Beruflich Dokumente
Kultur Dokumente
Leukore Pada Kehamilan - Evaluation of Vaginal Complaints During Pregnancy The Approach To Diagnosis
Hochgeladen von
Yan Agus AchtiarOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Leukore Pada Kehamilan - Evaluation of Vaginal Complaints During Pregnancy The Approach To Diagnosis
Hochgeladen von
Yan Agus AchtiarCopyright:
Verfügbare Formate
PREGNANCY DERMATOSES AND FETAL EXPOSURE (A INGBER AND Y RAMOT, SECTION EDITORS)
Evaluation of Vaginal Complaints During Pregnancy:
the Approach to Diagnosis
Orna Reichman & Michael Gal & Vera Leibovici &
Arnon Samueloff
Published online: 29 June 2014
#Springer Science+Business Media New York 2014
Abstract Vaginal discharge during pregnancy is commonly
accompanied by pruritus, malodor, dysuria, or dyspareunia.
Almost half of pregnant women are estimated to present with
such symptoms. Differential diagnosis is diverse and includes
entities that are specific to pregnancy, some of which may pose
a hazard to maternal and fetal outcomes. Accurate diagnosis is
essential and requires a detailed medical history combined with
a thorough genital examination, measurement of vaginal pH,
and a microscopic evaluation of vaginal secretions (wet
mount). This review will present the approach to diagnosing
vaginal complaints during pregnancy, together with the criteria
and techniques for diagnosing each of the etiologies.
Keywords Vaginal discharge
.
Pregnancy
.
Wet mount
.
Vaginitis
Introduction
Symptoms of vaginal discomfort, including a nonwhite color
discharge, pruritus, malodor, and dyspareunia, are common
during pregnancy. The recently published findings of a
population-based survey conducted in Brazil revealed patho-
logical discharge in 43 % of pregnant women [1]. However,
the symptoms of such condition are nonspecific and shared by
various etiologies. Further, medical history alone does not
provide a sufficient basis for diagnosis [2, 3, 4]. Most causes
of vaginal complaints can be diagnosed by combining medical
history with a thorough genital examination, measurements of
vaginal pH, and wet mount (microscopy of vaginal secretion)
[5, 6]. Cultures and molecular biology assays, based on
nucleic acid amplification tests (NAATs), such as polymerase
chain reaction (PCR), can help diagnose specific pathogens.
The physiological changes during pregnancy, including
anatomical and hormonal adaptation, aggravate normal
leucorrhea [7]. The cervix contains a collagen-rich connective
tissue with an inner monolayer of columnar cells (endocervix
endocervical glands) that changes dramatically during preg-
nancy. Proliferation and rearrangement of the cervix is strik-
ing, and by the end of pregnancy, the endocervical glands
occupy approximately half the mass of the cervix. This en-
largement causes eversion of the columnar endocervical
glands, known as cervical ectropion. The cervical ectropion
tissue tends to bruise easily; gentle touch (e.g., coitus, PAP
smear, cervical sampling) tends to cause bleeding. Further-
more, the endocervical mucus glands produce a copious
amount of tenacious mucus that contains immunoglobulins
and cytokines and serves as an immune barrier to protect the
pregnancy from ascending infection, as well as a mechanical
obstruction of the cervical canal [7].
In addition to the physiological changes during pregnancy
that aggravate vaginal complaints, the differential diagnosis of
pathological conditions includes entities that are unique to
pregnancy, such as the premature rupture of membranes and
chorioamnionitis, which could both present with vaginal dis-
charge as a primary symptom [7]. These conditions may pose
hazards to maternal and fetal outcomes, including maternal
O. Reichman
:
M. Gal
:
A. Samueloff
OBGYN, Shaare Zedek Medical Center, Hebrew University,
Jerusalem, Israel
M. Gal
e-mail: galm@szmc.org.il
A. Samueloff
e-mail: smuelof@cc.huji.ac.il
V. Leibovici
Hadassah Medical School, Hebrew University, Jerusalem, Israel
e-mail: Rveralibo@hadassah.org.il
O. Reichman (*)
DivisionOBGYN, Shaare Zedek Medical Center, Hebrew
University Medical School, Jerusalem, Israel
e-mail: orna.reich@gmail.com
Curr Derm Rep (2014) 3:159164
DOI 10.1007/s13671-014-0083-0
160 Curr Derm Rep (2014) 3:159164
and fetal morbidity and mortality. Therefore, accurate diagno-
sis of vaginal symptoms during pregnancy is vital.
This review will present the approach to diagnosing vagi-
nal complaints during pregnancy. Criteria and techniques for
diagnosing each of the etiologies will be detailed.
The Approach to Diagnosing Vaginal Complaints
During Pregnancy
Confirm That Symptoms Actually Originate from the Vagina
Fromour experience, most women do not distinguish between
the vulva and vagina and refer to the genital area as one entity.
Proper evaluation of vaginal complaints necessitates a thor-
ough genital examination to verify with the patient the
location of symptoms and to confirm that the discomfort
originates or at least involves the vagina. If the discomfort is
isolated to close anatomical areas, such as the vulva, vestibule,
or perineum, a different differential diagnosis should be pur-
sued. It is advisable during examination to touch gently with a
cotton-tipped applicator the various anatomical genital struc-
tures, including the labia major, labia minor, inter-labial sulci,
perineum, perianal area, vestibule, and clitoris, and only then
to evaluate the vagina. This will help focus the location of the
problem and narrow the differential diagnosis.
Performing a Speculum Examination to Evaluate the Cervix
and Vagina
Check if there is watery discharge secreted from the cervix. A
clear or greenish color indicates meconium and suggests pre-
mature rupture of the membranes. Observe the cervix and
verify if there is an active ectropion. Make sure there is no
abnormal lesion suspicious of cervical carcinoma and that the
PAP smear is normal. Cervicitis is defined by either (1)
purulent or mucopurulent endocervical exudate, visible in
the endocervical canal or by an endocervical swab specimen
and (2) endocervical bleeding caused by gentle passage of a
cotton swab through the cervical os [8]. If cervicitis is
diagnosed, perform a screening test for sexually transmitted
diseases (STDs), focused on Neisseria gonorrhea, Chlamydia
trachomatis, and Trichomonas vaginalis [8]. Of the various
sexually transmitted diseases, these three have the potential to
Fig. 1 pH more than and less than 4.5. a *Trichomonas vaginalis has a
wide clinical presentation; some patients present with acute vaginitis and
complain of dyspareunia; malodorous, purulent discharge and itch; the
others (up to 50 %) are asymptomatic. #Gonorrhea and Chlamydia
chlamydia is usually asymptomatic, both can cause cervicitis, diagnosis is
with NAATs (nucleic acid amplification tests). +Chorioamnionitisthe
level of vaginal pH in pregnant women with chorioaminionitis is not
reported in the English literature. **Maternal/fetal sepsis,
chorioamnionitissee criteria for diagnosis in Table 1. b *Yeast
infection has a wide clinical presentation. Symptoms can include
discharge only or a combination of discharge itch and dyspareunia.
Some women are asympt omat i c. **Mat ernal / f et al sepsi s,
chorioamnionitissee criteria for diagnosis in Table 1
Fig. 2 Epithelial cells are shown
by the black arrows. In 2a, 2b,
and 2c the cells are squamous
cells (matured epithelial cells)
with enlarged cytoplasm and a
small nuclei in contrast to
inflammatory conditions (2d) that
the cells are immature (parabasal,
intermediate cells) and have an
enlarged nuclei compared to the
cytoplasm with excess in
inflammatory cells (dashed
arrow). Clue cells are epithelial
cells with abnormal flora adhered
to the borders of the cell. They are
the hallmark of bacterial
vaginosis (2c dashed arrow). The
flora is shown by the wide white
arrow. Normal morphology of
rods is present in picture 2a and
abnormal morphology of cocci
(characteristic of BV) is present in
2c
Curr Derm Rep (2014) 3:159164 161
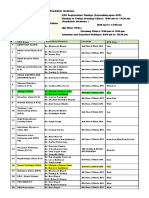
Table 1 Etiologies that cause vaginal symptoms during pregnancy and their diagnostic criteria
Etiology Diagnostic criteria
Pregnancy specific Premature rupture
of membranes
1. Clinical diagnosisper speculum visualization of amniotic fluid originating from the uterus.
2. Nitrazine test [10] (amniotic fluid pH>7)inexpensive, nonspecific
3. Presence of arborization (ferning), a characteristic of dried amniotic fluid on a slide
4. Placental alpha microglobulin-1 (AmniSure [11])not affected by semen or blood, expensive
5. Insulin-like growth factor binding protein 1 (Actim Prom [12])not affected by semen,
blood, or urine
6. Fetal fibronectin [13]a negative result excludes membrane rupture
7. Oligohydramnios/anhydramnios, combined with an appropriate medical history
8. Equivocal casesinject indigo carmine to amniotic fluid while a tampon is inserted in the
vagina
Chorioamnionitis Clinical chorioamnionitis: maternal fever 38 C and at least two of the following
(after excluding other causes of sepsis) [14]:
1. Maternal tachycardia (<100 beats/min(
2. Maternal leukocytosis (>15,000 cells/mm(
3. Fetal tachycardia (>160 beats/min)
4. Uterine tenderness
5. Foul odor of the amniotic fluid
The level of vaginal pH in pregnant women with chorioaminionitis is not reported in the English
literature.
Microbiological chorioamnionitis [15] when clinical presentation is equivocal and diagnosis is
crucial.
Perform amniocentesis
1. Culture for bacteria
2. Perform a gram stain, search for presence of leukocyte esterase, check glucose concentration,
and verify levels of white blood cells
Cervical mucus plug Clinical diagnosisdetachment of the cervical mucus plug bloody show, commonly followed
by labor, can appear after a digital vaginal examination [8]
Vaginal bleeding antenatal
bleeding (abruption)
Clinical diagnosisper speculum visualization of blood originating from the uterus
Infectious diseases Yeast most common
Candida Albicans
1. Presence of Candida on wet mount or Grams [16, 17]
2. Positive yeast culture [16, 17]
Vaginal pH is in the normal range
Trichomonas vaginalis 1. Presence of motile trichomonas on wet mount
2. Elevated vaginal pH (>4.5)
3. Commercially available nucleic acid amplification test (NAAT) [8]gold standard
4. Rapid antigen test immunochromatography (OSOM Trichomonas Rapid Test (Genzyme))
5. Culture on Diamonds mediumpreviously the gold standard, takes 7 days, less commonly
used at present
Bacterial vaginosis Amsels criteria [18], at least three of the following:
1. Pasty discharge
2. Positive whiff test a drop of KOH to vaginal discharge will worsen malodor
3. Positive clue cells on wet mount
4. Elevated pH
Nugent score [19]the score is determined by the average number of one of three morphotypes
of bacteria
03 normal, 46 intermediate, 710 bacterial vaginosis
1. Lactobacillus (04)
2. Gardnerella and Bacteroides (04)
3. Curved gram variable rods (02)
Neisseria gonorrhea,
Chlamydia trachomatis
Clinically could present as cervicitis but most patients with C. trachomatis are asymptomatic.
Diagnosis is based on commercially available nucleic acid amplification test (NAAT) [8]
Group A Streptococcus Positive vaginal culture
Immune induced Erosive lichen planus (ELP) Primarily a clinical diagnosis. A biopsy may be obtained to support the clinical diagnosis.
Sometimes immunofluorescence helps to diagnose [20]
Desquamative inflammatory
vaginitis (DIV)
Clinical syndrome of purulent vaginitis, diagnosis is based on the exclusion of causes of
purulent vaginitis [21]
Hormonal/
physiological
conditions
Normal leucorrhea
Cervical ectropion
162 Curr Derm Rep (2014) 3:159164
cause cervicitis or vaginitis and can present with vaginal
symptoms as the chief complaint. The gold standard screening
for these infections is by NAATs, including PCR and ligase
chain reactions that are performed by sampling the cervix/
vagina with one of the currently available commercial appli-
cators. Other STDs that involve the genital area, such as
syphilis (Treponema pallidum), genital warts (human papillo-
ma virus), and genital herpes rarely involve the vagina alone;
the lesion and discomfort primarily involve the vulva, perine-
um, perianal area, and the vestibule. It is important to realize
that if screening is positive for one of the STDs, screening for
all other STDs is necessary, including those that do not cause
vaginal symptoms. After evaluation of the cervix, the vaginal
walls should be examined for redness, petechiae, and erosions.
The appearance of discharge detected visually with bare eyes
is nonspecific and should not lead to diagnosis [2, 3].
Measuring pH of the Vaginal Walls
Vaginal pH reflects the hormonal and bacterial status of the
vagina and is an excellent screening tool for evaluating vaginal
health (Fig. 1a, b). The vaginal epithelium, a dynamic strati-
fied squamous tissue that undergoes maturation in response to
estrogen, is characterized by three cell types, all originating
from the basal layer: the parabasal cells, the intermediate cells
(which are enriched with glycogen), and the squamous cells.
This multiple layer serves to protect the tissue from friction
injury [9]. Vaginal microbiota is in a delicate equilibrium with
hormones. The enriched glycogen in the intermediate cells
acts as a precursor of pyruvate and facilitates the growth of
the hydrogen peroxide producing Lactobacilli, which ferment
pyruvate to lactic acid and induce an acidic pH of 4.00.5.
The acidic environment inhibits growth of anaerobic bacteria
[9]. Normal vaginal pH indicates (1) adequate levels of estro-
gen, (2) a multilayer epithelium (the presence of at least
intermediate cells with glycogen), and (3) healthy microbiota
with predominant hydrogen peroxide producing Lactobacilli.
A normal pH 4.5 likely rules out premature rupture of mem-
branes, bacterial vaginosis, T. vaginalis, and inflammatory
conditions such as desquamative inflammatory vaginitis
(DIV) and erosive lichen planus (ELP).
To measure vaginal pH, obtain, with a cotton-tipped
applicator, a sample from the mid lateral vaginal wall
and measure the pH with a narrow-range paper 4.07.0.
This is a simple, quick, and inexpensive test. Most
importantly, it narrows the differential diagnosis. It is
important to realize that elevated pH can result from
nonpathological conditions such as post antibiotic treat-
ment and douchi ng ( t r ans i ent er adi cat i on of
Lactobacilli), post coitus (sperm elevates pH), and mu-
cus discharge originating from the cervix. In such cases,
a microscope examination of vaginal secretions (wet
mount) is necessary.
Performing a Wet Mount (Microscopy of Vaginal Secretions)
A health care provider with adequate training in microscopy
of vaginal secretions is capable of defining the maturation
status of vaginal epithelium, describing the morphology of
vaginal flora, and detecting excess inflammatory cells and
pathogens including yeast and Trichomonas [6]. Wet mount
is especially important in cases of elevated vaginal pH
(Fig. 1a), to distinguish between true pathologies and false-
positive screening. The latter includes post antibiotic treat-
ment, post douching, and post coitus. To prepare a wet mount,
obtain, with a cotton-tipped applicator, a sample from the mid
lateral vaginal wall and spread on two separate microscopic
slides. Drip on one sample a drop of 0.9 % saline and on the
other a drop of 10 % potassium hydrochloride (KOH). Apply
a cover slide on each drop. Observe with a microscope,
initially magnified 100 and subsequently magnified 400.
Figure 2 depicts a wet mount of four common conditions: (2a)
normal wet mount, (2b) yeast infection, the lined arrows
indicate hyphae and budding yeast, (2c) bacterial vaginosis
(BV), and (2d) inflammatory vaginitis (Fig. 2).
Diagnostic Criteria for Etiologies Causing Vaginal
Symptoms During Pregnancy
The various etiologies causing vaginal symptoms during preg-
nancy and their diagnostic criteria are presented in Table 1.
Table 1 (continued)
Etiology Diagnostic criteria
Contact dermatitis Various creams and lubrications Suggestive exposure based on history. Confirm diagnosis by an allergy test
Allergy to latex (condoms)
Allergy to sperm
Miscellaneous Trauma, post coitus, foreign
body, douching, urine
incontinence
Suggestive, based on history
Curr Derm Rep (2014) 3:159164 163
Conclusions
Accurate diagnosis of vaginal discharge during pregnancy is
important. Though the differential diagnosis is diverse, the
tools required are accessible and uncomplicated. While the
symptoms are nonspecific, the term nonspecific vaginitis
can be avoided as Gardner wrote, over 30 years ago [22]
any knowledgeable physician owning a vaginal speculumand
a microscope should rarely find the need for using the diag-
nosis non specific vaginitis, and that its frequent use might
well imply carelessness, indifference or a failure to employ
available diagnostic methods
Compliance with Ethics Guidelines
Conflict of Interest O Reichman, M Gal, V Leibovici, and A
Samueloff declare no conflicts of interest.
Human and Animal Rights and Informed Consent This article does
not contain any studies with human or animal subjects performed by any
of the authors.
References
Papers of particular interest, published recently, have been
highlighted as:
Of major importance
1. Fonseca TM, Cesar JA, Mendoza-Sassi RA, Schmidt EB.
Pathological vaginal discharge among pregnant women: pattern
of occurrence and association in a population-based survey.
Obstet Gynecol Int. 2013;2013:590416.
2. Diseases characterized by vaginal discomfort. Sexual transmitted
disease treatment guidelines, 2010 http://www.cdc.gov/std/
treatment/2010/vaginal-discharge.htm (last entered May 6 2014).
3. Anderson MR, Klink K, Cohrssen A. Evaluation of vaginal com-
plaints. JAMA. 2004;291(11):136879. A mile stone paper inte-
grating 18 publications calculating the sensitivity, specificity and
likelihood ratio of symptoms and signs for evaluating vaginal
complaints.
4. Trichomoniasis and bacterial vaginosis in pregnancy: inadequately
managed with the syndromic approach. Bulletin of the World
Health Organization http://www.who.int/bulletin/volumes (last
entered May 6 2014).
5. The vulva and vagina manual, Dennerstein G, Scurry J, Brenan J,
Allen D, Grazia M. M, Gynederm Publishing 2005.
6. Kottmel A, Petersen EE. Vaginal wet mount. J Sex Med.
2013;10(11):26169.
7. Williams Obstetric 23rd edition 2010 p.109, 1168.
8. Workowski KA, Berman S. Centers for Disease Control and
Prevention (CDC), Sexually transmitted diseases treatment guide-
lines, 2010. MMWR Recomm Rep. 2010;59(RR-12):1110. This
is the gold standard for diagnosing and treating sexual transmitted
diseases.
9. Buchanan DL, Kurita T, Taylor JA, Lubahn DB, Cunha GR, Cooke
PS. Role of stromal and epithelial estrogen receptors in vaginal
epithelial proliferation, stratification and cornification.
Endocrinology. 1998;139:434552.
10. Seeds AE, Hellegers AU. Acid-base determinations in human
amniotic fluid throughout pregnancy. Am J Obstet Gynecol.
1968;101(2):257.
11. Lee SE, Park JS, Norwitz ER, Kim KW, Park HS, Jun JK.
Measurement of placental alpha-microglobulin-1 in cervicovaginal
discharge to diagnose rupture of membranes. Obstet Gynecol.
2007;109(3):634.
12. Darj E, Lyrens S. Insulin-like growth factor binding protein-1, a
quick way to detect amniotic fluid. Acta Obstet Gynecol Scand.
1998;77(3):295.
13. Eriksen NL, Parisi VM, Daoust S, Flamm B, Garite TJ, Cox SM.
Fetal fibronectin: a method for detecting the presence of amniotic
fluid. Obstet Gynecol. 1992;80(3 Pt 1):4514.
14. Newton ER. Chorioamnionitis and intraamniotic infection. Clin
Obstet Gynecol. 1993;36(4):795.
15. Gauthier DW, Meyer WJ. Comparison of gram stain, leukocyte
esterase activity, and amniotic fluid glucose concentration in
predicting amniotic fluid culture results in preterm premature rup-
ture of membranes. Am J Obstet Gynecol. 1992;167(4 Pt 1):1092.
16. Mandell: Mandell, Douglas, and Bennett's Principles and Practice
of Infectious Diseases, 7
th
ed. 2009 churchil Livingston.
17. Centers for disease control and prevention: diagnosing and testing
for genital vulvo-vaginal candidiasis http://www.cdc.gov/fungal/
diseases/candidiasis/genital/diagnosis.html (last entered MAY 6)
18. Amsel R, Totten PA, Spiegel CA, Chen KS, Eschenbach DA,
Holmes KK. Nonspecific vaginitis: diagnostic criteria and micro-
bial and epidemiologic associations. Am J Med. 1983;74:1422.
This is the classic paper for the clinical criteria of diagnosing
bacterial vaginosis.
19. Nugent RP. J Clin Microbiol. 1991;29:291.
20. Helander SD, Rogers RS. The sensitivity and specificity of direct
immunofluorescence testing in disorders of mucous membranes. J
Am Acad Dermatol. 1994;30(1):65.
21. Sobel JD, Reichman O, Misra D, Yoo W. Prognosis and treatment
of desquamative inflammatory vaginitis. Obstet Gynecol.
2011;117(4):8505.
22. Gardner HL. Non specific vaginitis: a non-entity. Scand J Infec
Dis Suppl. 1983;40:710.
164 Curr Derm Rep (2014) 3:159164
Das könnte Ihnen auch gefallen
- Writing Committee:: Guidelines For All Doctors in The Diagnosis and Management of Migraine and Tension-Type Headache 2004Dokument53 SeitenWriting Committee:: Guidelines For All Doctors in The Diagnosis and Management of Migraine and Tension-Type Headache 2004Yan Agus AchtiarNoch keine Bewertungen
- Dapus 2Dokument4 SeitenDapus 2Yan Agus AchtiarNoch keine Bewertungen
- Interpreting Chest X-Rays: Illustrated With 100 CasesDokument5 SeitenInterpreting Chest X-Rays: Illustrated With 100 CasesYan Agus AchtiarNoch keine Bewertungen
- Midland College Syllabus Fall 2008 RSPT 1307 Cardiopulmonary Anatomy and Physiology (3-0-0) Course DescriptionDokument6 SeitenMidland College Syllabus Fall 2008 RSPT 1307 Cardiopulmonary Anatomy and Physiology (3-0-0) Course DescriptionYan Agus AchtiarNoch keine Bewertungen
- Dapus 3Dokument10 SeitenDapus 3Yan Agus AchtiarNoch keine Bewertungen
- Jurnal Yan Agus FK UjDokument5 SeitenJurnal Yan Agus FK UjYan Agus AchtiarNoch keine Bewertungen
- Kedokteran 092010101002 Bambang PrabawigunaDokument6 SeitenKedokteran 092010101002 Bambang PrabawigunaYan Agus AchtiarNoch keine Bewertungen
- List Game Goman PC GamesDokument321 SeitenList Game Goman PC GamesYan Agus AchtiarNoch keine Bewertungen
- Abnormal Labor-ModifiedDokument8 SeitenAbnormal Labor-ModifiedListya NormalitaNoch keine Bewertungen
- Gyeke Et Al Paper 1 Vol 17 4Dokument18 SeitenGyeke Et Al Paper 1 Vol 17 4Yan Agus AchtiarNoch keine Bewertungen
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5795)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1091)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- DH VSCC Intern Manual 4th Edition - WEB PDFDokument124 SeitenDH VSCC Intern Manual 4th Edition - WEB PDFXyzNoch keine Bewertungen
- GQ USA - March 2023Dokument120 SeitenGQ USA - March 2023davidtorrez1988Noch keine Bewertungen
- Neuroimaging Advances in Holoprosencephaly: Re Ning The Spectrum of The Midline MalformationDokument13 SeitenNeuroimaging Advances in Holoprosencephaly: Re Ning The Spectrum of The Midline Malformationfamiliesforhope100% (1)
- Intensive Care Unit (ICU)Dokument36 SeitenIntensive Care Unit (ICU)ruind99hjhkj100% (1)
- ACLSDokument275 SeitenACLSShajahan SideequeNoch keine Bewertungen
- Vasospasm: Endothelial Cell InjuryDokument4 SeitenVasospasm: Endothelial Cell InjuryPuja ArgaNoch keine Bewertungen
- Nutrition and AIDSDokument250 SeitenNutrition and AIDSLies Pramana SariNoch keine Bewertungen
- CAREGIVING NC II Lecture Week 6and 7Dokument15 SeitenCAREGIVING NC II Lecture Week 6and 7Ivy MagdayNoch keine Bewertungen
- Kanukula 2019Dokument7 SeitenKanukula 2019Dianne GalangNoch keine Bewertungen
- Sarcoidosis y UveitisDokument10 SeitenSarcoidosis y UveitisJavier Infantes MolinaNoch keine Bewertungen
- Preeclampsia and EclampsiaDokument24 SeitenPreeclampsia and EclampsiaAngel Marie TeNoch keine Bewertungen
- B Arab Board For Community Medicine Examination Edited 6 1Dokument115 SeitenB Arab Board For Community Medicine Examination Edited 6 1Sarah Ali100% (2)
- Bimanual Vaginal Examination - OSCE Guide - Geeky MedicsDokument6 SeitenBimanual Vaginal Examination - OSCE Guide - Geeky MedicsJahangir AlamNoch keine Bewertungen
- Correction of Severe Bimaxillary ProtrusionDokument37 SeitenCorrection of Severe Bimaxillary ProtrusionRobbyRamadhonieNoch keine Bewertungen
- NearfatalasthmaDokument8 SeitenNearfatalasthmaHeath HensleyNoch keine Bewertungen
- Pengaruh Pemberian Ropivakain Infiltrasi Terhadap Tampilan Kolagen Di Sekitar Luka Insisi Pada Tikus WistarDokument10 SeitenPengaruh Pemberian Ropivakain Infiltrasi Terhadap Tampilan Kolagen Di Sekitar Luka Insisi Pada Tikus WistarKunni MardhiyahNoch keine Bewertungen
- ThyrotoxicosisDokument16 SeitenThyrotoxicosisFiorella Peña MoraNoch keine Bewertungen
- 5.respiratory Distress Dental LectureDokument40 Seiten5.respiratory Distress Dental LecturehaneeneeNoch keine Bewertungen
- Case Study #3 Renal 1. LabDokument9 SeitenCase Study #3 Renal 1. Labapi-207971474Noch keine Bewertungen
- Blood Donation RequirementsDokument29 SeitenBlood Donation RequirementsMaria Cecilia FloresNoch keine Bewertungen
- Seattle Angina QuestionnaireDokument6 SeitenSeattle Angina QuestionnaireAmelia SianiparNoch keine Bewertungen
- Camh Suicide Prevention HandbookDokument96 SeitenCamh Suicide Prevention Handbook873810skah100% (3)
- OPD Schedule DoctorsDokument3 SeitenOPD Schedule DoctorssahilNoch keine Bewertungen
- b53 Swasa Kosa Mudra 07Dokument3 Seitenb53 Swasa Kosa Mudra 07shadowfalcon03Noch keine Bewertungen
- Assessment Diagnosis Goals and Objectives Planning Intervention Rationale EvaluationDokument3 SeitenAssessment Diagnosis Goals and Objectives Planning Intervention Rationale EvaluationCrissa AngelNoch keine Bewertungen
- English Drama ScriptDokument7 SeitenEnglish Drama ScriptNadia ASNoch keine Bewertungen
- Appenndix C CompleteDokument2 SeitenAppenndix C Completebrooksey2Noch keine Bewertungen
- Burns and ScaldsDokument14 SeitenBurns and ScaldsMuhamad IqbalNoch keine Bewertungen
- Manual Lifegain INGLESDokument207 SeitenManual Lifegain INGLESNicolás Di LulloNoch keine Bewertungen
- Symptoms: Products & ServicesDokument20 SeitenSymptoms: Products & ServicesLany T. CataminNoch keine Bewertungen