachycardia,
arrythmias, hemoptysis, and dyspnea. These
signs and symptoms indicate perforation of
bronchial tree. Refer the patient immediately!
9. Lung Scan
Procedure using inhalation or I.V. injection of a
radioisotope, scans are taken with a scintillation camera.
Imaging of distribution and blood flow in the lungs.
(Measure blood perfusion)
Confirm pulmonary embolism or other blood- flow
abnormalities
Nursing interventions BEFORE the procedure:
Allay the patients anxiety
Instruct the patient to Remain still during the
procedure
Nursing interventions AFTER the procedure
Check the catheter insertion site for bleeding
Assess for allergies to injected radioisotopes
Increase fluid intake, unless contraindicated.
10. Sputum Examination
Laboratory test
Indicated for microscopic examination of the sputum:
Gross appearance, Sputum C&S, AFB staining, and
for Cytologic examination/ Papanicolaou examination
Nursing interventions:
Early morning sputum specimen is to be
collected (suctioning or expectoration)
Rinse mouth with plain water
Use sterile container.
Sputum specimen for C&S is collected before
the first dose of anti-microbial therapy.
For AFB staining, collect sputum specimen for
three consecutive mornings.
11. Biopsy of the Lungs
Percutaneous removal of a small amount of lung tissue
For histologic evaluation
- Transbronchoscopic biopsydone during bronchoscopy,
- Percutaneous needle biopsy
- Open lung biopsy
Medical and Surgical Nursing
Respiratory System Lecture Notes
Prepared by: Mark Fredderick R. Abejo RN,, MAN
MS Abejo 10
Nursing interventions BEFORE the procedure:
Withhold food and fluids
Place obtained written informed consent in the
patients chart.
Nursing interventions AFTER the procedure:
Observe the patient for signs of Pneumothorax
and air embolism
Check the patient for hemoptysis and
hemorrhage
Monitor and record vital signs
Check the insertion site for bleeding
Monitor for signs of respiratory distress
12. Lymph Node Biopsy
Scalene or cervicomediastinal
To assess metastasis of lung cancer
13. Pulmonary Function Test / Studies
Non-invasive test
Measurement of lung volume, ventilation, and diffusing
capacity
Nursing interventions:
Document bronchodilators or narcotics used
before testing
Allay the patients anxiety during the testing
LUNG VOLUMES: (ITER)
Inspiratory reserve volume (3000 mL)
The maximum volume that can be inhaled following a
normal quiet inhalation.
Tidal volume (500 mL)
The volume of air inhaled and exhaled with normal quiet
breathing
Expiratory reserve volume (1100 mL)
The maximum volume that can be exhaled following the
normal quiet exhalation
Residual volume (1200 mL)
The volume of air that remains in the lungs after forceful
exhalation
LUNG CAPACITIES:
Functional Residual Capacity (ERV 1100 mL + RV 1200 mL =
2300 mL )
The volume of air that remains in the lungs after normal,
quiet exhalation
Inspiratory Capacity (TV 500 mL + IRV 3000 mL = 3500 mL )
The amount of air that a person can inspire maximally
after a normal expiration
Vital capacity (IRV 3000 mL + TV 500 mL + ERV 1100 mL =
4600 mL )
The maximum volume of air that can be exhaled after a
maximum inhalation
Reduced in COPD
Total Lung Capacity (IRV 3000 mL + TV 500 mL + ERV 1100
mL + RV 1200 mL = 5800 mL )
Total of all four volumes
14. Arterial Blood Gas
Laboratory test
Indicate respiratory functions
Assess the degree to which the lungs are able to provide
adequate oxygen and remove CO
2
Assess the degree to which the kidneys are able to
reabsorb or excrete bicarbonate.
Assessment of arterial blood for tissue oxygenation,
ventilation, and acid-base status
Arterial puncture is performed on areas where good
pulses are palpable (radial, brachial, or femoral).
Radial artery is the most common site for withdrawal of
blood specimen
Nursing interventions:
Utilize a 10-ml. Pre-heparinized syringe to
prevent clotting of specimen
Soak specimen in a container with ice to
prevent hemolysis
If ABG monitoring will be done, do Allens
test to assess for adequacy of collateral
circulation of the hand (the ulnar arteries)
15. Pulmonary Angiography
This procedure takes X-ray pictures of the pulmonary
blood vessels (those in the lungs).
Because arteries and veins are not normally seen in an X-
ray, a contrast material is injected into one or more
arteries or veins so that they can be seen.
Medical and Surgical Nursing
Respiratory System Lecture Notes
Prepared by: Mark Fredderick R. Abejo RN,, MAN
MS Abejo 11
16. Ventilation - Perfusion Scan
Radioactive albumin injection is part of a nuclear scan
test that is performed to measure the supply of blood
through the lungs.
After the injection, the lungs are scanned to detect the
location of the radioactive particles as blood flows
through the lungs.
The ventilation scan is used to evaluate the ability of air
to reach all portions of the lungs. The perfusion scan
measures the supply of blood through the lungs.
A ventilation and perfusion scan is most often performed
to detect a pulmonary embolus. It is also used to evaluate
lung function in people with advanced pulmonary disease
such as COPD and to detect the presence of shunts
(abnormal circulation) in the pulmonary blood vessels.
17. Thoracentesis
Procedure suing needle aspiration of intrapleural fluid or
air under local anesthesia
Specimen examination or removal of pleural fluid
Nursing intervention BEFORE Thoracentesis
Secure consent
Take initial vital signs
Instruct to remain still, avoid coughing during
insertion of the needle
Inform patient that pressure sensation will be
felt on insertion of needle
Nursing intervention DURING the procedure:
Reassess the patient
Place the patient in the proper position:
Upright or sitting on the edge of
the bed
Lying partially on the side,
partially on the back
Nursing interventions after Thoracentesis
Assess the patients respiratory status
Monitor vital signs frequently
Position the patient on the affected side, as
ordered, for at least 1 hour to seal the puncture
site
Turn on the unaffected side to prevent leakage
of fluid in the thoracic cavity
Check the puncture site for fluid leakage
Auscultate lungs to assess for pneumothorax
Monitor oxygen saturation (SaO
2
) levels
Bed rest
Check for expectoration of blood
RESPIRATORY CARE MODALITIES
1. Oxygen Therapy
Oxygen is a colorless, odorless, tasteless, and dry gas that
supports combustion
Man requires 21% oxygen from the environment in order
to survive
Indication: Hypoxemia
Signs of Hypoxemia
o Increased pulse rate
o Rapid, shallow respiration and dyspnea
o Increased restlessness or lightheadedness
o Flaring of nares
o Substernal or intercostals retractions
o Cyanosis
Low flow oxygen provides partial oxygenation with patient
breathing a combination of supplemental oxygen and room air.
Low-flow administration devices:
o Nasal Cannula 24-45% 2-6 LPM
o Simple Face Mask 0-60% 5-8 LPM
o Partial Rebreathing Mask 60-90% 6-10 LPM
o Non-rebreathing Mask 95-100% 6-15 LPM
o Croupette
o Oxygen Tent
High flow oxygen provides all necessary oxygenation, with
patients breathing only oxygen supplied from the mask and
exhaling through a one-way vent.
High flow administration devices
o Venturi Mask 24-40% 4-10 LPM
Preferred for clients with COPD because it
provides accurate amount of oxygen.
o Face Mask
o Oxygen Hood*
o Incubator / isolette*
Note: * can be used for both low and high flow administration
The nurse should prevent skin breakdown by checking
nares, nose and applying gauze or cotton as necessary
Ensure that COPD patients receive only LOW flow
oxygen because these persons respond to hypoxia, not
increased CO levels.
Medical and Surgical Nursing
Respiratory System Lecture Notes
Prepared by: Mark Fredderick R. Abejo RN,, MAN
MS Abejo 12
2. Tracheobronchial suctioning
Suction only when necessary not routinely
Use the smallest suction catheter if possible
Client should be in semi or high Fowlers position
Use sterile gloves, sterile suction catheter
Hyperventilate client with 100% oxygen before and
after suctioning
Insert catheter with gloved hand (3-5 length of catheter
insertion) without applying suction. Three passes of the
catheter is the maximum, with 10 seconds per pass.
Apply suction only during withdrawal of catheter
The suction pressure should be limited to less than 120
mmHg
When withdrawing catheter rotate while applying
intermittent suction
Suctioning should take only 10 seconds (maximum of 15
seconds)
Evaluate: clear breath sounds on auscultation of the chest.
3. Bronchial Hygiene Measures
Suctioning: oropharyngeal; nasopharyngeal
a. Steam inhalation
The purpose of steam inhalation are as follows:
- to liquefy mucous secretions
- to warm and humidify air
- to relieve edema of airways
- to soothe irritated airways
- to administer medication
It is a dependent nursing function
Inform the client and explain the purpose of the procedure
Place the client in Semi-Fowlers position
Cover the clients eyes with washcloth to prevent irritation
Check the electrical device before use
Place the steam inhalator in a flat, stable surface.
Place the spout 12 18 inches away from the clients nose or
adjust distance as necessary
CAUTION: avoid burns. Cover the chest with towel to
prevent burns due to dripping of condensate from the steam.
Assess for redness on the side of the face which indicates
first degree burns.
To be effective, render steam inhalation therapy for 15 20
minutes
Instruct the client to perform deep breathing and coughing
exercises after the procedure to facilitate expectoration of
mucous secretions.
Provide good oral hygiene after the procedure.
Do after-care of equipment.
b. Aerosol inhalation
done among pediatric clients to administer brochodilators or
mucolytic-expectorants.
.
c. Medimist inhalation
done among adult clients to administer bronchodilators or
mucolytic-expectorants.
4. Chest Physiotheraphy ( CPT )
Includes postural drainage, chest percussion and vibration,
and breathing retraining. Effective coughing is also an
important component.
Goals are removal of bronchial secretions, improved
ventilation, and increased efficiency of respiratory
muscles.
Postural drainage uses specific positions to use gravity to
assist in the removal of secretions.
Vibration loosens thick secretions by percussion or
vibration.
Breathing exercises and breathing retraining improve
ventilation and control of breathing and decrease the
work of breathing.
These are procedures for patients with respiratory
disorders like COPD, cystic fibrosis, lung abscess, and
pneumonia. The therapy is based on the fact that mucus
can be knocked or shaken from airways and helped to
drain from the lungs.
Postural drainage
Use of gravity to aid in the drainage of secretions.
Patient is placed in various positions to promote flow of
drainage from different lung segments using gravity.
Areas with secretions are placed higher than lung
segments to promote drainage.
Patient should maintain each position for 5-15 minutes
depending on tolerability.
Percussion
Produces energy wave that is transmitted through the
chest wall to the bronchi.
The chest is struck rhythmically with cupped hands over
the areas were secretions are located.
Avoid percussion over the spine, kidneys, breast or
incision and broken ribs. Areas should be percussed for
1-2 minutes
Vibration
Works similarly to percussion, where hands are placed on
clients chest and gently but firmly rapidly vibrate hands
against thoracic wall especially during clients exhalation.
This may help dislodge secretions and stimulate cough.
This should be done at least 5-7 times during patient
exhalation.
Medical and Surgical Nursing
Respiratory System Lecture Notes
Prepared by: Mark Fredderick R. Abejo RN,, MAN
MS Abejo 13
Suctioning
Nursing Interventions in CPT
Verify doctors order
Assess areas of accumulation of mucus secretions.
Position to allow expectoration of mucus secretions
by gravity
Place client in each position for 5-10 to 15 minutes
Percussion and vibration done to loosen mucus
secretions
Change position gradually to prevent postural
hypotension
Client is encouraged to cough up and expectorate
sputum
Procedure is best done 60 to 90 minutes before
meals or in the morning upon awakening and at
bedtime.
Provide good oral care after the procedure
5. Incentive Spirometry
Types: volume and flow
Device ensures that a volume of air is inhaled and the
patient takes deep breaths.
Used to prevent or treat atelectasis
To enhance deep inhalation
Nursing care
Positioning of patient, teach and encourage use,
set realistic goals for the patient, and record the
results.
6. Closed Chest Drainage ( Thoracostomy Tube )
Chest tube is used to drain fluid and air out of the
mediastinum or pleural space into a collection chamber
to help re-establish normal negative pressure for lung re-
expansion.
Purposes
To remove air and/or fluids from the pleural space
To reestablish negative pressure and re-expand the
lungs
Procedure
The chest tube is inserted into the affected chest
wall at the level of 2
nd
to 3
rd
intercostals space to
release air or in the fourth intercostals space to
remove fluid.
Types of Bottle Drainage
One-bottle system
The bottle serves as drainage and water-seal
Immerse tip of the tube in 2-3 cm of sterile NSS to
create water-seal.
Keep bottle at least 2-3 feet below the level of the
chest to allow drainage from the pleura by gravity.
Never raise the bottle above the level of the heart
to prevent reflux of air or fluid.
Assess for patency of the device
Observe for fluctuation of fluid along the tube. The
fluctuation synchronizes with the respiration.
Observe for intermittent bubbling of fluid;
continues bubbling means presence of air-leak
In the absence of fluctuation:
Suspect obstruction of the device
Assess the patient first, then if patient is stable
Check for kinks along tubing;
Milk tubing towards the bottle (If the hospital allows the
nurse to milk the tube)
If there is no obstruction, consider lung re-expansion;
(validated by chest x-ray)
Air vent should be open to air.
Two-bottle system
If not connected to the suction apparatus
The first bottle is drainage bottle;
The second bottle is water-seal bottle
Observe for fluctuation of fluid along the tube
(water-seal bottle or the second bottle) and
intermittent bubbling with each respiration.
NOTE! IF connected to suction apparatus
1. The first bottle is the drainage and water-seal bottle;
2. The second bottle is suction control bottle.
3. Expect continuous bubbling in the suction control bottle;
4. Intermittent bubbling and fluctuation in the water-seal
5. Immerse tip of the tube in the first bottle in 2 to 3 cm of
sterile NSS
6. Immerse the tube of the suction control bottle in 10 to 20
cm of sterile NSS to stabilize the normal negative
pressure in the lungs.
7. This protects the pleura from trauma if the suction
pressure is inadvertently increased
Medical and Surgical Nursing
Respiratory System Lecture Notes
Prepared by: Mark Fredderick R. Abejo RN,, MAN
MS Abejo 14
Three-bottle system
The first bottle is the drainage bottle;
The second bottle is water seal bottle
The third bottle is suction control bottle.
Observe for intermittent bubbling and
fluctuation with respiration in the water- seal
bottle
Continuous GENTLE bubbling in the suction
control bottle. These are the expected observations.
Suspect a leak if there is continuous bubbling in
the WATER seal bottle or if there is VI GOROUS
bubbling in the suction control bottle.
The nurse should look for the leak and report the
observation at once. Never clamp the tubing
unnecessarily.
If there is NO fluctuation in the water seal bottle, it may mean
TWO things
Either the lungs have expanded or the system is NOT
functioning appropriately.
In this situation, the nurse refers the observation to the
physician, who will order for an X-ray to confirm the
suspicion.
Important Nursing considerations
Encourage doing the following to promote drainage:
Deep breathing and coughing exercises
Turn to sides at regular basis
Ambulate
ROM exercise of arms
Mark the amount of drainage at regular intervals
Avoid frequent milking and clamping of the tube to
prevent tension pneumothorax
What the nurse should do if:
If there is continuous bubbling:
The nurse obtains a toothless clamp
Close the chest tube at the point where it exits the chest
for a few seconds.
If bubbling in the water seal bottle stops, the leak is
likely in the lungs,
But if the bubbling continues, the leak is between the
clamp and the bottle chamber.
Next, the nurse moves the clamp towards the bottle checking the
bubbling in the water seal bottle.
If bubbling stops, the leak is between the clamp
and the distal part including the bottle.
But if there is persistent bubbling, it means that the
drainage unit is leaking and the nurse must obtain
another set.
In the event that the water seal bottle breaks, the
nurse temporarily kinks the tube and must obtain a
receptacle or container with sterile water and
immerse the tubing.
She should obtain another set of sterile bottle as
replacement. She should NEVER CLAMP the tube
for a longer time to avoid tension pneumothorax.
In the event the tube accidentally is pulled out, the
nurse obtains vaselinized gauze and covers the
stoma.
She should immediately contact the physician.
Removal of chest tubedone by physician
The nurse Prepares:
Petrolatum Gauze
Suture removal kit
Sterile gauze
Adhesive tape
Place client in semi-Fowlers position
Instruct client to exhale deeply, then inhale and do
valsalva maneuver as the chest tube is removed.
Chest x-ray may be done after the chest tube is
removed
Asses for complications: subcutaneous emphysema;
respiratory distress
7. Artificial Airway
a. Oral airways- these are shorter and often have a larger lumen.
They are used to prevent the tongue form falling backward.
b. Nasal airways- these are longer and have smaller lumen Which
causes greater airway resistance
c. Tracheostomy- this is a temporary or permanent surgical
opening in the trachea. A tube is inserted to allow ventilation and
removal of secretions. It is indicated for emergency airway access
for many conditions. The nurse must maintain tracheostomy care
properly to prevent infection.
RESPIRATORY DISEASES AND
DISORDERS
I. PNEUMONIA inflammation of the lung parenchyma
leading to pulmonary consolidation because alveoli is filled
with exudates
A. ETIOLOGIC AGENTS
1. Streptococcus pneumoniae (pneumococcal
pneumonia)
2. Hemophilus influenzae (bronchopneumonia)
3. Klebsiella pneumoniae
4. Diplococcus pneumoniae
5. Escherichia coli
6. Pseudomonas aeruginosa
Medical and Surgical Nursing
Respiratory System Lecture Notes
Prepared by: Mark Fredderick R. Abejo RN,, MAN
MS Abejo 15
B. HIGH RISK GROUPS
1. Children less than 5 yo
2. Elderly
C. PREDISPOSING FACTORS
1. Smoking
2. Air pollution
3. Immunocompromised
(+) AIDS
Kaposis Sarcoma
Pneumocystis Carinii Pneumonia
DOC: Zidovudine (Retrovir)
Bronchogenic Ca
4. Prolonged immobility (hypostatic pneumonia)
5. Aspiration of food (aspiration pneumonia)
6. Over fatigue
D. SIGNS AND SYMPTOMS
1. Productive cough, greenish to rusty
2. Dyspnea with prolong expiratory grunt
3. Fever, chills, anorexia, general body malaise
4. Cyanosis
5. Pleuritic friction rub
6. Rales/crackles on auscultation
7. Abdominal distention paralytic ileus
E. DIAGNOSTICS
1. Sputum GS/CS confirmatory; type and sensitivity;
(+) to cultured microorganism
2. CXR (+) pulmonary consolidation
3. CBC
Elevated ESR (rate of erythropoeisis) N = 0.5-
1.5% (compensatory mech to decreased O2)
Elevated WBC
4. ABG PO2 decreased (hypoxemia)
F. NURSING MANAGEMENT
1. Enforce CBR (consistent to all respi disorders)
2. Strict respiratory isolation
3. Administer medications as ordered
Broad spectrum antibiotics
Penicillin pneumococcal infections
Tetracycline
Macrolides
Azithromycin (OD x 3/days)
1. Too costly
2. Only se: ototoxicity transient
hearing loss
Anti-pyretics
Mucolytics/expectorants
4. Administer O2 inhalation as ordered
5. Force fluids to liquefy secretions
6. Institute pulmonary toilet measures to promote
expectoration of secretions
DBE, Coughing exercises, CPT
(clapping/vibration), Turning and repositioning
7. Nebulize and suction PRN
8. Place client of semi-fowlers to high fowlers
9. Provide a comfortable and humid environment
10. Provide a dietary intake high in CHO, CHON,
Calories and Vit C
11. Assist in postural drainage
Patient is placed in various position to drain
secretions via force of gravity
Usually, it is the upper lung areas which are
drained
Nursing management:
Monitor VS and BS
Best performed before meals/breakfast or
2-3 hours p.c. to prevent gastroesophageal
reflux or vomiting (pagkagising maraming
secretions diba? Nakukuha?)
Encourage DBE
Administer bronchodilators 15-30 minutes
before procedure
Stop if pt. cant tolerate the procedure
Provide oral care after procedure as it may
affect taste sensitivity
Contraindications:
Unstable VS
Hemoptysis
Increased ICP
Increased IOP (glaucoma)
12. Provide pt health teaching and d/c planning
Avoidance of precipitating factors
Prevention of complications
Atelectasis
Meningitis
Regular compliance to medications
Importance of ffup care
II. PULMONARY TUBERCULOSIS (KOCHS DISEASE)
infection of the lung parenchyma caused by invasion of
mycobacterium tuberculosis or tubercle bacilli (gram negative,
acid fast, motile, aerobic, easily destroyed by heat/sunlight)
A. PRECIPITATING FACTORS
1. Malnutrition
2. Overcrowding
3. Alcoholism: Depletes VIT B1 (thiamin) alcoholic
beriberi malnutrition
4. Physical and emotional stress
5. Ingestion of infected cattle with M. bovis
6. Virulence (degree of pathogenecity)
B. MODE OF TRANSMISSION: Airborne droplet
infection
Tracheostomy usually done at bedside, 10-20 minutes
Stress test: 30 minutes
Mammography: 10-20 minutes
LARYNGOSPASM tracheostomy STAT
OR Tracheostomy: laryngeal, thyroid, neck CA
DIAPHRAGM primary muscle for respiration
INTERCOSTAL MUSCLES secondary muscle for respiration
ALVEOLI (Acinar cells) functional unit of the lungs; site for gas
exchange (via diffusion)
VENTILATION movement of air in and out of the lungs
RESPIRATION lungs to cells
Internal
External
RETROLENTAL FIBROPLASIA retinopathy/blindness in
immaturity d/t high O2 flow in pedia patients
Medical and Surgical Nursing
Respiratory System Lecture Notes
Prepared by: Mark Fredderick R. Abejo RN,, MAN
MS Abejo 16
C. SIGNS AND SYMPTOMS
1. Productive cough (yellowish)
2. Low grade afternoon fever, night sweats
3. Dyspnea, anorexia, malaise, weight loss
4. Chest/back pain
5. Hemoptysis
D. DIAGNOSTICS
1. Skin testing
Mantoux test PPD
Induration width (within 48-72 h)
8-10 mm (DOH)
10-14 mm (WHO)
5 mm in AIDS patients is +
indicates previous exposure to tubercle
bacilli
2. Sputum AFB (+) tubercle bacilli
3. CXR (+) pulmo infiltrated due to caseous necrosis
4. CBC elevated WBC
E. NURSING MANAGEMENT
1. Enforce CBR
2. Institute strict respiratory isolation
3. Administer O2 inhalation
4. Forced fluids
5. Encourage DBE and coughing
NO CLAPPING in chronic PTB d/t
hemoptysis may lead to hemorrhage
6. Nebulize and suction PRN
7. Provide comfortable and humid environment
8. Institute short course chemotherapy
Intensive phase
INH
SE: peripheral neuritis (increase vit
B6 or pyridoxine
Rifampicin
SE: red orange color of bodily
secretions
PZA
May be replaced with Ethambutol
(SE: optic neuritis) if (+)
hypersensitivity to drug
SE: allergic reactions; hepatotoxicity
and nephrotoxicity
1. Monitor liver enzymes
2. Monitor BUN and CREA
INH given for 4 months, PZA and
Rifampicin is given for 2 months, A.C. to
facilitate absorption
These 3 drugs are given simultaneously to
prevent development of resistance
Standard Regimen
Streptomycin injection (aminoglycosides)
Neomycin, Amikacin, Gentamycin
1. common SE: 8
th
CN damage
tinnitus hearing loss
ototoxicity
2. nephrotoxicity
a. BUN (N = 10-20)
b. CREA (N = 8-10)
9. Health teaching and d/c planning
Avoidance of precipitating factors : alcoholism,
overcrowding
Prevention of complications
Atelectasis
Military TB (extrapulmonary TB:
meningeal, Potts, adrenal glands, skin,
cornea)
Strict compliance to medications
Never double the dose! Continue taking
the meds if missed a day)
Diet modifications: increased CHON, CHO,
Calories, Vit C
Importance of ffup care
III. HISTOPLASMOSIS acute fungal infection caused by
inhalation of contaminated dust with Histoplasma capsulatum
from birds manure
A. PREDISPOSING FACTORS
Inhalation of contaminated dust
2. SIGNS AND SYMPTOMS
PTB like symptoms
Productive cough
Fever, chills, anorexia, generalized body
malaise
Cyanosis
Chest and joint pains
Dyspnea
Hemoptysis
3. DIAGNOSTICS
Histoplasmin skin test is (+)
ABG analysis reveals pO2 low
4. NURSING MANAGEMENT
Enforce CBG
Administer meds as ordered
Antifungal agents
Amphotericin B (Fungizone) SE:
nephrotoxicity and hypokalemia
Monitor transaminases, BUN and
CREA
Corticosteroids
Anti-pyretics
Mucolytics/expectorants
Administer oxygen inhalation as ordered
Forced fluids
Nebulize and suction as necessary
Prevent complications
Bronchiectasis, atelectasis
Prevention of spread
Spraying of breeding places
Kill bird and owner! Hehe!
CHRONIC OBSTRUCTIVE PULMONARY DISEASES
1. Chronic Bronchitis
2. Bronchial Asthma
3. Bronchiectasis
4. Pulmonary Emphysema
Medical and Surgical Nursing
Respiratory System Lecture Notes
Prepared by: Mark Fredderick R. Abejo RN,, MAN
MS Abejo 17
I. CHRONIC BRONCHITIS (Blue Bloaters) Inflammation
of the bronchi due to hypertrophy or hyperplasia of goblet
mucous producing cells leading to narrowing of smaller
airways
A. PREDISPOSING FACTORS
1. Smoking
2. Air pollution
B. SIGNS AND SYMPTOMS
1. Consistent productive cough
2. Dyspnea on exertion with prolonged expiratory
grunt
3. Anorexia and generalized body malaise
4. Cyanosis
5. Scattered rales/rhonchi
6. Pulmonary hypertension
Peripheral edema
Cor pulmonale
C. DIAGNOSTICS
1. ABG analysis: decreased PO2, increased PCO2,
respiratory acidosis; hypoxemia cyanosis
D. NURSING MANAGEMENT
1. Enforce CBR
2. Administer medications as ordered
Bronchodilators
Antimicrobials
Corticosteroids
Mucolytics/expectorants
3. Low inflow O2 admin; high inflow will cause
respiratory arrest
4. Force fluids
5. Nebulize and suction client as needed
6. Provide comfortable and humid environment
7. Health teaching and d/c planning
avoidance of smoking
prevent complications
CO2 narcosis coma
Cor pulmonale
Pleural effusion
Pneumothorax
Regular adherence to meds
Importance of ffup care
II. BRONCHIAL ASTHMA reversible inflammatory lung
condition caused by hypersensitivity to allergens leading to
narrowing of smaller airways
A. PREDISPOSING FACTORS
1. Extrinsic (Atopic/Allergic Asthma)
Pollens, dust, fumes, smoke, fur, dander, lints
2. Intrinsic (Non-Atopic/Non-Allergic)
Drugs (aspirin, penicillin, B-blockers)
Foods (seafoods, eggs, chicken, chocolate)
Food additives (nitrates, nitrites)
Sudden change in temperature, humidity and
air pressure
Genetics
Physical and emotional stress
3. Mixed type combination of both
B. SIGNS AND SYMPTOMS
1. Cough that is productive
2. Dyspnea
3. Wheezing on expiration
4. Tachycardia, palpitations and diaphoresis
5. Mild apprehension, restlessness
6. Cyanosis
C. DIAGNOSTICS
1. PFT decreased vital lung capacity
2. ABG analysis PO2 decreased
D. NURSING MANAGEMENT
1. Enforce CBR
2. Administer medications as ordered
Bronchodilators administer first to facilitate
absorption of corticosteroids
Inhalation
MDI
Corticosteroids
Mucolytics/expectorants
Mucomyst
Antihistamine
3. Administer oxygen inhalation as ordered
4. Forced fluids
5. Nebulize and suction patient as necessary
6. Encourage DBE and coughing
7. Provide a comfortable and humid environment
8. Health teaching and d/c planning
Avoidance of precipitating factors
Prevention of complications
Medical and Surgical Nursing
Respiratory System Lecture Notes
Prepared by: Mark Fredderick R. Abejo RN,, MAN
MS Abejo 18
Status asthmaticus
DOC: Epinephrine
Aminophylline drip
Emphysema
Regular adherence to medications
Importance of ffup care
III. BRONCHIECTASIS permanent dilation of the bronchus
due to destruction of muscular and elastic tissue of the
alveolar walls (subject to surgery)
A. PREDISPOSING FACTORS
1. Recurrent lower respiratory tract infection
Histoplasmosis
2. Congenital disease
3. Presence of tumor
4. Chest trauma
B. SIGNS AND SYMPTOMS
1. Consistent productive cough
2. Dyspnea
3. Presence of cyanosis
4. Rales and crackles
5. Hemoptysis
6. Anorexia and generalized body malaise
C. DIAGNOSTICS
1. ABG analysis reveals low PO2
2. Bronchoscopy direct visualization of bronchi
lining using a fibroscope
Pre-op
Secure consent
Explain procedure
NPO 4-6 hours
Monitor VS and breath sounds
Post-operative
Feeding initiated upon return of gag reflex
Instruct client to avoid talking, coughing
and smoking as it may irritate respiratory
tract
Monitor for s/sx of frank or gross bleeding
Monitor for signs of laryngeal spasm
DOB and SOB prepare trache set
D. SURGERY
1. Segmental lobectomy
2. Pneumonectomy
Most feared complications
Atelectasis
Cardiac tamponade: muffled heart sounds,
pulsus paradoxus, HPN
E. NURSING MANAGEMENT
1. Enforce CBR
2. Low inflow O2 admin; high inflow will cause
respiratory arrest
3. Administer medications as ordered
Bronchodilators
Antimicrobials
Corticosteroids (5-10 minutes after
bronchodilators)
Mucolytics/expectorants
4. Force fluids
5. Nebulize and suction client as needed
6. Provide comfortable and humid environment
7. Health teaching and d/c planning
Avoidance of smoking
Prevent complications
Atelectasis
CO2 narcosis coma
Cor pulmonale
Pleural effusion
Pneumothorax
Regular adherence to meds
Importance of ffup care
IV. PULMONARY EMPHYSEMA terminal and irreversible
stage of COPD characterized by :
Inelasticity of alveoli
Air trapping
Maldistribution of gasses (d/t increased air trapping)
Overdistention of thoracic cavity (Barrel chest)
compensatory mechanism increased AP diameter
Medical and Surgical Nursing
Respiratory System Lecture Notes
Prepared by: Mark Fredderick R. Abejo RN,, MAN
MS Abejo 19
A. PREDISPOSING FACTORS
1. Smoking
2. Air pollution
3. Hereditary: involves alpha-1 antitrypsin for
elastase production for recoil of the alveoli
4. Allergy
5. High risk group elderly degenerative
decreased vital lung capacity and thinning of
alveolar lobes
B. SIGNS AND SYMPTOMS
1. Productive cough
2. Dyspnea at rest
3. Prolonged expiratory grunt
4. Resonance to hyperresonance
5. Decreased tactile fremitus
6. Decreased breath sounds ( if (-) BS lung collapse)
7. Barrel chest
8. Anorexia and generalized body malaise
9. Rales or crackles
10. Alar flaring
11. Pursed-lip breathing (to eliminate excess CO2)
C. DIAGNOSTICS
1. ABG analysis reveal
Panlobular, centrilobular PO2 elevation and
PCO2 depression respiratory acidosis (blue
bloaters)
Panacinar/centriacinar PCO2 depression and
PO2 elevation (pink puffers hyperaxemia)
2. Pulmo function test decreased vital lung capacity
D. NURSING MANAGEMENT
1. Enforce CBR
2. Administer medications as ordered
Bronchodilators
Antimicrobials
Corticosteroids
Mucolytics/expectorants
3. Low inflow O
2
admin; high inflow will cause
respiratory arrest and oxygen toxicity
4. Force fluids
5. Pulmonary toilet
6. Nebulize and suction client as needed
7. Institute PEEP in mechanical ventilation
PEEP positive end expiratory pressure
allows for maximum alveolar diffusion
prevent lung collapse
8. Provide comfortable and humid environment
9. Diet modifications: high calorie, CHON, CHO,
vitamins and minerals
10. Health teaching and d/c planning
Avoidance of smoking
Prevent complications
Atelectasis
CO
2
narcosis coma
Cor pulmonale
Pleural effusion
Pneumothorax
Regular adherence to meds
Importance of ffup care
RESTRICTIVE LUNG DISEASE
V. PNEUMOTHORAX partial or complete collapse of the
lungs due to accumulation of air in pleural space
A. TYPES
1. Spontaneous air enters pleural space without an
obvious cause
Ruptured blebs (alveolar filled sacs)
inflammatory lung conditions
2. Open air enters pleural space through an opening
in pleural wall (most common)
Gun shot wounds
Multiple stab wounds
3. Tension air enters pleural space during inspiration
and cannot escape leading to overdistention of the
thoracic cavity mediastinal shift to the affected
side (ie. Flail chest) paradoxical breathing
B. PREDISPOSING FACTORS
1. Chest trauma
2. Inflammatory lung condition
3. tumors
C. SIGNS AND SYMPTOMS
1. Sudden sharp chest pain, dyspnea, cyanosis
2. Diminished breath sounds
3. Cool, moist skin
4. Mild restlessness and apprehension
5. Resonance to hyperresonance
D. DIAGNOSTICS
1. ABG analysis: PO2 decreased
2. CXR confirms collapse of lungs
E. NURSING MANAGEMENT
1. Assist in endotracheal intubation
2. Assist in thoracentesis
3. Administer meds as ordered
Narcotic analgesics Morphine sulfate
Antibiotics
4. Assist in CTT to H20 sealed drainage
Das könnte Ihnen auch gefallen
- Fluid and Electrolytes for Nursing StudentsVon EverandFluid and Electrolytes for Nursing StudentsBewertung: 5 von 5 Sternen5/5 (12)
- Lecture Notes on Anatomy and Physiology of the Cardiovascular SystemDokument18 SeitenLecture Notes on Anatomy and Physiology of the Cardiovascular SystemLudwigJayBarayuga100% (5)
- Medsurg Cardio Ana&PhysioDokument6 SeitenMedsurg Cardio Ana&Physiorabsibala80% (10)
- Cardiac DrugsDokument10 SeitenCardiac Drugssurviving nursing school100% (3)
- Cardiac DisordersDokument15 SeitenCardiac Disordersgold_enriquez100% (3)
- Genito-Urinary Nursing GuideDokument7 SeitenGenito-Urinary Nursing Guideshenric16Noch keine Bewertungen
- Respiratory DisordersDokument15 SeitenRespiratory Disordersmnlstr100% (5)
- Chapter 14 Fluid and Electrolytes ChartsDokument7 SeitenChapter 14 Fluid and Electrolytes ChartsBNA_RN100% (3)
- Mus Culo SkeletalDokument16 SeitenMus Culo Skeletalshenric16100% (2)
- Medical Surgical Nursing Cardio Vascular System ClassDokument15 SeitenMedical Surgical Nursing Cardio Vascular System Classvallal100% (2)
- The GastroDokument25 SeitenThe Gastroangel_maui100% (7)
- Endocrine NursingDokument2 SeitenEndocrine NursingUnclePorkchop94% (34)
- Adult III Cardiac Study GuideDokument15 SeitenAdult III Cardiac Study GuideNursingSchoolNotes100% (6)
- Cardiovascular SystemDokument10 SeitenCardiovascular Systemsurviving nursing school100% (2)
- Cardiac NursingDokument26 SeitenCardiac Nursingjgcriste95% (20)
- Heart Anatomy, Function, Diseases and TestsDokument62 SeitenHeart Anatomy, Function, Diseases and TestsJean Soriano98% (65)
- FLASH CardsDokument3 SeitenFLASH Cardsclarheena100% (2)
- Respiratory Exam GuideDokument18 SeitenRespiratory Exam GuideIbi Yulia Setyani100% (1)
- Nursing Memory JoggersDokument2 SeitenNursing Memory JoggersMarcus, RN96% (24)
- Lower Respiratory Study SheetDokument13 SeitenLower Respiratory Study SheetJune Rhoades100% (2)
- MAP, CO, and SV+HRDokument11 SeitenMAP, CO, and SV+HRjenwiley318096% (73)
- Neurologic NursingDokument14 SeitenNeurologic Nursingtheglobalnursing100% (6)
- Fluid and Electrolytes Study GuideDokument16 SeitenFluid and Electrolytes Study GuideDianaNursing96% (28)
- Lab ValuesDokument3 SeitenLab Valuessurviving nursing schoolNoch keine Bewertungen
- Gastrointestinal NursingDokument8 SeitenGastrointestinal Nursingohsnapitslei90% (10)
- Cardiac Notes NursingDokument16 SeitenCardiac Notes NursingYemaya8494% (17)
- Cardiac DrugsDokument5 SeitenCardiac Drugseric100% (17)
- Renal and Urinary DisordersDokument11 SeitenRenal and Urinary DisordersChristian Espanilla100% (4)
- Resp Lecture NotesDokument18 SeitenResp Lecture Notessurviving nursing schoolNoch keine Bewertungen
- Medical Surgical Nursing PinoyDokument67 SeitenMedical Surgical Nursing Pinoyalfred31191% (23)
- Medical Surgical NursingDokument59 SeitenMedical Surgical NursingChey Dianne Seriña100% (11)
- Med Surg Study GuideDokument98 SeitenMed Surg Study Guideprogramgrabber100% (2)
- Cardiovascular Nursing Bullet Points I PDFDokument4 SeitenCardiovascular Nursing Bullet Points I PDFKhalid Epping100% (3)
- Cardiac Drugs Study Guide CourseDokument19 SeitenCardiac Drugs Study Guide CourseAmanda Brittain100% (6)
- Medical Surgical Nursing PathophysiologyDokument23 SeitenMedical Surgical Nursing Pathophysiologymarc joseph100% (2)
- Respiratory Care Review: An Intense Look at Respiratory Care Through Case StudiesVon EverandRespiratory Care Review: An Intense Look at Respiratory Care Through Case StudiesNoch keine Bewertungen
- The 12-Lead Electrocardiogram for Nurses and Allied ProfessionalsVon EverandThe 12-Lead Electrocardiogram for Nurses and Allied ProfessionalsNoch keine Bewertungen
- Nursing: Lab Values: a QuickStudy Laminated 6-Page Reference GuideVon EverandNursing: Lab Values: a QuickStudy Laminated 6-Page Reference GuideNoch keine Bewertungen
- Pathophysiology of Nursing DemystifiedVon EverandPathophysiology of Nursing DemystifiedBewertung: 5 von 5 Sternen5/5 (1)
- A Handbook for Student Nurses, 201617 edition: Introducing key issues relevant for practiceVon EverandA Handbook for Student Nurses, 201617 edition: Introducing key issues relevant for practiceBewertung: 4 von 5 Sternen4/5 (1)
- Schaum's Outline of Emergency Nursing: 242 Review QuestionsVon EverandSchaum's Outline of Emergency Nursing: 242 Review QuestionsBewertung: 4.5 von 5 Sternen4.5/5 (3)
- Dimensional Analysis For Nursing StudentsVon EverandDimensional Analysis For Nursing StudentsNoch keine Bewertungen
- Nursing Study Guide: Your Nursing Assistant To Do Well In SchoolVon EverandNursing Study Guide: Your Nursing Assistant To Do Well In SchoolBewertung: 3 von 5 Sternen3/5 (2)
- Nursing Mnemonics: The Ultimate Tips and Notes For NursesVon EverandNursing Mnemonics: The Ultimate Tips and Notes For NursesBewertung: 5 von 5 Sternen5/5 (1)
- The Basics: A Comprehensive Outline of Nursing School ContentVon EverandThe Basics: A Comprehensive Outline of Nursing School ContentBewertung: 5 von 5 Sternen5/5 (3)
- Schaum's Outline of Critical Care Nursing: 250 Review QuestionsVon EverandSchaum's Outline of Critical Care Nursing: 250 Review QuestionsBewertung: 5 von 5 Sternen5/5 (1)
- Cardiovascular Nursing: Scope and Standards of PracticeVon EverandCardiovascular Nursing: Scope and Standards of PracticeBewertung: 5 von 5 Sternen5/5 (2)
- FUNDAMENTALS OF NURSING: Passbooks Study GuideVon EverandFUNDAMENTALS OF NURSING: Passbooks Study GuideBewertung: 5 von 5 Sternen5/5 (1)
- Nursing Fundamentals DeMYSTiFieD, Second EditionVon EverandNursing Fundamentals DeMYSTiFieD, Second EditionBewertung: 2 von 5 Sternen2/5 (2)
- Nursing Fundamentals DeMYSTiFieD: A Self-Teaching GuideVon EverandNursing Fundamentals DeMYSTiFieD: A Self-Teaching GuideNoch keine Bewertungen
- PATHOPHYSIOLOGY: Passbooks Study GuideVon EverandPATHOPHYSIOLOGY: Passbooks Study GuideBewertung: 4.5 von 5 Sternen4.5/5 (2)
- COMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideVon EverandCOMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideNoch keine Bewertungen
- MEDICAL-SURGICAL NURSE: Passbooks Study GuideVon EverandMEDICAL-SURGICAL NURSE: Passbooks Study GuideNoch keine Bewertungen
- Fhsis Annual 2018Dokument496 SeitenFhsis Annual 2018shenric16Noch keine Bewertungen
- RA 11223 Universal Health Care ActDokument18 SeitenRA 11223 Universal Health Care Actrommel mendozaNoch keine Bewertungen
- Evidence Based Nursing PracticeDokument21 SeitenEvidence Based Nursing Practiceshenric16Noch keine Bewertungen
- Philippine Government Policies On Maternal, Newborn and Child Health and NutritionDokument20 SeitenPhilippine Government Policies On Maternal, Newborn and Child Health and Nutritioncarlos-tulali-1309100% (33)
- Drug StudyDokument40 SeitenDrug Studyapi-374468390% (61)
- Health Approach To Albularyo Hilots and HealersDokument17 SeitenHealth Approach To Albularyo Hilots and HealersPaul Lexus Gomez LorenzoNoch keine Bewertungen
- Uhc Irr DraftDokument107 SeitenUhc Irr Draftshenric16Noch keine Bewertungen
- Evidence Based Nursing PracticeDokument21 SeitenEvidence Based Nursing Practiceshenric16Noch keine Bewertungen
- Anti Psychotic DrugsDokument2 SeitenAnti Psychotic DrugsJohn Corpuz100% (1)
- HUMAN SEXUALITYDokument37 SeitenHUMAN SEXUALITYshenric16Noch keine Bewertungen
- Nursing Board Exam Test Drill 3Dokument2 SeitenNursing Board Exam Test Drill 3Kira100% (15)
- Proper Patient Positioning Techniques in the ORDokument33 SeitenProper Patient Positioning Techniques in the ORshenric16Noch keine Bewertungen
- Health Teaching PDFDokument1 SeiteHealth Teaching PDFshenric16Noch keine Bewertungen
- Professional Adjustment Leadership Management and ResearchDokument10 SeitenProfessional Adjustment Leadership Management and Researchshenric16100% (1)
- Fundamentals of NursingDokument31 SeitenFundamentals of NursingAngelica Soriano93% (14)
- Palmer Complete Edited Royal PentagonDokument26 SeitenPalmer Complete Edited Royal Pentagonshenric16100% (1)
- Community Health Nursing Practice Questions With RationalesDokument15 SeitenCommunity Health Nursing Practice Questions With RationalesFelice Lamzon Labrador100% (2)
- Community Health Nursing Practice Questions With RationalesDokument15 SeitenCommunity Health Nursing Practice Questions With RationalesFelice Lamzon Labrador100% (2)
- Community Health Nursing Practice Questions With RationalesDokument15 SeitenCommunity Health Nursing Practice Questions With RationalesFelice Lamzon Labrador100% (2)
- 100 Item Comprehensive Exam With Answers and RationaleDokument21 Seiten100 Item Comprehensive Exam With Answers and RationaleAijem Ryan93% (15)
- Maternal Ob NotesDokument37 SeitenMaternal Ob Notesshenric16Noch keine Bewertungen
- Course Audit Professional AdjustmentDokument9 SeitenCourse Audit Professional Adjustmentshenric16Noch keine Bewertungen
- Reviewer For NleDokument14 SeitenReviewer For Nleshenric16Noch keine Bewertungen
- Maternal Ob NotesDokument37 SeitenMaternal Ob Notesshenric16Noch keine Bewertungen
- Cognitive DisordersDokument2 SeitenCognitive DisordersSherrizah Alexis Naag NavaNoch keine Bewertungen
- Community Health NursingDokument49 SeitenCommunity Health Nursingshenric16Noch keine Bewertungen
- Community Health Nursing Practice Questions With RationalesDokument15 SeitenCommunity Health Nursing Practice Questions With RationalesFelice Lamzon Labrador100% (2)
- Final Outline Psychiatric NursingDokument52 SeitenFinal Outline Psychiatric Nursingshenric16100% (1)
- Nle - July 2011Dokument12 SeitenNle - July 2011shenric16100% (1)
- Community Health NursingDokument49 SeitenCommunity Health Nursingshenric16Noch keine Bewertungen
- Pex 07 01Dokument6 SeitenPex 07 01Stacy Cudjoe100% (1)
- Yoga Breathing Techniques - Implications For Stress Management, Health, and Psychophysiological ResearchDokument44 SeitenYoga Breathing Techniques - Implications For Stress Management, Health, and Psychophysiological ResearchTheArtofInspirationNoch keine Bewertungen
- Portable Spirometer Using Air Pressure Sensor MPX5500DP Based On Microcontroller Arduino UnoDokument10 SeitenPortable Spirometer Using Air Pressure Sensor MPX5500DP Based On Microcontroller Arduino UnoBiomed TNoch keine Bewertungen
- Lecture 5. Gas Exchange: Cellular Respiration, Oxidative Processes Within External Respiration, Exchange of O2 and CO2Dokument24 SeitenLecture 5. Gas Exchange: Cellular Respiration, Oxidative Processes Within External Respiration, Exchange of O2 and CO2Jay JayNoch keine Bewertungen
- MYP Biology Booklet # 3 Grade9 - MS1Dokument27 SeitenMYP Biology Booklet # 3 Grade9 - MS1Aref Dahabrah100% (1)
- 5-Pulmonary Function TestsDokument35 Seiten5-Pulmonary Function TestsDoha JKNoch keine Bewertungen
- DR Amsalu Bekele Ass - Professor of Medicine Head of Chest Unit Department of Internal Medicine Addis Ababa University, School of Medicine Addis Ababa, EthiopiaDokument81 SeitenDR Amsalu Bekele Ass - Professor of Medicine Head of Chest Unit Department of Internal Medicine Addis Ababa University, School of Medicine Addis Ababa, EthiopiaBethelhem BirhanuNoch keine Bewertungen
- Vedic MathematicsDokument46 SeitenVedic MathematicsJitendra PatelNoch keine Bewertungen
- JoS - Breathing Exercises For SatanistsDokument7 SeitenJoS - Breathing Exercises For SatanistsJosh SandsNoch keine Bewertungen
- Ars NovaDokument18 SeitenArs NovaAndre SantosNoch keine Bewertungen
- Chapter 19 PULMONARY FUNCTION TESTINGDokument13 SeitenChapter 19 PULMONARY FUNCTION TESTINGZahra Margrette Schuck0% (1)
- Yoga Therapy in Practice: Prânâyâma Can Be Practiced SafelyDokument5 SeitenYoga Therapy in Practice: Prânâyâma Can Be Practiced SafelyJayaprakash ParamasivamNoch keine Bewertungen
- CHPT 42 Circulation Gas Exchange 2014Dokument32 SeitenCHPT 42 Circulation Gas Exchange 2014azn2017Noch keine Bewertungen
- Gas Exchange NotesDokument10 SeitenGas Exchange NotesSamantha PiersNoch keine Bewertungen
- PEX RESPI Jiveen RajendraDokument9 SeitenPEX RESPI Jiveen RajendraJiveenNoch keine Bewertungen
- Lab 06 SpirometryDokument28 SeitenLab 06 SpirometryMâřâh MöHămmădNoch keine Bewertungen
- The Principles of Voice Production in Choral Singing by Petronella LaidlawDokument8 SeitenThe Principles of Voice Production in Choral Singing by Petronella LaidlawCharlotteNoch keine Bewertungen
- CH22Dokument25 SeitenCH22Farah FarahNoch keine Bewertungen
- Marine Fitness CourseDokument432 SeitenMarine Fitness CoursesrollinsNoch keine Bewertungen
- Critical CareDokument21 SeitenCritical Carepaulzilicous.artNoch keine Bewertungen
- Students' Guide to PneumoniaDokument15 SeitenStudents' Guide to PneumoniaArgenic BernzNoch keine Bewertungen
- Kundalini Breathing ExerciseDokument2 SeitenKundalini Breathing ExerciseAbdRdr63100% (4)
- How to Breathe Better with Deep Breathing TechniquesDokument1 SeiteHow to Breathe Better with Deep Breathing TechniquesNouka VENoch keine Bewertungen
- The Perfect Answer Biology Revision Guide - Edexcel IGCSE 9-1 - 1st EditionDokument36 SeitenThe Perfect Answer Biology Revision Guide - Edexcel IGCSE 9-1 - 1st EditionKevir Man85% (13)
- Ilovepdf MergedDokument351 SeitenIlovepdf MergedSwara SawantNoch keine Bewertungen
- General Guidelines For Blood Type ODokument5 SeitenGeneral Guidelines For Blood Type OzmajarhNoch keine Bewertungen
- Channeling Your Higher SelfDokument25 SeitenChanneling Your Higher Selfmadhanalive100% (8)
- Cap No GraphyDokument21 SeitenCap No GraphyPrabhakar KumarNoch keine Bewertungen
- Coughing TechniqueDokument18 SeitenCoughing TechniqueSiva ShanmugamNoch keine Bewertungen
- Thinking Trumpet BookDokument37 SeitenThinking Trumpet BookSoy Yo LorenNoch keine Bewertungen