Beruflich Dokumente
Kultur Dokumente
Bizarre Metal Splint
Hochgeladen von
Ahmad Assari0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
15 Ansichten1 SeiteBizarre Metal Splint
Copyright
© © All Rights Reserved
Verfügbare Formate
PDF, TXT oder online auf Scribd lesen
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenBizarre Metal Splint
Copyright:
© All Rights Reserved
Verfügbare Formate
Als PDF, TXT herunterladen oder online auf Scribd lesen
0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
15 Ansichten1 SeiteBizarre Metal Splint
Hochgeladen von
Ahmad AssariBizarre Metal Splint
Copyright:
© All Rights Reserved
Verfügbare Formate
Als PDF, TXT herunterladen oder online auf Scribd lesen
Sie sind auf Seite 1von 1
not concerned with their health needs
to be approached with due care and
appropriate understanding of human
physiology Im sure we may all have
come across obese or overweight indi-
viduals who may not necessarily agree
with such generalised statements.
As your keen readers would have
spotted in issue 10 (214: 489), the
British Society of Periodontology is
embarking upon a large campaign to
raise awareness of periodontal diseases
for both clinicians and patients, with
particular emphasis on the systemic
links. A recent joint workshop between
leading world-renowned clinicians and
researchers of the European Federation
of Periodontology and the American
Academy of Periodontology evaluated
the entire evidence base in a systematic
way (see www.efp.org for a comprehen-
sive summary).
The association is indeed modest,
with an Odds Ratio of 1.81,
1
but the
biological plausibility is valid obese
patients are at a heightened constant
state of systemic infammation as well
as at a high risk of insulin resistance,
both of which we know can impact host
immune responses hence its association
with periodontal disease.
2
When researchers started noticing a
link between smoking and periodon-
tal diseases,
3
the association was put
down to the assumption of poor oral
hygiene, just as suggested here by C.
Marks. Well-conducted research by
Bergstrm
4
fnally proved smoking
as its own risk factor, and the rest, as
they say, is history.
Therefore, may we suggest to our
colleagues living in this world of
evidence-based medicine and dentistry,
that we allow our dedicated researchers
to do what they do best, and await for
further defnitive research to give clini-
cians the fully-informed guidance we
need on the management of periodonti-
tis in overweight and obese patients.
M. Tank, O. Patel, S. Boghani, A. Al-Omar
London
1. Suvan J, DAiuto F, Moles D, Petrie A, Donos N.
Association between overweight/obesity and peri-
odontitis in adults. A systematic review. Obes Rev
2011; 12: e381404.
2. Linden G, Lyons A, Scannapieco F. Periodontal
systemic associations: review of the evidence.
J Clin Periodont 2013; 40 Suppl 14: S8S19.
3. Pindborg J. Tobacco and gingivitis (I). J Dent Res
1947; 26: 261264.
4. Bergstrm J, Preber H. Cigarette smoking in
patients referred for periodontal treatment. Scan J
Dent Res 1986; 94: 102108.
DOI: 10.1038/sj.bdj.2013.749
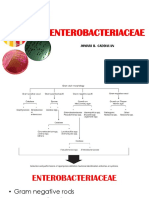
BIZARRE METAL SPLINT
Sir, I recently saw a 64-year-old male
patient who presented with pain from
the lower left quadrant and requested
an extraction of a retained root in
this region.
On intraoral examination, to my
amazement there was a bizarre metal
splint covering all the teeth in both the
upper and lower arches (Figs1-2). This
had been in place for over a year, as
confrmed by the patient and judging
by the amount of calculus visible.
The splints were constructed by the
patient, a former engineer who was
quite good with his hands. He claimed
the splints had helped to stabilise his
mobile teeth, enabling him to chew
food much better.
The retained root was not visible
in the oral cavity, but an OPG X-ray
revealed a retained root in the region of
the 36 and the splints frmly secured in
place (Fig.3).
The irony of it all was that the patient
wanted the retained root removed, but
his precious splint kept intact at all
times. The patient also failed to men-
tion if he had attempted an extraction
himself leaving a retained root behind.
We agreed that a hospital referral was
in the patients best interest, in case of
any other underlying pathology.
Hopefully the hospital may have per-
suaded the patient to have the splints
removed, which may have resulted in
the removal of the underlying teeth, as
the splints seemed frmly secured with
some sort of strong cement.
The end result may be the provision
of a denture after the extraction of the
mobile teeth, unless the patient decides
to construct a DIY implant himself!
Though homemade devices are rare in
the UK this is an example of one such
rare case.
V. Egemonye
London
DOI: 10.1038/sj.bdj.2013.750
NOT AN IANB
Sir, I have been successfully using a
local anaesthetic (LA) technique intro-
duced to me by Professor Brian Millar
(Kings Dental Institute, London) which
is reliable, predictable and gives far
greater patient comfort than inferior
alveolar nerve blocks (IANBs). Pain-
less IANBs are not always achievable,
quick in onset or capable of achieving
profound anaesthesia.
1
There is also
the potential for nerve damage inde-
pendent of the LA used but especially
associated with the use of articaine.
2,3
Initially, I apply topical anaesthetic
gel and give a buccal infltration along-
side the tooth I intend to anaesthetise.
After waiting for onset of anaesthe-
sia from the infltration, I administer
0.1ml articaine 4% with 1:100,000
adrenaline (Septanest), both mesially
and distally of the tooth to be treated,
BRITISH DENTAL JOURNAL VOLUME 215 NO. 3 AUG 10 2013 105
LETTERS
Figs 1-2 An engineers home-made
precious splint
Fig. 3 The OPG revealed a retained root and
the splints frmly secured in place
2013 Macmillan Publishers Limited. All rights reserved.
Das könnte Ihnen auch gefallen
- Salivary Glands DisordersDokument7 SeitenSalivary Glands DisordersAhmad AssariNoch keine Bewertungen
- An Overview of The Surgical Correction of Dentofacial DeformityDokument9 SeitenAn Overview of The Surgical Correction of Dentofacial DeformityAhmad AssariNoch keine Bewertungen
- Genetic and Environmental Factors of Dentofacial DeformitiesDokument7 SeitenGenetic and Environmental Factors of Dentofacial DeformitiesAhmad AssariNoch keine Bewertungen
- Untreated Dentofacial DeformitiesDokument1 SeiteUntreated Dentofacial DeformitiesAhmad AssariNoch keine Bewertungen
- UntitledDokument5 SeitenUntitledBunga Erlita RosaliaNoch keine Bewertungen
- The Prevalence of Tooth Wear in UKDokument6 SeitenThe Prevalence of Tooth Wear in UKAhmad AssariNoch keine Bewertungen
- The Coronal Flap Surgical TechniqueDokument7 SeitenThe Coronal Flap Surgical TechniqueAhmad AssariNoch keine Bewertungen
- 114 PDFDokument3 Seiten114 PDFAhmad AssariNoch keine Bewertungen
- CDHO Factsheet Multiple SclerosisDokument4 SeitenCDHO Factsheet Multiple SclerosisAhmad AssariNoch keine Bewertungen
- Lect 4 ChisqDokument22 SeitenLect 4 ChisqnirajmishraNoch keine Bewertungen
- Parent's AttitudeDokument5 SeitenParent's AttitudeAhmad AssariNoch keine Bewertungen
- Parent's AttitudeDokument5 SeitenParent's AttitudeAhmad AssariNoch keine Bewertungen
- Dental Clinics of North America Volume 54 Issue 3 2010 (Doi 10.1016/j.cden.2010.03.003) Xiaojie Wang Adrian Lussi - Assessment and Management of Dental Erosion PDFDokument14 SeitenDental Clinics of North America Volume 54 Issue 3 2010 (Doi 10.1016/j.cden.2010.03.003) Xiaojie Wang Adrian Lussi - Assessment and Management of Dental Erosion PDFAhmad AssariNoch keine Bewertungen
- 114 PDFDokument3 Seiten114 PDFAhmad AssariNoch keine Bewertungen
- Parent's AttitudeDokument5 SeitenParent's AttitudeAhmad AssariNoch keine Bewertungen
- Lipski AnatomyDokument8 SeitenLipski AnatomyAhmad AssariNoch keine Bewertungen
- Zanette SAADD2011Dokument8 SeitenZanette SAADD2011Ahmad AssariNoch keine Bewertungen
- I0003 3006 59 2 90 PDFDokument13 SeitenI0003 3006 59 2 90 PDFAhmad AssariNoch keine Bewertungen
- Reed, K, 2012Dokument11 SeitenReed, K, 2012Felipe LarraínNoch keine Bewertungen
- Cronbachs AlphaDokument3 SeitenCronbachs AlphaAndrew AndersonNoch keine Bewertungen
- I0003 3006 59 2 90 PDFDokument13 SeitenI0003 3006 59 2 90 PDFAhmad AssariNoch keine Bewertungen
- I0003 3006 59 2 90 PDFDokument13 SeitenI0003 3006 59 2 90 PDFAhmad AssariNoch keine Bewertungen
- Multiple Sclerosis ManifestationsDokument5 SeitenMultiple Sclerosis ManifestationsAhmad AssariNoch keine Bewertungen
- An Update On Local Anesthetics in Dentistry DR HaasDokument6 SeitenAn Update On Local Anesthetics in Dentistry DR HaasdeenmNoch keine Bewertungen
- Tooth EruptionDokument3 SeitenTooth EruptionAhmad AssariNoch keine Bewertungen
- A New Classification of Endodontic-Periodontal LesionsDokument5 SeitenA New Classification of Endodontic-Periodontal LesionsAhmad AssariNoch keine Bewertungen
- Multiple Sclerosis Oral HealthDokument16 SeitenMultiple Sclerosis Oral HealthAhmad AssariNoch keine Bewertungen
- Materiale Ceramice in StomatologieDokument23 SeitenMateriale Ceramice in StomatologieMogos PaulNoch keine Bewertungen
- Effect of Bleaching On Restorative Materials and Restorations-A Systematic ReviewDokument10 SeitenEffect of Bleaching On Restorative Materials and Restorations-A Systematic ReviewAhmad AssariNoch keine Bewertungen
- A SEM Evaluation of A 6% Hydrogen Peroxide Tooth Whitening Gel On Dental Materials in VitroDokument5 SeitenA SEM Evaluation of A 6% Hydrogen Peroxide Tooth Whitening Gel On Dental Materials in VitroAhmad AssariNoch keine Bewertungen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Client - Assessment - Record vw430vDokument11 SeitenClient - Assessment - Record vw430vjulianNoch keine Bewertungen
- Antibiotics Chart 2Dokument10 SeitenAntibiotics Chart 2Vee MendNoch keine Bewertungen
- An Essay On Yoga and HealthDokument2 SeitenAn Essay On Yoga and HealthGentleStrength100% (1)
- Dharam Pani Pandey, Dr. Uday Shankar Sharma, Dr. Ram Babu. Electrical Muscle Stimulation (EMS) Improve Functional Independence in Critically Ill PatientsDokument8 SeitenDharam Pani Pandey, Dr. Uday Shankar Sharma, Dr. Ram Babu. Electrical Muscle Stimulation (EMS) Improve Functional Independence in Critically Ill PatientsDr. Krishna N. SharmaNoch keine Bewertungen
- Case Presentation On Chronic Kidney Disease1Dokument18 SeitenCase Presentation On Chronic Kidney Disease1d100% (1)
- Paediatric Emergencies2Dokument244 SeitenPaediatric Emergencies2Amber MonroeNoch keine Bewertungen
- Quiz 12 AnswersDokument3 SeitenQuiz 12 AnswersAllah YarNoch keine Bewertungen
- Aceclofenac Efficacy and Safety Vs DiclofenacDokument6 SeitenAceclofenac Efficacy and Safety Vs DiclofenacpdelaxNoch keine Bewertungen
- Circuit Weight Training in Cardiac PatientsDokument5 SeitenCircuit Weight Training in Cardiac PatientsVivin YulvinaNoch keine Bewertungen
- Taenia Saginata: (Taeniarhynchus Saginatus) Beef TapewormDokument12 SeitenTaenia Saginata: (Taeniarhynchus Saginatus) Beef TapewormIsabelle Hazel BenemileNoch keine Bewertungen
- Fast Food EssayDokument5 SeitenFast Food Essayapi-242285238Noch keine Bewertungen
- EXO-Notes JBC ENTEROBACTERIACEAEDokument70 SeitenEXO-Notes JBC ENTEROBACTERIACEAECha Tangan-PenolNoch keine Bewertungen
- HAAD Test 4 QuestionsDokument17 SeitenHAAD Test 4 QuestionsPhine PhineNoch keine Bewertungen
- 2013 Afphm Oral Exam - Sample QuestionsDokument14 Seiten2013 Afphm Oral Exam - Sample QuestionsCaity YoungNoch keine Bewertungen
- Acute GastroenteritisDokument63 SeitenAcute GastroenteritisSathya MoorthyNoch keine Bewertungen
- CR ViewerDokument2 SeitenCR ViewerJehan ZebNoch keine Bewertungen
- Section D Day 2 Shift: 7:00 AM - 3:00 PM January 12, 2019: College of Health Sciences Marawi CityDokument3 SeitenSection D Day 2 Shift: 7:00 AM - 3:00 PM January 12, 2019: College of Health Sciences Marawi CityMiyuki Bartolaba MangondatoNoch keine Bewertungen
- Flavonoids Analgesic AgentDokument17 SeitenFlavonoids Analgesic AgentStella AguirreNoch keine Bewertungen
- Depression, Postpartum and Obstetric Social PsychologyDokument14 SeitenDepression, Postpartum and Obstetric Social PsychologyNurul AiniNoch keine Bewertungen
- Mastoiditis Treatment & ManagementDokument10 SeitenMastoiditis Treatment & ManagementIvan PathfinderNoch keine Bewertungen
- Introduction To ParasitologyDokument73 SeitenIntroduction To ParasitologyKarylle CateNoch keine Bewertungen
- Differential Diagnosis of Genital Ulcer Differential Diagnosis of Genital UlcersDokument3 SeitenDifferential Diagnosis of Genital Ulcer Differential Diagnosis of Genital UlcersNurhayati HasanahNoch keine Bewertungen
- Staph Is Short For StaphylococcusDokument12 SeitenStaph Is Short For Staphylococcusdel rosarioNoch keine Bewertungen
- Final MBBS Part 1 Classes Schedule - Live UpdateDokument6 SeitenFinal MBBS Part 1 Classes Schedule - Live UpdateKrishna VamsiNoch keine Bewertungen
- Nutrition Chapter 1-5Dokument49 SeitenNutrition Chapter 1-5Maria MarieNoch keine Bewertungen
- Interorient Maritime Enterpriseces, Inc. Vs CreerDokument11 SeitenInterorient Maritime Enterpriseces, Inc. Vs CreerStef OcsalevNoch keine Bewertungen
- Penyakit Kulit Dan KelaminDokument97 SeitenPenyakit Kulit Dan KelaminSelvi Putri Oktari100% (1)
- Kuesioner MNSI PDFDokument2 SeitenKuesioner MNSI PDFvithaa_100% (1)
- Third Degree Block After Mi........ Observe The PatientDokument23 SeitenThird Degree Block After Mi........ Observe The PatientSunn Ren TeeNoch keine Bewertungen
- Diabetes A Public Health Issue For The Twentyfirst CenturyDokument4 SeitenDiabetes A Public Health Issue For The Twentyfirst CenturyLight YagamiNoch keine Bewertungen