Beruflich Dokumente
Kultur Dokumente
Glioblastoma Multiforme of Optic Nerve in Adults With Hyper Intense Diffuse Weighted Imaging
Hochgeladen von
International Organization of Scientific Research (IOSR)Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Glioblastoma Multiforme of Optic Nerve in Adults With Hyper Intense Diffuse Weighted Imaging
Hochgeladen von
International Organization of Scientific Research (IOSR)Copyright:
Verfügbare Formate
IOSR Journal of Dental and Medical Sciences (IOSR-JDMS)
e-ISSN: 2279-0853, p-ISSN: 2279-0861.Volume 13, Issue 6 Ver. III (Jun. 2014), PP 09-12
www.iosrjournals.org
www.iosrjournals.org 9 | Page
Glioblastoma Multiforme of Optic Nerve in Adults with Hyper
intense Diffuse Weighted Imaging
Karthik Adiraju ;Phani Harshitha Yarlagadda;Sohil Patel
(General Medicine,Kamineni Institute Of Medical Sciences,India )
(General Medicine,Kamineni Institute Of Medical Sciences,India)
(Fellow NeuroRadiology,Massachusettes General Hospital,Boston,U.S)
Abstract: We present a case of glioblastomamultiforme of the optic nerve with Hyper intense Diffusion
Weighted Imaging(DWI) in a 56 year old man without Neurofibromatosis1 who presented with generalized
tonic clonic seizures and loss of vision in right eye. Presence of hyperintenseDWI imaging of optic nerve makes
this case unique.Further details about diagnostic methods available with major emphasis on Magnetic
Resonance Imaging in adults is been done.
Keywords: GlioblastomaMultiforme,Gliomas,Imaging options of GBM,Optic Nerve Tumors,Optic nerve
thickening.
I. Introduction:
Glioblastoma Multiforme of the optic nerve a rare kind of cancer, usually slow-growing and found in
children. It is rarely found in individuals over the age of 20. It has also been associated with the genetic disorder
neurofibromatosis Type 1(NF1). Generally optic nerve gliomas are not hyperintense on diffusion weighted
imaging(DWI) .It is mostly seen in conditions of infarction and papilledema.The malignant optic glioma of
adulthood, on the other hand, is an extremely rare optic pathway tumor. Till 1990, only 30 cases were reported
in this century. In a review of literature in 2004 by Bettina Wabbles et al, 45 cases of adult malignant optic
gliomas have been described. Of these patients 51% were male, 49% females; the mean age at diagnosis was 54
years (median 59yrs, range 22 to 79yrs) .The most common sign of ONG is progressive loss of vision and may
lead to death in children.
II. Casepresentation
A 56 years old man presented with complaints of loss of vision in the right eye since 2days. Itwas not
associated with any pain or discharge. There was also a history of irritability and generalized tonic clonic
seizures since two to three years. His general physical examination was normal. Best corrected visual acuity in
the left eye was 6/24 .Anteriorsegment examination revealed sluggish pupillary reaction in both the eyes. On
fundus examination, no papilloedemaor any vessel occlusion was not seen bilaterally. The color vision on
Ishiara's chart was 5/14 in the left eye and none in the left eye. On confrontation test, temporal fields of both
right and left eyes were decreased.
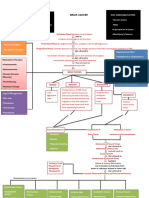
With this background, an MRI of the brain was done on 1.5 Tesla Siemens Essenzasystem. We found
that there was thickening of the right optic nerve (Fig1)showinghyperintense signal on T2W/ FLAIR
images(Fig2). The lesion appeared hypointense to isointense on T1W images and showed hyper intensity on
DWI . The right optic nerve appear expanded. The intracanalicular optic nerves appeared normal with thickening
of intraorbital part on right side(Fig3). The post contrast images (using 20ml of Gadodiamin revealed a small
(size) enhancing focus in posterior part of optic nerve on the right side. Rest of the lesion showed no significant
enhancement.
The patient was then taken up forbiopsy.Histopathological examination of the biopsy showed cerebral
tissue with varying degree of cellularity, characteristic cyto-morphology, abundant mitotic figures, increased
vascularity consistent with a diagnosis of glioblastomamultiforme.(Fig4)
III. Discussion
Gliomas account for 40-50% of all primary and metastaticintracranial tumors. Glioblastoma is the most
common typeof glioma.WHO 2000 classification grades astrocytic tumors fromgrade I to grade IV. WHO
Grade I tumor includes pilocyticastrocytoma, pleomorphic xanthoastrocytoma andsubependymal giant cell
astrocytoma. Other astrocytomasinclude diffuse astrocytoma (grade II), anaplasticastrocytoma(grade III) and
glioblastoma (grade IV).
Gliomas of the optic pathway are classified as (a) the relatively benign optic nerve glioma (typically
occurring in the pediatric age group) and (b) the malignant optic glioma of adulthood .Benign optic nerve
gliomas represent 4% of orbital tumors, 4% of intracranial gliomas, and 2% of intracranial tumors. They also
Glioblastoma Multiforme of Optic Nerve in Adultswith Hyperintense Dwi
www.iosrjournals.org 10 | Page
constitute two thirds of all primary optic nerve tumors. The benign optic nerve glioma is more common and is
considered a low grade Astrocytoma. From 10 to 38% of pediatric patients with optic nerve glioma have NF-1;
conversely, 15-40% of children with NF-1 have opticnerveglioma. Bilateral optic nerve gliomas are almost
pathognomonic for NF-1.
The malignant optic glioma of adulthood, on the other hand, is an extremely rare optic pathway tumor.
Till 1990, only 30 cases were reported in this century. In a review of literature in 2004 by Bettina Wabbles et al,
45 cases of adult malignant optic gliomas have been described. Of these patients 51% were male, 49% females;
the mean age at diagnosis was 54 years (median 59yrs, range 22 to 79yrs)
The sites of occurrence of malignant optic glioma in addition to the optic chiasma and the optic
nerve(s) were found to be the hypothalamus in 50% of patients, the temporal lobe in 22.5% and the basal
ganglia in 15%. Other more infrequent sites were the midbrain, parietal cortex, cerebellum and the cervical,
thoracic and lumbar subarachnoidalspaces.The malignant optic glioma of adulthood is classified pathologically
as either ananaplastic astrocytoma or a glioblastomamultiforme . In adults, malignant optic gliomas are rare and
are rapidly fatal visual pathway tumors.Anatomical classification forOPGs was proposed by Dodge et al in
1958, defining tumors asinvolving either the optic nerves alone (Stage 1), the chiasm with or without
nerveinvolvement (Stage 2), and the hypothalamus or other adjacent structures (Stage 3). The modified Dodge
classification further categories stage 1 into stage 1a (i.e. involvement of Single optic nerve), 1b(Bilateral Optic
nerve involvement), 1c (Cisternal segment of the optic nerve). Stage 2 is categorized into 2a (Central
chiasmatic) and 2b (Asymmetric chiasmatic).Stage 3a is optic tracts involvement, 3b is asymmetric tract
involvement. Stage 4 is diffuse posterior tract involvement and stage 4b is asymmetric posterior tract
involvement. The Hypothalamic involvement, leptomeningeal dissemination and associated neurofibromatosis
are also taken in account ( i.e. H+/- , LM+/- and NF1 +/-)
IV. Signs And Symptoms Of Optic Nerve Glioma
The most common sign of ONG is progressive loss of vision .Other includes: Changes in visual
acuity,proptosis may occur in later stages, involuntary eye movements, changes in appetite and sleep, neurologic
deficits, nausea, headache and vomiting. Rarely, childhood Optic Nerve Glioma can result in death.Symptoms
of an optic nerve glioma are caused by the tumor pressing against the nerves
.
V. Imaging Optic Nerve Gliomas:
5.1RADIOGRAPHY films used orbits imaged ANGIOGRAPHY not currently used examines blood vessels
around the orbit. COMPUTED TOMOGRAPHY great soft tissue definition ,also visualizes bony detail.
5.2MAGNETIC RESONANCE IMAGING is currently GOLD STANDARD in tumor imaging Superior
contrast resolution of soft tissue structures.Gliomas generally demonstrate high signal intensity on T2w images
and low signal intensity on T1w images, unless hemorrhage or calcification is present. Low grade astrocytoma
(WHO grade I and II) tend to be well defined, nonhemorrhagic and demonstrate little mass effect, vasogenic
edema or heterogeneity. Anaplastic astrocytomas (WHO grade III) are less well defined and demonstrate
moderate amount of mass effect, heterogeneity and edema with varying degrees of enhancement. Glioblastoma
(WHO grade IV) are poorly defined and often have considerable mass effect, vasogenic edema, hemorrhage and
heterogeneity. Irregular ring enhancement with nodularity and necrotic foci are typical of Glioblastoma .
5.3DIFFUSION WEIGHTED IMAGING (DWI)Apart from conventional and contrast MR, glioma grading have
been further attempted on the basis of DWI.It is a form of MR imaging based upon the diffusion of water
molecules within a voxel. The greater the cellularity, the greater the diffusion restriction, e.g. tumors.DWI can
be used for early identification of ischemic stroke,differentiation of epidermoid cyst from arachnoid cyst
,abscess,cortical lesions in CJD ,differentiation of herpes encephalitis from diffuse temporal gliomas,extent of
diffuse axonal injury ,active MS plaque (old plaques will not be bright) The signal intensity of gliomas on DWI
is variable (hyper-, iso-, or hypointense) but no case in literature has been reported with hyper intense DWI in
GBM of optic nerve.DWI and/or ADC maps may not be reliable to distinguish neoplastic cell infiltration from
peritumoral edema in patients with malignant glioma .
5.4MAGNETIC RESONANCE SPECTROSCOPY (MRS) MRI with non-invasive characterization of tissue
spectroscopic patterns of gliomas different than normal brain tissue potentially help in delineating tumour
spread VISUAL EVOKED POTENTIALS (VEPs) uses electroencephalography to evaluate conduction of
visual pathway from optic nerve through optic chiasm to occipital cortex useful in detecting anterior visual
pathway disturbance Findings indicate that results may not be reliable for children under 5 years old (peak age
for ONG).MRS shows increased Cho values in glioma with associated decrease in NAA/Cho and Cr/Cho ratios
with lipid-lactate peaks. One study has shown that specific metabolites, when standardized to water, are of
diagnostic value in the division of tumors into three categories. Specifically, the lactate/water ratio can be used
Glioblastoma Multiforme of Optic Nerve in Adultswith Hyperintense Dwi
www.iosrjournals.org 11 | Page
to differentiate GBMs, anaplastic astrocytomas, and low-grade tumors. The choline/water, choline/creatine, and
lactate/creatine ratios can be used to distinguish high-grade from low-grade tumors (5).
5.5MR PERFUSION STUDIESshows a correlation between relative cerebral blood volume and tumor grade.
5.6PET-CT SCAN Helpful in staging of the disease Effectively locates the tumour which is useful for treatment
Can assess tumour progression/recession following treatment Allows the possibility for a less invasive technique
that could easily replace more invasive ones PET-MRI SCAN Same application as a PET-CT scanner Better
soft tissue than CT More expensive.
VI. Figures:
Fig 1.optic nerve thickness on right side
Fig2.Hyperintense imaging of Optic Nerve
Fig3.Intraorbital optic nerve thickening
Glioblastoma Multiforme of Optic Nerve in Adultswith Hyperintense Dwi
www.iosrjournals.org 12 | Page
Fig 4.sMitotic Activity of GBM specimen
VII. Treatment Options
To halt the progression in vision loss or tumour growth .Types of treatment include: surgery,
chemotherapy and radiation therapy .CHEMOTHERAPY has now been determined as the best form of
treatment for all ages . If Chemotherapy fails, radiation therapy is then used.RADIATION THERAPY: Major
side effects of cranial irradiation: Mental retardation Endocrinopathies Cerebrovascular disease Fortunately side
effects are less common today due to treatments that are more precisely focused on Abnormal tissue .This
patient is on chemotherapy and under follow up.
VIII. Conclusion
Glioblastoma are very rare in adults compared to children.They are generally malignant in adults
resulting in loss off vision. GBM of optic nerve can present with hyperintense DWI .The possibility of tumor
cannot be excluded in differential diagnosis of hyper intense DWI in optic nerve apart from infarction and
edema. New imaging and treatment options can be used for earlier detection, more accurate treatment planning
and better prognosis.
References
[1]. Agamanoliz, D.P. (n.d.). Neuropathology. http://www.neuropathologyweb.org/ .
[2]. Auntminnie Case of the Day. (2008) Childhood Optic Nerve Glioma.
[3]. Carlson, A.H. (2007). Siemens Demonstrates Prototype MRI-PET System.
[4]. Gujar, S., Maheshwari, S., Bjorkman-Burtscher, I. &Sundgren, P. (2005) Magnetic resonance spectroscopy. Journal of Neuro-
opthalmology, 25 (3), 217-226.
[5]. Hollander, M.D., Fitzpatrick, M., OConnor, S.G., Flanders, A.E., Tartaglino, L.M. (1999). Optic Gliomas.Optic pathway glioma:
correlation of imaging findings with the presence of neurofibromatosis. American Journal of Neuroradiology, 22 , 1963-1969.
[6]. Listernick, R., Louis, D., Packer, R. &Gutmann, D. (1997) Optic Pathway Gliomas in Children with Neurofibromatosis 1: Consensus
Statement from the NF1 Optic Pathway Glioma Task Force . Annals of Neurology , 41 (2), 143-149. Liu, G.T. (2006). Optic gliomas
of the anterior visual pathway.
[7]. Dean BL, Drayer BP, Bird CR, et al. Gliomas: Classification with MR Imaging. Radiology 174: 411-415.
[8]. Richards J Hicks: Supratentorial adult brain tumors. In Clinical MRI Robert Edelman et al (third ed.) Philadelphia, PA. Saunders
Elsevier, 2006 pp 1098-1100.
[9]. Sugahara T, Korogi Y, Kochi M, et al. Usefulness of diffusion-weighted MRI with echo-planar technique in the evaluation of
cellularity in gliomas. J MagnResonImaging .
[10]. Taylor T, Jaspan T, Milano G, Gregson R, Parker T, Ritzmann T, Benson C, Walker D. Radiological classification of optic pathway
gliomas: experience of a modified functional classification system. The British Journal of Radiology, 2008.
[11]. Woiciechowsky C, Vogel S, Meyer R, Lehmann R. Magnetic resonance imaging of a glioblastoma of theoptic chiasm. J Neurosurg
83:923-925.
[12]. Taphoorn MJB, de Vries-Knoppert WAEJ, PonssenH,Wolbers JG. Malignant optic glioma in adults. J Neurosurg 1989;70:277-279.
[13]. Bilaniuk LT, Atlas SW, Zimmerman RA. The orbit.In: Lee SH, Rao KCVG, Zimmerman RA, eds. Clinical MRI and CT. New York,
NY: McGraw-Hill; 1992:119-19
Das könnte Ihnen auch gefallen
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Study The Changes in Al-Ahwaz Marshal Using Principal Component Analysis and Classification TechniqueDokument9 SeitenStudy The Changes in Al-Ahwaz Marshal Using Principal Component Analysis and Classification TechniqueInternational Organization of Scientific Research (IOSR)Noch keine Bewertungen
- Philosophical Analysis of The Theories of Punishment in The Context of Nigerian Educational SystemDokument6 SeitenPhilosophical Analysis of The Theories of Punishment in The Context of Nigerian Educational SystemInternational Organization of Scientific Research (IOSR)Noch keine Bewertungen
- Students' Perceptions of Grammar Teaching and Learning in English Language Classrooms in LibyaDokument6 SeitenStudents' Perceptions of Grammar Teaching and Learning in English Language Classrooms in LibyaInternational Organization of Scientific Research (IOSR)Noch keine Bewertungen
- Necessary Evils of Private Tuition: A Case StudyDokument6 SeitenNecessary Evils of Private Tuition: A Case StudyInternational Organization of Scientific Research (IOSR)Noch keine Bewertungen
- Project Based Learning Tools Development On Salt Hydrolysis Materials Through Scientific ApproachDokument5 SeitenProject Based Learning Tools Development On Salt Hydrolysis Materials Through Scientific ApproachInternational Organization of Scientific Research (IOSR)Noch keine Bewertungen
- The Effect of Instructional Methods and Locus of Control On Students' Speaking Ability (An Experimental Study in State Senior High School 01, Cibinong Bogor, West Java)Dokument11 SeitenThe Effect of Instructional Methods and Locus of Control On Students' Speaking Ability (An Experimental Study in State Senior High School 01, Cibinong Bogor, West Java)International Organization of Scientific Research (IOSR)Noch keine Bewertungen
- Effects of Formative Assessment On Mathematics Test Anxiety and Performance of Senior Secondary School Students in Jos, NigeriaDokument10 SeitenEffects of Formative Assessment On Mathematics Test Anxiety and Performance of Senior Secondary School Students in Jos, NigeriaInternational Organization of Scientific Research (IOSR)100% (1)
- Enhancing Pupils' Knowledge of Mathematical Concepts Through Game and PoemDokument7 SeitenEnhancing Pupils' Knowledge of Mathematical Concepts Through Game and PoemInternational Organization of Scientific Research (IOSR)Noch keine Bewertungen
- Development of Dacum As Identification Technique On Job Competence Based-Curriculum in High Vocational EducationDokument5 SeitenDevelopment of Dacum As Identification Technique On Job Competence Based-Curriculum in High Vocational EducationInternational Organization of Scientific Research (IOSR)Noch keine Bewertungen
- Geohydrological Study of Weathered Basement Aquifers in Oban Massif and Environs Southeastern Nigeria: Using Remote Sensing and Geographic Information System TechniquesDokument14 SeitenGeohydrological Study of Weathered Basement Aquifers in Oban Massif and Environs Southeastern Nigeria: Using Remote Sensing and Geographic Information System TechniquesInternational Organization of Scientific Research (IOSR)Noch keine Bewertungen
- Youth Entrepreneurship: Opportunities and Challenges in IndiaDokument5 SeitenYouth Entrepreneurship: Opportunities and Challenges in IndiaInternational Organization of Scientific Research (IOSR)100% (1)
- Need of Non - Technical Content in Engineering EducationDokument3 SeitenNeed of Non - Technical Content in Engineering EducationInternational Organization of Scientific Research (IOSR)Noch keine Bewertungen
- Child Mortality Among Teenage Mothers in OJU MetropolisDokument6 SeitenChild Mortality Among Teenage Mothers in OJU MetropolisInternational Organization of Scientific Research (IOSR)Noch keine Bewertungen
- Comparison of Psychological Variables Within Different Positions of Players of The State Junior Boys Ball Badminton Players of ManipurDokument4 SeitenComparison of Psychological Variables Within Different Positions of Players of The State Junior Boys Ball Badminton Players of ManipurInternational Organization of Scientific Research (IOSR)Noch keine Bewertungen
- Lipoproteins and Lipid Peroxidation in Thyroid DisordersDokument6 SeitenLipoproteins and Lipid Peroxidation in Thyroid DisordersInternational Organization of Scientific Research (IOSR)Noch keine Bewertungen
- Comparison of Selected Anthropometric and Physical Fitness Variables Between Offencive and Defencive Players of Kho-KhoDokument2 SeitenComparison of Selected Anthropometric and Physical Fitness Variables Between Offencive and Defencive Players of Kho-KhoInternational Organization of Scientific Research (IOSR)Noch keine Bewertungen
- Microencapsulation For Textile FinishingDokument4 SeitenMicroencapsulation For Textile FinishingInternational Organization of Scientific Research (IOSR)Noch keine Bewertungen
- Study of Effect of Rotor Speed, Combing-Roll Speed and Type of Recycled Waste On Rotor Yarn Quality Using Response Surface MethodologyDokument9 SeitenStudy of Effect of Rotor Speed, Combing-Roll Speed and Type of Recycled Waste On Rotor Yarn Quality Using Response Surface MethodologyInternational Organization of Scientific Research (IOSR)Noch keine Bewertungen
- Core Components of The Metabolic Syndrome in Nonalcohlic Fatty Liver DiseaseDokument5 SeitenCore Components of The Metabolic Syndrome in Nonalcohlic Fatty Liver DiseaseInternational Organization of Scientific Research (IOSR)Noch keine Bewertungen
- Comparison of Explosive Strength Between Football and Volley Ball Players of Jamboni BlockDokument2 SeitenComparison of Explosive Strength Between Football and Volley Ball Players of Jamboni BlockInternational Organization of Scientific Research (IOSR)Noch keine Bewertungen
- Advancing Statistical Education Using Technology and Mobile DevicesDokument9 SeitenAdvancing Statistical Education Using Technology and Mobile DevicesInternational Organization of Scientific Research (IOSR)Noch keine Bewertungen
- Comparative Effect of Daily Administration of Allium Sativum and Allium Cepa Extracts On Alloxan Induced Diabetic RatsDokument6 SeitenComparative Effect of Daily Administration of Allium Sativum and Allium Cepa Extracts On Alloxan Induced Diabetic RatsInternational Organization of Scientific Research (IOSR)Noch keine Bewertungen
- Application of Xylanase Produced by Bacillus Megaterium in Saccharification, Juice Clarification and Oil Extraction From Jatropha Seed KernelDokument8 SeitenApplication of Xylanase Produced by Bacillus Megaterium in Saccharification, Juice Clarification and Oil Extraction From Jatropha Seed KernelInternational Organization of Scientific Research (IOSR)Noch keine Bewertungen
- Auxin Induced Germination and Plantlet Regeneration Via Rhizome Section Culture in Spiranthes Sinensis (Pers.) Ames: A Vulnerable Medicinal Orchid of Kashmir HimalayaDokument4 SeitenAuxin Induced Germination and Plantlet Regeneration Via Rhizome Section Culture in Spiranthes Sinensis (Pers.) Ames: A Vulnerable Medicinal Orchid of Kashmir HimalayaInternational Organization of Scientific Research (IOSR)Noch keine Bewertungen
- A Review On Refrigerants, and Effects On Global Warming For Making Green EnvironmentDokument4 SeitenA Review On Refrigerants, and Effects On Global Warming For Making Green EnvironmentInternational Organization of Scientific Research (IOSR)Noch keine Bewertungen
- Investigation of Wear Loss in Aluminium Silicon Carbide Mica Hybrid Metal Matrix CompositeDokument5 SeitenInvestigation of Wear Loss in Aluminium Silicon Carbide Mica Hybrid Metal Matrix CompositeInternational Organization of Scientific Research (IOSR)Noch keine Bewertungen
- Factors Affecting Success of Construction ProjectDokument10 SeitenFactors Affecting Success of Construction ProjectInternational Organization of Scientific Research (IOSR)Noch keine Bewertungen
- Research Analysis On Sustainability Opportunities and Challenges of Bio-Fuels Industry in IndiaDokument7 SeitenResearch Analysis On Sustainability Opportunities and Challenges of Bio-Fuels Industry in IndiaInternational Organization of Scientific Research (IOSR)Noch keine Bewertungen
- Parametric Optimization of Single Cylinder Diesel Engine For Specific Fuel Consumption Using Palm Seed Oil As A BlendDokument6 SeitenParametric Optimization of Single Cylinder Diesel Engine For Specific Fuel Consumption Using Palm Seed Oil As A BlendInternational Organization of Scientific Research (IOSR)Noch keine Bewertungen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Adults Brain Tumor in Cipto Mangunkusumo General Hospital A Descriptive EpidemiologyDokument5 SeitenAdults Brain Tumor in Cipto Mangunkusumo General Hospital A Descriptive EpidemiologyHarun NANoch keine Bewertungen
- Brain Tumor Segmentation and Detection Using Deep LearningDokument5 SeitenBrain Tumor Segmentation and Detection Using Deep Learningmohammad arshad siddiqueNoch keine Bewertungen
- Mufon Ufo JournalDokument21 SeitenMufon Ufo JournalSAB78Noch keine Bewertungen
- "Confessions of A Cyberchondriac" - Reading Activity For ESL ClassesDokument1 Seite"Confessions of A Cyberchondriac" - Reading Activity For ESL ClassesGustavo Pedrotti GrittiNoch keine Bewertungen
- Valentino Rački, Igor Vlatković, Mila Prskalo Daniela PetrićDokument1 SeiteValentino Rački, Igor Vlatković, Mila Prskalo Daniela PetrićIgor VlatkovićNoch keine Bewertungen
- Project Stage Ifinal PDFDokument33 SeitenProject Stage Ifinal PDFNadeem A. KhanNoch keine Bewertungen
- Impact of Excessive Mobile Phone Usage On Human JCSB 1000235Dokument5 SeitenImpact of Excessive Mobile Phone Usage On Human JCSB 1000235nidNoch keine Bewertungen
- Neurorehabilitation in Neuro-Oncology 2019 E-BookDokument254 SeitenNeurorehabilitation in Neuro-Oncology 2019 E-BookWoffe SoloNoch keine Bewertungen
- Siemens Healthineers Magnetom Flash 71 MR Spectroscopy in Neuroimaging Ryner 1800000005860250Dokument10 SeitenSiemens Healthineers Magnetom Flash 71 MR Spectroscopy in Neuroimaging Ryner 1800000005860250Ana Sofia PintoNoch keine Bewertungen
- Management of Patients With Oncologic or Degenerative Neurologic DisordersDokument84 SeitenManagement of Patients With Oncologic or Degenerative Neurologic DisordersDwiKrismaPratabaNoch keine Bewertungen
- REIRRADIATIONBOOKDokument167 SeitenREIRRADIATIONBOOKGabriela Silva MartinsNoch keine Bewertungen
- A Case Series On Meningioma Based On Who Grading SystemDokument15 SeitenA Case Series On Meningioma Based On Who Grading SystemIJAR JOURNALNoch keine Bewertungen
- Musawi 23Dokument22 SeitenMusawi 23Full MarksNoch keine Bewertungen
- 10 1016@j Jconrel 2017 09 001Dokument88 Seiten10 1016@j Jconrel 2017 09 001ummi isnainiNoch keine Bewertungen
- Pituitary TumorsDokument6 SeitenPituitary Tumorsapi-271668042Noch keine Bewertungen
- Craniopharyngioma-The Anesthetic, Critical Care and Syrgical Challenges in The Managemnet of CPNDokument5 SeitenCraniopharyngioma-The Anesthetic, Critical Care and Syrgical Challenges in The Managemnet of CPNpitriaNoch keine Bewertungen
- Cogni Psych PrelimsDokument30 SeitenCogni Psych PrelimsJuvy IringanNoch keine Bewertungen
- Brain Cancer Concept MapDokument3 SeitenBrain Cancer Concept MapIced Coffee100% (4)
- Neurological DiseasesDokument91 SeitenNeurological Diseasesrabia khalidNoch keine Bewertungen
- Respiratory Asthma: Common Signs and Symptoms of Asthma IncludeDokument18 SeitenRespiratory Asthma: Common Signs and Symptoms of Asthma IncludeAen Panda BebeNoch keine Bewertungen
- Surgery MCQ-1Dokument35 SeitenSurgery MCQ-1Fan Eli100% (15)
- Glioma Difuso de La Linea MediaDokument9 SeitenGlioma Difuso de La Linea MediaJOHN LOPERANoch keine Bewertungen
- Final-Exam Neurosurgery - 3-VersionDokument6 SeitenFinal-Exam Neurosurgery - 3-VersionMAMA LALANoch keine Bewertungen
- From First Symptoms To Diagnosis: Initial Clinical Presentation of Primary Brain TumorsDokument7 SeitenFrom First Symptoms To Diagnosis: Initial Clinical Presentation of Primary Brain TumorsMohammad AamirNoch keine Bewertungen
- Research Paper On MriDokument7 SeitenResearch Paper On Mriibhuglbkf100% (3)
- Daftar Pustaka: Jurnal Pendidikan Khusus, 5 (2), 83-93Dokument3 SeitenDaftar Pustaka: Jurnal Pendidikan Khusus, 5 (2), 83-93donatNoch keine Bewertungen
- Musawi 24Dokument22 SeitenMusawi 24Full MarksNoch keine Bewertungen
- Radiation Oncology Imaging and Treatment (2013) (PDF) (UnitedVRG)Dokument1.310 SeitenRadiation Oncology Imaging and Treatment (2013) (PDF) (UnitedVRG)MariusNoch keine Bewertungen
- Research Project On CancerDokument13 SeitenResearch Project On Cancerapi-549770007Noch keine Bewertungen
- Evaluation of Headache in Adults - UpToDateDokument18 SeitenEvaluation of Headache in Adults - UpToDateSebastianNoch keine Bewertungen