Beruflich Dokumente
Kultur Dokumente
Beta Blockers and Asthma
Hochgeladen von
AzmachamberAzmacareCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Beta Blockers and Asthma
Hochgeladen von
AzmachamberAzmacareCopyright:
Verfügbare Formate
CHEST Original Research
ASTHMA
journal.publications.chestnet.org CHEST / 145 / 4 / APRIL 2014 779
striction.
2
These concerns may largely relate to adverse
events occurring in patients with uncontrolled asthma
before widespread use of inhaled corticosteroids.
As such, b -blockers are withheld from patients with
asthma despite strong clinical indications.
Only selective b -blockers have previously been
sys tematically evaluated in patients with reversible
airways disease (asthma and COPD), where single-
dose exposure reportedly caused a mean fall in FEV
1
G
uidelines recommend avoiding b -blockade in
patients with asthma because of concerns regard-
ing the potential for acute bronchoconstriction.
1
This
is caused by catecholamine antagonism at the pulmo-
nary b
2
-adrenocepter, which may uncover unopposed
increased cholinergic tone resulting in airway con-
Background: b -Blockers are avoided in asthma over concerns regarding acute bronchoconstric-
tion. Risk is greatest following acute exposure, including the potential for antagonism of b
2
-agonist
rescue therapy.
Methods: A systematic review of databases was performed to identify all randomized, blinded,
placebo-controlled clinical trials evaluating acute b -blocker exposure in asthma. Effect estimates
for changes in respiratory function, symptoms, and b
2
-agonist response were pooled using random
effects meta-analysis with heterogeneity investigated.
Results: Acute selective b -blockers in the doses given caused a mean change in FEV
1
of 2 6.9%
(95% CI, 2 8.5 to 2 5.2), a fall in FEV
1
of 20% in one in eight patients ( P 5 .03), symptoms affect-
ing one in 33 patients ( P 5 .18), and attenuation of concomitant b
2
-agonist response of 2 10.2%
(95% CI, 2 14.0 to 2 6.4). Corresponding values for acute nonselective b -blockers in the doses
given were 2 10.2% (95% CI, 2 14.7 to 2 5.6), one in nine patients ( P 5 .02), one in 13 patients
( P 5 .14), and 2 20.0% (95% CI, 2 29.4 to 2 10.7). Following investigation of heterogeneity, clear
differences were found for celiprolol and labetalol. A dose-response relationship was demon-
strated for selective b -blockers.
Conclusions: Selective b -blockers are better tolerated but not completely risk-free. Risk from
acute exposure may be mitigated using the smallest dose possible and b -blockers with greater
b
1
-selectivity. b -Blocker-induced bronchospasm responded partially to b
2
-agonists in the doses
given with response blunted more by nonselective b -blockers than selective b -blockers. Use
of b -blockers in asthma could possibly be based upon a risk assessment on an individual patient
basis. CHEST 2014; 145(4):779786
Adverse Respiratory Effect of Acute
b -Blocker Exposure in Asthma
A Systematic Review and Meta-analysis
of Randomized Controlled Trials
Daniel R. Morales , MBChB ; Cathy Jackson , MD ; Brian J. Lipworth , MD ;
Peter T. Donnan , PhD ; and Bruce Guthrie , PhD
Manuscript received May 27, 2013; revision accepted October 2,
2013.
Afliations: From the Quality, Safety, and Informatics Group
(Drs Morales and Guthrie), Asthma and Allergy Research Group
(Dr Lipworth), and Dundee Epidemiology and Biostatistics
Unit (Dr Donnan), Medical Research Institute, University of
Dundee, Dundee; and the Bute Medical School (Dr Jackson),
University of St Andrews, Fife, Scotland .
Funding/Support: This study was funded by a Scottish Gov-
ernment Chief Scientist Ofce Clinical Academic Fellowship,
which provided research costs and support for Dr Morales [Grant
CAF/11/07].
Correspondence to: Daniel R. Morales, MBChB, Quality, Safety,
and Informatics Group, Medical Research Institute, University of
Dundee, Mackenzie Bldg, Dundee, DD2 4BF, Scotland; e-mail:
danielmorales@nhs.net
2014 American College of Chest Physicians. Reproduction
of this article is prohibited without written permission from the
American College of Chest Physicians. See online for more details.
DOI: 10.1378/chest.13-1235
Downloaded From: http://journal.publications.chestnet.org/ by M Darwich on 10/15/2014
780 Original Research
effects method was performed because heterogeneity was detected.
Random-effects metaregression was used to evaluate group baseline
FEV
1
and effect of steroid exposure categorized for each study as
no exposure, mixed exposure, and exposed. Metaregression was
performed in STATAv11 (SAS Institute Inc) and meta-analysis in
Review Manager (RevMan) v5.1 (The Cochrane Collaboration).
Sensitivity Analyses
Only patients with asthma were included. Sensitivity analysis
was performed according to whether trials reported a denition
of asthma according to American Thoracic Society or British
Thoracic Society guidelines, reversibility in FEV
1
of 15% in
response to b
2
-agonist, or response to methacholine/histamine prov-
ocation challenges. Sensitivity analysis was also performed accord-
ing to whether trials explicitly reported withholding b
2
-agonists
for at least 8 h. Missing SDs were calculated using individual
patient data and from P values as described.
6
For remaining miss-
ing values, the median P value was imputed and sensitivity analyses
performed using the minimum and maximum P values to ensure
conclusions remained unaltered.
Results
Of 1,989 references screened, 32 studies were
included ( Fig 1 , e-Table 3
7-41
). A total of 16 studies
evaluated selective b -blockers, six studies evaluated
nonselective b -blockers, and 10 studies evaluated both.
No randomized blinded placebo-controlled trials eval-
uating topical b -blockers in unselected patients were
found. For selective b -blockers, 23 studies provided
data on mean absolute percentage change in FEV
1
,
13 on symptoms, and ve on fall in FEV
1
of 20%.
For nonselective b -blockers, 14 studies provided data
on mean absolute percentage change in FEV
1
, six on
symptoms, and three on fall in FEV
1
of 20%.
The most common b -blockers studied were atenolol,
metoprolol, and propranolol (e-Tables 3, 4). A total
of 600 acute selective b -blocker exposures were evalu-
ated in 330 patients with asthma (mean age, 46 years;
67.5% men). A total of 301 acute nonselective b -blocker
exposures were evaluated in 218 patients with asthma
(mean age, 40.5 years; 68.9% men). Mean baseline
FEV
1
for selective and nonselective patients were
2.28 L and 2.50 L, respectively. In total, 28 trials (88%)
were single-dose studies (e-Table 3), with respiratory
measurements taken on average 108 min postdose.
Acute Selective b -Blockade
Compared with placebo, acute selective b -blockade
caused a mean absolute fall in FEV
1
of 2 6.9% (95% CI,
2 8.5 to 2 5.2; P , .001) ( Fig 2 ). The risk difference for
fall in FEV
1
of 20% was 0.13 (95% CI, 0.01-0.24;
P 5 .03) ( Fig 3 ), equating to a number needed to treat
of eight. The risk difference for symptoms was 0.03
(95% CI, 2 0.01 to 0.06; P 5 .18) (e-Fig 1) equating to
a number needed to treat of 33, which was not statis-
tically signicant.
of 7.46% with no change in symptoms.
3
However,
b -blockers vary according to b
1
-adrenoceptor selec-
tivity and partial agonist and a -blocking activity. The
effects of selective b -blockers may also vary by dose
and individual susceptibility, in which case use of mean
values alone may mask a clinically signicant risk in
a small proportion of patients. b -Blocker exposure is
not uncommon in asthma, with 2.2% of patients pre-
scribed b -blockers each year, so their risk needs to
be properly evaluated.
4
Nonselective b -blockers have
not been systematically evaluated, although they are
widely used in clinical practice, including labetalol,
used rst-line for the treatment of pregnancy-induced
hypertension, and topical agents used in glaucoma .
Nonselective b -blockers such as nadolol and pro-
pranolol have been investigated for their paradoxical
potential to reduce airway hyperresponsiveness and
inammation in asthma.
5
These benets may only
be seen following chronic exposure, and in this sense
patients must rst be able to tolerate acute exposure.
Additionally, b
2
-agonists are rst-line rescue therapy
for acute bronchoconstriction, and, in theory, their
efcacy could be reduced when given to patients
receiving b -blockers. The aim of this meta-analysis is
to systematically evaluate changes in respiratory func-
tion and b
2
-agonist efcacy following acute b -blockade.
Materials and Methods
A systematic review of MEDLINE, EMBASE, and Cochrane
Central Register of Controlled Trials (CENTRAL) databases
was performed using a prespecied protocol and search strat-
egy (e-Tables 1, 2 ) to identify all randomized, blinded, placebo-
controlled clinical trials published on or before January 20, 2013,
evaluating acute b -blocker exposure (up to 7 days) in asthma.
References and full texts were independently screened by a
minimum of two reviewers, with agreement based on consensus.
References of included studies were searched to identify addi-
tional trials. Only English language publications and published
data were included. Methodological quality and risk of bias were
evaluated for each trial using the Cochrane collaboration tool for
assessing risk of bias. Publication bias was examined using funnel
plots looking for asymmetry and performing the Egger test. The
systematic review was reported according to PRISMA (Preferred
Reporting Items for Systematic Reviews) requirements.
Statistical Analysis
Mean percentage change in FEV
1
was calculated and presented
as the mean absolute percentage difference in FEV
1
. A fall in FEV
1
of 20% and development of symptoms was presented as the risk
difference. A fall in FEV
1
of 20% was dened to better assess
individual response. b
2
-Agonist responsiveness was calculated
as mean percentage change in FEV
1
and presented as the mean
absolute difference compared with placebo. All measures of FEV
1
were calculated relative to original baseline FEV
1
values. Hetero-
geneity was assessed using the I
2
statistic. Subgroup analysis was
used to evaluate if individual drug-level effects and dose-response
relationships were feasible. A generic inverse variance method of
analysis was used for continuous outcomes, and a Mantel-Haenszel
method of analysis was used for dichotomous outcomes. A random-
Downloaded From: http://journal.publications.chestnet.org/ by M Darwich on 10/15/2014
journal.publications.chestnet.org CHEST / 145 / 4 / APRIL 2014 781
The risk difference for fall in FEV
1
of 20% was
0.11 (95% CI, 2 0.04 to 0.26; P 5 .14) (e-Fig 2),
equating to a number needed to treat of nine, which
was not statistically signicant. The risk difference
Figure 1. PRISMA (Preferred Reporting Items for Systematic Reviews) ow diagram for study selection .
Figure 2. Mean change in FEV
1
following acute selective b -blocker exposure. df 5 degrees of freedom.
Acute Nonselective b -Blockade
Compared with placebo, acute nonselective
b -blockade caused a mean absolute fall in FEV
1
of
2 10.2% (95% CI, 2 14.7 to 2 5.6; P , .001) ( Fig 4 ).
Downloaded From: http://journal.publications.chestnet.org/ by M Darwich on 10/15/2014
782 Original Research
Nonselective b -blockers also varied in relation to
mean change in FEV
1
following acute exposure ( Fig 8 ).
Compared with placebo, labetalol did not cause a sta-
tistically signicant mean change in FEV
1
(difference,
2 2.7%; 95% CI, 2 9.6 to 4.1; P 5 .43) (e-Fig 8),
whereas propranolol did (difference, 2 17.0%; 95% CI,
2 21.4 to 2 12.6; P , .001) (e-Fig 9).
Dose-Response Relationship: An increasing dose-
response relationship was demonstrated following
acute exposure to metoprolol, atenolol, and bisoprolol
(e-Figs 10-12). Mean change in FEV
1
following acute
exposure to 50 mg, 100 mg, and 200 mg of metoprolol
was 2 6.0%, 2 8.9%, and 2 13.0%, respectively. Mean
change in FEV
1
following acute exposure to 50 mg,
100 mg, and 200 mg of atenolol was 2 5.4%, 2 11.4%,
and 2 10.9%, respectively. Mean change in FEV
1
following acute exposure to 10 mg and 20 mg of biso-
prolol was 2 5.8% and 2 7.5%, respectively.
Baseline FEV
1
and Steroid Exposure: Meta-regression
analyses are presented in e-Table 5. There was little
evidence to suggest steroid exposure inuenced mean
change in FEV
1
following either acute selec tive (3.9%;
95% CI, 2 7.2 to 15.0 for exposed vs unexposed;
P 5 .469) or nonselective b -blocker exposure (5.8%;
95% CI, 2 25.3 to 36.8, for exposed vs unexposed;
P 5 .688). Mean baseline FEV
1
did not inuence mean
for symptoms was 0.08 (95% CI, 0.01-0.15; P 5 .02)
( Fig 5 ), equating to a number needed to treat of 13.
b
2
-Agonist Response Following Acute b -Blockade
Of studies evaluating selective and nonselective
b -blockers, 17 (74%) and nine (64%) included data
on b
2
-agonist response, respectively (e-Table 3). Rela-
tive to original baseline values, the crude mean FEV
1
response to b
2
-agonists was 1 22.7% for placebo,
1 16.0% for selective b -blockade, and 2 0.7% for non-
selective b -blockade ( Fig 6 ). Following meta-analysis,
the absolute mean difference in FEV
1
response to
b
2
-agonists relative to placebo was 2 10.2% (95% CI,
2 14.0 to 2 6.4; P , .001) (e-Fig 3) for selective
b -blockade and 2 20.0% (95% CI, 2 29.4 to 2 10.7;
P , .001) (e-Fig 4) for nonselective b -blockade.
Subgroup Analysis
Individual b -Blocker Comparison: Selective
b -blockers varied in relation to the degree of fall in
FEV
1
following acute exposure ( Fig 7 ). Compared
with placebo, celiprolol did not cause a statistically
signicant mean change in FEV
1
(difference, 1.8%;
95% CI, 2 2.3 to 5.8; P 5 .39) (e-Fig 5), whereas meto-
prolol (difference, 2 9.3%; 95% CI, 2 12.0 to 2 6.6;
P , .001) (e-Fig 6) and atenolol (difference, 2 10.2%;
95% CI, 2 12.6 to 2 7.8; P , .001) (e-Fig 7) did.
Figure 3. Fall in FEV
1
of 20% following acute selective b -blocker exposure. M-H 5 Mantel-Haenszel.
See Figure 2 legend for expansion of other abbreviation.
Figure 4. Mean change in FEV
1
following acute nonselective b -blocker exposure. See Figure 2 legend
for expansion of abbreviation.
Downloaded From: http://journal.publications.chestnet.org/ by M Darwich on 10/15/2014
journal.publications.chestnet.org CHEST / 145 / 4 / APRIL 2014 783
Discussion
Acute selective b -blockade in the doses given caused
statistically signicant mean reductions in FEV
1
, non-
signicant increases in symptoms, and signicant abso-
lute falls in FEV
1
of 20% (affecting 13% of subjects).
For mean changes in FEV
1
and symptoms, ndings
were similar to a previous meta-analysis, which eval-
uated selective b -blockers only and did not include
fall in FEV
1
of 20% as an outcome.
3
Our ndings
suggest that, although the mean effects of acute selec-
tive b -blockade are relatively small, it may cause clin-
ically signicant events in a minority of susceptible
patients who have exaggerated cholinergic tone. The
b
2
-agonist response after selective b -blockade was
partially attenuated relative to placebo. However, blunt-
ing of this magnitude is possibly of limited clinical
signicance, as pulmonary function typically increased
well beyond original baseline FEV
1
.
Acute nonselective b -blockade in the doses given
caused larger mean falls in FEV
1
, a signicant increase
in symptoms (affecting 8%), and similar but nonsig-
nicant falls in FEV
1
of 20%. As expected, nonse-
lective b -blockade completely attenuated b
2
-agonist
response relative to placebo, with post b
2
-agonist
FEV
1
values approximately returning to baseline.
In other studies involving patients with nonselective
b -blockade, b
2
-agonists completely reversed hista-
mine and methacholine challenge following acute and
chronic b -blockade.
42-44
These studies differ because
bronchoconstriction was experimentally induced to
more closely mimic what happens during acute asthma
or titrated exposure.
Falls in FEV
1
of 20% may represent patients who
are more susceptible to b -blockade, in which use of
mean values alone may underestimate risk. It remains
possible that other factors are important to trigger
clinically signicant exacerbations, including uncon-
trolled airway inammation or genetic factors such
as the arginine-16 b
2
-adrenoceptor polymorphism.
Approximately 15% of white patients with asthma are
homozygous for arginine-16 b
2
-adrenoceptor polymor-
phism, which predisposes to asthma exacerbations in
patients using salmeterol with inhaled corticosteroids.
45
change in FEV
1
following either selective ( 2 1.9%;
95% CI, 2 5.5 to 1.7; P 5 .272) or nonselective
b -blocker exposure ( 2 1.0%; 95% CI, 2 11.1 to 9.0;
P 5 .829).
Risk of Bias and Sensitivity Analyses
Many methodological qualities had an unclear risk
of bias, as studies did not provide explicit detail to
make an informed judgment (e-Fig 13). For studies
evaluating mean change in FEV
1
, funnel plot asym-
metry was observed for selective b -blockers ( P value
0.005) (e-Fig 14 ) but not for nonselective b -blockers
( P 5 0.111). Results from sensitivity analyses were
consistent with the main ndings.
Figure 5. Symptoms following acute nonselective b -blocker exposure. See Figure 2 and 3 legends for
expansion of abbreviations.
Figure 6. Mean change in FEV
1
and response to b
2
-agonist by
class of b -blocker. Mean FEV
1
response to b
2
-agonists was 1 22.7%
for placebo, 1 16.0% for selective b -blockade, and 2 0.7% for
nonselective b -blockade. Following meta-analysis, absolute mean
difference in FEV
1
between placebo was 2 10.2% and 2 20.0%
for selective and nonselective b -blockers, respectively, suggesting
the placebo b
2
-agonist response is partially blunted by selective
and completely blunted by nonselective b -blockade. Baseline
represented by the dotted horizontal line. Unweighted 95% CIs
calculated from pooling mean percentage change in FEV
1
from
all studies.
Downloaded From: http://journal.publications.chestnet.org/ by M Darwich on 10/15/2014
784 Original Research
be tolerated.
5,42,44
Subgroup analysis suggests differ-
ences in treatment effect within class, particularly
among celiprolol and labetalol. b
1
-adrenoceptor selec-
tivity varies, with b
1
-/ b
2
-afnity ratios ranging from
13.5 for bisoprolol to 4.7 for atenolol and 2.3 for
metoprolol.
49,50
Celiprolol is a b -blocker with partial
agonist activity and greater selectivity than atenolol
or bisoprolol, which may explain better tolerability.
51
However, labetalol is nonselective with a -blocking
properties, and, therefore, selectivity cannot not be the
only reason for better tolerability. a -Blockade is not
therapeutic in asthma, but nonselective a -blockade
may protect against bronchoconstriction in patients
with asthma with b -blockade, suggesting a protective
action only when sympathetic activity is blocked.
52-54
Although labetalol caused nonsignicant falls in FEV
1
,
heterogeneity remained, and other outcome data are
lacking to comprehensively evaluate its safety for use
in asthma.
Mean baseline FEV
1
or steroid exposure did not
appear to inuence treatment effect. This was done
because individuals with lower baseline FEV
1
may be
at higher risk where even small changes in FEV
1
are
of clinical signicance. It was not possible to evaluate
baseline hyperresponsiveness. Increased methacho-
line sensitivity may occur following b -blockade but
remains unaffected in many patients following acute
or chronic exposure.
10,14,44
One study evaluated exhaled
nitric oxide and reported no signicant variation follow-
ing nebivolol in steroid-naive patients, a nding also
seen with propranolol in steroid-treated patients.
13,44
Although meta-regression explores statistical hetero-
geneity with different study characteristics, it can
suffer from confounding, lack of power, and aggrega-
tion bias. In many instances reporting of steroid expo-
sure was limited, and we cannot be certain steroid
exposure does not attenuate b -blocker response.
Limitations and Strengths
In general, moderate to high b -blocker doses were
administered acutely, and no studies titrated exposure.
Most patients had mild to moderate asthma, and
results may not be applicable to patients with severe
or unstable asthma. However, most studies included
patients with 15% reversibility to b
2
-agonists that could
be more sensitive to b -blockers. The degree of bron-
chomotor tone regulated by sympathetic and parasym-
pathetic drive also probably determines susceptibility
to acute b -blockade, as will transient heightened airway
hyperresponsiveness, which may follow respiratory
tract infections. Respiratory function was evaluated
using FEV
1
, which may be less sensitive than other
methods.
55
Studies often failed to describe aspects
of study design, and it is possible that some heteroge-
neity may be due to bias. However, only randomized
The lack of data on topical b -blockers is important,
as deaths following oral and topical exposures have
occurred. Two studies were excluded because patients
were selected on the basis of prior timolol exposure.
From these, timolol and betaxolol caused mean falls
in FEV
1
of 14.2% and 9.6%, respectively.
46,47
It is
plausible that topical exposure is riskier than oral
because rapid absorption into the systemic circulation
occurs without rst-pass metabolism, and topical agents
have similar effects to IV administration in terms
of b
2
-adrenoceptor occupancy and cardiopulmonary
effects.
48
Heterogeneity in Treatment Effect
A dose-response relationship was seen with selective
b -blockers in keeping with loss of b
1
-adrenoceptor
selectivity at higher doses. Although not demon-
strated here, low-dose nonselective b -blockade can
Figure 7. Mean change in FEV
1
for individual selective b -blockers.
Baseline represented by dotted horizontal line. dose 5 mean dose;
n 5 number of patients.
Figure 8. Mean change in FEV
1
for individual nonselective
b -blockers. Baseline represented by dotted horizontal line. See
Figure 7 legend for expansion of abbreviations.
Downloaded From: http://journal.publications.chestnet.org/ by M Darwich on 10/15/2014
journal.publications.chestnet.org CHEST / 145 / 4 / APRIL 2014 785
Tridas, Genkyotex S.A., and Nycomed. The Asthma and Allergy
Research Group has received unrestricted grant support from Teva
Pharmaceuticals USA, Chiesi Ltd, and Almirall S.A. and other
funding for multicenter trials from RocheGenentech, Janssen
Pharmaceuticals, Inc, AstraZeneca, and Teva Pharmaceuticals USA.
Dr Donnan has received fees for consulting from the Scottish Medi-
cines Consortium and grant support from GlaxoSmithKline plc,
Otsuka America Pharmaceutical, Inc and Amgen Inc. Drs Morales,
Jackson, and Guthrie have reported that no potential conicts of
interest exist with any companies/organizations whose products
or services may be discussed in this article .
Role of sponsors: The sponsor had no role in the design of the
study, the collection and analysis of the data, or the preparation of
the manuscript .
Additional information: The e-Figures and e-Tables can be
found in the Supplemental Materials area of the online article.
References
1 . British Thoracic Society; Scottish Intercollegiate Guidelines
Network . British guideline on the management of asthma.
Thorax. 2008 ;63(suppl 4):iv1-iv121.
2 . Lipworth BJ , Williamson PA . Think the impossible: beta-
blockers for treating asthma . Clin Sci (Lond) . 2010 ; 118 ( 2 ):
115 - 120 .
3 . Salpeter S , Ormiston T , Salpeter E . Cardioselective beta-
blockers for reversible airway disease . Cochrane Database
Syst Rev . 2002 ; ( 1 ): CD002992 .
4 . Morales DR , Guthrie B , Lipworth BJ , Donnan PT , Jackson C .
Prescribing of b -adrenoceptor antagonists in asthma: an obser-
vational study . Thorax . 2011 ; 66 ( 6 ): 502 - 507 .
5 . Hanania NA , Singh S , El-Wali R , et al . The safety and effects
of the beta-blocker, nadolol, in mild asthma: an open-label
pilot study . Pulm Pharmacol Ther . 2008 ; 21 ( 1 ): 134 - 141 .
6 . Elbourne DR , Altman DG , Higgins JP, Curtin F , Worthington
HV , Vail A . Meta-analyses involving cross-over trials: method-
ological issues . Int J Epidemiol . 2002 ; 31 ( 1 ): 140 - 149 .
7 . Benson MK , Berrill WT , Cruickshank JM , Sterling GS . A
comparison of four beta-adrenoceptor antagonists in patients
with asthma . Br J Clin Pharmacol . 1978 ; 5 ( 5 ): 415 - 419 .
8 . Beumer HM , Teirlinck C , Wiseman RA . Comparative inves-
tigation of the respiratory and cardiovascular effect of mepin-
dolol, propranolol and pindolol in asthmatic patients . Int J
Clin Pharmacol Biopharm . 1978 ; 16 ( 6 ): 249 - 253 .
9 . Boye NP , Vale JR . Effect in bronchial asthma of a new beta-
adrenergic blocking drug atenolol (ICI 66, 082) . Eur J Clin
Pharmacol . 1977 ; 11 ( 1 ): 11 - 14 .
10 . Cannon RE , Slavin RG , Gonasun LM . The effect on asthma
of a new beta blocker, pindolol . Am Heart J . 1982 ; 104 ( 2 pt 2 ):
438 - 442 .
11 . Chatterjee SS . The cardioselective and hypotensive effects
of bisoprolol in hypertensive asthmatics . J Cardiovasc Phar-
macol . 1986 ; 8 ( suppl 11 ): S74 - S77 .
12 . Chodosh S , Tuck J , Blasucci DJ . The effects of dilevalol,
metoprolol, and placebo on ventilatory function in asthmatics .
J Cardiovasc Pharmacol . 1988 ; 11 ( suppl 2 ): S18 - S24 .
13 . Dal Negro RW , Tognella S , Micheletto C . Pharmacokinetics
of the effect of Nebivolol 5mg on airway patency in patients
with mild to moderate bronchial asthma and arterial hyper-
tension . Clin Drug Investig . 2002 ; 22 ( 3 ): 197 - 204 .
14 . Devereux G , Fishwick K , Aiken TC , Bourke SJ , Hendrick DJ .
Adverse effects of a single dose of ( 1 )-sotalol in patients with
mild stable asthma . Br J Clin Pharmacol . 1998 ; 46 ( 1 ): 79 - 82 .
15 . Doshan HD , Brown R , Applin WJ , Kapoor M , Caruso FS .
Effects of high doses of celiprolol in asthmatic patients .
J Cardiovasc Pharmacol . 1986 ; 8 ( suppl 4 ): S109 - S111 .
16 . Doshan HD , Rosenthal RR , Brown R , Slutsky A , Applin WJ ,
Caruso FS . Celiprolol, atenolol and propranolol: a comparison
blinded placebo-controlled trials were included, which
are considered the gold standard for clinical research.
Implications for Clinical Practice
The principal indication for b -blockers in asthma
is for cardiovascular comorbidities. Although reason-
ably well tolerated by the majority, acute selective
b -blockade may cause detrimental changes in lung
function in susceptible patients with asthma. However,
risk from acute exposure in patients with controlled
asthma may be mitigated by commencing the lowest
dose possible and using a highly selective agent, with
reassurance that any bronchoconstriction responds
reasonably well to b
2
-agonists. As such, it may be pos-
sible to consider their use in asthma on an individual
basis following a risk assessment in patients with well-
controlled asthma. Although many patients with asthma
tolerated exposure to nonselective b -blockade, acute
risk is greater, which could possibly be mitigated
through gradual dose titration and initial concomitant
cover with a long-acting muscarinic antagonist, to pre-
vent unopposed increased cholinergic tone uncovered
by acute b -blockade.
44
Irrespective of which b -blocker
is contemplated, acute exposure appears to have
the greatest risk, which may attenuate upon chronic
exposure.
5,44
Although bronchospasm induced by moderate- to
high-dose b -blockade appears to respond reasonably
well to conventional doses of b
2
-agonists, partial blunting
may occur that is greater when nonselective b -blockers
are given compared with selective b -blockers. In
this regard, higher doses of b
2
-agonists are probably
required to achieve sufcient b
2
-receptor occupancy
with concomitant b -blockade, as demonstrated.
5,44
The
acute and chronic dosing effects of selective and non-
selective b -blockade on long-acting b
2
-agonist response
in patients taking combination therapy requires fur-
ther prospective evaluation.
Acknowledgments
Author contributions: Dr Morales is guarantor of the data.
Dr Morales: contributed to conceiving the idea, study design,
interpretation of the ndings, data analysis, drafting of the manu-
script, and approving the nal draft.
Dr Jackson: contributed to conceiving the idea, study design,
interpretation of the ndings, drafting of the manuscript, and
approving the nal draft.
Dr Lipworth: contributed to study design, interpretation of the
ndings, drafting of the manuscript, and approving the nal draft.
Dr Donnan: contributed to conceiving the idea, study design,
interpretation of the ndings, data analysis, drafting of the manu-
script, and approving the nal draft.
Dr Guthrie: contributed to conceiving the idea, study design,
interpretation of the ndings, drafting of the manuscript, and
approving the nal draft.
Financial/nonnancial disclosures: The authors have reported
to CHEST the following conicts of interest: Dr Lipworth has
received fees for speaking, consulting and advisory boards from
Teva Pharmaceuticals USA, Chiesi Ltd, Sandoz, Cipla, Synexus,
Downloaded From: http://journal.publications.chestnet.org/ by M Darwich on 10/15/2014
786 Original Research
35 . Sue DY , Hansen JE , Wasserman K . The value of exercise
in testing beta blockade and airway reactivity in asthmatic
patients . Am Heart J . 1982 ; 104 ( 2 pt 2 ): 442 - 445 .
36 . Suzuki S , Mue S , Ohmi T . Effect of atenolol on pulmonary
function in asthma . Acta Ther . 1981 ; 7 ( 1 ): 55 - 65 .
37 . Tantucci C , Bruni B , Dottorini ML , et al . Comparative eval-
uation of cardioselectivity of metoprolol OROS and atenolol:
a double-blind, placebo-controlled crossover study . Am Heart
J . 1990 ; 120 ( 2 ): 467 - 472 .
38 . Thiringer G , Svedmyr N . Interaction of orally administered
metoprolol, practolol and propranolol with isoprenaline in
asthmatics . Eur J Clin Pharmacol . 1976 ; 10 (3-4): 163 - 170 .
39 . Lawrence D.S , Sahay JN , Chatterjee SS, Cruickshank JM.
b -Blockers in asthma . Drugs . 1983 ; 25 ( suppl 2 ): 232 - 236 .
40 . Matthys H , Doshan HD , Rhle KH , Applin WJ , Braig H ,
Pohl M . Bronchosparing properties of celiprolol, a new beta
1, alpha 2-blocker, in propranolol-sensitive asthmatic patients .
J Cardiovasc Pharmacol . 1986 ; 8 ( suppl 4 ): S40 - S42 .
41 . Sue DY , Hansen JE , Wasserman K . Beta-adrenergic block-
ade with pindolol (LB-46) in mild to moderate asthma . Chest .
1981 ; 80 ( 5 ): 537 - 542 .
42 . Short PM , Williamson PA , Lipworth BJ . Effects of hydrocorti-
sone on acute b -adrenoceptor blocker and histamine induced
bronchoconstriction . Br J Clin Pharmacol . 2012 ; 73 ( 5 ): 717 - 726 .
43 . Hanania NA , Mannava B , Franklin AE , et al . Response to
salbutamol in patients with mild asthma treated with nadolol .
Eur Respir J . 2010 ; 36 ( 4 ): 963 - 965 .
44 . Short PM , Williamson PA , Anderson WJ , Lipworth BJ . Ran-
domized placebo-controlled trial to evaluate chronic dosing
effects of propranolol in asthma . Am J Respir Crit Care Med .
2013 ; 187 ( 12 ): 1308 - 1314 .
45 . Basu K , Palmer CN , Tavendale R , Lipworth BJ , Mukhopadhyay
S . Adrenergic beta(2)-receptor genotype predisposes to exac-
erbations in steroid-treated asthmatic patients taking frequent
albuterol or salmeterol . J Allergy Clin Immunol . 2009 ; 124 ( 6 ):
1188 - 1194 .
46 . Friren B , Michaud JE . Safety comparison of topical brin-
zolamide 1% and timolol 0.5% in patients with asthma or
chronic obstructive pulmonary disease . Todays Therapeutic
Trends . 2004 ; 22 ( 1 ): 69 - 80 .
47 . Schoene RB , Abuan T , Ward RL , Beasley CH . Effects of
topical betaxolol, timolol, and placebo on pulmonary function
in asthmatic bronchitis . Am J Ophthalmol . 1984 ; 97 ( 1 ): 86 - 92 .
48 . Korte JM , Kaila T , Saari KM . Systemic bioavailability and
cardiopulmonary effects of 0.5% timolol eyedrops . Graefes
Arch Clin Exp Ophthalmol . 2002 ; 240 ( 6 ): 430 - 435 .
49 . Baker JG . The selectivity of beta-adrenoceptor antagonists
at the human beta1, beta2 and beta3 adrenoceptors . Br J
Pharmacol . 2005 ; 144 ( 3 ): 317 - 322 .
50 . Badgett RG , Lawrence VA , Cohn SL . Variations in pharma-
cology of beta-blockers may contribute to heterogeneous
results in trials of perioperative beta-blockade . Anesthesiology .
2010 ; 113 ( 3 ): 585 - 592 .
51 . Wheeldon NM , McDevitt DG , Lipworth BJ . Selectivity of
antagonist and partial agonist activity of celiprolol in normal
subjects . Br J Clin Pharmacol . 1992 ; 34 ( 4 ): 337 - 343 .
52 . Baudouin SV , Aitman TJ , Johnson AJ . Prazosin in the treat-
ment of chronic asthma . Thorax . 1988 ; 43 ( 5 ): 385 - 387 .
53 . Patel KR , Kerr JW . The airways response to phenylephrine
after blockade of alpha and beta receptors in extrinsic bron-
chial asthma . Clin Allergy . 1973 ; 3 ( 4 ): 439 - 448 .
54 . Dorow P . The role of alpha-receptors in bronchoconstriction
induced by beta-blockade . Respiration . 1982 ; 43 ( 5 ): 359 - 362 .
55 . Short PM , Williamson PA , Lipworth BJ . Sensitivity of impulse
oscillometry and spirometry in beta-blocker induced bron-
choconstriction and beta-agonist bronchodilatation in asthma .
Ann Allergy Asthma Immunol . 2012 ; 109 ( 6 ): 412 - 415 .
of pulmonary effects in asthmatic patients . J Cardiovasc
Pharmacol . 1986 ; 8 ( suppl 4 ): S105 - S108 .
17 . Ellis ME , Sahay JN , Chatterjee SS , Cruickshank JM , Ellis SH .
Cardioselectivity of atenolol in asthmatic patients . Eur J Clin
Pharmacol . 1981 ; 21 ( 3 ): 173 - 176 .
18 . Ellis ME , Hussain M , Webb AK , Barker NP , Fitzsimons TJ .
The effect of cimetidine on the relative cardioselectivity of
atenolol and metoprolol in asthmatic patients . Br J Clin Phar-
macol . 1984 ; 17 ( suppl 1 ): 59S - 64S .
19 . Falliers CJ , Vrchota J , Blasucci DJ , Maloy JW , Medakovic M .
The effects of treatments with labetalol and hydrochlo-
rothiazide on ventilatory function of asthmatic hypertensive
patients with demonstrated bronchosensitivity to propranolol .
J Clin Hypertens . 1985 ; 1 ( 1 ): 70 - 79 .
20 . Falliers CJ , Vincent ME , Medakovic M . Effect of single doses
of labetalol, metoprolol, and placebo on ventilatory function
in patients with bronchial asthma: interaction with isoproter-
enol . J Asthma . 1986 ; 23 ( 5 ): 251 - 260 .
21 . Fogari R , Zoppi A , Tettamanti F , Poletti L , Rizzardi G ,
Fiocchi G . Comparative effects of celiprolol, propranolol,
oxprenolol, and atenolol on respiratory function in hyperten-
sive patients with chronic obstructive lung disease . Cardiovasc
Drugs Ther . 1990 ; 4 ( 4 ): 1145 - 1149 .
22 . Jackson SH , Beevers DG . Comparison of the effects of sin-
gle doses of atenolol and labetalol on airways obstruction in
patients with hypertension and asthma . Br J Clin Pharmacol .
1983 ; 15 ( 5 ): 553 - 556 .
23 . Lammers JW , Folgering HT , van Herwaarden CL . Ventilatory
effects of atenolol and bevantolol in asthma . Clin Pharmacol
Ther . 1985 ; 38 ( 4 ): 428 - 433 .
24 . Larsson K . Influence of labetalol, propranolol and prac-
tolol in patients with asthma . Eur J Respir Dis . 1982 ; 63 ( 3 ):
221 - 230 .
25 . Lawrence DS , Sahay JN , Chatterjee SS , Cruickshank JM .
Asthma and beta-blockers . Eur J Clin Pharmacol . 1982 ; 22 ( 6 ):
501 - 509 .
26 . Lfdahl CG , Svedmyr N . Cardioselectivity of atenolol and
metoprolol. A study in asthmatic patients . Eur J Respir Dis .
1981 ; 62 ( 6 ): 396 - 404 .
27 . Lfdahl CG , Dahlf C , Westergren G , Olofsson B , Svedmyr N .
Controlled-release metoprolol compared with atenolol in
asthmatic patients: interaction with terbutaline . Eur J Clin
Pharmacol . 1988 ; 33 ( suppl ): S25 - S32 .
28 . Matthys H , Doshan HD , Rhle KH , et al . The broncho-
sparing effect of celiprolol, a new beta 1- alpha 2-receptor
antagonist on pulmonary function of propranolol-sensitive
asthmatics . J Clin Pharmacol . 1985 ; 25 ( 5 ): 354 - 359 .
29 . Mue S , Sasaki T , Ohmi T , et al . Inuence of Acebutolol on
the haemodynamic and respiratory function of asthmatic
patients . J Pharmacother . 1979 ; 2 ( 2 ): 67 - 71 .
30 . Nair S , Maguire WC , Laddu AR . The effect of acebutolol, a
beta adrenergic blocking agent, and placebo on pulmonary
functions in asthmatics . Int J Clin Pharmacol Ther Toxicol .
1981 ; 19 ( 12 ): 519 - 526 .
31 . Nicolaescu V , Manicatide M , Stroescu V . -Adrenergic block-
ade with practolol in acetylcholine-sensitive asthma patients .
Respiration . 1972 ; 29 ( 2 ): 139 - 154 .
32 . Nicolaescu V , Racoveanu C , Manicatide M . Effects of exer-
cise on practolol-treated asthmatic patients . Eur J Clin Phar-
macol . 1973 ; 6 ( 1 ): 3 - 8 .
33 . Repsher LH , Vincent ME , Medakovic M . The effect of
single doses of labetalol, metoprolol and placebo on ventila-
tory function in patients with bronchial asthma . J Hypertens .
1986 ; 4 ( suppl 5 ) S510 - S512 .
34 . Skinner C , Gaddie J , Palmer KN . Comparison of intravenous
AH 5158 (ibidomide) and propranolol in asthma . BMJ . 1975 ;
2 ( 5962 ): 59 - 61 .
Downloaded From: http://journal.publications.chestnet.org/ by M Darwich on 10/15/2014
Das könnte Ihnen auch gefallen
- Toxicoepigenetics: Core Principles and ApplicationsVon EverandToxicoepigenetics: Core Principles and ApplicationsShaun D. McCulloughNoch keine Bewertungen
- Assessment of Synthetic Glucocorticoids in Asthmatic SputumDokument3 SeitenAssessment of Synthetic Glucocorticoids in Asthmatic SputumDewiRahmatikaNoch keine Bewertungen
- Bapineuzumab For Mild To Moderate Alzheimer 'S Disease in Two Global, Randomized, Phase 3 TrialsDokument13 SeitenBapineuzumab For Mild To Moderate Alzheimer 'S Disease in Two Global, Randomized, Phase 3 TrialsRoza EtlaboraNoch keine Bewertungen
- Journal of The New Zealand Medical AssociationDokument4 SeitenJournal of The New Zealand Medical AssociationerickmattosNoch keine Bewertungen
- TORCH Salmeterol Fluticasona en EpocDokument15 SeitenTORCH Salmeterol Fluticasona en EpocAgustina AndradeNoch keine Bewertungen
- Jurnal Kortikosteroid PDFDokument9 SeitenJurnal Kortikosteroid PDFindry_purnamasari0% (1)
- Contro Pacientes DiabeticosDokument3 SeitenContro Pacientes DiabeticosFrancisco Josue TinajeroNoch keine Bewertungen
- The Active Comparator, New User Study Design in Pharmacoepidemiology: Historical Foundations and Contemporary ApplicationDokument8 SeitenThe Active Comparator, New User Study Design in Pharmacoepidemiology: Historical Foundations and Contemporary ApplicationDici RachmandaNoch keine Bewertungen
- Results of A Phase 2b Trial With GB001, A ProstaglDokument12 SeitenResults of A Phase 2b Trial With GB001, A ProstaglKaran KalraNoch keine Bewertungen
- Intranasal Corticosteroids in Management of Acute Sinusitis: A Systematic Review and Meta-AnalysisDokument9 SeitenIntranasal Corticosteroids in Management of Acute Sinusitis: A Systematic Review and Meta-AnalysisagustinadianasariaguNoch keine Bewertungen
- Intoxicacion Por Betabloqueadores ToxicologyDokument42 SeitenIntoxicacion Por Betabloqueadores ToxicologyIza ÁlvarezNoch keine Bewertungen
- Beta Bloker in Asthma 1Dokument6 SeitenBeta Bloker in Asthma 1melawatiNoch keine Bewertungen
- Colistin Monotherapy Versus Combination Therapy For Carbapenem-Resistant Organisms NEJM EvidenceDokument27 SeitenColistin Monotherapy Versus Combination Therapy For Carbapenem-Resistant Organisms NEJM Evidencerac.oncologyNoch keine Bewertungen
- Propranolol em Queimados MetanaliseDokument9 SeitenPropranolol em Queimados MetanaliseIsadora PereiraNoch keine Bewertungen
- Beta-Blocker Use and COPD Mortality: A Systematic Review and Meta-AnalysisDokument6 SeitenBeta-Blocker Use and COPD Mortality: A Systematic Review and Meta-AnalysisegerpratamaNoch keine Bewertungen
- Full Text ADokument6 SeitenFull Text AJoão NaveNoch keine Bewertungen
- Probiotics For Prevention of Antibiotic-Associated Diarrhea and Meta-AnalysisDokument6 SeitenProbiotics For Prevention of Antibiotic-Associated Diarrhea and Meta-AnalysisRicky FullerNoch keine Bewertungen
- A Proteomic Approach For The Diagnosis of Bacterial Meningitisjournal - Pone.0010079Dokument9 SeitenA Proteomic Approach For The Diagnosis of Bacterial Meningitisjournal - Pone.0010079Paijo SusenoNoch keine Bewertungen
- Heterologous Primary and Booster COVID-19 Vaccination: Evidence Based Regulatory ConsiderationsDokument26 SeitenHeterologous Primary and Booster COVID-19 Vaccination: Evidence Based Regulatory ConsiderationsHelpNoch keine Bewertungen
- NIH Public Access: Author ManuscriptDokument16 SeitenNIH Public Access: Author ManuscriptamorsantoNoch keine Bewertungen
- Bromelain As A Treatment For Osteoarthritis: A Review of Clinical StudiesDokument7 SeitenBromelain As A Treatment For Osteoarthritis: A Review of Clinical StudiesKent AaronNoch keine Bewertungen
- Does Prolonged B Lactam Infusions Improve Clinical Outcomes Compared To Intermittent Infusions A Meta Analysis and Systematic Review of Randomized Controlled TrialsDokument13 SeitenDoes Prolonged B Lactam Infusions Improve Clinical Outcomes Compared To Intermittent Infusions A Meta Analysis and Systematic Review of Randomized Controlled TrialskradoNoch keine Bewertungen
- Eectiveness Tolerability and Safety of Tofacitinib inDokument14 SeitenEectiveness Tolerability and Safety of Tofacitinib indanny gomezNoch keine Bewertungen
- Itepekimab 120Dokument11 SeitenItepekimab 1205fqkqkcdhtNoch keine Bewertungen
- Group 5 Pubmed Accepted Results PDFDokument683 SeitenGroup 5 Pubmed Accepted Results PDFDnyanesh LimayeNoch keine Bewertungen
- Beta Agonistas en SdraDokument3 SeitenBeta Agonistas en SdrajuanNoch keine Bewertungen
- Antibiotic Treatment Outcomes in Community-Acquired Pneumonia (#576717) - 734320Dokument7 SeitenAntibiotic Treatment Outcomes in Community-Acquired Pneumonia (#576717) - 734320tofanNoch keine Bewertungen
- Abx Empirica de NacDokument9 SeitenAbx Empirica de NacMarcelo Jimenez CruzNoch keine Bewertungen
- Paper Alumnos 5Dokument14 SeitenPaper Alumnos 5Victor Martinez HagenNoch keine Bewertungen
- Severe and Difficult-to-Treat Asthma in Adults: Review ArticleDokument12 SeitenSevere and Difficult-to-Treat Asthma in Adults: Review ArticlePatricio MiguelNoch keine Bewertungen
- Thorax 2010 Chapman 747 52 PDFDokument7 SeitenThorax 2010 Chapman 747 52 PDFnetifarhatiiNoch keine Bewertungen
- TRIBUTE Manuscript Peer Amends 19 Jan 2018 PostDokument28 SeitenTRIBUTE Manuscript Peer Amends 19 Jan 2018 PostOdessa EnriquezNoch keine Bewertungen
- Impact of Self-Reported Gastroesophageal Reflux Disease in Subjects From Copdgene CohortDokument9 SeitenImpact of Self-Reported Gastroesophageal Reflux Disease in Subjects From Copdgene CohortkasabeNoch keine Bewertungen
- Toxicidad de AntituberculososDokument38 SeitenToxicidad de AntituberculososVigilancia EpidemiologicaNoch keine Bewertungen
- Buteyko ChildrenDokument4 SeitenButeyko Childrendghiwaudy728Noch keine Bewertungen
- Ethos 2020Dokument14 SeitenEthos 2020Radu CiprianNoch keine Bewertungen
- AllergenDokument9 SeitenAllergenVero IbarraNoch keine Bewertungen
- Acebrofilina+budesonidaDokument3 SeitenAcebrofilina+budesonidaAgencia FaroNoch keine Bewertungen
- 6panchal EtalDokument5 Seiten6panchal EtaleditorijmrhsNoch keine Bewertungen
- Grandjean 2000Dokument13 SeitenGrandjean 2000Ivan VeriswanNoch keine Bewertungen
- Revision Bibliografica JUNIO 2022Dokument12 SeitenRevision Bibliografica JUNIO 2022Sergio Herrero BermejoNoch keine Bewertungen
- Safety and Efficacy of Mirabegron in Daily Clinical Practice Kallner 2016Dokument6 SeitenSafety and Efficacy of Mirabegron in Daily Clinical Practice Kallner 2016Elysabet aristaNoch keine Bewertungen
- Falla RenalDokument3 SeitenFalla RenalLujan PilarNoch keine Bewertungen
- Lee 2020Dokument13 SeitenLee 2020Javier BlancNoch keine Bewertungen
- Glutamina IVDokument11 SeitenGlutamina IVBLADIMIR ALEJANDRO GIL VALENCIANoch keine Bewertungen
- The Role of Adjuvant Therapy in Pemphigus: A Systematic Review and Meta-AnalysisDokument8 SeitenThe Role of Adjuvant Therapy in Pemphigus: A Systematic Review and Meta-Analysismasayuki haradaNoch keine Bewertungen
- Dupilumab AsthmaDokument11 SeitenDupilumab AsthmaMr. LNoch keine Bewertungen
- Safety and Tolerability of BAN2401 - A Clinical Study in Alzheimer's Disease With a Protofibril Selective Aβ AntibodyDokument10 SeitenSafety and Tolerability of BAN2401 - A Clinical Study in Alzheimer's Disease With a Protofibril Selective Aβ AntibodyPau Fer Mujica CNoch keine Bewertungen
- 15.benralizumab 111Dokument11 Seiten15.benralizumab 1115fqkqkcdhtNoch keine Bewertungen
- Oncologie GistDokument6 SeitenOncologie GistMada IacobNoch keine Bewertungen
- FULLTEXT01Dokument21 SeitenFULLTEXT01mason.sadeghiNoch keine Bewertungen
- 0006 07Dokument6 Seiten0006 07farantinaNoch keine Bewertungen
- Jurnal AsthmaDokument11 SeitenJurnal AsthmaNadira Juanti PratiwiNoch keine Bewertungen
- PH 4Dokument4 SeitenPH 4adlbrlnNoch keine Bewertungen
- Is Albumin Use SAFE in Patients With Traumatic Brain Injury?Dokument3 SeitenIs Albumin Use SAFE in Patients With Traumatic Brain Injury?Leon L GayaNoch keine Bewertungen
- Meta-Analysis Evaluating Respiratory Fluoroquinolones For Community-Acquired PneumoniaDokument21 SeitenMeta-Analysis Evaluating Respiratory Fluoroquinolones For Community-Acquired PneumoniaDiana Valeria Melo CNoch keine Bewertungen
- 136 Full CopdDokument7 Seiten136 Full CopdAnty FftNoch keine Bewertungen
- Do NotDokument8 SeitenDo NotAkhmad AfriantoNoch keine Bewertungen
- β-Blockers for the prevention of acute exacerbations of chronic obstructive pulmonary disease (βLOCK COPD) : a randomised controlled study protocolDokument10 Seitenβ-Blockers for the prevention of acute exacerbations of chronic obstructive pulmonary disease (βLOCK COPD) : a randomised controlled study protocolAnonymous SdnoIOtjNoch keine Bewertungen
- Risk Factors For Drug-Resistant Streptococcus Pneumoniae and Antibiotic Prescribing Practices in Outpatient Community-Acquired PneumoniaDokument4 SeitenRisk Factors For Drug-Resistant Streptococcus Pneumoniae and Antibiotic Prescribing Practices in Outpatient Community-Acquired PneumoniakingkinresmytaNoch keine Bewertungen
- SEEK/Pulmonary Board ReviewDokument102 SeitenSEEK/Pulmonary Board ReviewAzmachamberAzmacare100% (2)
- SEEK/Pulmonary Board ReviewDokument34 SeitenSEEK/Pulmonary Board ReviewAzmachamberAzmacareNoch keine Bewertungen
- Ethics/Pulmonary Board ReviewDokument43 SeitenEthics/Pulmonary Board ReviewAzmachamberAzmacareNoch keine Bewertungen
- Exercise Testing/Pulmonary Board ReviewDokument42 SeitenExercise Testing/Pulmonary Board ReviewAzmachamberAzmacareNoch keine Bewertungen
- Fungal Diseases/Pulmonary Board ReviewDokument54 SeitenFungal Diseases/Pulmonary Board ReviewAzmachamberAzmacareNoch keine Bewertungen
- Pathology Airway Disease /lung Cancer/pulmonary Board ReviewDokument109 SeitenPathology Airway Disease /lung Cancer/pulmonary Board ReviewAzmachamberAzmacare100% (1)
- Inhaled Corticosteroids Safety and Adverse Effects-DikonversiDokument8 SeitenInhaled Corticosteroids Safety and Adverse Effects-DikonversiRachmi MerrinaNoch keine Bewertungen
- AsthmaDokument39 SeitenAsthmamits98Noch keine Bewertungen
- Treatment of Bronchospasm During Anesthesia .28Dokument4 SeitenTreatment of Bronchospasm During Anesthesia .28Anish H DaveNoch keine Bewertungen
- Pediatric Chronic Sinusitis Diagnosis and ManagementDokument10 SeitenPediatric Chronic Sinusitis Diagnosis and ManagementcaromoradNoch keine Bewertungen
- IUMS2014, ProceedingDokument1.487 SeitenIUMS2014, Proceedingamir-scribdNoch keine Bewertungen
- Air Statement of Ti Gyit ENG VersionDokument18 SeitenAir Statement of Ti Gyit ENG VersionSoe Min NaingNoch keine Bewertungen
- Vyntus-Family BR EN PDFDokument7 SeitenVyntus-Family BR EN PDFLajoskaNoch keine Bewertungen
- National Health ProgramDokument7 SeitenNational Health ProgramJyoti singhNoch keine Bewertungen
- Importance of Consistent ICS Dosing in AsthmaDokument52 SeitenImportance of Consistent ICS Dosing in AsthmaEva SusantiNoch keine Bewertungen
- Asthma Action Plan For Children PDF DownloadDokument2 SeitenAsthma Action Plan For Children PDF DownloadAlejandro MalagáNoch keine Bewertungen
- Nursing Practice 2-5Dokument47 SeitenNursing Practice 2-5Emir Mukhtar Malcampo KamidNoch keine Bewertungen
- CO4 HealthDokument3 SeitenCO4 HealthJennelyn Orilla Brezo - Arcosiba100% (2)
- Comprehensive Edited)Dokument82 SeitenComprehensive Edited)mikrobyo_ng_wmsuNoch keine Bewertungen
- First AidDokument52 SeitenFirst Aidapi-351099966Noch keine Bewertungen
- MDPH Asthma BrochureDokument2 SeitenMDPH Asthma BrochureShakina FareedNoch keine Bewertungen
- Nejmra 2032506Dokument15 SeitenNejmra 2032506subha95Noch keine Bewertungen
- Clinical Group Study Case 1Dokument8 SeitenClinical Group Study Case 1Olivia JagroopNoch keine Bewertungen
- Case Presentation: AsthmaDokument21 SeitenCase Presentation: AsthmaCalingalan Hussin CaluangNoch keine Bewertungen
- Material Safety Data Sheet: Development Associates, IncDokument3 SeitenMaterial Safety Data Sheet: Development Associates, IncDedi MulyadiNoch keine Bewertungen
- Me (Scenarios) (Printed)Dokument17 SeitenMe (Scenarios) (Printed)Anup Lal RajbahakNoch keine Bewertungen
- Symptomatic Treatment of Cough Among Adult Patients With Lung Cancer CHEST Guideline and Expert Panel ReportDokument14 SeitenSymptomatic Treatment of Cough Among Adult Patients With Lung Cancer CHEST Guideline and Expert Panel ReportThaísa NogueiraNoch keine Bewertungen
- Cambio Climático y AsmaDokument3 SeitenCambio Climático y Asmaagonzal1974Noch keine Bewertungen
- TERBUTALINE (Terbutaline Sulfate) : Why Is This Medicine Prescribed To You?Dokument1 SeiteTERBUTALINE (Terbutaline Sulfate) : Why Is This Medicine Prescribed To You?Toni Marie Q. Mangubat-OpiñaNoch keine Bewertungen
- NEJM 2014 Fundamentals of Lung AuscultationDokument7 SeitenNEJM 2014 Fundamentals of Lung AuscultationFelipe CeaNoch keine Bewertungen
- Epidemiology of AsthmaDokument8 SeitenEpidemiology of AsthmaMaria Alejandra Siachoque JaraNoch keine Bewertungen
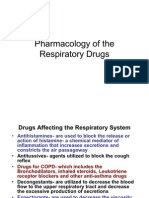
- Pharmacology - Respiratory DrugsDokument61 SeitenPharmacology - Respiratory DrugsBenjamin Joel Breboneria100% (5)
- Pedia CardsDokument40 SeitenPedia CardsKristine Marie Santos100% (1)
- Dental Management of Patients With Respiratory Disease: (Copd)Dokument12 SeitenDental Management of Patients With Respiratory Disease: (Copd)Fahd AlahaidebNoch keine Bewertungen
- Intravenous Nutrient Therapy: The "Myers' Cocktail"Dokument15 SeitenIntravenous Nutrient Therapy: The "Myers' Cocktail"Heather PorterNoch keine Bewertungen