Beruflich Dokumente
Kultur Dokumente
2009-EDTR-015 Ophthalmology As A Career 2009
Hochgeladen von
87mmOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
2009-EDTR-015 Ophthalmology As A Career 2009
Hochgeladen von
87mmCopyright:
Verfügbare Formate
The Royal College of Ophthalmologists
OPHTHALMOLOGY
AS A CAREER
A SHORT GUIDE TO A CAREER IN
OPHTHALMOLOGY
IN THE UK
2009
RCOphth January 2009 Charity No: 299872
What is ophthalmology?
Ophthalmology is a branch of medicine dealing with the
diagnosis, treatment, and prevention of diseases of the eye
and visual system.
Ophthalmology is unique amongst medical specialties. The
eye, its surrounding structures and the visual pathways may
be afected by a great variety of clinical conditions. Their
successful management depends on the ophthalmology
team combining the diagnostic and therapeutic abilities
of a physician and technical skills of a microsurgeon with
an understanding of the whole patient. Ophthalmology
integrates with many other branches of medicine did you
know that the commonest cause of visual impairment under
the age of 65 years is diabetes?
One of the fundamental properties of the eye is that many
of its components are transparent. This enables the details of
its structure and abnormalities to be observed directly, in a
manner not possible for most other parts of the human body.
The retina of a diabetic patient, modern treatment of diabetic retinopathy
has prevented many patients from becoming blind.
Ophthalmologists are applying new discoveries from the
basic sciences to clinical practice. Innovative technologies
for imaging the eye have helped to diagnose and treat
many conditions, and there have been numerous advances
in microsurgical techniques that have improved surgical
outcomes. Novel treatments for degenerative diseases of the
retina give hope to patients with a previously poor prognosis.
These developments make it a very exciting time for the
specialty.
An Optical Coherence Tomography (OCT) scan of the retina allowing a
magnifed view of the layers of the retina and retinal pigment epithelium in
living eyes, this has greatly helped in the diagnosis of retinal disease.
A confocal scanning laser ophthalmoscopy scans the optic nerve head to
produce an image which allows patients with glaucoma to be followed
accurately.
What is an ophthalmologist?
An ophthalmologist is a medically trained doctor who
commonly acts as both physician and surgeon. (S)he
examines, diagnoses and treats diseases and injuries in and
around the eye.
The majority of ophthalmologists are surgical
ophthalmologists. Most of the working week is spent seeing
patients in outpatient clinics with many requiring follow-
up of an ongoing condition. Although patients often have
conditions related to ageing, such as cataract, glaucoma
and macular degeneration, diseases of the eye and its
So you want to be an
Ophthalmologist?
2
RCOphth January 2009 Charity No: 299872
surrounding structures may be part of an underlying systemic
disease, e.g. diabetes. There is therefore, close collaboration
with many other specialists, including diabetologists,
rheumatologists, neurologists, neurosurgeons, ENT and
maxillofacial surgeons, plastic surgeons, paediatricians
and geneticists. Did you know that ophthalmologists also
examine and treat eye conditions in premature babies?
A minority of patients require procedures using diferent
kinds of laser or surgery, usually performed under local
anaesthesia and as a day case. Most ophthalmologists have
two operating sessions per week. The surgical workload of
the general ophthalmologist may include cataract extraction,
squint and glaucoma surgery, oculoplastic and nasolacrimal
surgery. Many consultants now specialise in a particular area
although most also continue to perform cataract surgery. Did
you know that over 300,000 cataract operations per year are
performed under the NHS through small incision (keyhole)
surgery known as phakoemulsifcation, making this the
commonest operation under the NHS and of any type of
surgery undertaken in the world?!
Specialist interests in ophthalmology
Cataract and Refractive Surgery
Corneal and External Diseases
Glaucoma
Medical Ophthalmology
Medical Retina
Neuro-ophthalmology
Ocular Oncology
Oculoplastics
Orbital/lacrimal disorders
Paediatric Ophthalmology
Strabismus
Vitreoretinal surgery
Eye emergencies, of which there are a large number, may
be seen frst by a general casualty ofcer but in larger
departments a separate Eye Casualty department is
stafed by ophthalmologists and/or nurse practitioners.
Patients may present with conditions that include a simple
foreign body on the cornea, chemical burns, angle-closure
glaucoma, blockage to the blood supply to the retina, and
retinal detachment. Even patients with brain tumours may
frst present to an eye casualty department. Consultant
ophthalmologists take part in an on-call rota but night work
is unusual.
Do ophthalmologists work as part of a team?
Apart from ophthalmologists other health professionals play
an important role in the care of ophthalmic patients, and
teamwork is essential to ophthalmic practice.
Hospital Doctors and General Practitioners Patients may
be referred from or to other medical teams for assessment.
Ophthalmologists liaise particularly with neurologists,
rheumatologists, diabetologists and endocrinologists. GPs
will often be the frst port of call for patients with eye disease
and may refer to, or seek advice from, the ophthalmology
unit.
It is Monday afternoon and you are about to perform cataract
surgery on Mrs Bs right eye. She has very dense cataracts
reducing her vision to only counting fngers (in each eye). She
had been struggling to look after her grandchildren during
the day when her children were at work, and could hardly see
to watch television.
Although she managed
to get around at home,
she was scared to go
out on her own. Surgery
is straightforward and
Mrs B goes home a
short while later. The
following morning your secretary gets a phone call from Mrs Bs
daughter who wants to speak to you urgently. She tells you that
her mother is overjoyed, and is in foods of tears because she is
so happy as she can now see her grandchildren clearly for the
frst time in a number of years. All the family wish to thank you
for restoring her sight. For you, there is a real sense of purpose
and achievement.
A
c
a
t
a
r
a
c
t
,
t
h
e
l
e
n
s
i
n
t
h
e
e
y
e
h
a
s
b
e
c
o
m
e
o
p
a
q
u
e
.
3
RCOphth January 2009 Charity No: 299872
Ophthalmic Nurses have training and experience in
ophthalmology, and provide specialist support for eye clinics,
wards and operating theatres. Some also undergo further
training to become nurse practitioners, working in casualty
and assessing patients with routine ophthalmic conditions.
Operating theatre in action
Orthoptists undergo professional training to become expert
in problems of ocular movement, binocular vision and
childrens sight. Dealing with children with squint (where the
eyes are not parallel, e.g. may turn in or out) forms a large part
of their work. They may work as part of the team within the
eye unit itself, or independently as community orthoptists.
Optometrists (aka Opticians) also undergo professional
training. Many practise in the High Street, refracting patients
and prescribing and dispensing spectacles. They perform
screening examinations to detect conditions, such as
diabetes and glaucoma. Some work part-time or full-time
within the Hospital Eye Service, where they provide specialist
services such as the ftting of complex contact lenses and
low vision aids. Increasingly they are assessing patients
with particular eye problems such as glaucoma. They have
limited but increasing rights to prescribe pharmacological
treatments.
Electrophysiologists mainly work in larger hospital eye
departments and provide electrodiagnostic and monitoring
services for patients with suspected or established inherited
retinal diseases or visual pathway disorders.
Visual Function Technicians carry out a large number of
investigations including visual feld testing. They may take
pictures of the eye (together with photographers) using
various techniques, such as digital fundus imaging, B-scan
ultrasound, optical coherence tomography and tomographic
imaging of the optic nerve.
Ocular Prosthetists are responsible for the supply and
ftting of ocular and oculofacial prostheses (artifcial eyes)
when tissue has been lost through trauma or surgery.
Ophthalmic Photographers use sophisticated equipment
to photograph the face, eyelids, outer eye, and retina.
Photographic (including angiogram) and video techniques
are essential in the diagnosis and monitoring of many
ophthalmic disorders. This is becoming an increasingly
important role in an eye unit.
How do I become an ophthalmologist?
Training in Ophthalmology
Training in medicine has undergone signifcant change
following the introduction of Modernising Medical Careers
(MMC). It is likely to continue to change as MMC develops.
This account represents the current training structure.
Examining a patients eye with a slit lamp microscope
4
RCOphth January 2009 Charity No: 299872
Outline of Specialist Training
Following the two foundation years doctors apply for
specialist training; in ophthalmology this normally lasts
7 years, is competence based and leads to a Certifcate
of Completion of Training (CCT). The essential, or core,
requirements are described by a series of nested learning
outcomes. These are derived from a description of what
consultant ophthalmologists, as health care professionals in
the UK, are able to do and how they approach their practice.
During the frst two years the trainee should acquire the
general clinical skills of an ophthalmologist, and have a basic
knowledge of the conditions covered by the specialty. As
well as general and specialist clinics and ophthalmic casualty
work the trainee will attend two theatre sessions per week.
During these sessions he/she should master the commonly
performed procedures, and assist at more complex
operations. Trainees may want to become involved in clinical
research projects.
As trainees become more senior the depth of their
knowledge increases and they learn specialist surgical and
clinical skills according to a curriculum set by the College.
More time is spent in both general and specialist clinics,
with an average of two to three theatre and laser sessions
per week. Regular assessment of trainees progress is
undertaken throughout the training. These include Case-
based Discussions (CbD), Direct Observation of Procedural
Skills (DOPS), Objective Assessment of Surgical and Technical
Skills (OSATS). There is also an annual assessment panel to
ensure that trainees are progressing as expected.
Becoming an Academic Ophthalmologist
A clinical academic training pathway has been established
through the National Institute for Health Research (NIHR) in
the form of Academic Clinical Fellowships (ACF) and Clinical
Lecturerships (CL). ACFs are usually at ST1-3 level and provide
a clinical and academic training environment to prepare an
application for a Training Fellowship leading to a PhD (or
equivalent). CLs are aimed at trainees who are advanced in
their specialty training, have completed a research doctorate
or equivalent and who show outstanding potential for
continuing a career in academic medicine.
Training at the College HSA Skills Centre
Ophthalmic Trainees Group
Trainees are represented by the Ophthalmic Trainees Group
(OTG); members sit on RCOphth committees to represent
trainees views. The group also organises meetings for trainees
and acts as a forum to allow discussion of common problems
that arise during training.
Flexible Training
Trainees unable to work full-time for personal reasons may
undertake an equivalent training programme, but over a
longer period. Local arrangements are made through the
Regional Postgraduate Dean.
5
RCOphth January 2009 Charity No: 299872
FRCOphth Part 1
No previous experience in ophthalmology is necessary for
candidates to sit the Part 1 FRCOphth and the structure is
based on the learning outcomes from the curriculum for the
frst two years of training. This will include basic sciences,
theoretical optics and some pathology.
The examination will consist of two papers including:
120 MCQ questions over 3 hours
OSE examination in booklet format over 2 hours
Topics the examination assesses are:
Anatomy - orbit and adnexae, ocular anatomy, cranial cavity,
CNS, head and neck, cardiovascular system
Physiology general principles, ocular, physiology of vision
Biochemistry and Cell Biology
Pathology general principles, basic ocular pathology,
microbiology, immunology
Growth and senescence
Optics physical and geometric, clinical
Therapeutics
Lasers
Epidemiology and Evidence Based Medicine
Instrument Technology
Biostatistics
Clinical Genetics
Patient Investigations
The Refraction Certifcate
This tests the understanding of clinical refraction, particularly
retinoscopy, focimetry and the prescription of glasses.
All applicants must have passed the FRCOphth Part 1 by the
end of the second year and the Refraction Certifcate by the
end of the third year of training.
FRCOphth Part 2
Written Component
A 2 hour MCQ paper of 90 questions consisting of 1 best
answer out of 4 options;
A 3 hour EMQ paper of 45 questions each consisting of 2
parts, 90 items in total.
Candidates successfully completing the Written Component
will automatically sit the Practical Component of the
examination approximately 10 weeks later.
Practical Component
The frst part of the practical component is a Structured Viva
consisting of 5 stations, each with 2 examiners, of 10 minutes
duration each. Each station will allow assessment of decision-
making, clinical reasoning and judgement.
Station 1: Patient investigations and data interpretation
Station 2: Patient management
Station 3: Health promotion and disease prevention
Station 4: Attitudes, ethics and responsibilities
Station 5: Audit, research and evidence based practice
The next part is a Clinical Examination, each with 2 examiners;
each station will allow assessment of knowledge of basic and
clinical sciences and communication skills as follows:
Station 1: Cataract and anterior segment (15 minutes)
Station 2: Glaucoma and lid (15 minutes)
Station 3: Posterior segment (15 minutes)
Station 4: Strabismus and orbit (15 minutes)
Station 5: Medicine and Neurology (30 minutes)
Station 6: Communication Skills (10 minutes)
Final accreditation is achieved when all the competencies
set down in the curriculum are achieved and normally the
FRCOphth Part 2 must be passed by Year 7 in Ophthalmic
Specialist Training.
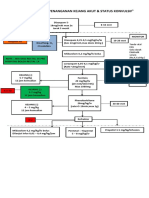
The new examination structure
for a trainee in Ophthalmology
6
RCOphth January 2009 Charity No: 299872
What happens at the end of training?
Consultant Ophthalmologists
The majority of trainees aim to become consultants, for
which the FRCOphth (or equivalent) and CCT are essential.
There are approximately 760 ophthalmic consultant posts
in the UK. Consultants are responsible for all the patients in
their care, and for supervising and training junior doctors.
Posts may be full-time, part-time or job-share. There are many
applicants for each consultant job and the specialty is highly
competitive.
Academic Ophthalmologists
There are many academic departments in ophthalmology
throughout the UK that are stafed by Professors, Senior
Lecturers and Clinical Lecturers. Professors and Senior
Lecturers have honorary consultant contracts and Lecturers
have honorary SpR/StR contracts. Ophthalmologists wishing
to pursue an academic career would normally be required to
undertake a higher degree during their training, and should
seek advice early on clinical training requirements from their
nearest academic ophthalmology department.
Other Career Options
Some doctors may not wish to become consultants or may
be unable to pursue their career to consultant level, but still
want to continue a career in ophthalmology. Fortunately
there are other options available. The doctors in the following
grades are known as Staf and Associate Specialist doctors
(SAS doctors):
Clinical Assistants are doctors who have some basic
training in ophthalmology and usually work in the outpatient
department on a sessional basis. These posts are particularly
suitable for those wanting to work part-time, or to combine
an interest in ophthalmology with a commitment in another
specialty, such as general practice.
For a Staf Grade or Trust Grade post, completion of basic
specialist training is required. The type of work performed is
dependent upon the individuals interests and experience.
Posts may be full-time or part-time and many perform
surgery in addition to outpatient work. Some may provide
on call cover for their department. Some SAS doctors run
departments such as Diabetic Retinal Screening Services.
Under a new contract implemented in 2008 these posts will
be renamed as Specialty Doctor.
An Associate Specialist is a personal appointment made
for an individual with appropriate qualifcations and training
who has generally spent a number of years as a staf grade
ophthalmologist. This is a more senior appointment and
these ophthalmologists commonly have a subspecialty
interest, and many work unsupervised and perform surgery.
The 2008 contract means that no further appointments will
be made to this grade after March 2009.
I am more interested in the medical side than the surgical
side. What can I do?
Medical Ophthalmology
The primary purpose of the specialty is the medical
assessment, investigation, diagnosis and management of
systematic disorders afecting vision, particularly:
Infammatory disorders afecting vision (e.g. uveitis,
scleritis, corneal graft rejection, systemic vasculitis)
Vascular disorders afecting vision (e.g. diabetes,
arteriosclerosis, hypertension, stroke)
Neurological disorders afecting vision (e.g. multiple
sclerosis, stroke, pituitary disorders, thyroid eye disease)
Public visual health (e.g. diabetic retinopathy screening)
Other important aspects include:
Genetic disorders afecting vision (e.g. retinitis
pigmentosa)
Retina specifc disorders afecting vision (e.g. age-related
macular degeneration)
Visual rehabilitation (e.g. age-related macular de-
generation, stroke)
Ophthalmic procedures particularly laser therapy for
diabetic retinopathy and local injection therapy for age-
related macular degeneration
7
RCOphth January 2009 Charity No: 299872
It is predominantly outpatient based. The workload of an
ophthalmic physician is varied ranging from the personal
delivery of care such as laser therapy for diabetic retinopathy
through to the intellectual challenge of neuro-ophthalmic
disorders. As the majority of conditions are responsive to
therapy, it is very rewarding.
Training is under the auspices of The Joint Royal Colleges
of Physicians Training Board (JRCPTB). Like other medical
specialties, trainees frst complete core medical training,
and then enter a four-year competence based medical
ophthalmology curriculum.
For further information visit http://www.jrcptb.org.uk.
The future of ophthalmology
What will a career in ophthalmology be like in fve years or ten
years from now? It is possible to make some guesses based
on the trends of the last fve or ten years and from what can
be predicted about the numbers of people reaching old
age in the years ahead. However, it is much more difcult
to predict the efect of factors such as new treatments and
the efects of future government policy on the way in which
ophthalmology is practised.
We can be sure that the number of people reaching old age
and extreme old age will continue to rise until around 2030
and therefore that the number of people requiring treatment
for cataract, glaucoma, age-related maculopathy and type
2 diabetes will also rise. Efective new treatments for age-
related maculopathy are already having an efect on the way
in which hospital eye departments are organised and stafed.
Twenty years ago, most consultant ophthalmologists
were general ophthalmologists. Now, nearly all consultant
ophthalmologist posts require a subspecialty interest such as
glaucoma or oculoplastics, and in larger eye units, consultants
may work exclusively in one subspecialty of ophthalmology.
This trend looks likely to continue and in the future, it may be
the case that cataract surgery will become a subspecialty in
its own right, with the nations demand for cataract surgery
being served by a smaller number of ophthalmologists
undertaking high-volume operating lists. The number of
ophthalmologists who do not operate at all will probably
increase.
Current health policy in Britain provides an incentive for
more care to be delivered in general practice or community
care settings. Although ophthalmology is still a strongly
hospital-based specialty, this is likely to change, as there is
an increasing demand for primary care ophthalmology to be
delivered in places other than hospitals. This will require a
new type of ophthalmologist with skills in teaching, team-
building and aspects of public health and epidemiology.
Ophthalmology will continue to encompass a rich mixture of
medical, surgical and epidemiological challenges. We can be
fairly sure that it will never be boring.
What can I do as a medical student?
Ophthalmology is a highly competitive specialty. If, as a
medical student, you are seriously considering a career in
ophthalmology, it is worthwhile thinking how you might
enhance your portfolio. You may like to include ophthalmology
in one of your student selected components/special study
modules and your elective period. The Patrick Trevor-Roper
Undergraduate Travel Award www.rcophth.ac.uk is open
to all undergraduate medical students from the UK and Eire
only. There are two awards to be made annually, each for the
sum of 550. This money can be used to fund electives in
ophthalmology and may be spent on travelling or subsistence.
The Duke Elder Undergraduate Prize Examination www.
rcophth.ac.uk takes place once a year in Medical Schools
throughout the country. This is a competitive national EMQ
examination run by The Royal College of Ophthalmologists.
Your medical school may also award an ophthalmology
prize; fnd out from your eye department or medical school
ofce if this is the case. The following medical schools have
awards but this is not an exhaustive list: Barts and the London,
Belfast, Birmingham, Bristol, Edinburgh, Liverpool, Newcastle,
Nottingham, UCL.
8
RCOphth January 2009 Charity No: 299872
Training in ophthalmology: the trainees perspective
Miss Katya Tambe, ASTO in Oculoplastics
The University Hospital of Leicester
I started my medical career in India aspiring to be a hand
surgeon, until I realised I frst had to do general surgery
involving messy abdomens and smelly abscesses!!! I was
a surgeon by heart and the speciality that appealed above
the rest was OPHTHALMOLOGY! I have never regretted my
decision.
I can think of no other speciality that is more interesting,
diverse and rewarding. There are patients that I can treat
medically while others need surgery. Which other speciality
in medicine allows one to look at the pathology specimen
without having to dissect the part out? It is aptly said that the
eye is the window to the body!
The surgical aspect is the most thrilling and varied. One
might ask how much is there to do in an eye? Believe it or
not one has the option to subspecialise in cornea, glaucoma,
medical retina, vitreo-retinal surgery and paediatrics. If you
are into gadgetry and advanced technology look no further
than ophthalmology. There is an ever increasing array of
diagnostic and surgical instruments at your disposal. Id give
a special mention to oculoplastic surgery as that is my sub-
speciality interest encompassing almost every tissue around
the eye and every age group. The orbital work reminds me of
my frst aspiration to work with bones!
Ophthalmology is a great career option for males and
females, for those who wish to have a family life and for those
who want to dedicate their life to medicine. We are one of the
few surgical branches who still have a so-called nine to fve
job (if there ever was one in medicine!). Busy days and a good
nights sleep is the norm. Its a dynamic branch with lots of
opportunity to do research if you are academically inclined.
If anyone is looking for career guidance I would say if you
have a passion for surgery, technology, like attention to
detail, have good manual dexterity, binocular vision and want
to make a diference to a patients life, ophthalmology would
top the charts!
Volunteer work as an ophthalmologist in the
developing world
Jag Gandhi, Specialist Registrar
Manchester Royal Eye Hospital
The highest satisfaction in my time in ophthalmology has
been obtained during those periods when I have been out
to Sub-Saharan African countries as a volunteer cataract
surgeon. As such, I have travelled to countries such as
Namibia, Rwanda, Ghana, Kenya and Zambia. As a very
junior trainee (senior house ofcer) I found two consultant
colleagues who made expeditions to Africa to ofer their
skills in an annual African eye camp. This visit was usually of
one or two weeks duration. I have subsequently continued
to participate in such eye care programmes in Sub-Saharan
Africa in the grade of specialist registrar.
Visual impairment and blindness, as you might expect, is
very commonplace in poor parts of the world. Thus there are
opportunities at all levels of clinical experience to participate
in eye care ventures. The time you decide to invest can vary
considerably, extending anywhere from a fortnight to a two-
year sabbatical. The ophthalmic trainee with a year or two
of experience may wish to practise ophthalmology with
a chiefy medical slant. Surgical work is best left to a stage
where the doctor concerned has learned how to handle
ocular tissues competently and this point especially applies to
intraocular surgery. We must recall that the aim, as always, is
to ofer our patients the best possible care and so appreciate
that operating in the developing world in a modest clinical
environment is a challenge even for experienced surgeons.
More than half of the blindness in the developing world
is secondary to cataract and therefore most visiting
ophthalmologists aim to undertake cataract surgery because
it is a problem with an excellent solution. This is a gratifying
9
RCOphth January 2009 Charity No: 299872
privilege; the ability to literally treat blindness in one person
after another. The epidemiology of visual impairment in the
underdeveloped world is dominated by cataract blindness,
glaucoma and trachoma. Although you enjoy satisfaction
as a clinician when you practise in the developed world,
working in the developing world elevates you to a new (and
previously unconsidered) plane of personal satisfaction.
Additionally, a whole set of issues regarding medical care
in poor parts of the world present themselves to you with
memorable immediacy and thus give you an entirely new
perspective, both as a person and as a doctor.
In the age of the Internet it is remarkably easy to research
your interest in contributing to eye care in poor parts of the
world. There are a myriad of non-governmental organisations
(NGOs) to be found that welcome volunteer ophthalmic
doctors. Examples are Unite For Sight, an efective American
organisation founded by a medical student, which values
the support of volunteers at diferent stages of professional
development, from medical student to senior consultant.
Similarly, another charitable body is Surgical Eye Expeditions
(SEE) International, whose eye camps are mainly undertaken
by doctors in the registrar and consultant grades. By working
with a well-established NGO your trip is better organised and
therefore more useful all round, not least because you are
supported by a host ophthalmologist throughout.
Finding out more
If you are already at medical school talk to members of
the local eye department, seek the perspective of both
junior and senior members of the team. Find out what
opportunities there are locally to gain practical experience in
ophthalmology as a medical student. Have you considered
doing an ophthalmic elective in this country or abroad?
The Royal College of Ophthalmologists (RCOphth), previously
part of the Royal College of Surgeons of England, is a young
and enthusiastic college; it has just celebrated its frst 20 years
as an independent college. Look at the rest of the website
to see what is currently happening in the ophthalmic world.
Additional documents
The College will supply additional information about curricula
of training, examinations, training of overseas doctors and
other topics on request.
Useful contacts
Your local Department of Ophthalmology
Your Regional Postgraduate Dean
The Royal College of Ophthalmologists
17 Cornwall Terrace
London, NW1 4QW
Tel No: 020 7935 0702
Fax No: 020 7935 9838
e-mail: training@rcophth.ac.uk
web site: www.rcophth.ac.uk
The British Medical Association
Medical Career and Information Service
BMA House
Tavistock Square
London, WC1H 9JP
Tel No: 020 7387 4499
Fax No: 020 7383 6403
Website: www.bma.org.uk
The General Medical Council
178 - 202 Great Portland Street
London, W1N 6JE
Tel No: 020 7580 7642
Fax No: 020 7436 1383
Website: www.gmc-uk.org
10
Das könnte Ihnen auch gefallen
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- CCO Myeloma Nursing TU13 SlidesDokument47 SeitenCCO Myeloma Nursing TU13 SlidesLaura TololoiNoch keine Bewertungen
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- CvadDokument11 SeitenCvadNjideka A.Noch keine Bewertungen
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (894)
- A Mathematical Model For Analysis of The Cell Cycle in Human TumoursDokument24 SeitenA Mathematical Model For Analysis of The Cell Cycle in Human TumoursObetz ClNoch keine Bewertungen
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Obat LASA Apotek UII Farma Analgesic Kardivaskular AntibiotikDokument4 SeitenObat LASA Apotek UII Farma Analgesic Kardivaskular AntibiotikDina Nur UpizahNoch keine Bewertungen
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- Pancreas functions in digestion and glucose metabolismDokument4 SeitenPancreas functions in digestion and glucose metabolismClayton VerBerkmösNoch keine Bewertungen
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- Algoritma Penanganan Kejang AkutDokument1 SeiteAlgoritma Penanganan Kejang AkutEwa ClaudiaNoch keine Bewertungen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Bhs Inggris ElsaDokument11 SeitenBhs Inggris ElsaElsa karuniatiNoch keine Bewertungen
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Practical Living With FibromyalgiaDokument62 SeitenPractical Living With FibromyalgiaMaurice ClarkeNoch keine Bewertungen
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Nucleus DropDokument1 SeiteNucleus DropYovinus DenyNoch keine Bewertungen
- Diabetes BrochureDokument3 SeitenDiabetes Brochureapi-348372254Noch keine Bewertungen
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Malocclusion (2nd Concept Map)Dokument4 SeitenMalocclusion (2nd Concept Map)Stephanie Joy EscalaNoch keine Bewertungen
- Blood Donation Application FormDokument2 SeitenBlood Donation Application FormFadjar MulyaNoch keine Bewertungen
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Working in The Heat & Cold in AlbertaDokument96 SeitenWorking in The Heat & Cold in Albertacanadiangrizzer1100% (1)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- IONTOPHORESISDokument10 SeitenIONTOPHORESISAashishRanjanNoch keine Bewertungen
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- Salient Features of Water ActDokument4 SeitenSalient Features of Water Actparth sarthi100% (2)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Ezetimibe + SimvastatinDokument13 SeitenEzetimibe + SimvastatinDavid Raju GollapudiNoch keine Bewertungen
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Cyber PhysiologyDokument16 SeitenCyber PhysiologyOVVCMOULINoch keine Bewertungen
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- Nursing Care Plan - UtiDokument2 SeitenNursing Care Plan - Utisweet_karisma05100% (6)
- Charlie Castro's CV: 35-year-old Filipino RN Seeks New OpportunitiesDokument13 SeitenCharlie Castro's CV: 35-year-old Filipino RN Seeks New OpportunitiesJasonV.PanayNoch keine Bewertungen
- FAA Pilot Mental Health Final Report - 07.12.2023Dokument27 SeitenFAA Pilot Mental Health Final Report - 07.12.2023Gonzalo Alexis GodoyNoch keine Bewertungen
- Kaishore Guggulu For Pitta and Vaat100% Working Aggressive Nature Skin Problem Vaat PittaDokument5 SeitenKaishore Guggulu For Pitta and Vaat100% Working Aggressive Nature Skin Problem Vaat PittadineshgomberNoch keine Bewertungen
- Questions G 2Dokument8 SeitenQuestions G 2Nader Smadi100% (1)
- DR Nur Farhanah SPPD - Penggunaan AB Rasional 1 PDFDokument16 SeitenDR Nur Farhanah SPPD - Penggunaan AB Rasional 1 PDFFlorantia Setya NugrohoNoch keine Bewertungen
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Meningitis (Completed)Dokument26 SeitenMeningitis (Completed)seema83% (6)
- Fundnursetaylil ADokument32 SeitenFundnursetaylil AChristine N Mike MitchellNoch keine Bewertungen
- ANOVA Analysis of Sales Closing MethodsDokument5 SeitenANOVA Analysis of Sales Closing MethodsShrivats SinghNoch keine Bewertungen
- Estimating Vitamin C in Food & DrinksDokument30 SeitenEstimating Vitamin C in Food & Drinksdan jose skNoch keine Bewertungen
- Monografi Obat WHODokument84 SeitenMonografi Obat WHOade_boy2imutNoch keine Bewertungen
- Nri2022 8336561Dokument14 SeitenNri2022 8336561Carolina SidabutarNoch keine Bewertungen
- Brain Wave Vibration PDFDokument26 SeitenBrain Wave Vibration PDFnikanor1100% (4)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)