Beruflich Dokumente
Kultur Dokumente
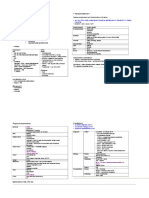
CVS Drug Revision Notes (6 Pages Only)
Hochgeladen von
drusmansaleem0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
93 Ansichten6 Seitenvery short cvs drugs
Copyright
© © All Rights Reserved
Verfügbare Formate
PDF, TXT oder online auf Scribd lesen
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenvery short cvs drugs
Copyright:
© All Rights Reserved
Verfügbare Formate
Als PDF, TXT herunterladen oder online auf Scribd lesen
0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
93 Ansichten6 SeitenCVS Drug Revision Notes (6 Pages Only)
Hochgeladen von
drusmansaleemvery short cvs drugs
Copyright:
© All Rights Reserved
Verfügbare Formate
Als PDF, TXT herunterladen oder online auf Scribd lesen
Sie sind auf Seite 1von 6
CARDIOVASCULAR DRUGS
DRUGS USED IN HYPERTENSION
Diuretics
Thiazides Mild hypertension
Loop Diuretics Moderate, Severe and Malignant HPN
Sympathoplegics
Alpha 2 selective agonists
(Clonidine, Methlydopa)
Decrease in sympathetic outflow
Methyldopa Methyl NE in brain
Major compensatory response:
salt retention
Toxicity
Sudden discontinuation of clonidine: Rebound Hypertension
- Reinstitute clonidine therapy
- Give alpha blockers (Phentolamine)
Methyldopa causes hematologic immunotoxicity (+ Coombs)
Methyldopa causes more sedation than clonidine
Ganglion Blocking Drugs
Nicotinic blockers: obsolete due to AE
Hexamethonium
Trimethaphan
Extremely powerful blood pressure-
lowering drugs
Major compensatory response:
salt retention
Toxicity: parasympathetic blockade
-blurred vision, constipation, hesitancy, sexual dysfunction
- sympathetic blockade: sexual dysfunction, orthostatic hypotension
Postganglionic Sympathetic Nerve Terminal Blockers
Reserpine:
depelete NE stores at adrenergic
nerve terminal
Guanethidine:
block release of NE stores
Major compensatory response:
salt retention
Reserpine: penetrates CNS
Both have long duration of action
Toxicity
Reserpine: behavioral depression (most serious)
Guanethedine: sexual dysfunction, orthostatic hypotension
MAO inhibitors:
Form false transmitter
(octopamine)
Decreased vascular responses
(less NE with octopamine)
Large doses of indirect acting sympathomimetics (tyramine) may result
in hypertensive crisis MAO inh no longer used for HPN
Adrenoceptor Blockers
Alpha 1 selective agents
(Prazosin)
Reduce vascular resistance and
venous return
Beta blockers
(Propranolol)
Initially reduce CO
Decrease vacular resistance
(reduced angiotensin levels due
to reduced renin release)
Nonselective alpha blockers of no use: d/t compensatory tachycardia
Beta blockers: slightly elevated glucose, LDL, TG
Vasodilators
- Act directly on smooth muscle cells through non
autonomic mechanisms
- Mechanisms
o Release of NO
o Open K channels : hyperpolarization
o Block Ca channels
o Activate D1 receptors
- Marked compensatory mechanisms
o Minoxidil and Hydralazine
o Salt retention and tachycardia
Hydralazine:
acts on the release of NO from
endothelial cells
- Effect on arterioles > veins
- Suitable for chronic therapy
Toxicity
- Compensatory responses: salt retention, tachycardia
- Drug-induced SLE (reversible, increased risk if dose >200mg/d)
Minoxidil:
-Converted to active Minoxidil
sulfate (K channel opener)
- hyperpolarization
- Severe hypertension
-
Toxicity
- Compensatory responses
- Hirsutism
- Pericardial abnormalities
Calcium Channel Blocking Agents
Nifedipine
Verapamil
Diltiazem
- Effective vasodilators
- Suitable for chronic use in any
severity of HPN
- Fewer compensatory response
Parenteral vasodilators ( used in hypertensive emergencies)
Nitroprusside:
Release of NO
- Short acting
- infused continuously
Toxicity
- Excessive hypotension, tachycardia
- Accumulationof cyanide or thiocynate if infusion continued
over days
Diazoxide:
Open K channels
Hyperpolarization
-IV or bolus
-duration of action: hours
-also reduces insulin release (can be
treated for hypoglycemia from insulin
secreting tumors)
Toxicity
- Hypotension
- Hyperglycemia
- Salt and water retention
Fenoldepam:
D1 receptor activation
- Prompt marked arteriolar
vasodilation
- IV infusion
- Short duration of action
Angiotensin Antagonists
ACE inhibitors:
Inhibit angiontensin-
converting enzyme,
kininase II and peptidyl
dipeptidase
- More extensively used
- Reduced blood levels of A-II
and aldosterone
- Increase in bradykinin
- Protect diabetic kidney
- CI in pregnancy
By Usman Ali Akbar
Captopril
Adverse Effects
- Minimal compensatory response
- Cough (30% of patients)
- Renal damage with preexisting vascular disease
- Renal damage in fetus
Angiotensin II blockers:
Competitively inhibit A-II at
its AT1 receptor site
Losartan
- Reduce aldosterone
levels
- Cause K retention
- CI in pregnancy
Adverse Effects
- Lower incidence of cough
- Fetal renal toxicity
Clinical Uses
Usual stepwise treatment of HPN:
1) Lifestyle measures
2) Diuretics
3) Sympathoplegics usually B blocker first
4) ACE inhibitors
5) Vasodilators usually Ca channel blocker first
Malignant Hypertension
- Accelerated phase of severe hypertension
- Rising blood pressure and rapidly progressing organ
damage
- Managed with powerful vasodilators (nitroprusside,
fenoldopam or diazoxide) with diuretics (furosemide) and
B blockers
- Lower BP to 140-160/90-110 within few hours
CARDIOVASCULAR DRUGS
DRUGS USED FOR ANGINA PECTORIS
Types of Angina
Atherosclerotic
-classic angina
-angina of effort
- atheromatous plaques that partially
occlude coronaries
- rest leads to relief of pain within 5-15
minutes
- 90% of angina cases
Vasospastic
-rest angina, variant angina
- Prinzmetals angina
- reversible spasm of coronaries
-occur at any time
Unstable
-crescendo angina
-acute coronary syndrome
-increased frequency and severity of
attacks
-immediate precursor of MI
-medical emergency
Determinants of Cardiac Oxygen Requirement
- Major determinant: myocardial fiber tension
(higher tension, higher O2 requirement)
Preload (diastolic filling
pressure)
Function of blood volume and venous tone
Afterload Determined by arterial BP and large artery
stiffness
Heart rate Time-integrated fiber tension
(faster HR, more time at systolic)
Double product: SBP x HR
Cardiac contractility Controlled by sympathetic outflow
Ejection time Inversely related to force of contraction
Increased Ejection time, increase O2
requirement
Therapeutic strategies
-defect: inadequate coronary O2 delivery relative to O2 requirement
- Increase O2 delivery
- Decrease O2 requirement
Drugs that reduce O2 Requirement
Nitrates
-release NO (inc cGMP)
- Reduced preload, CO,
afterload
-increase coronary flow via
collaterals
-reduce vasospasm
Venodilation
-Decreased diastolic heart size
and fiber tension
Arteriolar dilation
-dec PR and BP
- Smooth muscle relaxation
- Most sensitive:
Veins > arteries>
arterioles
- Rapidly denatured in liver
and smooth muscle (large
first pass effect 90%)
- Vasodilating effect:
Dinitrate> mononitrate
Adverse Effects
- Reflex tachycardia
- Increased force of contraction
Toxicity
- Most common: reflex tachycardia, orthostatic
hypotension
- Headache from meningeal artery vasodilation
By Usman Ali Akbar
- Interact with Sildenafil (potentially dangerous
hypotension)
- Cause methemoglobinemia at high blood
concentration
- Monday disease: headache, tachycardia, dizziness
Other forms
- Nitroglycerin: most important
Range of duration of action
10-20 min (sublingual)
8-10 hr (transdermal)
IV nitroglycerin: reduce platelet aggregation
- Isosorbide dinitrate
- Isosorbide mononitrate
- Amyl nitrate: volatile, inhalatational
Nitrites in the treatment of Cyanide Poisoning
- Immediate exposure to amyl nitrite
- IV Na nitrite: increase methemoglobin level
- IV Na thiosulfate: convert cyanomethemoglobin to
thiocynate and methemoglobin
Ca channel Blocking Drugs (Nifedipine, Diltiazem, Verapamil)
- Block voltage gated L
type Ca Channels
- Decrease Ca influx,
reduce muscle
contractility
- All are orally active
- Nifedipine: greater
vasodilation
- Reduce BP and double
product
Clinical Use
- Prophylactic (Nifedipine abort acute angina attacks)
- Nimodipine: approved only for stroke associated with SAH
- Verapamil, Diltiazem: AV nodal arrhythmias
Toxicity
- Constipation, pretibial edema
- Nausea, flushing, dizziness
- Bepridil: greater CV toxicity than other Ca channel blockers
(torsades pointe)
- Verapamil: AV block, sinus node depression
B Blocking Drugs
- decrease HR, BP, cardiac
force
-reduce the double product
-effective in prophylaxis of
atherosclerotic anginas
-used only for prophylactic
therapy of angina, no value in
acute attack
-prevent exercise-induced
angina, no effect in vasospastic
form
Summary
Nitrates - Useful in all 3 types of angina
Ca blockers - Treatment for angina of effort and vasospastic
angina
B blockers - Refractory unstable angina
- Prophylaxis of angina of effort
- Not useful for vasospastic angina
- Not useful for acute attack of angina of effort
- Emergency treatment of acute coronary
syndrome
CARDIOVASCULAR DRUGS
DRUGS USED IN HEART FAILURE
Cardiac Glycosides
Digitalis
-foxglove plant
Digoxin (P)
MOA:
- inhibition of Na/K ATPase
-increase intracellular Ca
- Steroid nucleus and lactone ring
- Increased ventricular ejection
- Increased renal perfusion
- Decreased CO
- Decreased preload, afterload, HR
Clinical Uses
- Traditional positive inotropic agent used in CHF
- Improves functional status but does not prolong life
- Atrial fibrillation and Atrial Flutter
-reduce the conduction velocity
-increase the refractory period of AV node
-ventricular rate is controlled with efficient filling and ejection
Interactions
- Quinidine : reduction in digoxin clearance
- Extracellular K and Mg: inhibit digitalis effect
-loop diuretics may precipitate digitalis toxicity
- Extracellular Ca: facilitate digitalis effect
Digitalis toxicity
- Arrhythmias most serious manifestation
- Nausea, vomiting, Diarrhea
- Chronic intoxication: Ca overload ( increased automaticity)
- Treatment
-correct K or Mg deficiency (not for acute toxicity)
-antiarrhythmic drugs (not for acute toxicity) - Lidocaine
-Digoxin antibodies
Other Drugs used in Heart Failure
Diuretics
Furosemide - Immediate reduction of pulmonary
congestion and severe edema
Thiazides - Mild chronic failure
Spironolactone/ Epleronone - Long term benfits
Angiontensin Antagonists
- reduce morbidity and mortality in CHF
-no direct positive inotropic action
-reduce aldosterone secretion, salt and water retention and vascular
resistance
Beta 1 Selective Adrenoceptor Agonists
Dobutamine - Acute heart failure
- Not appropriate for CHF
(tolerance, lack of oral efficacy, arrhthmogenic effects)
Dopamine
Beta Adrenoceptor Antagonists
Carvedilol, Labetalol,
Metoprolol
- Reduce progression of CHF
- No value in acute heart failure
Phosphodiesterase Inhibitors
Amrinone and Milrinone - Increase cAMP, Increase in intracellular Ca
- Vasodilation
- Not used in CHF
Vasodilators
Nitroprusside - Acute severe failure with congestion
- Reduced cardiac size, reduced resistance to ventricular
ejection
Nitroglycerin
Nesiritide - Vasodilation
- Natriuretic effects
- For acute failure only
By Usman Ali Akbar
Hydralazine - Chronic Heart Failure
ISDN
ARDIOVASCULAR DRUGS
ANTI ARRHYTHMIC DRUGS
Normal Electrical Activity in Cardiac Cell
Na current - Dominates the upstroke of the action potential phase
(Phase 0)in most parts of heart
- Most important determinant of conduction of AP
Ca current - Dominates in the AV node
- Plateau of phase 2
K current - Rapid repolarization
Refractory
period
- Function of rapidly Na channels recover from inactivation
Drug Class
Class I - Sodium channel blockers
Class II - Beta adrenoceptor blockers
Class III - Potassium channel blockers
Class IV - Calcium channel blockers
Class I Antiarrhythmics (Local Anesthetics)
-MOA: slow or block conduction
- slow or abolish abnormal pacemakers
- use dependent or state dependent in their action
-reduce both phase O and phase 4 Na currents
IA: Procainamide (P)
Quinidine, Disopyramide
- Block Na
- Prolong the AP (block
K), increase effective
refractory period
Increase in QT interval
- All types of arrhythmias
- Affect both atrial and ventricular
arrhythmias
- Also block K channels (phase 3)
- Slow conduction velocity
- Slow AV conduction (high dose)
- Increased QRS duration on ECG
- Commonly used in acute phase of MI
(Procainamide)
Toxicity
- All may precipitate new arrhythmias
- Torsades pointes (particularly quinidine, except amiodarone)
- Hyperkalemia: exacerbates toxicity
-Na lactate: given to reverse drug induced arrhythmias
-Sympathomimetics: to reverse drug induced hypotension
Procainamide
- Hypotension
- Induces Lupus like / SLE reaction
Quinidine
- Cinchonism (headache, vertigo, tinnitus)
- Cardiac depression, GI upset (diarrhea)
- Autoimmune reactions (thrombocytopenia)
- Reduce digoxin clearance, increase serum digoxin
Disopyramide
- Antimuscarinic effects, precipitate HF
IB: Lidocaine (P)
Mexiletine, Tocainide
- Shorten the AP
- does not shorten effective
refractory period or increase
contractility
- -ventricular > atrial
- Atrial arrhythmias not
responsive unless caused by
digitalis
- No significant effect on ECG
- Prefer ischemic tissues (for
post MI)
- reduces abnormal automaticity
Toxicity
- May precipitate arrhythmias (less than IA)
- Hyperkalemia increase cardiac toxicity
- Tocainide: agranulocytosis
IC: Flecainide (P)
Encainide, Moricizine, Propafenone
- No effect on AP duration or QT
interval
- Powerful depressants of Na
current
- Approved only for refractory
ventricular tachycardias and
intractable SVT
- Markedly slow conduction
velocity
- Increase QRS duration on ECG
Toxicity
-proarrhythmic effect (more likely to exacerbate or precipitate
arrhythmias) CAST Trial
-restricted to use in arrhythmias that fail to respond to other drugs
-contraindicated for post MI
Amiodarone: Class III drug with IA effects, greatest AP prolonging effect
Phenytoin: reverse digitalis induced arrhythmias, classified with IB
Class II Antiarrhythmics (Beta Blockers)
- -MOA: B adrenoceptor blockade
Reduction in cAMP, Na and Ca currents
No effect in AP
- AV node is particularly sensitive to B blockers
- PR interval prolonged
Esmolol (P) - Short acting B blocker
- Used exclusively in acute arrhythmias
Propranolol (P), Timolol,
Metoprolol
- Prophylactic drugs in patients who have
MI
- Protective effect (2 years or longer after
infarct)
Toxicity
- Patients with arrhythmias more prone to B blocker induced
depression of cardiac output
- Judicious use: reduces progression of CHF, reduce incidence
of potentially fatal arrhythmias
Class III Antiarrhythmics (K Channel Blockers)
-Hallmark: prolongation of AP duration
-due to blockade of phase 3 K channels
-reduce outward phase 3 K current
-main effect: prolong refractory period
-same toxicity as in Class IA
-eliminated in tears
-phase 4 K current NOT affected
-increase QT interval on ECG
Sotalol (P) - Chiral compound
Toxicity
- May precipitate torsade pointes, B blockade (sinus
bradycardia or asthma)
Ibutilide (P), Dofetilide - Atrial flutter, atrial fibrillation
Toxicity: induction of torsade de pointes
Amiodarone
-most efficacious among
antiarrhythmic drugs
-blocks Na, K, Ca channels
and B adrenoceptors
- Markedly prolongs AP, block Na
channels
- Only for arrhythmias resistant to other
drugs
- Cyp inhibitor (ex. increase
antithrombotic effects of warfarin)
Toxicity:
- Microcrystalline deposits in cornea and skin
- Thyroid dysfunction
- Paresthesias, tremor
By Usman Ali Akbar
- Pulmonary fibrosis
- Rarely cause new arrhythmias
Bretylium
-used only in the
treatment of refractory
post MI arrhythmias
(recurrent VFib)
- Combines general sympathoplegic
with K channel blocking effect in
ischemic tissue
- Acts on ischemic cells, little change on
ECG
- May precipitate new arrhythmias or marked hypotension
Class IV Antiarrhythmics (Ca Channel Blockers)
-state and use dependent selective depression of Ca current in tissues
that require L type ca channels
-converting AV nodal reentry to NSR (nodal arrhythmias)
- decrease conduction velocity at AV node
- increased ERP (refractoriness prolonged)
- increased PR interval (consistently)
-reduce inward calcium current during AP and phase 4
Verapamil (P) - Major toxicity: excessive
pharmacologic effect
- Contractility, AV conduction, blood
pressure depressed
- Nifedipine and other dihydropyridines not useful as antiarrhythmic
due to compensatory sympathetic discharge
Miscellaneous Antiarrhythmic Drugs
Adenosine
- slows or completely blocks conduction in the AV node
- activates Ik1 K channels in AV node (hyperpolarize)
- effective in abolishing AV nodal arrhythmias (DOC)
- short duration of action (15s)
- only antiarrhythmic drug that consistently alters the resting
potential of AV node
Toxicity:
- flushing and hypotension
- chest pain and dyspnea
- overcome by short duration of action
Digitalis
- treatment of rapid atrial or AV nodal arrhythmias
- slows AV conduction in atrial flutter or fibrillation
Potassium Ion
- depresses ectopic pacemakers including those caused by
digitalis toxicity
Magnesium Ion
- similar effects as potassium on digitalis-induced
arrhythmias
Nonpharmacologic Treatment of Arrhythmias
- External defibrillation
- Implanted defibrillators
- Implanted pacemakers
- Radiofrequency ablation of arrhythmogenic foci
CARDIOVASCULAR DRUGS
DIURETIC AGENTS
-most enter in luminal end (except aldosterone receptor antagonist who
enter from the basolateralside)
Proximal
Convoluted Tubule
- Reabsorption of AA, glucose and cations
- Major site of NaCl and NaHCO3
- 60-70% of total reabsorption of Na
- Weak acid transport: most in S2 segment
- Weak base: transported in S1 and S2
- Transport of uric acid
- Target of carbonic anhydrase inhibitors
Thick Ascending
Loop of Henle
- Pumps Na, K, Cl out of the lumen into the interstitial
of kidney
- Major site of Ca and Mg reabsorption
-due to net positive selective channel
- Na-K-Cl transporter: 20-30% of reabsorption of
sodium (gradient for counter current concentrating
mechanism)
--target of Loop diuretics
Distal Convoluted
Tubule
- 5-8% of Na reabsorption
- NaCl active transport: target of thiazide diuretics
- PTH mediated Ca reabsorption
Cortical Collecting
Tubule
- 2-5% of Na reabsorption via Na channels
- Controlled by aldosterone
- Primary site of acidification of urine
- Primary site of K excretion
- Site of K sparing diuretics
Medullary
Collecting Tubule
- Water reabsorption (ADH mediated)
Carbonic Anhydrase Inhibitors
Acetazolamide (P)
MOA: inhibit carbonic
anhydrase (brush border) and
intracellular carbonic
anhydrase in PCT
- Major renal effect:
bicarbonate diuresis
metabolic acidosis
- Significant K wasting
- Sulfonamide derivatives
- Self-limiting within 2-3 days
- treatment of glaucoma :
reduce IOP
- prevent acute mountain sickness
acidosis in CSF results in
hyperventilation which can protect
mountain sickness
- only used as a diuretic if edema is
accompanied by significant metabolic
acidosis
Toxicity
- drowsiness and paresthesia
- alkalinization of urine may cause precipitation of Ca salts and form
renal stones
- marked renal K wasting
- hepatic encephalopathy in patients with hepatic impairment
(increased ammonia reabsorption)
Loop Diuretics
Furosemide (P)
MOA: inhibit cotransport of
Na, K and Cl
Bumetanide, Torsemide
- Significant increase of Ca
excretion
- Significant K wasting
- Proton excretion
- sulfonamide derivatives
- Ethacrynic Acid: phenoxyacetic
acid derivative
- Relatively short acting
- Diluting ability of nephron is
reduced
- Loss of lumen-positive potential
(reduce reabsorption of cations)
- Inhibition of prostaglandin
synthesis (NSAIDS) decreases
efficiency of loop diuretics
By Usman Ali Akbar
- Hypokalemic alkalosis - Treatment of edematous states
- Acute pulmonary edema
(pulmonary vasodilating action)
- Treatment of severe
hypercalcemia
Toxicity:
- Hypokalemic metabolic alkalosis
- Hypovolemia
- Ototoxicity
Thiazide Diuretics
Hydrochlorthiazide (P)
MOA: inhibit NaCl transport in
DCT
-moderate but sustained Na
and Cl diuresis
-hypokalemic metabolic
alkalosis
- increased Ca reabsorption
- Sulfonamide derivatives
- Longer duration of action than
loop diuretics
- Dilutionalhyponatremia
- Major application in HPN
- Can be used for chronic renal
calcium stone formation (reduce
urine Ca concentration)
Toxicity
- Massive sodium diuresis with hyponatremia
- Chronic therapy: K wasting
- Significant hyperglycemia in diabetic patients
Synergistic effect with loop diuretics
K sparing Diuretics
-increase in Na clearance
-decrease in K and H ion excretion
-cause hyperkalemic metabolic acidosis
Spironolactone - Steroid derivatives
- Pharmacologic antagonists of
aldosterone in collecting tubules
- Reduce gene expression
controlling Na ion channel
synthesis
Epleronone
Amiloride - Block Na channels
Triamterene
Clinical Uses
- Indicated in aldosteronisms
- Spironolactone and Epleronone: long term effects in HF
Toxicity
- Hyperkalemia (most important)
- Never be given with K supplements
- Caution with use of ACE inhibitors and ARBS
- Spironolactone: gynecomastia, antiandrogenic effects
Osmotic Diuretics
-increased volume of urine
-increased Na excretion
Mannitol (P)
Glycerin, Isosorbide, Urea
- Given IV
- Holds water by virtue of isosmotic
effect
- Major location : PCT
- Reduce brain volume/ ICP
- Useful in acute glaucoma and in
neurologic conditions (reduce
ICP)
Toxicity
- Hyponatremia and pulmonary edema
- Headache, nausea and vomiting
Antidiuretic Hormone Agonists and Antagonists
ADH agonists
ADH and Desmopressin (P) - Peptides , IV
- Reduce urine volume
- Increase urine concentration
- Useful in pituitary diabetes
insipidus
Toxicity
- Dangerous hyponatremia
- Large doses, hypertension
ADH antagonists
Demeclocycline and Lithium
ion
- Oral
- Demeclocycline : Useful for
SIADH
Toxicity
- Lithium with greater toxicity
- Lithium : cause nephrogenic diabetes insipidus (never used
to treat SIADH
- Demeclocycline in Children <8: bone and teeth
abnormalities
By Usman Ali Akbar
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Urinary Tract Infection & PyelonephritisDokument3 SeitenUrinary Tract Infection & PyelonephritisUsman Ali AkbarNoch keine Bewertungen
- Obstructive Airway Disease: Dr. Khalid Al-Mobaireek King Khalid University HospitalDokument53 SeitenObstructive Airway Disease: Dr. Khalid Al-Mobaireek King Khalid University HospitalUsman Ali AkbarNoch keine Bewertungen
- Polycystic Kidneys: Adult PKD: ComplicationsDokument1 SeitePolycystic Kidneys: Adult PKD: ComplicationsUsman Ali AkbarNoch keine Bewertungen
- Chronic Renal Failure: Concise Long Case ApproachDokument3 SeitenChronic Renal Failure: Concise Long Case ApproachUsman Ali AkbarNoch keine Bewertungen
- Renal Tubular Acidosis Summary - AdjDokument1 SeiteRenal Tubular Acidosis Summary - AdjUsman Ali AkbarNoch keine Bewertungen
- DialysisDokument2 SeitenDialysisUsman Ali AkbarNoch keine Bewertungen
- King Khalid University Hospital Department of Obstetrics & Gyncology Course 481Dokument40 SeitenKing Khalid University Hospital Department of Obstetrics & Gyncology Course 481Usman Ali AkbarNoch keine Bewertungen
- Recurrent Nausea Andor VomitingDokument8 SeitenRecurrent Nausea Andor VomitingUsman Ali AkbarNoch keine Bewertungen
- GI Bleeding Team Work - 2nd EditionDokument9 SeitenGI Bleeding Team Work - 2nd EditionUsman Ali AkbarNoch keine Bewertungen
- Anaemia in PregnancyDokument13 SeitenAnaemia in PregnancyUsman Ali AkbarNoch keine Bewertungen
- Recurrent VomitingDokument16 SeitenRecurrent VomitingUsman Ali AkbarNoch keine Bewertungen
- Alas!! EmpytinessDokument2 SeitenAlas!! EmpytinessUsman Ali AkbarNoch keine Bewertungen
- Organophosphate PoisoningDokument23 SeitenOrganophosphate PoisoningUsman Ali AkbarNoch keine Bewertungen
- Cord ProlapseDokument2 SeitenCord ProlapseUsman Ali AkbarNoch keine Bewertungen
- Subject: Permission For Badminton Court NID, Multan: TH THDokument1 SeiteSubject: Permission For Badminton Court NID, Multan: TH THUsman Ali AkbarNoch keine Bewertungen
- DR Othman Alharbi, MBBS FRCPC Assistance Professor & Consultant Gastroenterology College of Medicine King Saud UniversityDokument18 SeitenDR Othman Alharbi, MBBS FRCPC Assistance Professor & Consultant Gastroenterology College of Medicine King Saud UniversityUsman Ali AkbarNoch keine Bewertungen
- GRAM NEGATIVE RODS (5) Fastidious Organisms From Animal Sources (A)Dokument1 SeiteGRAM NEGATIVE RODS (5) Fastidious Organisms From Animal Sources (A)Usman Ali AkbarNoch keine Bewertungen
- Untold Stanza... : - Nasim Alam (N-61)Dokument1 SeiteUntold Stanza... : - Nasim Alam (N-61)Usman Ali AkbarNoch keine Bewertungen
- Through The Strange WindsDokument5 SeitenThrough The Strange WindsUsman Ali AkbarNoch keine Bewertungen
- Lect 1:: M2Pasysl21 Urinary SystemDokument4 SeitenLect 1:: M2Pasysl21 Urinary SystemUsman Ali AkbarNoch keine Bewertungen
- When Hope DiesDokument2 SeitenWhen Hope DiesUsman Ali AkbarNoch keine Bewertungen
- Death and The Mother For MergeDokument4 SeitenDeath and The Mother For MergeUsman Ali AkbarNoch keine Bewertungen