Beruflich Dokumente
Kultur Dokumente
Cardiovascular Review
Hochgeladen von
sparticuslives0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
29 Ansichten8 SeitenCardio 4
Copyright
© © All Rights Reserved
Verfügbare Formate
DOCX, PDF, TXT oder online auf Scribd lesen
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCardio 4
Copyright:
© All Rights Reserved
Verfügbare Formate
Als DOCX, PDF, TXT herunterladen oder online auf Scribd lesen
0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
29 Ansichten8 SeitenCardiovascular Review
Hochgeladen von
sparticuslivesCardio 4
Copyright:
© All Rights Reserved
Verfügbare Formate
Als DOCX, PDF, TXT herunterladen oder online auf Scribd lesen
Sie sind auf Seite 1von 8
Page 1 of 8
Ms. April Anne D. Balanon GreywolfRed
PRELIMS
The Respiratory and Cardiovascular System
HANDOUT 1 OXYGENATION:
A. 4Anatomy of the Cardiovascular System
1. Heart
hollow, muscular organ that lies in the mediastinum
rests on the diaphragm
a. Pericardium
- encases the heart.
- thin membranous sac containing 20-30 ml serous fluid
- protects the heart from trauma and friction
b. Heart Wall
- Epicardium: thin serous outer layer
- Myocardium: thick muscular middle layer
- Endocardium: smooth inner layer in contact with blood
c. Heart Chambers (separated by a membranous muscular septum)
- Right Atrium
low-pressure
receives systemic venous blood via superior & inferior vena cava
- Right Ventricle
low-pressure
receives blood from RA via tricuspid valve
ejects deoxygenated blood via pulmonic valve to the pulmonary artery
- Left Atrium
low-pressure
receives oxygenated blood from the lungs via four pulmonary veins
- Left Ventricle
high-pressure
receives blood from atrium via mitral valve
Ejects oxygenated blood to the aorta into systemic circulation
d. Heart Valves
- AV (Atrioventricular valves )
Tricuspid Valve between right atrium and ventricle
Mitral valve between the left atrium and ventricle
- Semilunar valves : between ventricles and artery
Pulmonic valve between right ventricle and pulmonary artery
Aortic valve between left ventricle and aorta
- Papillary musles
Muscle bundles on the ventricular walls
Chordae Tendinae: fibrous bands extending from the papillary muscles to the valve cusps
e. Cardiac Conduction System
- propagation of electricall impulses throughout the myocardium (precursor to heart muscle contraction)
Electrical Pathways
SA (Sinoatrial) Node: pacemaker
o initiating rhythmic impulss t 60-100 impulses/minute
AV (Atrioventricular) Node :
o receives impulses from the SA node, relays them to the ventricles
Bundle of His:
o conducts impulses from the AV node (RBB & LBB)
o RBB and LBB terminate in the Purkinje fibers
Purkinje Fibers:
o propagate electrical impulses into the endocardium and myocardium
Electrical Impulse Activity
Phases of the electrocardiogram
Page 2 of 8
Ms. April Anne D. Balanon GreywolfRed
PRELIMS
The Respiratory and Cardiovascular System
HANDOUT 1 OXYGENATION:
Normal Sinus Rhythm
f. Coronary Arteries
- supply the heart with blood
- Right Coronary Artery supplies blood to the right heart wall
- Left Main Coronary Artery supplies blood to the left heart
2. The Vasculature
a. The Circulatory System
- Pulmonary Circulation
low pressure
low resistance
right side of the heart pumps blood into the pulmonary circulation
- Systemic Circulation
high pressure
high resistance
left side of the heart pumps blood into the systemic circulation
b. Blood Vessels
- classified according to size, location and function
1. Arteries
large diameter, thick-walled vessels
carry blood away from the heart
2. Arterioles
small, thick-walled vessels
represent the major part of vascular resistance
resistance vessels serve as "circulatory stopcocks"
control the distribution of blood to various organs.
3. Capillaries
extremely small, extremely thin-walled vessels (one cell thick)
allow exchange of gases, nutrients, and other small molecules between the blood stream and
tissues
in capillary hydrostatic pressure/permeability can lead to edema.
4. Venules
small thin-walled vessels
bring blood back to the heart
highly distensible and contain a large fraction of the blood volume
5. Veins
large diameter thin-walled vessels
bring blood back to heart
Distensible and contain a large fraction of the blood volume.
Page 3 of 8
Ms. April Anne D. Balanon GreywolfRed
PRELIMS
The Respiratory and Cardiovascular System
HANDOUT 1 OXYGENATION:
B. Functions of the Cardiovascular Sytem
1. Heart
a. Cardiac Output
volume of blood ejected by each ventricle in 1 minute (SV x HR)
Stroke Volume : amount of blood ejected by the left ventricle with each heart beat
Heart Rate : number of heartbeats per minute (60-100)
b. Cardiac Cycle
each complete heartbeat
Systole : contraction phase
Diastole : relaxation (filling phase)
Page 4 of 8
Ms. April Anne D. Balanon GreywolfRed
PRELIMS
The Respiratory and Cardiovascular System
HANDOUT 1 OXYGENATION:
c. Heart Sounds
results from vibrations caused by valve closure and ventricular filling
1
st
Sound S1, tricuspid and mitral valve closure
2
nd
Sound S2, aortic and pulmonic valve closure
3
rd
Sound S3, Ventricular Gallop
Normal below 30 y/o, Pathologic in older (rapid diastole)
4
th
Sound S4, Atrial Gallop
Resistance to diastole due to hypertrophy or injury of ventricular wall
2. Vasculature
- responsible for distributing blood to various tissues of the body.
3. Neurologic Factors Regulating Heart Function
a. Sympathetic Nervous System Stimulation (norepinephrine)
arteriolar vasoconstriction
HR
+inotropic f/x
b. Parasympathetic Nervous System (acetylcholine)
HR
slowed AV conduction
c. Chemoreceptors (carotid and aortic bodies)
O2/CO2 = HR
d. Baroreceptors (aortic arch, carotid sinus, vena cava, PA, atria)
HR = BP changes
C. Assessment
1. Health History
a. Chief Complaint
Myocardial Ischemia/Infarction
Pain (sterna, upper abdomen)
belt-squeezing, radiating to shoulders, neck, arms
Arrythmias/Ischemia
Palpitations
rapid & irregular/pounding heartbeat
Peripheral Vascular Diseasse
Intermittent claudication (extremity pain with exercise)
Page 5 of 8
Ms. April Anne D. Balanon GreywolfRed
PRELIMS
The Respiratory and Cardiovascular System
HANDOUT 1 OXYGENATION:
Compromised Cardiac Function
Dyspnea (DOB, SOB)
Orthopnea
Paroxysmal Nocturnal Dyspnea
Decreased CO2
Fatigue (with or without activity)
Sudden Decrease in CO2
Syncope (with or without dizziness)
Decreased Peripheral Perfusion
Diaphoresis with clamminess and cyanosis
Heart Failure
Edema/Weight gain greater than 3lb in 24 hours
b. History for Risk Factors
Non-Modifiable
- Age, incidence post 40 y/o
- Gender, greater in men but not after menopause
- Race, mortality greater for nonwhites
- + Family history of Cardiovascular Disease
- other illness (diabetic)
Minor Factors
- Personality type
- Sedentary living
- Stress (may contribute to the devt of coronary heart disease)
- Oral Contraceptive Use
Modifiable
- Smoking (2-4x greater risk to CardioVD)
- High calorie, fat, cholesterol, sugar and sodium diet
- High serum lipids (Hyperlipidemia), best indicator is HDL:LDL
- Hypertension (esp. elevated systolic pressure)
- Obesity, contributes to severity of other factors
- Sedentary Lifestyle
2. Physical Assessment
a. Vital Signs - PR, CR, BP, RR
b. Inspection
distress, anxiety, altered LOC
skin color (pallor, cyanosis) , buccal, peripheral
neck vein distention - reflects right atrial pressure (Jugular Vein Pressure, JVD)
respirations (dyspnea, orthopnea)
presence of edema - fluid volume overload
nail clubbing - sign of chronic hypoxia
capillary filling - measure of peripheral circulation (less than 3 secs.)
venous stasis or arterial ulcers , check sacrum for those on bedrest
varicose veins
c. Palpation
PMI (Located at 5th intercostal space, Left MCL)
if too low indicates enlarged heart
Thrills (palpable murmur) thrusts/heaves
Peripheral pulses (carotid, brachial, radial, femoral, popliteal, dorsalis pedis, anterior tibial)
check all bilateral and compare
Grade 0:no puls
1+:weak 2+:normal 3+:increased 4+:bounding
temperature - check bilateral
Page 6 of 8
Ms. April Anne D. Balanon GreywolfRed
PRELIMS
The Respiratory and Cardiovascular System
HANDOUT 1 OXYGENATION:
d. Auscultation
heart rate
rhythm
heart sounds S1 (lub) and S2 (dub)
murmurs
swishing sounds in-between heart sounds (Lub-swish-Dub)
pericardial friction rub
rough, grating sound from inflamed pericardial sac
Bruit, murmur heard outside of the heart
(carotid, jugular, temporal, abdominal, aortic, renal and femoral arteries)
take B/P in both arms, lying, sitting and standing
e. Pulse Assessment
note whether regular or irregular
Regular
o evenly spaced, may vary slightly with respiration
Regularly Irregular
o regular pattern overall with "skipped" beats
Irregularly Irregular
o chaotic, no real pattern, very difficult to measure rate accurately
Tachycardia
o pulse greater than 100 beats/minute
Bradychardia
o pulse less than 60 beats/minute.
Tachycardia and bradycardia are not necessarily abnormal.
Athletes tend to be bradycardic at rest. Tachycardia is a normal response to stress or exercise.
f. BP Assessment
inflate the cuff to 30 mmHg above the estimated systolic pressure, release slowly.
dont use too small a cuff. The pressure will be 10, 20, even 50 mmHg too high
Maximum Cuff Pressure - When the baseline is known or hypertension is not suspected, it is
acceptable in adults to inflate to 200 mmHg
be aware that there could be an ausculatory gap (a silent interval between the true systolic and
diastolic pressures).
g. Perform Respiratory Assessment
- cough, crackles, wheezing, hemoptysis, cheyne-stokes respiration
h. perform Abdominal Assessment
- note liver enlargement /ascites, bladder distention, bruits just above the umbilicus
3. Laboratory and Diagnostic Tests
a. WBC count
b. Lipid Profile cholesterol:LDL, HDL, trigylcerides
c. Cardiac Enzymes (creatinine phosphokinase, troponin, lactate dehdrogenase)
d. Blood Coagulation prothrombin, partial thromboplasitn
e. Chest radiograph heart size
f. ECG hearts electrical activity
g. Holter Montoring 24-hour ECG
h. Exercise ECG ECG with physical stress
i. Echocardiography cardiac (valvular) structures and fuction
j. Radionuclide Testing ventricular function, myocardial bloodflow
k. Cardiac Catheterization chamber pressures and O2 saturation
l. Arteriography coronary arteries (visualization)
m. Ventriculography ventricles (visualization)
n. Central Venous Pressure filling pressure of right ventricle, cardiac function
o. Pulmonary Artery Pressure left heart pressures
Pulmonary Artery Wedge Pressure
p. Arterial Line peripheral arterial pressures
Page 7 of 8
Ms. April Anne D. Balanon GreywolfRed
PRELIMS
The Respiratory and Cardiovascular System
HANDOUT 1 OXYGENATION:
D. Health Promotion
1. Modifying Risk Factors
2. Preventing Venous Stasis
a. Leg Exercises
- for those with impaired mobility (bed-ridden)
- contraction of muscles promote blood back to the heart
b. Application of Antiembolism Stockings
- provide varying degrees of compression on different areas of the leg
- exert external pressure decreasing venous blood from pooling in the extremities
- MUST fit properly, and be applied in the morning before client has gotten out of bed
c. Use of Pneumatic Compression Devices (intermittent or sequential)
d. Avoiding Constriction
- garters, socks with elastic bands, orthopedic casts, leg-crossing
3. Edema Reduction
a. Elevation of Limbs-no pressure on points
b. Diet Teaching-restrict fat consumption ( 30% of daily caloric intake), limit salt intake
c. Fluid Restriction-until balance is restored, monitor I&O
fluid retention=If greater than 2L
wt gain > 1kg/day
4. Positioning
- lying flat promotes venous return
(heart works harder in the supine than in the upright position)
- gravity enhances arterial flow
- hyotensive: elevate legs 20 to 30 degrees
5. Pain Management
a. Chest Pain
stop all activity, rest, sit comfortably, avoid lying flat, administer O2, nitroglycerine SL,
assess BP & PR
b. Claudication, Peripheral Ischemic Pain
not life-threatening but crippling; avoid cold, cigarette smoking
6. Increased Activity & Energy Conservation
gradual and progressive
refrain using the Valsalva maneuver
have constant rest periods
space activities
7. Client Teaching
recognition of warning signs:
perfusion
Page 8 of 8
Ms. April Anne D. Balanon GreywolfRed
PRELIMS
The Respiratory and Cardiovascular System
HANDOUT 1 OXYGENATION:
promotion of blood flow & skin integrity
avoidance of fatigue
8. Medications
explain tx regimen to client and SO, provide written information
9. CPR
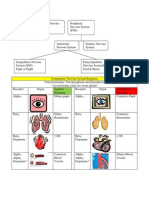
E. Nursing Diagnoses
1. Decreased Cardiac Output
inadequate blood pumped by the heart to meet metabolic demands of the body (active or high risk)
2. Ineffective Tissue Perfusion (Renal, Cerebral, Cardiopulmonary, Gastrointestinal, Peripheral)
decrease in oxygen resulting in failure to nourish the tissues at the capillary level
3. Activity Intolerance
insufficient physiologic or psychological energy to endure or complete required or desired daily activity
F. Overview of Cardiovascular Alterations
1. Arrhythmias (Dysrhythmia)
any sinus rhythm deviating from normal
2. Coronary Artery Disease
focal narrowing of large and medium-sized coronary arteries due to plaque formation
3. Myocardial Infarction
destruction of myocardial tissue in heart regions abruptly deprived of blood supply
(due to coronary blood flow)
4. Heart Failure (left sided or left ventricular & right-sided or right ventricular
syndrome of pulmonary or systemic circulatory congestion
caused by myocardial contractility ( CO2 to meet oxygen requirements of tissues
5. Acute Pulmonary Edema
rapid fluid accumulation in the extravascular lung spaces (alveoli and interstitial)
6. Cardiac Arrest
sudden, unexpected cessation of the hearts pumping action and effecting circulation
7. Endocarditis
infection of the endocarium or heart valves due to bacteria/organsm invation
(acute, subacute, chronic)
8. Pericarditis
inflammation of pericardium (acute, chronic)
9. Pacemaker Implantation
temporary or permanent electronic device to replace function of SA node
pacer is in direct contact of the heart muscle wall, battery operated
10. Hemorrhage
loss of a large amount of blood during a short period
(internal, external, arterial, venous, capillary)
11. Valvular Disorders of the Heart
stenosis (narrowing of the valve opening)
regurgitation/insufficiency (failure of valve to close completely)
Das könnte Ihnen auch gefallen
- CEN Brochure SAFH InformationDokument3 SeitenCEN Brochure SAFH InformationsparticuslivesNoch keine Bewertungen
- Today 5Dokument1 SeiteToday 5sparticuslivesNoch keine Bewertungen
- Expense Analysis WorksheetDokument2 SeitenExpense Analysis WorksheetsparticuslivesNoch keine Bewertungen
- Expense Analysis WorksheetDokument2 SeitenExpense Analysis WorksheetsparticuslivesNoch keine Bewertungen
- CEN Brochure SAFH InformationDokument3 SeitenCEN Brochure SAFH InformationsparticuslivesNoch keine Bewertungen
- Neonatal Icu Skills ChecklistDokument5 SeitenNeonatal Icu Skills ChecklistsparticuslivesNoch keine Bewertungen
- Expense Analysis WorksheetDokument2 SeitenExpense Analysis WorksheetsparticuslivesNoch keine Bewertungen
- Expense Analysis WorksheetDokument2 SeitenExpense Analysis WorksheetsparticuslivesNoch keine Bewertungen
- EndocrineDokument2 SeitenEndocrinesparticuslivesNoch keine Bewertungen
- EndocrineDokument2 SeitenEndocrinesparticuslivesNoch keine Bewertungen
- Expense Analysis WorksheetDokument2 SeitenExpense Analysis WorksheetsparticuslivesNoch keine Bewertungen
- EndocrineDokument2 SeitenEndocrinesparticuslivesNoch keine Bewertungen
- EndocrineDokument2 SeitenEndocrinesparticuslivesNoch keine Bewertungen
- Cardiovascular ReviewDokument8 SeitenCardiovascular ReviewsparticuslivesNoch keine Bewertungen
- ANS ChartDokument3 SeitenANS ChartsparticuslivesNoch keine Bewertungen
- Cardiovascular ReviewDokument8 SeitenCardiovascular ReviewsparticuslivesNoch keine Bewertungen
- Vascular Disorders CH 38Dokument6 SeitenVascular Disorders CH 38sparticuslives100% (1)
- Vascular Disorders CH 38Dokument6 SeitenVascular Disorders CH 38sparticuslives100% (1)
- PCA and Epidural Presentation Outline 2014Dokument10 SeitenPCA and Epidural Presentation Outline 2014sparticuslives100% (1)
- Cardiovascular ReviewDokument8 SeitenCardiovascular ReviewsparticuslivesNoch keine Bewertungen
- Vascular Disorders CH 38Dokument6 SeitenVascular Disorders CH 38sparticuslives100% (1)
- ANS ChartDokument3 SeitenANS ChartKara Dawn MasonNoch keine Bewertungen
- Criteria For INACTIVE MRSA StatusDokument2 SeitenCriteria For INACTIVE MRSA StatussparticuslivesNoch keine Bewertungen
- ANS ChartDokument3 SeitenANS ChartKara Dawn MasonNoch keine Bewertungen
- Explanation of AbbreviationsDokument1 SeiteExplanation of AbbreviationssparticuslivesNoch keine Bewertungen
- Explanation of AbbreviationsDokument1 SeiteExplanation of AbbreviationssparticuslivesNoch keine Bewertungen
- Explanation of AbbreviationsDokument1 SeiteExplanation of AbbreviationssparticuslivesNoch keine Bewertungen
- PCA and Epidural Presentation Outline 2014Dokument10 SeitenPCA and Epidural Presentation Outline 2014sparticuslives100% (1)
- Explanation of AbbreviationsDokument1 SeiteExplanation of AbbreviationssparticuslivesNoch keine Bewertungen
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)