Beruflich Dokumente
Kultur Dokumente
Causes, Presentations, and Treatment of Fulminant Myocarditis
Hochgeladen von
Stacey WoodsOriginalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Causes, Presentations, and Treatment of Fulminant Myocarditis
Hochgeladen von
Stacey WoodsCopyright:
Verfügbare Formate
Ful mi nant Myocardi ti s
Fredric Ginsberg, MD
a,
*, Joseph E. Parrillo, MD
b
BACKGROUND
Myocarditis is an illness caused by inflammation of heart muscle.
1
Viral infections are
the most common cause. Other causes include bacterial and protozoan infections
(Boxes 1 and 2). Myocarditis can also occur in the setting of autoimmune and other
systemic illnesses, including systemic lupus erythematosus, polymyositis, sclero-
derma, sarcoidosis, Whipples disease, and sprue.
a
Division of Cardiovascular Medicine, Cooper University Hospital, One Cooper Plaza, Camden,
NJ 08103, USA;
b
Heart and Vascular Hospital, Hackensack University Medical Center, 30 Pros-
pect Avenue, Hackensack, NJ 07601, USA
* Corresponding author.
E-mail address: Ginsberg-Fredric@CooperHealth.edu
KEYWORDS
Immune mechanisms
Lymphocytic myocarditis
Inotropic agents
Fulminant myocarditis
Mechanical circulatory support
Extracorporeal membrane oxygenator
Ventricular assist device
KEY POINTS
Myocarditis is most often caused by a viral infection. Less common causes include other
infectious agents and autoimmune diseases.
Fulminant myocarditis is an unusual complication with a rapidly progressive course result-
ing in severe heart failure and cardiogenic shock. Fulminant myocarditis should be treated
with full supportive care, using aggressive pharmacologic therapy and mechanical circu-
latory support, because significant improvement in left ventricular function will often
occur. Cardiac transplantation is required in a small minority of patients.
Cardiac magnetic resonance imaging is becoming a frequently used modality to aid in the
diagnosis of myocarditis.
Endomyocardial biopsy should be used in fulminant myocarditis for diagnosis and poten-
tially to direct therapy. Although there are limitations in the interpretation and application
of biopsy results, newer methods of analyzing biopsies allow the identification of a pre-
sumed viral cause and identification of persistence of viral infection.
Immunosuppressive therapy should not be used routinely in the treatment of myocarditis
but should be strongly considered in patients who have severe heart failure and who do
not improve or deteriorate during conventional heart failure treatment. Clinical trials are
being performed to try to identify appropriate patients for this therapy.
Crit Care Clin 29 (2013) 465483
http://dx.doi.org/10.1016/j.ccc.2013.03.004 criticalcare.theclinics.com
0749-0704/13/$ see front matter 2013 Elsevier Inc. All rights reserved.
The most common type of myocarditis seen on myocardial biopsy is lymphocytic
myocarditis, whereby myocardial inflammation with lymphocytes, myocytolysis, and
fibrosis are present. Two other distinct pathologic types of myocarditis are (1) eosin-
ophilic myocarditis, which is characterized by eosinophilic infiltration and degranula-
tion and associated with hypersensitivity reactions, most often to medications and
Box 1
Common viral causes of myocarditis
RNA Viruses
Coxsackie A and B
Echovirus
Poliovirus
Hepatitis A, B and C
Respiratory syncytial virus
Mumps
Rubella
Dengue
Yellow fever
Influenza A and B
DNA Viruses
Adenovirus
Cytomegalovirus
Herpes simplex virus
Varicella
Parvo B19
Epstein-Barr virus
Human immunodeficiency virus
Box 2
Nonviral infectious causes of myocarditis
Bacterial: brucella, Corynebacterium diphtheriae, gonococcus, Haemophilus influenzae,
meningococcus, mycobacterium, Mycoplasma pneumoniae, pneumococcus, salmonella,
Serratia marcescens, staphylococcus, Streptococcus pneumoniae, S pyogenes, Treponema
pallidum, Tropheryma whippelei, and Vibrio cholerae
Spirochetal: Borrelia and leptospira
Fungal: actinomyces, aspergillus, blastomyces, candida, Coccidioides, Cryptococcus,
Histoplasma, mucormycosis, Nocardia, and Sporothrix
Protozoal: Toxoplasma gondii and Trypanosoma cruzi
Parasitic: ascaris, Echinococcus granulosus, Paragonimus westermani, schistosoma, Taenia
solium, Trichinella spiralis, visceral larva migrans, and Wuchereria bancrofti
Rickettsial: Coxiella burnetii, Rickettsia rickettsii, and R tsutsugamushi
Ginsberg & Parrillo 466
vaccines, including the smallpox vaccine,
2,3
and (2) giant cell myocarditis, an autoim-
mune disease.
4
Rarely, inflammation may be seen with granulomas, such as in
sarcoidosis.
The spectrumof illness caused by myocarditis varies widely. In the mildest form, pa-
tients are asymptomatic or have mild symptoms typical of a viral illness and recover
without specific therapy. Other common presentations include moderate to severe
chest pain, often mimicking acute myocardial infarction, or the new onset of acute
or subacute heart failure. Heart failure symptoms may be mild, and patients may
respond well to medical therapy. However, many patients with myocarditis will present
with severe heart failure or cardiogenic shock with circulatory collapse. Fulminant
myocarditis is diagnosed when patients have a distinct time of symptomonset, usually
within the preceding 2 weeks, severe class IV heart failure symptoms, and hypoten-
sion or cardiogenic shock requiring treatment with inotropes, vasopressors or me-
chanical circulatory support. Fulminant myocarditis is distinguished form acute,
nonfulminant myocarditis, where the onset of illness is less distinct, heart failure symp-
toms are less severe, hypotension is infrequent, and inotropes or vasopressors are
generally not required (Table 1).
5,6
Patients with fulminant myocarditis compose about
10% of the cases of myocarditis with heart failure
7
and about 10% of biopsy-positive
myocarditis cases, although fulminant myocarditis composed 38% of the cases of
myocarditis in children in one series.
8
EPIDEMIOLOGY
Although a specific cause of myocarditis is not determined in most cases, in North
America and Europe it is presumed that a viral infection is the most common cause.
1
Many viruses have been implicated as causative agents (see Box 1). Coxsackie B in-
duces acute myocarditis progressing to dilated cardiomyopathy in murine models
9
and was thought to be the most common cause of human myocarditis up to the
1990s. Adenovirus, parvovirus B-19 (PVB19), and human herpesvirus 6 (HHV 6) are
thought to be the more common causes now. In a series of patients with myocarditis
and positive endomyocardial biopsy (EMB), PVB 19, HHV 6, or both were implicated in
most patients.
10
Another series implicated PVB 19 in 28.7% of cases, HHV 6 in 11%,
enterovirus in 6%, and Epstein-Barr (EB) virus and adenovirus in fewer patients.
11
In
adult PVB 19 myocarditis, inflammation of coronary artery endothelial cells leads to
myocardial ischemia and necrosis from reduced blood flow, mimicking ischemic syn-
dromes caused by coronary artery atherosclerosis.
12,13
In children, PVB 19 has been
implicated as a common cause of fulminant myocarditis.
14
Enterovirus has been
Table 1
Comparison of fulminant myocarditis and acute, severe myocarditis
Onset of Illness
Heart Failure
Symptoms Hypotension Cardiogenic Shock
Fulminant Distinct onset of
symptoms in
prior 12 wk
Class IV Present with need
for inotropes and
vasopressors
Often present, need
for IABP, VAD, or
ECMO (children)
Acute, severe Indistinct onset
of symptoms
Class III-IV Not present or mild Not present
Abbreviations: ECMO, extracorporeal membrane oxygenator; IABP, intra-aortic balloon counter-
pulsation; VAD, ventricular assist device.
Fulminant Myocarditis 467
associated in case reports of sudden cardiac death caused by acute myocarditis.
15
Myocarditis is a common finding in patients infected with human immunodeficiency
virus (HIV). However, the causative agent responsible in these cases may be associ-
ated viral infections, such as cytomegalovirus, or other infections, such as Mycobac-
teria, fungi, or parasites, rather than HIV itself.
1,16
Dengue viral infection has been
associated with fatal fulminant myocarditis.
17
Lyme disease is complicated by
myocarditis in 1% of cases. Patients with Lyme myocarditis typically present with
heart block but may also have severe ventricular arrhythmia and severe left ventricular
dysfunction.
18
Other infectious illnesses associated with myocarditis include acute
rheumatic fever, diphtheria, and Campylobacter enteritis.
19,20
In Central and South
America, the most common cause of myocarditis is the protozoan Trypanosoma cruzi,
the cause of Chagas disease.
Unfortunately, it is difficult to make a clinical diagnosis of a specific viral cause of
myocarditis. This diagnosis usually requires the measurement of antiviral antibody
titers in acute and convalescent phase sera. Viral cultures of tissue specimens are
unreliable.
19
The identification of viral genomes incorporated in myocyte DNA, using
polymerase chain reaction (PCR) techniques, suggests that a particular virus is the
causative agent.
PATHOGENESIS
Based on observations of human myocarditis, as well as murine models of the disease
caused by Coxsackie B3, the pathogenesis of viral myocarditis can be described in 3
stages.
2,5,21
In the first stage, there is viremia, binding of virus to myocytes, and viral
replication within myocytes. Viral proteases and activation of cytokines may produce
myocyte damage and apoptosis.
22
Cytoskeletal proteins may be cleaved by viral pro-
teases. The presence of this viral replication phase is difficult to detect clinically
because patients may be asymptomatic during this phase or may only have nonspe-
cific viremic symptoms. In addition, certain viruses, such as PVB 19, may attack endo-
thelial cells in coronary arteries, venules, and capillaries, and myocardial damage may
be a result of the impairment of blood flow.
12
Direct cytolysis of myocytes caused by the initial viral infection in stage 1 is thought
to be particularly important in fulminant myocarditis. Early and extensive loss of myo-
cytes and myocardial tissue leads to the rapid development of severe heart failure.
The second stage involves host immune activation. Stimulation of cellular immunity
as well as humoral responses attenuate viral proliferation and can result in recovery
from the illness. However, unabated immune activation can result in activated T cells
targeting myocardial antigens, which cross-react with viral peptides. T-cell activation
leads to the release of cytokines, such as tumor necrosis factor, interleukin-1, and
interleukin-6, resulting in further myocyte damage.
1,22
The activation of CD4 cells
and antibody production plays a less important pathogenetic role. It is thought that
this secondary immune response to viral infection is often the most important mech-
anism in disease pathogenesis.
22
Evidence supporting these mechanisms includes the following: Myocardial biopsy
with recombinant DNA techniques can detect viral genomes in 20% to 35% of pa-
tients. Tissue-specific autoantibodies have been detected in 25% to 73% of patients
with evidence of myocarditis on biopsy, with antibodies directed against contractile,
structural, and mitochondrial myocyte proteins. Inappropriate expression of the major
histocompatibility complex can frequently be demonstrated on biopsy specimens.
1
Elevated levels of inflammatory cytokines have been detected in patients with active
myocarditis.
Ginsberg & Parrillo 468
In the third stage, myocardial damage is mediated by persistent activation of cellular
immunity, with left ventricular dilation and remodeling leading to neurohormonal acti-
vation, systolic dysfunction, and manifestations of heart failure.
5,22
The virus may be
effectively cleared or may persist in the myocardium. These processes may abate,
with reduction in left ventricular size and improvement of left ventricular function, or
can continue to progress with worsening ventricular function, the development of
dilated cardiomyopathy, and chronic heart failure. Chronic dilated cardiomyopathy
is the major long-term sequela of acute myocarditis (Fig. 1).
DIAGNOSIS
Patients ill with myocarditis present with nonspecific symptoms of dyspnea (72%),
chest pain (32%), and symptoms of arrhythmia (18%).
23
The presentation may be
indistinguishable fromacute coronary syndromes because of coronary artery disease.
There may have been a preceding viral prodrome with fever, malaise, and arthralgias.
Physical examination may show fever and a pericardial rub if pericarditis is present. In
patients with fulminant myocarditis, patients have tachycardia, hypotension, S3
gallop, elevated jugular venous pressure, and other signs of severe heart failure,
including pulmonary rales and wheezes with impending respiratory failure. Murmurs
of mitral regurgitation and tricuspid regurgitation may be heard.
19
In a series of acute
myocarditis in children, 36% presented with heart failure, 22% with arrhythmia, 10%
with syncope, and 13%with shock.
8
The differential diagnosis includes acute myocar-
dial infarction, pericarditis, or chest pain from pulmonary causes, including pulmonary
embolism or pneumonia. Generalized sepsis is also a consideration.
Laboratory findings can include leukocytosis and an elevated erythrocyte sedimen-
tation rate. Cardiac biomarkers, such as creatine kinase (CPK), troponin T, and
troponin I, may be elevated, with sensitivity of troponin I reported at 34% and speci-
ficity of 89%.
24
In fulminant myocarditis, elevated serum urea nitrogen, creatinine, and
liver transaminases reflect end-organ failure. The 12-lead electrocardiogram in fulmi-
nant myocarditis may show sinus tachycardia, nonspecific ST segment depression,
and T-wave inversion; but conduction disturbances, such as heart block or left bundle
branch block, are often present. ST segment elevation mimicking acute myocardial
infarction can be seen. The presence of a wide QRS complex or pathologic Q waves
has been associated with a poorer prognosis.
25
Echocardiography is essential to diagnose and quantitate regional and global left
ventricular wall motion abnormalities, left ventricular and right ventricular size and
function, the presence of pericardial effusion, and valvular regurgitation. Fulminant
myocarditis is characterized by a nondilated left ventricle with severe systolic
dysfunction and increased wall thickness reflecting myocardial edema, whereas in
acute but nonfulminant myocarditis, the left ventricle is dilated with normal wall thick-
ness. Right ventricular dysfunction is more common in fulminant myocarditis and por-
tends a poorer prognosis.
5,25,26
Cardiac catheterization and coronary angiography
are often necessary to exclude acute ischemia as the cause of chest pain or acute
heart failure.
There is increasing use of cardiac magnetic resonance imaging (CMR) as a nonin-
vasive means to diagnose myocarditis.
2729
Diagnostic criteria include the following:
(1) focal or diffuse myocardial edema in T2-weighted images, (2) early gadolinium
enhancement indicating inflammation, and (3) late gadolinium enhancement (LGE) in
subepicardial or midmyocardial areas indicating necrosis and fibrosis. Abnormalities
may be diffuse or patchy, often confined to the lateral free wall of the left ventricle
or the base of the intraventricular septum (Fig. 2). Diagnostic accuracy of CMR is
Fulminant Myocarditis 469
Fig. 1. The pathogenesis of viral myocarditis involves direct myocardial injury from viral infection as well as immune-mediated myocyte damage from
cytokines, proteases, and autoantibodies. The outcome of these processes can be healing of inflammation and resolution of acute myocarditis or persis-
tent inflammation and development of chronic dilated cardiomyopathy. INF, interferon; TNF, tumor necrosis factor.
G
i
n
s
b
e
r
g
&
P
a
r
r
i
l
l
o
4
7
0
reported at 78% when 2 or 3 criteria are present and 68% when only LGE is present.
CMRis more likely to be abnormal when performed more than 7 days after the onset of
symptoms. In 2 reports of cases of fulminant myocarditis, CMRperformed 6 days after
presentation showed only myocardial edema without gadolinium enhancement, indi-
cating inflammation with little fibrosis.
30
CMR can also be used to direct myocardial
biopsy in patients with patchy involvement. A given finding on CMR may correlate
with the severity of disease acutely, but the value of CMR for assessing long-term
prognosis is unknown.
3134
In one series, LGE was associated with larger left ventri-
cles, poorer ejection fractions, and poorer outcomes.
10
Percutaneous EMB is used to aid in the diagnosis of myocarditis and is considered
the definitive diagnostic technique. The Dallas criteria are one standard for histopath-
ologic diagnosis. These criteria define active myocarditis as the presence of an inflam-
matory myocardial infiltrate (more than 5 lymphocytes per high-power field)
accompanied by myocyte necrosis. Borderline myocarditis is defined as inflammation
without myocyte necrosis. However, there is no difference in prognosis in patients with
either of these biopsy results.
7
Thus, lymphocyte infiltration (with or without myocyte
necrosis) is the most important diagnostic criterion. Examining specimens for viral ge-
nomes using PCR or using immunohistochemistry technology to identify upregulated
HLA proteins offers improved diagnostic yield.
11,21,35
Fig. 2. CMR with LGE: normal and abnormal findings in myocarditis. (A) Normal myocar-
dium with no evidence of irreversible myocyte injury. (B) Regional subepicardial enhance-
ment of the lateral wall (arrow). (C) Subepicardial enhancement of lateral and midwall
enhancement of the septal wall (arrows). (D) Diffuse subepicardial enhancement.
Fulminant Myocarditis 471
Limitations of using the Dallas criteria on right ventricular biopsy specimens include
a high frequency of interobserver variation and a low sensitivity for diagnosis in sus-
pected cases of myocarditis. Various series have reported positive right ventricular
biopsy results in only 10% to 67% of patients. These results may relate to the timing
of biopsies in respect to the stage or chronicity of illness. In addition, myocardial
inflammation is often not diffuse but is patchy and may predominantly involve the
left ventricle, so random right ventricular biopsies may miss affected myocardium.
35
Performing a biopsy earlier in a patients clinical course, taking multiple biopsy spec-
imens, and performing left ventricular biopsies are ways of improving diagnostic yield.
EMB should be performed in centers with a high-volume experience, with proven
safety, and availability of appropriate pathologic techniques.
36
It is important to
emphasize that a negative biopsy finding does not preclude the diagnosis of myocar-
ditis. A positive biopsy finding has a high positive predictive value.
7
Endomyocardial biopsy should be performed in patients with fulminant myocarditis,
severe ventricular arrhythmias, or advanced heart block according to recommenda-
tions in the scientific statement from the American Heart Association/American Col-
lege of Cardiology/European Society of Cardiology. EMB was deemed useful,
beneficial, and effective (class I indication) to differentiate lymphocytic myocarditis
from giant cell myocarditis and eosinophilic myocarditis because immunosuppressive
therapy is mandated in the latter two conditions.
37,38
EMB should always be per-
formed before initiating immunosuppressive therapy (Table 2).
MANAGEMENT
Heart Failure Management and Circulatory Support
Patients with fulminant myocarditis demonstrate hypotension, respiratory failure, and
signs of end organ hypoperfusion, including oliguria and neurologic abnormalities.
Initial treatment often requires mechanical ventilation, inotropic agents, and vasopres-
sors. Dobutamine is a potent beta
1
-agonist with less beta
2
- and alpha-agonist proper-
ties. Dobutamine increases myocardial contractility, reduces systemic vascular
Table 2
Cardiac testing in fulminant myocarditis
ECG 1. Nonspecific ST segment and T-wave changes
2. ST segment elevation mimicking acute pericarditis
3. ST segment changes mimicking acute transmural myocardial
infarction
Chest radiography Pulmonary edema
Echocardiography 1. Regional LV wall motion abnormality
2. Global LV wall motion abnormality
3. LV wall thickening caused by myocardial edema
CMR imaging 1. Focal or diffuse myocardial edema
2. Early gadolinium enhancement indicating inflammation
3. LGE in subepicardial or midmyocardial areas indicating necrosis
and fibrosis
Cardiac catheterization Often necessary to exclude acute myocardial infarction; no
coronary artery obstruction
EMB Lymphocyte infiltration (Dallas criteria)
Myocytolysis
Rarely eosinophilic or giant cell inflammation (nonviral causes)
Abbreviations: ECG, electrocardiogram; LV, left ventricular.
Ginsberg & Parrillo 472
resistance, and reduces pulmonary capillary wedge pressure. However, dobutamine
can be proarrhythmic, and patients can develop tolerance to the drug.
39
Milrinone is
another parenteral inotropic agent, which works by inhibiting myocyte phosphodies-
terase. This drug increases inotropy, stroke volume, and cardiac index and decreases
systemic vascular resistance, systemic blood pressure, and pulmonary capillary
wedge pressure. Milrinone is difficult to use in patients who are already hypotensive
but may be combined with vasopressors. It is less proarrhythmic than dobutamine.
40,41
Arterial vasoconstrictors, such as norepinephrine and dopamine, are used for patients
with refractory hypotension. However, these agents increase myocardial oxygen con-
sumption and do not increase cardiac index (Table 3).
In patients with fulminant myocarditis and cardiogenic shock not responding to
pharmacologic therapy, intra-aortic balloon counterpulsation (IABP) can be used. If
this is not effective in maintaining adequate cardiac output, then mechanical circula-
tory assistance should be instituted. There are catheter-base devices, implanted
percutaneously, which can provide a cardiac output of 3.5 to 5.0 L/min for several
days. The TandemHeart device (CardiacAssist, Pittsburgh, PA) requires placement
of a catheter via a transatrial septal puncture. The Impella pump (Abiomed, Danvers,
MA) is entirely intracorporeal and pulls blood fromthe left ventricle and pumps through
the catheter tip in the aorta. In the most seriously ill patients, extracorporeal mem-
brane oxygenators (ECMO) or ventricular assist devices (VADs) are used to provide
greater hemodynamic support. In ECMO, often used for support of critically ill pediat-
ric patients, a pump provides circulation through an external oxygenator. VADs are
mechanical pumps that provide physiologic cardiac output and reduce left ventricular
afterload. VADs can support left and right ventricular function. Complications of VADs
include infection, sepsis, thromboemboli, and bleeding.
42,43
In patients with myocarditis, VADs can be used to provide adequate circulation for a
more extended time period. Beneficial reverse remodeling may occur while patients
are on VAD support, resulting in improved myocyte structure and function, allowing
resolution of myocarditis and improvement or recovery of left ventricular function to
occur. Unresolved issues regarding VAD usage in patients with myocarditis include
appropriate patient selection, timing of VAD placement, best medical therapy during
VAD support, and optimal duration of VAD support. In one study, 80% of patients
who ultimately recovered required VAD support for up to 90 days.
44
The optimal
means of serial assessment of native cardiac function while on VAD support needs
to be delineated, and the best weaning protocol also needs definition.
Several reports suggest that fulminant myocarditis with circulatory failure may
occur more frequently in children. In one registry of 514 pediatric patients with
myocarditis, ECMO was used in 18.9% of patients, VADs in 4.3%, and both were
Table 3
Medical therapy for fulminant myocarditis
Acute, severe heart failure: pulmonary
congestion/edema
Intravenous diuretic: furosemide
Reduced cardiac output: hypotension,
oliguria, confusion
Inotropes: dobutamine, milrinone
Cardiogenic shock Vasopressors: norepinephrine
Therapy for left ventricular systolic
dysfunction: succinate recuperative phase
receptor blockers
Beta-blockers: carvedilol, metoprolol
ACE-inhibitors, or angiotensin
Aldosterone blockers: spironolactone
Fulminant Myocarditis 473
used in 2.9%; 4.1% of patients eventually required cardiac transplantation.
45
In
another series of 20 patients at a single center, 10 children required ECMO and 3
had biventricular assist devices. Early use of ECMO in pediatric fulminant myocarditis
was recommended when the following were present: (1) end organ dysfunction, (2)
severe ventricular arrhythmia, and (3) the need for cardiopulmonary resuscitation
(unless of very short duration).
6
Cardiac transplantation is the final option for treating critically ill patients with
myocarditis. However, these patients have a higher rate of transplant rejection and
a lower survival rate when compared with patients transplanted for ischemic or other
causes of cardiomyopathy. Myocarditis has been reported to recur in the transplanted
heart.
46
After hemodynamics improve, when patients have recovered from shock, medical
therapy for heart failure with left ventricular systolic dysfunction is instituted. There
are data in murine models of myocarditis supporting the use of angiotensin-
converting enzyme (ACE) inhibitors, angiotensin blockers, and beta-blockers. These
drugs reduce inflammation and lessen necrosis and fibrosis.
2,21,32,47
There are
convincing data in humans supporting the use of these medication as well as aldoste-
rone antagonists in patients with dilated cardiomyopathy. Therefore, in patients with
myocarditis and heart failure, the use of standard multidrug medical therapy for heart
failure and left ventricular systolic dysfunction is indicated.
46,47
These medications
have been shown to improve symptoms, prolong life, and regress the adverse left ven-
tricular remodeling in patients with dilated cardiomyopathy of various causes.
4850
Treatment with ACE inhibitors should be initiated at low doses, with upward titration
to maximally tolerated doses. Patients should be closely monitored for potential side
effects, including renal insufficiency, hyperkalemia, and angioedema. Relative contra-
indications to the use of ACE inhibitors include hypotension, renal failure, hyperkale-
mia, bilateral renal artery stenosis, and hepatic failure.
Therapy with beta-adrenergic blockade was associated with improved survival in
a multivariate analysis of patients with acute myocarditis.
11
Large randomized
controlled clinical trials, which included patients with idiopathic dilated cardiomyopa-
thy, have unequivocally shown benefit from beta-blockers in patients with left ventric-
ular systolic dysfunction
5155
; these agents should also be used in patients with heart
failure caused by myocarditis. Beta-blockers should be initiated after patients are on a
stable dose of ACE inhibitors and when signs of fluid overload have resolved. Contra-
indications to beta-blocker therapy include bronchospastic disease or severe chronic
obstructive lung disease, heart block, or significant underlying bradycardia. Hypoten-
sion should be corrected before initiating beta-blocker therapy.
Digoxin has been shown in animal models to decrease levels of cytokines, but
digoxin was associated with adverse outcomes in one murine model of myocarditis.
Digoxin can be useful in helping to control ventricular rates in patients with atrial fibril-
lation. The use of digoxin can be considered in patients with significant left ventricular
systolic dysfunction who remain ill despite therapy with ACE inhibitors and beta-
blockers. However, no survival benefit for digoxin has ever been shown in patients
with heart failure caused by dilated cardiomyopathy.
56
Contraindications to the use
of digoxin include renal failure and heart block.
Lastly, the use of the aldosterone antagonist spironolactone has been shown to
have symptomatic and survival benefit in patients with class III-IV chronic systolic
heart failure.
57
In experimental models, these agents can reverse the progressive
myocardial fibrosis that occurs in the remodeling process of dilated cardiomyopathy.
These agents have not been studied in patients with myocarditis, but their use should
be strongly considered in patients with severe left ventricular dysfunction (ejection
Ginsberg & Parrillo 474
fraction less then 35%) and symptomatic heart failure. Contraindications to the use of
aldosterone antagonists include renal insufficiency, with serum creatinine levels of
more than 2.0 mg/dl, or hyperkalemia. Serum potassium levels needs to be carefully
monitored during initiation and dose titration (see Table 3).
Arrhythmias and conduction abnormalities, when present during the acute phase of
myocarditis, are treated in a similar manner as in patients with other heart diseases,
using antiarrhythmic drugs or temporary pacemakers as required. However, a period
of observation is strongly recommended to assess for improvement in cardiac func-
tion before implantation of a permanent pacemaker or internal cardioverter-
defibrillator.
Immunosuppressive Therapy
Because immune mechanisms are involved in the pathogenesis of myocarditis, trials
have been performed to evaluate the effectiveness of immunosuppressive therapy.
However, no studies have been done to evaluate this therapy in patients with fulminant
myocarditis. Reported trials vary with regard to types of patients (acute vs subacute
myocarditis vs chronic dilated cardiomyopathy) and kinds of therapy (prednisone,
azathioprine, or immune globulin). The high rate of spontaneous recovery of normal
left ventricular function (40%) in patients with acute myocarditis also needs to be taken
into account.
The Myocarditis Treatment Trial enrolled 111 patients with a positive EMB and left
ventricular ejection fraction less than 45%, with a duration of illness of less than
2 years.
58
Three treatment groups were compared: daily prednisone plus azathioprine,
prednisone plus cyclosporine, and placebo. Mortality was 20% at 1-year and 56% at
3 years. These investigators found no difference in ejection fraction, no change in left
ventricular size, and no difference in 1-year mortality between treated and untreated
groups. Their conclusion was that these immunosuppressive strategies were not
beneficial. Significant limitations of this study include a 30% dropout rate and signif-
icant interobserver variability among pathologists diagnoses of biopsy specimens
using the Dallas criteria.
Small studies suggested that in patients with heart failure and low ejection fraction,
intravenous immunoglobulin has a pronounced antiinflammatory effect as measured
by circulating levels of inflammatory markers.
59
Uncontrolled studies suggested a
benefit in patients with myocarditis from treatment with intravenous immune glob-
ulin.
60,61
However, a placebo-controlled double-blind trial of intravenous immune
globulin in patients with myocarditis or idiopathic dilated cardiomyopathy of less
than 6 months showed no significant improvement with therapy as assessed by ejec-
tion fraction or functional capacity at 6 and 12 months.
62
In this study, the average left
ventricular ejection fraction improved from 25% 8% at baseline to 41% 17% at
6 months in both treated and untreated groups. The 1-year event-free survival rate
was 91.9% in both groups, indicating a favorable prognosis. At this time, treatment
with intravenous immune globulin is not recommended.
12
In another study, patients with positive endomyocardial biopsy specimens and pro-
gressive heart failure who responded to 6 months of therapy with prednisone and
azathioprine were more likely to have circulating cardiac autoantibodies and no viral
genome in their myocardium as compared with nonresponders.
63
More recently, a
randomized, placebo-controlled trial of prednisone plus azathioprine was performed
in 85 patients with chronic heart failure (>6 month illness) with active lymphocytic
myocarditis on EMB and absence of viruses seen on PCR analysis. The study showed
significant improvement in left ventricular ejection fraction in the treated group
(average ejection fraction increased from 26.5% to 45.6%) and no improvement in
Fulminant Myocarditis 475
controls (average ejection fraction 27.7%21.3%). In addition, there was significant
improvement in left ventricular dimensions and patients functional status in the group
receiving immunosuppression. This study suggests that this therapy may have favor-
able effects in patients who persist with active myocardial inflammation even after the
virus has been cleared.
64
In view of the limitations of histopathologic diagnosis using the Dallas criteria,
another group of investigators used immunohistologic markers of inflammation, upre-
gulation of HLA, to diagnose active myocarditis and to use as an indication for immu-
nosuppressive therapy.
65
This criterion has the advantage of indicating that
autoimmunity is playing a role in pathogenesis. Also, because HLA is distributed
throughout the myocardium, biopsy sampling error is eliminated as a confounding var-
iable in assessing the response to therapy. In this study, 84 of 202 patients with
chronic (>6 months) idiopathic dilated cardiomyopathy (ejection fraction <40%)
were found to have a strong expression of HLA in biopsy specimens and were ran-
domized to receive placebo or prednisone plus azathioprine for 3 months. At the
follow-up, a significant improvement in the prespecified secondary endpoints of left
ventricular ejection fraction, left ventricular volumes, and functional capacity was
seen in the treated group; this improvement was maintained at 2 years (71.8%
improvement in the treated group vs 30.8% in the untreated group). However, there
was no improvement in the prespecified composite primary endpoint of death, cardiac
transplant, or hospital readmission. This study was limited by a 31% dropout rate.
In summary, there is no evidence that patients with acute lymphocytic myocarditis
benefit from the routine use of immunosuppressive therapy. However, this treatment
approach should be considered in patients with myocarditis and positive endomyo-
cardial biopsy findings on a case-by-case basis, including those who experience
progressive and severe worsening of left ventricular function who are not responding
to supportive therapies. Other investigators recommend avoiding the use of immuno-
suppression if viral clearance has not been demonstrated.
12
Appropriately powered,
controlled, prospective studies of homogeneous patient groups using immunosup-
pressive therapy are still needed. Immunosuppressive therapy should be used in pa-
tients with myocarditis associated with connective tissue diseases, such as systemic
lupus erythematosus, eosinophilic or granulomatous forms of the disease, and in giant
cell myocarditis (Fig. 3).
Phase 2 trials are ongoing to evaluate antiviral therapy with beta-interferon in
patients with chronic myocarditis with persistent viral infection.
12
No large experience
has been reported using this therapy in acute myocarditis. Evaluating the mechanisms
of myocardial recovery during VAD support may help direct research toward novel
approaches to the treatment of severe myocarditis.
OUTCOMES
It is important todefine the patient population under study andthe criteria usedfor diag-
nosing myocarditis in any series assessing prognosis and mortality. No clinical markers
reliably predict which patients with myocarditis will recover or worsen.
7
In the Myocar-
ditis Treatment Trial, factors predicting a worse prognosis included hypotension (mean
systolic and diastolic blood pressure of patients who did poorly was 84/49 mm Hg),
higher pulmonary capillary wedge pressure (mean of 24 mm Hg), and the use of me-
chanical ventilation. Factors that were not predictive of mortality included sex, age,
heart rate, cardiac index, peak CPK, or the use of IABP for circulatory support.
58
In another study of 147 patients with biopsy-positive lymphocytic myocarditis and
heart failure with left ventricular ejection fraction less than 40%, 10% were diagnosed
Ginsberg & Parrillo 476
with fulminant myocarditis and 90% with acute, nonfulminant myocarditis.
7
Patients
received aggressive treatments with inotropes, vasopressors, and mechanical sup-
port. Patients with fulminant myocarditis had better survival at 1 year than those
with acute myocarditis (93% vs 85%). Survival at 11 years was also better (93% vs
45%). Lower pulmonary capillary wedge pressure and higher cardiac index also pre-
dicted improved survival (Fig. 4).
Another study reported 181 patients with myocarditis confirmed by EMB using the
Dallas criteria, immunohistochemical analysis, and PCR. Left ventricular biopsy was
performed in 90% of the group. A total of 22% of patients died or received cardiac
transplantation at an average follow-up of 59 months. Presentation with class III or
IV symptoms and positive immunohistochemistry results were the only predictors of
poor outcomes in a multivariate analysis. Beta-blocker therapy was significantly asso-
ciated with improved outcome. The 5-year survival was only 39% in patients with
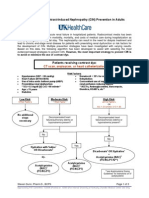
Fig. 3. Algorithm describing a reasonable approach to myocarditis management based on
currently available data. CAD, coronary artery disease; CHF, congestive heart failure; CMP,
cardiomyopathy; EF, ejection fraction; LV, left ventricular. (From Parrillo J. Myocarditis:
how should we treat in 1998? J Heart Lung Transplant 1998;17:9414; with permission.)
Fulminant Myocarditis 477
severe symptoms, positive immunohistochemistry, and absence of beta-blocker ther-
apy (Fig. 5).
11
Other retrospective analyses have reported that larger left ventricular size, worse left
ventricular systolic function, and LGE on CMR are predictive of worse long-term out-
comes.
10
LGE involving the septum and larger percentage of left ventricular mass
Fig. 4. Unadjusted transplantation-free survival according to clinicopathological classifica-
tion. Patients with fulminant myocarditis were significantly less likely to die or require heart
transplantation during follow-up than were patients with acute myocarditis (P 5 .05 by the
log-rank test). (From McCarthy R, Boehmer J, Hruban R, et al. Long-term outcome of fulmi-
nant myocarditis as compared with acute (nonfulminant) myocarditis. N Engl J Med
2000;342:693; with permission.)
Fig. 5. Prognosis for patients with acute myocarditis was predicted by 3 factors: NYHA
functional class, positive immunohistology for myocarditis at EMB, and therapy with
beta-blockers. NYHA, New York Heart Association. (From Kindermann I, Kindermann M,
Kandolf R, et al. Predictors of outcome in patients with suspected myocarditis. Circulation
2008;118:645; with permission.)
Ginsberg & Parrillo 478
showing LGE were associated with chronic left ventricular dysfunction.
13
In a study of
patients with fulminant myocarditis who received VAD therapy, factors favoring recov-
ery and VAD explant included rapid onset of symptoms, rapid recovery of left ventric-
ular function, and female sex.
66
Several articles have presented prognostic data in children with acute myocarditis.
One study reported 20 patients seen during a 12-year period. Ten patients received
support with ECMO, 7 of whom survived. Three patients received biventricular me-
chanical support. ECMO was initiated at a mean of 2 days after presentation and
was continued for 6 to 8 days.
6
In another report, 11 children with fulminant myocar-
ditis were seen over a 5-year period. Mean left ventricular ejection fraction was 22%.
One patient died of ventricular tachycardia. The remaining patients survived, left the
intensive care unit after a 2- to 3-week course, and had significant improvement of
left ventricular function at 30 days and complete normalization at 5 years. None of
these patients received mechanical circulatory support.
67
A retrospective review of 216 cases of pediatric myocarditis seen at 35 hospitals re-
ported 92% survival. A total of 45% of patients received milrinone, 34% received
dopamine, 35%epinephrine, and 37.5%received mechanical support. Seven percent
of patients received ECMO, and 1.9% underwent cardiac transplant. Mortality was
associated with a higher severity of illness scores.
68
Other studies report significantly higher mortality in pediatric myocarditis caused by
PVB19 and in patients with higher initial levels of troponin.
14
In a Japanese survey dur-
ing 1997 to 2002, pediatric patients with fulminant myocarditis had a 48.4%mortality.
8
In a database review of 514 pediatric patients with myocarditis, 4.1% of whom
received cardiac transplantation, those receiving ECMO and/or VAD therapy had a
76% survival rate.
45
SUMMARY
Myocarditis is an illness caused by inflammation of heart muscle, most often caused
by a viral infection. Autoimmune mechanisms are key in the pathogenesis of the con-
dition. Myocarditis can be mild and self-limiting, or it may cause severe illness with
heart failure and severe left ventricular dysfunction. Fulminant myocarditis refers to
those most critically ill patients with severe heart failure, respiratory failure, hypoten-
sion, and cardiogenic shock. Fulminant myocarditis is differentiated from acute,
severe myocarditis, when there is severe heart failure but not circulatory collapse or
shock. Although these patients may require intravenous inotropes and vasopressors
as well as mechanical circulatory support, most will survive and will experience signif-
icant improvement in left ventricular function.
Advanced diagnostic techniques, including myocardial biopsy with left ventricular
biopsy, analysis of biopsy specimens for viral genomes and HLA proteins, and CMR
imaging, are being used more frequently to guide therapy and prognostication. The
role of immunosuppressive therapy remains ill defined and controversial in patients
with fulminant myocarditis because most cases will recover after a period of aggressive
cardiac support. Most investigators do recommend immunosuppression if patients do
not show significant and timely improvement of heart failure and left ventricular func-
tion, especially in patients with acute, severe, nonfulminant myocarditis.
REFERENCES
1. Feldman A, McNamara D. Myocarditis. N Engl J Med 2000;343:138898.
2. Cooper LT. Myocarditis. N Engl J Med 2009;360:152638.
Fulminant Myocarditis 479
3. GinsbergFL, Parrillo JE. Eosinophilic myocarditis. In: Dec GW, editor. Heart failure
clinics, myocarditis. Philadelphia: W.B. Saunders Co 2005;1(3):41929.
4. Cooper L, Berry G, Shabetai R. Idiopathic giant cell myocarditis-natural history
and treatment. N Engl J Med 1997;336:18606.
5. Drazner MH, Gupta S, Mammen PP, et al. Fulminant myocarditis. Nat Clin Pract
Cardiovasc Med 2008;5:693706.
6. Teele S, Allan CK, Laussen PC, et al. Management and outcomes in pediatric pa-
tients presenting with acute fulminant myocarditis. J Pediatr 2011;158:63843.
7. McCarthy R, Boehmer J, Hruban F, et al. Long term outcome of fulminant
myocarditis as compared with acute (nonfulminant) myocarditis. N Engl J
Med 2000;342:6905.
8. Saji T, Matsuura H, Hasegawa K, et al. Comparison of the clinical presentation,
treatment, and outcome of fulminant and acute myocarditis in children. Circ J
2012;76:12228.
9. Fairweather D, Stafford KA, Sung YK. Update on Coxsackie B3 myocarditis.
Curr Opin Rheumatol 2012;24:4017.
10. Grun S, Schumm J, Greulich S, et al. Long-term follow-up of biopsy-proven viral
myocarditis. J Am Coll Cardiol 2012;59:160415.
11. Kindermann I, Kindermann M, Kandolf R, et al. Predictors of outcome in patients
with suspected myocarditis. Circulation 2008;118:63948.
12. Schultheiss HP, Kuhl U, Cooper LT. The management of myocarditis. Eur Heart J
2011;32:261625.
13. Marholdt H, Wagner A, Deluigi CC, et al. Presentation, patterns of myocardial
damage, and clinical course of viral myocarditis. Circulation 2006;114:158190.
14. Molina KM, Garcia X, Denfield SW, et al. Parvovirus B19 myocarditis causes sig-
nificant morbidity and mortality in children. Pediatr Cardiol 2013;34(2):3907.
http://dx.doi.org/10.1007/s00246-012-0468-4.
15. Gaaloul I, Riabi S, Harrath R, et al. Sudden unexpected death related to entero-
virus myocarditis: histopathology, immunohistochemistry and molecular pathol-
ogy diagnosis at post-mortem. BMC Infect Dis 2012;12:2127.
16. Barbaro G, Fisher SD, Lipshultz SE. Pathogenesis of HIV-associated cardiovas-
cular complications. Lancet Infect Dis 2001;1:11524.
17. Daniel RA, Silva AR, Neppelenbroek VB, et al. Fulminant myocarditis and viral
infection. J Clin Virol 2012. http://dx.doi.org/10.1016/j.jcv.2012.06.015.
18. Koene R, Boulware DR, Kemperman M, et al. Acute heart failure from Lyme car-
ditis. Circ Heart Fail 2012;5:e246.
19. Kavinsky CJ, Parrillo JE. Rheumatic fever and cardiovascular diseases. In:
Austen KF, Frank MM, Atkinson JP, et al, editors. Samters Immunol Dis. Philadel-
phia: Lippincott; 1995;5:82340.
20. De Cock D, Hiltrop T, Timmermans P, et al. Myocarditis associated with
campylobacter enteritis: report of three cases. Circ Heart Fail 2012;5:e1921.
21. Magnani JW, Dec GW. Myocarditis. Current trends in diagnosis and treatment.
Circulation 2006;113:87690.
22. Liu P, Mason J. Advances in the understanding of myocarditis. Circulation 2001;
104:107682.
23. Hufnagel G, Pankuweit S, Richter A, et al. The European Study of Epidemiology
and Treatment of Cardiac Inflammatory Disease (ESETCID). First epidemiolog-
ical results. Herz 2000;25:27985.
24. Smith SC, Ladenson JH, Mason JW, et al. Elevations of cardiac troponin I asso-
ciated with myocarditis; experimental and clinical correlates. Circulation 1997;
30:13549.
Ginsberg & Parrillo 480
25. Elamm C, Fairweather D, Cooper LT. Pathogenesis and diagnosis of myocar-
ditis. Heart 2012;98:83540.
26. Schultz JC, Hilliard AA, Cooper LT, et al. Diagnosis and treatment of viral
myocarditis. Mayo Clin Proc 2009;84(11):10019.
27. Liu PP, Yan AT. Cardiovascular magnetic resonance for the diagnosis of acute
myocarditis; prospects for detecting myocardial inflammation. J Am Coll Cardiol
2005;45:19235.
28. Abdel-Aty H, Boye P, Zagrosek A, et al. Diagnostic performance of cardiovascu-
lar magnetic resonance in patients with suspected acute myocarditis. J Am Coll
Cardiol 2005;45:181522.
29. Marholdt H, Goedecke C, Wagner A, et al. Cardiovascular magnetic resonance
assessment of human myocarditis. Circulation 2004;109:12508.
30. Mavrogeni S, Bratis K, Terrovitis, et al. Fulminant myocarditis: can cardiac
magnetic resonance predict evolution to heart failure? Int J Cardiol 2012;
159:e378.
31. Childs H, Friedrich MG. Cardiovascular magnetic resonance imaging in myocar-
ditis. Prog Cardiovasc Dis 2011;54:26675.
32. Ellis CR, DiSalvo T. Myocarditis. Basic and clinical aspects. Cardiol Rev 2007;
15:1707.
33. Nelson KH, Li T, Afonso L. Diagnostic approach and role of MRI in the assess-
ment of acute myocarditis. Cardiol Rev 2009;17:2430.
34. Friedrich MG, Sechtem U, Schulz-Menger J, et al. Cardiovascular magnetic
resonance in myocarditis: a JACC white paper. J Am Coll Cardiol 2009;
53(17):147587.
35. Parrillo JE. Inflammatory cardiomyopathy (myocarditis): which patients should
be treated with anti-inflammatory therapy? Circulation 2001;104:46.
36. McKenna W, Davies M. Immunosuppression for myocarditis. N Engl J Med
1995;333:3123.
37. Cooper LT, Baughman K, Feldman AM, et al. The role of endomyocardial
biopsy in the management of cardiovascular disease: a scientific statement
from the American Heart Association, the American College of Cardiology
and the European Society of Cardiology. Circulation 2007;116:221633.
38. Wu L, Lapeyre A, Cooper L. Current role of endomyocardial biopsy in the man-
agement of dilated cardiomyopathy and myocarditis. Mayo Clin Proc 2001;76:
10308.
39. Jain P, Massie B, Gattis W, et al. Current medical treatment for the exacerbation
of chronic heart failure resulting in hospitalization. Am Heart J 2003;145:S317.
40. Jaski B, Fifer M, Wright R, et al. Positive inotropic and vasodilator actions of mil-
rinone in patients with severe congestive heart failure. J Clin Invest 1985;75:
6439.
41. Cuffe M, Califf R, Adams K, et al. Short-term intravenous milrinone for acute
exacerbation of chronic heart failure: a randomized controlled trial. JAMA
2002;287:15417.
42. Wilson SR, Mudge GH Jr, Stewart JC, et al. Evaluation for a ventricular assist de-
vice: selecting the appropriate candidate. Circulation 2009;119:222532.
43. Mancini D, Burkoff D. Mechanical device-based methods of managing and
treating heart failure. Circulation 2005;12:43848.
44. Farrar D, Holman W, McBride L, et al. Long-term follow-up of Thoratec ventric-
ular assist device bridge-to-recovery patients successfully removed from sup-
port after recovery of ventricular function. J Heart Lung Transplant 2002;21:
51621.
Fulminant Myocarditis 481
45. Ghelani SJ, Spaeder MC, Pastor W, et al. Demographics, trends, and outcomes
in pediatric acute myocarditis in the United States, 2006 to 2011. Circ Cardio-
vasc Qual Outcomes 2012;5:6227.
46. Haas G. Etiology, evaluation, and management of acute myocarditis. Cardiol
Rev 2001;9:8895.
47. Winkel E, Costanzo M, Parrillo JE. Myocarditis. Curr Treat Options Cardiovasc
Med 2000;2:40719.
48. Pfeffer M, Braunwald E, Moye L, et al. Effect of captopril on mortality and
morbidity in patients with left ventricular dysfunction after myocardial infarction.
N Engl J Med 1992;327:66977.
49. The SOLVD Investigators: effect of enalapril on survival in patients with reduced
left ventricular ejection fractions and congestive heart failure. N Engl J Med
1991;25:293302.
50. Garg R, Yusuf S. Overview of randomized trials of angiotensin converting
enzyme inhibitors on mortality and morbidity in patients with heart failure.
JAMA 1995;273:14506.
51. Packer M. Current role of beta-adrenergic blockers in the management of
chronic heart failure. Am J Med 2001;110:81S4S.
52. CIBIS II Investigators: the Cardiac Insufficiency Bisoprolol Study II: a random-
ized trial. Lancet 1999;353:913.
53. Hjalmarson A, Goldstein S, Fagerberg B. The MERIT-HF Study Group: effects of
controlled release metoprolol on total mortality, hospitalizations and well-being
in patients with heart failure. JAMA 2000;283:1295302.
54. Bristow M, Gilbert E, Abraham W, et al. Carvedilol produces dose related im-
provements in left ventricular function and survival in subjects with chronic heart
failure. Circulation 1996;94:280716.
55. Packer M, Coats A, Fowler M, et al. Effects of carvedilol on survival in severe
chronic heart failure. N Engl J Med 2001;344:16518.
56. The Digitals Investigation Group: the effect of digoxin on mortality and morbidity
in patients with heart failure. N Engl J Med 1997;336:52533.
57. Pitt B, Zannad F, Remme W, et al. The effects of spironolactone on morbidity and
mortality in patients with severe heart failure. N Engl J Med 1999;341:70917.
58. Mason J, OConnell J, Herskowitz A, et al. A clinical trial of immunosuppressive
therapy for myocarditis. N Engl J Med 1995;333:26975.
59. Gullestad L, Aass H, Field J, et al. Immunomodulating therapy with intravenous
immunoglobulin in patients with chronic heart failure. Circulation 2001;103:
2205.
60. McNamara D, RosenblumW, Janosko K, et al. Intravenous immune globulin in the
therapy of myocarditis and acute cardiomyopathy. Circulation 1997;95:24768.
61. Patel P, Lenihan D. The current status of immune modulating therapy for myocar-
ditis: a case of acute parvovirus myocarditis treated with intravenous immuno-
globulin. Am J Med Sci 2003;26:36974.
62. McNamara DM, Holubkov R, Starling RC, et al. Controlled trial of intravenous
immune globulin in recent-onset dilated cardiomyopathy. Circulation 2001;
103:22549.
63. Frustaci A, Chimenti C, Calabrese F, et al. Immunosuppressive therapy for
active lymphocytic myocarditis: virological and immunologic profile of
responders versus non-responders. Circulation 2003;107:85763.
64. Frustaci A, Russo MA, Chimenti C. Randomized study on the efficacy of immu-
nosuppressive therapy in patients with virus-negative inflammatory cardiomyop-
athy: the TIMIC study. Eur Heart J 2009;30:19952002.
Ginsberg & Parrillo 482
65. Wojnicz R, Nowalany-Kozielska E, Wojciechowska C, et al. Randomized pla-
cebo controlled study for immunosuppressive treatment of inflammatory dilated
cardiomyopathy: two year follow-up results. Circulation 2001;104:3945.
66. Atluri PA, Ullery BW, MacArthur JW, et al. Rapid onset of fulminant myocar-
ditis portends a favourable prognosis and the ability to bridge mechanical cir-
culatory support to recovery. Eur J Cardiothorac Surg 2013;43(2):37982.
http://dx.doi.org/10.1093/ejcys/ezs242.
67. Amabile FA, Fraisse A, Bouvenot J, et al. Outcome of acute fulminant myocar-
ditis in children. Heart 2006;92:126973.
68. Klugman D, Berger JT, sable CA, et al. Pediatric patients hospitalized with
myocarditis: a multi-institutional analysis. Pediatr Cardiol 2010;31:2228.
Fulminant Myocarditis 483
Das könnte Ihnen auch gefallen
- Emergency diagnosis and treatment of acute pericarditis and myocarditisDokument6 SeitenEmergency diagnosis and treatment of acute pericarditis and myocarditisRexy NunuhituNoch keine Bewertungen
- Challenges and Opportunities in Pediatric Heart Failure and TransplantationDokument15 SeitenChallenges and Opportunities in Pediatric Heart Failure and TransplantationvijuNoch keine Bewertungen
- MyocarditisDokument29 SeitenMyocarditispanvilai0% (1)
- International Journal of Pharmaceutical Science Invention (IJPSI)Dokument4 SeitenInternational Journal of Pharmaceutical Science Invention (IJPSI)inventionjournalsNoch keine Bewertungen
- Viral MyocarditisDokument42 SeitenViral MyocarditisAlishba AtifNoch keine Bewertungen
- Adolescent Onset of Acute Heart FailureDokument19 SeitenAdolescent Onset of Acute Heart FailureVeronica Romero MouthonNoch keine Bewertungen
- MYOCARDITIS: A GUIDE TO THE INFLAMMATORY HEART DISEASEDokument56 SeitenMYOCARDITIS: A GUIDE TO THE INFLAMMATORY HEART DISEASENANNY MARSIDINNoch keine Bewertungen
- CARDIOMYOPATHIES AND MYOCARDITIS DIAGNOSIS AND TREATMENTDokument72 SeitenCARDIOMYOPATHIES AND MYOCARDITIS DIAGNOSIS AND TREATMENTASDASDDD2Noch keine Bewertungen
- DR Julian-MYOCARDITISDokument83 SeitenDR Julian-MYOCARDITISArmando Esteban Coa SandovalNoch keine Bewertungen
- Miocarditis Review NatureDokument11 SeitenMiocarditis Review NatureNox ÁtroposNoch keine Bewertungen
- Articulo COVID 19Dokument9 SeitenArticulo COVID 19Omaira TovarNoch keine Bewertungen
- Arritmias en Miocarditis ViralDokument13 SeitenArritmias en Miocarditis ViralOscar F RojasNoch keine Bewertungen
- Subacute and Chronic MeningitisDokument8 SeitenSubacute and Chronic MeningitisLucky PuspitasariNoch keine Bewertungen
- MiokarditisDokument65 SeitenMiokarditisMicija CucuNoch keine Bewertungen
- Cardiomyopathy and Myocarditis GuideDokument62 SeitenCardiomyopathy and Myocarditis GuideGrace CastilloNoch keine Bewertungen
- 392 2009 Article 69Dokument11 Seiten392 2009 Article 69PutraChamplenxNoch keine Bewertungen
- Myocarditis pathogenesis and clinical managementDokument13 SeitenMyocarditis pathogenesis and clinical managementYenna YinNoch keine Bewertungen
- Acute Viral Myocarditis: Epidemiology and Pathophysiology: Lara Shekerdemian, MD, MRCP Desmond Bohn, MB, MRCPDokument6 SeitenAcute Viral Myocarditis: Epidemiology and Pathophysiology: Lara Shekerdemian, MD, MRCP Desmond Bohn, MB, MRCPMike ShufflebottomNoch keine Bewertungen
- Cardiac EmergenciesDokument21 SeitenCardiac Emergenciesgus_lionsNoch keine Bewertungen
- Rheumatic Heart DiseaseDokument68 SeitenRheumatic Heart DiseaseFuji Khairunnisa0% (1)
- Myocarditis: Leslie T. Cooper Jr. and Kirk U. KnowltonDokument21 SeitenMyocarditis: Leslie T. Cooper Jr. and Kirk U. KnowltonAnonymous cdLyeXKBNoch keine Bewertungen
- Myocarditis in ChildrenDokument14 SeitenMyocarditis in ChildrenFildzah DheaNoch keine Bewertungen
- Recurrent MeningitisDokument14 SeitenRecurrent Meningitisidno1008Noch keine Bewertungen
- Journal Pre-Proof: IdcasesDokument8 SeitenJournal Pre-Proof: IdcasesDaniel GuevaraNoch keine Bewertungen
- Chapter 14 Diseases of The PericardiumDokument12 SeitenChapter 14 Diseases of The PericardiumfathirNoch keine Bewertungen
- Department of Internal Medicine Iii Hemorrhagic Syndromes: - Rajkumar Subasaravanan Subgroup "12"Dokument122 SeitenDepartment of Internal Medicine Iii Hemorrhagic Syndromes: - Rajkumar Subasaravanan Subgroup "12"Suba Saravanan 12Noch keine Bewertungen
- Myocarditis Nejm 2022 ReviewDokument13 SeitenMyocarditis Nejm 2022 ReviewNox ÁtroposNoch keine Bewertungen
- Pediatric Myocarditis FdneDokument12 SeitenPediatric Myocarditis FdneRonit KumarNoch keine Bewertungen
- Infecciones Oportunistas Del SNC en VIH LAncet 2010Dokument13 SeitenInfecciones Oportunistas Del SNC en VIH LAncet 2010Natalia Obando LermaNoch keine Bewertungen
- Acute Isolated MyocarditisDokument20 SeitenAcute Isolated Myocarditismerin sunilNoch keine Bewertungen
- Aureus or Escherichia Coli. Less Typically, Polymicrobial Abscesses Have Been NotedDokument7 SeitenAureus or Escherichia Coli. Less Typically, Polymicrobial Abscesses Have Been NotedDiana MinzatNoch keine Bewertungen
- 25 Kawasaki DiseaseDokument13 Seiten25 Kawasaki DiseaseVictor PazNoch keine Bewertungen
- Myocarditis: Review ArticleDokument13 SeitenMyocarditis: Review ArticlejaimeferNoch keine Bewertungen
- Nej MR A 2114478Dokument13 SeitenNej MR A 2114478Medicina Interna residentesNoch keine Bewertungen
- Myocarditis NEJM 2022Dokument13 SeitenMyocarditis NEJM 2022Πάνος ΣταγήςNoch keine Bewertungen
- Myocarditisreview Currentopinioninpediatrics2010Dokument6 SeitenMyocarditisreview Currentopinioninpediatrics2010vijuNoch keine Bewertungen
- Acute Viral Myocarditis: Current Concepts in Diagnosis and TreatmentDokument6 SeitenAcute Viral Myocarditis: Current Concepts in Diagnosis and TreatmentvijuNoch keine Bewertungen
- Infective Endocarditis and The CNS: StrokeDokument8 SeitenInfective Endocarditis and The CNS: Strokeriskiamanda13Noch keine Bewertungen
- KARDIOMIOPATI HIVDokument8 SeitenKARDIOMIOPATI HIVnetizen baikNoch keine Bewertungen
- Vaccines 10 01286 PDFDokument7 SeitenVaccines 10 01286 PDFAarathi raoNoch keine Bewertungen
- Myocarditis With Complete Heart Block Challenges in Diagnosis and Treatment Consultant360Dokument1 SeiteMyocarditis With Complete Heart Block Challenges in Diagnosis and Treatment Consultant360shrisane333Noch keine Bewertungen
- Dr. Kanupriya ChaturvediDokument67 SeitenDr. Kanupriya ChaturvediHeru MohamadNoch keine Bewertungen
- 28 Infective EndocarditisDokument10 Seiten28 Infective EndocarditisVictor PazNoch keine Bewertungen
- Key Answers Part 2 December 2019 PDFDokument29 SeitenKey Answers Part 2 December 2019 PDFNimer Abdelhadi AliNoch keine Bewertungen
- Med 9780190862800 Chapter 59Dokument8 SeitenMed 9780190862800 Chapter 59ntnquynhproNoch keine Bewertungen
- Update On Rheumatic Heart Disease: ReviewDokument7 SeitenUpdate On Rheumatic Heart Disease: ReviewAlfa AlfinNoch keine Bewertungen
- Pulmonary Infiltrates in The Non-HIV-Infected Immunocompromised PatientDokument12 SeitenPulmonary Infiltrates in The Non-HIV-Infected Immunocompromised PatientAri KuncoroNoch keine Bewertungen
- Acquired Heart DiseasesDokument41 SeitenAcquired Heart DiseasesSaman SarKoNoch keine Bewertungen
- JCM 12 01254Dokument12 SeitenJCM 12 01254Javier MartinNoch keine Bewertungen
- Viral Encephalitis PDFDokument7 SeitenViral Encephalitis PDFDeborah Bravian TairasNoch keine Bewertungen
- Aseptic Meningitis in Adults - UpToDateDokument16 SeitenAseptic Meningitis in Adults - UpToDateKondász Antal Gábor MedNoch keine Bewertungen
- CNS InfectionDokument6 SeitenCNS InfectionAnonymous nruHyuwtJNoch keine Bewertungen
- HIV-Associated Opportunistic Infections of The CNSDokument13 SeitenHIV-Associated Opportunistic Infections of The CNSmauroignacioNoch keine Bewertungen
- 2020 Article 435Dokument25 Seiten2020 Article 435Carlos Peña PaterninaNoch keine Bewertungen
- Artigo Neuromeningeal Cryptococcosis in A Patient Not Infected With HumanDokument4 SeitenArtigo Neuromeningeal Cryptococcosis in A Patient Not Infected With HumanRENATA SANTOS ASSUNCAONoch keine Bewertungen
- PericarditisDokument11 SeitenPericarditisrbarcellonaNoch keine Bewertungen
- Medical Progress: Review ArticleDokument11 SeitenMedical Progress: Review ArticleGaby Alejandra Ordonez AndradeNoch keine Bewertungen
- Diagnosis, Management, and Pathophysiology of Arterial and Venous Thrombosis in COVID-1Dokument2 SeitenDiagnosis, Management, and Pathophysiology of Arterial and Venous Thrombosis in COVID-1samuelNoch keine Bewertungen
- Heart Valve Disease: State of the ArtVon EverandHeart Valve Disease: State of the ArtJose ZamoranoNoch keine Bewertungen
- Secondary HypertensionVon EverandSecondary HypertensionAlberto MorgantiNoch keine Bewertungen
- IDSA Releases Guidance On Antibiotic Selection For Gram-Negative Antimicrobial-Resistant Bacterial Infections - ACP Internist Weekly - ACP InternistDokument3 SeitenIDSA Releases Guidance On Antibiotic Selection For Gram-Negative Antimicrobial-Resistant Bacterial Infections - ACP Internist Weekly - ACP InternistStacey WoodsNoch keine Bewertungen
- Tamiflu PrescribingDokument26 SeitenTamiflu PrescribingStacey WoodsNoch keine Bewertungen
- Id 397 TeicoplaninDokument2 SeitenId 397 TeicoplaninStacey WoodsNoch keine Bewertungen
- Switching Ace-Inhibitors: Change To Change From Enalapril Quinapril RamiprilDokument2 SeitenSwitching Ace-Inhibitors: Change To Change From Enalapril Quinapril RamiprilGlory Claudia KarundengNoch keine Bewertungen
- Antibiotic Selection - The Clinical AdvisorDokument6 SeitenAntibiotic Selection - The Clinical AdvisorStacey WoodsNoch keine Bewertungen
- Appropriate Use of Laxatives in The Older PersonDokument7 SeitenAppropriate Use of Laxatives in The Older PersonStacey WoodsNoch keine Bewertungen
- J Jacadv 2023 100389Dokument12 SeitenJ Jacadv 2023 100389Edward ElBuenoNoch keine Bewertungen
- Management of Bacterial and Fungal Infections in Cirrhosis JOH 2021Dokument17 SeitenManagement of Bacterial and Fungal Infections in Cirrhosis JOH 2021Francisco Javier Gonzalez NomeNoch keine Bewertungen
- Palliative2 Nausea MedtableDokument2 SeitenPalliative2 Nausea MedtableStacey WoodsNoch keine Bewertungen
- Therapeutic Drug Monitoring in Adults at NUH2011 FinalDokument2 SeitenTherapeutic Drug Monitoring in Adults at NUH2011 FinalStacey WoodsNoch keine Bewertungen
- Antithrombotic Therapy For VTE DiseaseDokument13 SeitenAntithrombotic Therapy For VTE DiseaseStacey WoodsNoch keine Bewertungen
- Multimorbidity Clinical Assessment and Management 1837516654789Dokument22 SeitenMultimorbidity Clinical Assessment and Management 1837516654789Stacey WoodsNoch keine Bewertungen
- 2023 ESPEN Practical and Partially Revised Guideline - Clinical Nutrition in The Intensive Care UnitDokument19 Seiten2023 ESPEN Practical and Partially Revised Guideline - Clinical Nutrition in The Intensive Care UnitStacey WoodsNoch keine Bewertungen
- Critical CareDokument8 SeitenCritical CareDzikrul Haq KarimullahNoch keine Bewertungen
- Splenectomy Guideline Final 2012Dokument6 SeitenSplenectomy Guideline Final 2012Stacey WoodsNoch keine Bewertungen
- Antibiotik WhoDokument49 SeitenAntibiotik WhodjebrutNoch keine Bewertungen
- C.a.U.S.E. - Cardiac Arrest Ultra-Sound Exam - A Better Approach To Managing Patients in Primary Non-Arrhythmogenic Cardiac ArrestDokument2 SeitenC.a.U.S.E. - Cardiac Arrest Ultra-Sound Exam - A Better Approach To Managing Patients in Primary Non-Arrhythmogenic Cardiac ArrestStacey WoodsNoch keine Bewertungen
- Drug Information Center/KAUH: Selecting Gluten-Free Antibiotics in Celiac DiseaseDokument6 SeitenDrug Information Center/KAUH: Selecting Gluten-Free Antibiotics in Celiac DiseaseStacey WoodsNoch keine Bewertungen
- Stimulant May Speed Antidepressant Response Time in ElderlyDokument3 SeitenStimulant May Speed Antidepressant Response Time in ElderlyStacey WoodsNoch keine Bewertungen
- Biomarkers of SepsisDokument8 SeitenBiomarkers of SepsisStacey WoodsNoch keine Bewertungen
- Procoagulant GuidelineDokument30 SeitenProcoagulant GuidelineStacey WoodsNoch keine Bewertungen
- Antimicrobials at The End of LifeDokument2 SeitenAntimicrobials at The End of LifeStacey WoodsNoch keine Bewertungen
- Potasio. 2014.Dokument19 SeitenPotasio. 2014.Nestor Enrique Aguilar SotoNoch keine Bewertungen
- Preoperative Insulin 2013Dokument3 SeitenPreoperative Insulin 2013Stacey WoodsNoch keine Bewertungen
- Fluid Choices Impact Outcome in Septic ShockDokument7 SeitenFluid Choices Impact Outcome in Septic ShockStacey WoodsNoch keine Bewertungen
- StrokeDokument2 SeitenStrokeStacey WoodsNoch keine Bewertungen
- Contrast NephRopathy GuidelinesDokument3 SeitenContrast NephRopathy GuidelinesStacey WoodsNoch keine Bewertungen
- Airway Clearance in The Intensive Care UnitDokument5 SeitenAirway Clearance in The Intensive Care UnitStacey WoodsNoch keine Bewertungen
- Elderly Patients Making Wise ChoicesDokument6 SeitenElderly Patients Making Wise ChoicesStacey WoodsNoch keine Bewertungen
- The ABC of Weaning Failure - A Structured ApproachDokument9 SeitenThe ABC of Weaning Failure - A Structured ApproachArul ShanmugamNoch keine Bewertungen
- Standard Surgical Attire Surgical ScrubDokument20 SeitenStandard Surgical Attire Surgical ScrubzekkipianoNoch keine Bewertungen
- Major Internship DTR JulyandaugustDokument1 SeiteMajor Internship DTR JulyandaugustGeraldineMoletaGabutin100% (1)
- Study On The Effect of Vatajstanyadushti in ChildrenDokument8 SeitenStudy On The Effect of Vatajstanyadushti in ChildrenRadha DeviNoch keine Bewertungen
- PE 3 ReviewerDokument5 SeitenPE 3 ReviewerZac GarciaNoch keine Bewertungen
- Application of Nursing ProcessDokument2 SeitenApplication of Nursing ProcessClarence ViboraNoch keine Bewertungen
- Mouth Throat Nose and Sinuses Assessment FindingsDokument5 SeitenMouth Throat Nose and Sinuses Assessment FindingsChris SmithNoch keine Bewertungen
- Sexual Health After MenopauseDokument98 SeitenSexual Health After MenopauseWirelessWomanNoch keine Bewertungen
- Piis1470204520302722 PDFDokument2 SeitenPiis1470204520302722 PDFkayegi8666Noch keine Bewertungen
- Tinnitus Today December 1998 Vol 23, No 4Dokument29 SeitenTinnitus Today December 1998 Vol 23, No 4American Tinnitus AssociationNoch keine Bewertungen
- Emergency Department Case Management: Second EditionDokument39 SeitenEmergency Department Case Management: Second EditionsadikinNoch keine Bewertungen
- Lesson PlanDokument5 SeitenLesson Planapi-458907281100% (1)
- Parenteral Nutrition CalculationsDokument62 SeitenParenteral Nutrition CalculationsaqeelaadnanNoch keine Bewertungen
- Research ProposalDokument4 SeitenResearch ProposalMintu SebastianNoch keine Bewertungen
- Rush University HCQDokument24 SeitenRush University HCQJuana Atkins100% (1)
- 125.6 (Medicine) DISCHARGE PLANDokument1 Seite125.6 (Medicine) DISCHARGE PLANNadja Jamilah100% (1)
- Hope 11 Assessment 1 4TH QTRDokument2 SeitenHope 11 Assessment 1 4TH QTRApril Rose Ferrancullo RelojNoch keine Bewertungen
- RRL Caring TITLE: Impact of Nursing Care in The Nursing Profession ObjectivesDokument13 SeitenRRL Caring TITLE: Impact of Nursing Care in The Nursing Profession ObjectivesroblesNoch keine Bewertungen
- Study Guide: MandatoryDokument21 SeitenStudy Guide: Mandatoryyolanda fransiskaNoch keine Bewertungen
- SWOT AnalysisDokument3 SeitenSWOT Analysisdadedidopyaaang100% (2)
- Digital Healthcare Market Research 3Dokument33 SeitenDigital Healthcare Market Research 3Nero AngeloNoch keine Bewertungen
- Shalini Tummala ResumeDokument2 SeitenShalini Tummala Resumeapi-385467850Noch keine Bewertungen
- Biological Child PsychiatryDokument264 SeitenBiological Child Psychiatrydejoguna126100% (2)
- Bupivacaine (Marcaine)Dokument2 SeitenBupivacaine (Marcaine)Michalis SpyridakisNoch keine Bewertungen
- Europass Curriculum Vitae: Personal InformationDokument7 SeitenEuropass Curriculum Vitae: Personal InformationAndrei TudoracheNoch keine Bewertungen
- Patient Scenario, Chapter 19, Nutritional Needs of A NewbornDokument3 SeitenPatient Scenario, Chapter 19, Nutritional Needs of A NewbornNobiliary ortizNoch keine Bewertungen
- RSVDokument8 SeitenRSVilyas9558Noch keine Bewertungen
- R G C I & R C: Ajiv Andhi Ancer NstituteDokument7 SeitenR G C I & R C: Ajiv Andhi Ancer NstituteShubham JainNoch keine Bewertungen
- List Cebu AFFIL PHYSICIANS1 (Wo Neuro) - As of 09012011Dokument6 SeitenList Cebu AFFIL PHYSICIANS1 (Wo Neuro) - As of 09012011Irish BalabaNoch keine Bewertungen
- G-Ranitidine: Commonly used medicines for acid reflux and ulcersDokument4 SeitenG-Ranitidine: Commonly used medicines for acid reflux and ulcersHoney Grace L LemorenasNoch keine Bewertungen