Beruflich Dokumente
Kultur Dokumente
TEMPLATE
Hochgeladen von
runnermn0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
88 Ansichten21 Seiteneducation
Copyright
© © All Rights Reserved
Verfügbare Formate
DOCX, PDF, TXT oder online auf Scribd lesen
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldeneducation
Copyright:
© All Rights Reserved
Verfügbare Formate
Als DOCX, PDF, TXT herunterladen oder online auf Scribd lesen
0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
88 Ansichten21 SeitenTEMPLATE
Hochgeladen von
runnermneducation
Copyright:
© All Rights Reserved
Verfügbare Formate
Als DOCX, PDF, TXT herunterladen oder online auf Scribd lesen
Sie sind auf Seite 1von 21
ASSOCIATE DEGREE NURSING ASSESSMENT NAME: _Alex Kortscheff________
MARSHALLTOWN COMMUNITY COLLEGE DATE: ______________________
Directions: Select one of the patients from your clinical rotation to complete the head to toe assessment form. This may be the patient you are assigned to in
the first or second week of clinical. Note the format of head to toe, which provides steps for an integrated, efficient, logical and complete assessment. The
assessment section is to be typed in the format below, with the grading rubric attached and submitted to your clinical instructor.(hard copy or electronic) The
grade will be reflected in the 10% section of your Medical-Surgical II course class activities and quizzes.
Section I:
SUBJECTIVE DATA
OBJECTIVE DATA
ASSESSMENT
GENERAL
Cultural considerations
Family relationships
Religious beliefs
Body image
General appearance: personal hygiene, odors, manner
of dress, stature and movement
Other:
VITAL SIGNS
Fever, chills, orthostatic signs/symptoms,
palpitations, pain scale
Temperature: _________, _________
Pulse: _________, _________
Respiration: _________, _________
Blood pressure: _________, _________
Auscultatory gap? __________________
Orthostatic pressures: L______S______S______
Pain (5
th
VS): ___________________
Other:
SKIN
Itch, rash, lesions, boils, color changes,
dryness, odors, masses, ulcers (where,
how long)
Color: pink, cyanotic, redness, yellow, pallor,
mottled. Where? _______________
Moisture: dry, moist, scaly. Where? ________
Temp: hot, cool, cold, warm
Texture: rough, smooth
Turgor: normal, decreased, edematous
Lesions: rash, moles, sores, warts, eruptions, scars,
ulcers (complete description), location
Braden Scale: __________________________
IV/PICC/Central Line: site (date started), tubing,
solution, change dates, dressing changes
Other:
2
SUBJECTIVE DATA
OBJECTIVE DATA
ASSESSMENT
NAILS
Recent nail changes or trauma, nail biting
Color: pink, cyanotic, pale
Shape: normal, clubbed
Other: clean, short, smooth, torn cuticles,
material under nails
Toenails: thick, long, need podiatric attention
Other:
HEAD
Trauma, headache, vertigo, hair loss, scalp
itchy
Size: normal, abnormal
Symmetry: normal, abnormal
Hair: medium, coarse, fine, dull, glossy,
clean, greasy, normal or abnormal
distribution
Scalp: clean, flakes present
Tenderness: absent, present
Lesions: absent, present
Other:
FACE AND SINUSES
Tenderness, pain
Symmetry: normal or abnormal at rest. Normal or
abnormal with movement
Sinuses: nontender, tender
Other:
EYES
Loss of vision, glasses, contacts, glaucoma,
cataracts, discharge, redness, itching,
photophobia, pain, burning, diplopia,
blurring, tearing
Visual acuity: Legally blind? __________
Read news/large print? _____
Pupils: equal, unequal, react to light,
accommodate
Sclera: white, jaundice, other _________
Conjunctiva: pink, pale, other _____________
Eyes: dry, moist, red, discharge present,
periorbital edema, blood vessels
visible in eyes, lid, lashes
Ophthalmic exam:
Other:
3
SUBJECTIVE DATA
OBJECTIVE DATA
ASSESSMENT
EARS
Deafness, tinnitus, pain, discharge, itching,
infections, problems with wax.
Does resident have a hearing aid? Does
resident wear a hearing aid?
Position: external ear, normal, abnormal
Shape: normal, abnormal
Auditory: HOH left ear _______, right ear ____
Deaf left ear _____, right ear _______
Normal left ear _____, right ear _____
Cerumen: amount, color, consistency, removal
Otoscopic exam: tympanic membrane
Other:
NOSE
Decreased smell, nose bleeds, dryness,
discharge, pain, obstruction, frequency of
colds
Discharge: absent, present
Patency: adequate, decreased, nasogastric tube ,
nasal cannula present
Other:
MOUTH
Bleeding gums, sore throat, dental
problems, pain, post-nasal drip, dentures,
bridges, dryness, voice change,
hoarseness, odors, lesions.
Describe dentures, location of missing
teeth, etc.
Lips: pink, red, cyanotic, dry, moist, swollen,
lesions
Oral cavity: dry, moist, phlegm present
Gums: pink red, swollen, sensitive, firm, bleed
easily, pale
Teeth: some missing, all missing, broken teeth,
decayed teeth, food or debris on teeth
Tongue: red, coated, smooth, sore, cracked,
swollen, patches, discolored
Dentures: not worn, food or debris on dentures, ill
fitting, broken
Other:
NECK
Stiff, pain difficulty swallowing, fullness,
lumps, swelling
ROM: full, limited, stiff
Nodes: nonpalpable, palpable
Carotid: normal, diminished, bounding, equal
bilaterally, bruit absent, bruit present
Masses: absent, present
Trachea: midline, deviated, tracheostomy
Other:
4
SUBJECTIVE DATA
OBJECTIVE DATA
ASSESSMENT
RESPIRATORY
Cough, sputum, pleurisy, hemoptysis,
dyspnea, pain, cyanosis, wheezing
Shape: normal, abnormal, barrel chest
Respiration: labored, effortless
Breath sounds: wheezes, rales, crackles, location
Cough: productive, nonproductive, sputum color
Cyanosis: lips, nails
Chest tube: _____________ Suction: __________
Sleep Apnea: ___________BIPAP ___ CPAP _____
Oxygen _____ liter flow _______ O2 Sats ________
Other:
CARDIOVASCULAR
Dyspnea, pain, orthopnea, palpitation,
claudication, murmur, edema, weight gain,
phlebitis, cold feet/hands, hypertension,
thrombophlebitis, varicose veins
Auscultation: apical pulse ________, regular,
Irregular, murmur, pulse deficit
Jugular vein: normal, distended
Legs/feet: hot, cold, cool, hair distribution, pulses,
normal or abnormal, mottled, cyanotic,
varicose veins, capillary refill _______
edema scale (________), Homans ____
Weight: gains, 1kg gain = 1 L. fluid retained
Telemetry: ____________ Rhythm: ___________
Other:
BREAST AND AXILLAE
Discharge, pain, lump, suture lines,
mastectomy, last mammogram, breast self
exam, family history
Appearance: dimpling, mastectomy, retraction
Nipples: normal, abnormal position, discharge
Palpation: normal, masses, tender
Axilla: clear, rash, moist, dry
Nodes: normal, palpable, tender
Other:
5
SUBJECTIVE DATA
OBJECTIVE DATA
ASSESSMENT
GASTROINTESTINAL
Nausea, vomiting, dysphagia, heartburn,
melena, hematemesis, bowel changes,
laxative/enema use, diarrhea,
constipation, incontinence, clay colored
stool, hernia, hemorrhoids, pain, ascites,
flatulence
Abdomen: distended, scars, hernia, varicosities,
masses, ileostomy, colostomy,
gastrostomy, feeding tube
Auscultation: bowel sounds absent, normo, hypo, or
hyperactive, Borborygmi
Percussion: intensity, pitch, quality, tympanic, dull
Palpation: normal, soft, rigid, guarding, masses,
rebound tenderness
Last BM: __________ Frequency, color, consistency
Other:
NUTRITIONAL
Diet and nutrition related conditions, food
intolerance, appetite
Cultural diet customs
Height: __________ Weight: __________
Weight changes: ______ Daily wt. ______
Diet: ______________________________
Enteral feeding: _____________________
Parenteral feeding: ___________________
Lab measurements: _______________
Dietary consult
Other:
GENITOURINARY
Frequency, nocturia, dysuria, hematuria,
incontinence, oliguria, hesitancy, urgency,
frequency, pain, changes in stream, history
of stones or STD
Indwelling urinary, ureterostomy, suprapubic catheter
Catheter lumen size ________, bulb size ________.
Urine color, clarity, odor
Urine Output per hour: ____________________
Male genitalia: penis, scrotum, prostate
Female genitalia: skin, labia, perineum
Other:
6
SUBJECTIVE DATA
OBJECTIVE DATA
ASSESSMENT
MUSCULOSKELETAL
Muscle pain, cramps, weakness, trauma,
tenderness, tremors, joint
pain/swelling/stiffness, ROM, numbness,
nodules, deformities.
Can:
turn over in bed? ___________
bear weight? ______________
ambulate independently? _______
raise arms above head? _________
move from place to place? _______
Size: normal, atrophy, hypertrophy
Strength: normal, abnormal
Bones: straight, shortened, thickened,
deformed
Joints: normal, tender, swollen, crepitation,
hot, red
Posture: normal, abnormal, spine curves,
ROM: full, limited, contractures (where)
Ambulation: none, independent, requires assistance
Fall Prevention/Risk:
Other:
NEUROLOGICAL
Headache, epilepsy, tics, vertigo, loss of
consciousness, syncope, tremor,
uncoordinated, numbness, aphasia,
dysarthria,, paresthesia, ataxia, memory
loss, balance, paralysis
Coordination: touch fingers to nose?
Gait: normal, abnormal, use of w/c,
walker, cane, non-ambulatory
Speech: normal, slurred, soft, hesitant
Paralysis: R side UE ______ LE _________
L side UE ______ LE _________
Weakness: R side UE ______ LE _________
L side UE ______ LE _________
Other:
ENDOCRINE
Polydipsia, polyphagia, polyuria,
hypoglycemia, , peripheral neuropathy,
parasthesias, tetany, dry skin, weight loss,
increased appetite
Diabetes: type I or II, skin lesions
FSBS: ______________________________
Thyroid: Exophthalmos, goiter, appetite, weight
loss/gain, dry skin, Trousseaus,
Chevosteks
Adrenal: Hirsutism, striae, moon face, truncal obesity,
hyperpigmentation
Chronic steroid effects:
Other:
7
SUBJECTIVE DATA
OBJECTIVE DATA
ASSESSMENT
MENTAL HEALTH
Nervousness, depression, suicidal,
excitable, hostile, anxious,
hyperventilation, insomnia, illusions,
memory impairment, hallucinations,
delusions
Orientation: person, place, time, date
Memory: recent; normal or impaired, long term;
normal or impaired
Judgment: good, impaired
Expression: normal, depressed, anxious, apathy,
anger, mood, affect, speech, eye contact
Thought process: coherent, incoherent, confused
Perception: alert, normal, abnormal
Reasoning: concrete, abstract
Insomnia
Other:
Section II: Medication Review
A. Medication List: List precisely as ordered by physician all medications scheduled and PRN whether given by student or not.
B. Medications are then to be integrated throughout your assessment as they apply/relate to the individual assessment areas. All medications from the
medication list (above) should be evident in your assessment.
C. Identify evidence of desired effects as well as noted side effects specific to the medication in your assessment when applicable.
Section III: Laboratory and Diagnostic Review
A. Laboratory and diagnostic information and rationale should be integrated into the appropriate systems. (Example: Nutritional note total protein, pre-
albumin, potassium, etc.)
Section IV: Nursing Diagnosis List
A. On a separate sheet of paper, put your complete list of prioritized nursing diagnosis related to the patient problems you have identified in your assessment of
the patient.
B. Each nursing diagnosis must be written using this format: Patient Problems related to Etiology as manifested by Signs & Symptoms
Section V: Content Accuracy
A. Grammar, Spelling, Terminology
B. Neatness, Organization
Section VI: References
A. APA Format, books, journals, scholarly internet sites, no older than 5 years and minimum 3 sources.
8
Section VII: Assessment submitted on designated day
Medication
Generic/Brand
Classification
Nursing
Implications (3)
Dosage Route
Schedule
/Time
Desired Effect Side Effects (3) Teaching (3)
Lovenox
Enoxaprin
Anticoagulant
1. History of stroke or surgery.
2. Bleeding or bruising.
3. Blood tests.
30mg Sub Q 0900
Daily
Prevents clots,
treats Acute
MI, Blood
thinner.
1. Allergic RXN,
itch, hives.
2. Fever
3. CP, SOB
1. Advise patient to report
symptoms of unusual
bleeding, bruising, dizziness,
itching, rash, fever,
swelling, or difficulty
breathing.
2. Instruct patient not to
take aspirin or NSAIDs
without consulting.
3. Instruct patient to take
full dose as scheduled.
Warfarin Sod.
Coumadin
Anticoagulant
1. Assess for signs of bleeding
and hemorrhage.
2. Assess for evidence of
additional or increased thrombosis.
3. Monitor PT, INR, hepatic
function, CBC
2mg +
1mg=
3mg
Dose
PO 1200
Daily
Prevention of
Thromboembolic
events
1. Bleeding
2. Cramps
3. Fever
1. Teach take medication as
Directed.
2. Review foods high in
vitamin K, limit intake, may
cause PT levels to fluctuate.
3. Caution to avoid IM
injections and activities
leading to injury.
EC Aspirin Tab
Ecotrin
Antipyretic
Non-opoid
Analgesic
1. Once a day with food, do not
Crush
2. Assess pain and limited
Movement
3. Assess fever and note signs
325
Mg
PO 0800 Analgesic reduces
Inflammation
1. GI Bleed
2. Dyspepsia,
Nausea
3. Allergy
9
Aspirin Chew Tab
NSAIDS
Antirheumatic
Platelet Aggreg-
ation Inhibitor
4. Do not crush
5. Drink 8oz water
6. Monitor blood levels
81 mg PO 0900
Daily
Treats pain, fever,
Arthritis, inflamm-
ation (MI)
1. Severe stomach
pain.
2. Bloody vomit,
Consistency
of coffee grounds
3. Allergy, itch,
hives.
Docusate Sodium
Colace Cap
Stool Softener
1. Assess bowel distention,
sounds, and function.
2. Asses stool color
3. Encourage fluids
100
Mg
PO 0900
BID
Softening and
passing of stool.
Incorp water.
1. Throat irritation
2. Mild cramping
3. Allergy, rash
Metoprolol Suc
XL Tab
Toptol XL
Lopressor
Beta Blocker
1. Take as directed; Take
with or after meal
Do not crush
2. Monitor BP, ECG, and Pulse
omit if SBP <80, symptomatic
3. Monitor prescription refills
25 mg PO 0900
Daily
Treats increased
BP and Angina
Pectoris (CP),
decreases
repeat heart
attack, heart
failure, and
cardiovascular
mortality.
1. Fatigue,
Weakness,
Constipation
2. Fever, chills
3. CP, CHF,
Bradycardia,
Pulmonary
Edema
Ondansetron
Zofran
SSRI
Antiemetic
1. Assess pain and swelling of
Stomach and bowel
2. Assess for allergies
3. Assess for nausea
4mg PO PRN
QID
Treats nausea and
vomiting
1. Allergy
2. Fever
3. Tachycardia
10
Omeprazole
Prilosec
Proton Pump
Inhibitor
1. Once daily before meals;
Do not crush.
2. Monitor CBC Differential
3. Assess epigastic and
Abdominal pain, blood in
Stools, emesis, gastric aspirate
40mg PO 0600
AC
Break-
fast
Treats heart burn,
Stomach ulcers,
GERD, acid
1. Allergy
2. CP
3. Blister, rash
Mirtazapine Tab
Remeron
Antidepressant
Tetracyclic
1. Give 1 tab by mouth at
Bedtime
2. Assess mental status
3. Monitor BP and pulse rate
During therapy
15mg PO 1900 Antidepressant
action after
Several weeks
1. Drowsiness
2. Constipation,
Dry mouth
3. Weight gain
Hydrocodone /
ADAP
Vicoden
Opioid / non-
Opioid
Analgesic
Combination
1. Twice daily, omit if sleepy;
Max ADAP 4gms/24 hrs
2. Assess BP, respirations before
And during (<10/min)
3. Assess bowel function,
constipation
5/500
Tab
PO 0800
1900
BID
Decreases
Severity of
Moderate pain,
Suppresses
Cough reflex
1. Confusion,
Dizziness,
Sedation
2. Constipation
3. Hypotension
Miralax Powder
Polyethylene
Glycol 3550
Laxative
1. Mix 17gm in 4oz water 2 times
Daily
2. Assess color, consistency,
and amount of stool
3. Assess abdominal distention,
Bowel sounds and function
17gm
In
4oz
Water
PO 0800
1900
Evacuation of GI
tract without
systematic
anticholinergic
effects
1. Abdominal
Bloating
2. Cramping,
Flatulence
3. Nausea
1. Instruct to drink 240ml every 10
min unit 4L consumed or fecal
discharge is clear and free of solid
matter.
2. Instruct to consume bulk
and fiber rich foods.
3. Consult with
provider if constipation
is not relieved by dose
11
Novolin N NPH
Humulin Insulin
Isopha
Pancreatic
Hormone
1. 18u morning, 14 u evening
2. Assess allergy
Sub Q Control hyper-
glycemia in
Diabetics,
Intermediate
Acting
1. Hypoglycemia
2. Allergy
3. Erythemia
swelling
Acetaminophen
Tylenol
Antipyretics,
non-opioid
analgesics
1. Asses overall health status
and alcohol usage before
given, may have higher risk of
hepatotoxicity.
2. Assess amount, frequency,
and type of drugs taken to
self-medicate.
3. Assess pain type, location, and
intensity prior and 30 min
after.
650mg PO Q4hrs
PRN
Treats mild pain
and fever.
1. Hepatic failure
2. Allergy
3. Renal failure
1. Advise to take as
directed no more that
recommended. Chronic
excessive use >4g/day
may result in
hepatotoxicity, renal
failure, or cardiac
damage. Adult should
use no longer than 10
days, Children 5 days.
2. Advise avoid alcohol if
taken more than the
occasional 1-2 doses.
3. Consult with provider if
discomfort or fever is
not relieved by dose.
Normal Saline
Flush
4. Assess IV catheter site for
Infiltration or signs of infection.
5. Assess hydration and
electrolyte consumption.
6. Assess for evidence of
Thrombosis.
2ml IV 1000
2200
BID
Prevent IV
catheters from
becoming
blocked and
removed
medication that
may be left at site.
1. Allergy
2. Irritation at
injection site
3. infiltration
1. Do not share medication with
others.
2. Advice to take as direct for best
possible benefit.
3. Store at room
temperature, do not freeze or
store in bathroom. Keep
away from children and pets.
12
Nicotine
Transdermal
Nicoderm CQ
Smoking
Deterrents
1. Asses history, number of
cigarettes smoked daily, patterns,
content of preferred brand.
2. Assess symptoms of smoking
withdrawal.
3. Evaluate progress in smoking
cessation
14mg Top
Patch
1000
Daily
Smoking deferent
used to help
quit smoking.
1. Headache
2. Insomnia
3. Burning at patch
site
1. Explain necessity of
immediate cessation of
smoking upon
initiation and throughout
therapy.
2. Encourage to
participate in smoking
cessation program while
using this product.
3. Instruct proper disposal,
keep out of reach of children
and pets.
4. 4.
13
5. 5.
Medication
Generic/Trade
Classification
Nursing
Implications (3)
Dosage Route
Schedule
/Time
Desired Effect Side Effects (3) Teaching (3)
Prenatal
Prenatal u
Vitamin
1.If patient has difficulty swallowing
offer chewable option.
2. Offer vitamin with a snack.
3. May cause constipation.
106.5u
/
1mg
Caps
PO Daily
Source of
essential
vitamins and
minerals.
1. Constipation.
2. Diarrhea
3. Upset stomach
1. Drink plenty of water.
2. Include physical activities in
daily routine.
3. Include fiber in diet.
Moms Scheduled
Docusate Sodium
Colace
Stool softener
1.Assess for abdominal distention,
and presence of bowel sounds.
2. Administer with a full glass of
water or juice.
3. This medication does not
stimulate intestinal peristalsis.
100mg
CAPS.
PO DAILY
2100
Prevent
constipation
1.Throat irritation
2. Mild cramps.
3. Rashes.
1. Laxatives should only for a
short time.
2. Encourage patients to use
other forms of bowel
regulation.
3. Advise patients not to use
laxatives when abdominal pain or fever
is present.
Moms PRN
acetaminophen
nonopioid
Tylenol
Analgesic.
1.Assess overall health status and
alcohol usage before
administering.
2.Assess type, location, and
Intensity of pain before
administration.
3. May alter results of blood
glucose monitoring.
650mg
Dose.
(2x
325mg
Tab)
PO PRN
Q6hrs
Relieve Mild
Pain (1-3),
Fever
1. Hepatic failure.
2. Renal failure.
3. Neutropenia.
1.Avoid alcohol use while
taking medication.
2. Caution patients to check
labels of all over the
counter medication
3.Call doctor if pain is
unrelieved by routine dosage.
14
Ibuprofen
Advil, Motrin
Non opioid
Analgesic.
1.Assess pain prior to
administration
and 1-2 hour after administration.
2.May cause prolonged bleeding
time.
3.Assess for rhinitis, asthma, and
urticarial as these increase risk
for developing hypersensitivity.
600mg/
Tab
PO
PRN
Q6hrs
Relieve
Mild
Pain (1-3),
Inflammation,
Fever.
1. Dizziness.
2. Blood dyscrasias.
3. Prolonged bleeding
time.
1.Take Ibuprofen with a full
Glass of water.
2.Avoid concurrent use alcohol,
aspirin, acetaminophen.
3.Inform health care
professional of medication
regimen prior
treatment or surgery.
hydrocodone-
acetaminophen
Norco
Opioid agonist
1.Assess blood pressure, pulse and
respiration before administration.
2. Assess bowel function
periodically.
3. Explain therapeutic value of
medication prior to administration
to enhance analgesic effect.
2 tab
Dose
of
(5-325
mg /
tab)
PO PRN
Q4hrs
Relieve
Moderate
Pain (4-6)
1. Drowsiness.
2. Dizziness.
3. Confusion.
1.Avoid alcohol use while
Taking medication.
1.Advise patient to change
Position slowly to minimize
Orthostatic hypotension.
3.Do not drive or operate
Heavy machinery while taking
medication.
oxycodone-
acetaminophen
Percocet
Opioid-analgesic
1.Assess type, location, and
intensity of pain prior to and 1
hour after administration.
2.Patients taking controlled-release
tablets may require additional
short-acting opioids.
3. Assess bowel functioning
routinely.
5-325
mg/tab
(2 tabs)
PO PRN
Q4hrs
Relieve
Moderate
Pain (7-10)
1. Confusion.
2. Sedation.
3. Hallucination.
1.Instruct patient on how and
when to ask for medication.
2. Caution patient that
controlled-release
oxycodone is a potential drug
of abuse.
3. Advise patients to avoid
concurrent abuse of alcohol.
Aluminum-
Hydroxide-
Magnesium-
Hydroxide-
Simethicone
Mylanta
1.Administer with meals or
immediately afterwards.
2.Administer dose at bedtime to
prolong effect.
3.Assess for epigastric and
abdominal pain.
200-
200-
20mg/
5ml
(15ml
Dose)
Oral
Susp.
PRN
TID
Treatment of
Heartburn and
Indigestion.
1. Confusion.
2. Hallucinations.
3. Headache
1. Take medication as directed.
2. Inform patients that
Smoking interferes with
action of histamine
antagonists.
3. Report onset of black tarry
stools.
15
Anti-ulcer.
Benzocaine-
menthol
20-0.5% topical
Spray
Dermoplast
1.Can cause methemoglobinemia
which is life threatening.
2.Do not use medicine on a child
younger than two years.
3. Overdose can cause fatal side
effects.
20-
0.5%
Topical
Spray
PRN Relieve
perineal
discomfort.
1.Dermatitis
2. Urticaria
3. Edema
1.Use the smallest amount of
Dosage needed to numb area.
2. Ask doctor before using
medication if you are
pregnant.
3. Call doctor if pain persists
for more than three days.
Witch hazel-
glycerin Pad
Tucks
Analgesic.
1.Clean affected area with warm
water and soap.
2. After application, discard pad.
3. Dry area by bloating or tissue
before application.
1 Dose
Each
Topical PRN
Q2hrs
Relieve
perineal
discomfort.
1.Nausea
2.Diarrhea
3.Vomiting
(if it enters blood)
1. Do not use more than
directed.
2. Ask doctor if discomfort
does not Improve in 7 days.
3. Stop use if bleeding occurs.
lansinoh,
Lanolin
Ointment
Analgesic.
1.Educate patient on other ways to
avoid dry skin.
2.Educate mothers than lanolin
promotes healing.
3.Small pea-sized amount is
Needed for each nipple.
N/A Topical PRN Decrease breast
Discomfort.
Apply to sore /
Cracked nipples.
1. Burning
2. Stinging.
3. Redness
1.Do not store medication at
temperature higher than 120.
2. No need to wash off
ointment before breastfeeding.
3. Proper latching technique
can help prevent sore nipples.
Babys Meds:
Erythromycin
Emgel
Anti-infective
1.Do not confuse erythromycin with
Azithromycin.
2. May cause increased serum
bilirubin, AST, ALT.
3.May cause false increase of
urinary catecholamines.
Thin
Strip.
5mg/
gm
Ocular,
Both
eyes
Once,
< 24
hours
after
birth.
Prevent
infection
1. Nausea
2. Vomiting.
3. Diarrhea
1. Inform doctor of signs of
allergies.
2. Notify doctor if side effects
persist.
3. Report signs of super
infections.
16
Phytonadione
Vitamin K
Vitamin
1. Monitor side effects and adverse
reactions.
2. Monitor frank and occult bleeding.
3. Parenteral route is preferred.
0.5-
1mg
IM Once.
Within
one
hour of
birth.
Prevent
Hypo-
thrombinemia.
1. Gastric upset.
2. Allergic reactions.
3. Pain at injection site.
1. Do not take over the
counter medications without
doctors order.
2. Cooking does not alter
vitamin K.
3. Avoid IM injections and
activities leading to injuries.
Hepatitis B
Vaccine
engerix-B
Vaccine
1. Monitor for side effects and
adverse reactions.
2. Administer vaccine within first
week of birth.
3. Combination vaccines should not
be used at birth.
0.5ml
(5mcg)
IM Once.
Before
Dis-
charge
Protection
against
infection.
1. Redness.
2. Local soreness.
3. Tenderness.
1. Call doctor if signs of
Anaphylaxis reactions occur.
2.Ensure that infant gets all
three doses at the right time.
3. Infants can get vaccines
even with mild cold.
Directions:
The medication sheet(s) must be completed for each patient assigned. It is to include all scheduled and PRN medications ordered. The sheet(s) must be completed prior to
administering medications on the clinical sit
17
Medical Surgical Nursing Adult II Name:__Alex Kortscheff_______
Graded Clinical Assessment Rubric Date:__9-10-13____________
Score: _______ / 100 Points / Grade is 5% of your course grade.
Criteria Excellent Good
Needs
Improvement
Unacceptable
Points
Earned
Sections I Correct information about Assessment content Assessment of client Assessment of client
18
Patient Assessment
Patient centered
Systematic from
head to toe
Symmetrically &
comparatively
Clear & concise
Applies
therapeutic
interview
techniques
Accesses multiple
resources
Inspection
Auscultation
Percussion
Palpation
the clients physical and
psychological status is
gathered through interview,
observation, record review
and comprehensive
assessment.
(40 points)
provides supporting
information that is usually
correct. Methods for
gathering assessment data
included some methods of
interview, observation,
record review and
comprehensive assessment.
A database is established to
make clinical judgments and
plan appropriate
interventions.
(35 points)
physical and psychological
status is often incomplete
or incorrect. Information
gathering techniques are
haphazard and lack
comprehensive review of
the clients status. The
database lacks key areas for
making sound clinical
judgments and for planning
appropriate interventions.
(30 points)
physical and
psychological status is
incomplete or
incorrect. Use of
information gathering
techniques is not
evident. The database
is incomplete. One is
unable to make safe
clinical judgments or
plan appropriate
interventions.
(25-0 points)
___/40
Sections II
Medication Review
Medication list
Medication
integration into
assessment areas
Desired
effects/side
effects identified
Identifies all current
scheduled and PRN
medications including
trade/generic, names,
desired effects and side
effects. Illuminates
connection between clients
assessment and illness.
(15 points)
Identifies most current
scheduled and PRN
medications completely.
Illuminates connection
between clients
assessments and illness.
(12 points)
Numerous incomplete areas
for review of current
scheduled and PRN
medications. Often is
unable to make a
connection between clients
assessment and illness.
(8 points)
Medication review is
incomplete showing
lack of time and effort.
(7-0 points)
___/15
19
Section III
Laboratory and
Diagnostic Review
Findings with
rationale
integrated in
assessment
Significant Lab/DX
procedures are identified
within assessment areas,
including: client values and
their significance for
application to client
assessment.
(15 points)
Significant Lab/DX
procedures are identified,
within assessment areas,
including: client values and
their significance for
application to client
assessment.
(12 points)
Review of Lab/DX
procedures is often very
brief and nonspecific to the
patient illness/assessment.
Some information is
inconsistent for application
to clients assessment.
(8points)
Analysis and
applications of Lab/DX
procedures is not
evident.
(7-0 points)
___/15
Section IV
Nursing Diagnosis List
Complete prioritized
nursing diagnosis
related to patient
problems
Format: problems
related to etiology
as manifested by
signs & symptoms
A comprehensive
nursing diagnosis
list with patient
problems and three
part statement is
provided.
(10 points)
Overall, the nursing
diagnosis list identifies the
patients prioritized
problems. The three part
statement defining the
problems has only minor
deficiencies.
(8 points)
The very minimum
requirements are met for
completing the nursing
diagnosis list. Some key
patient problems are
overlooked. The three part
statement lacks clarity and
completeness.
(6 points)
The nursing diagnosis
list is incomplete or
incorrect indicating lack
of time and effort.
(4-0 points)
____/10
Section V
Content Accuracy
Organization
Terminology
Grammar
Spelling
Neatness
Writing is complete and
grammatical, and flows
together easily. Correct
terminology and spelling
are provided. The
assessment paper is neat,
logical, and organized.
(10 points)
For the most part, writing is
complete and grammatical,
and flows together easily.
With a few exceptions,
correct terminology and
spelling is provided. The
assessment paper is
generally neat, logical and
well organized.
(8 points)
Reader can follow the
assessment paper structure,
but they are distracted by
some grammatical errors.
Some terminology is
incorrect, and/or spelling is
incorrect. Frequently
organization of content fails
to flow smoothly.
(6 points)
Writing is incomplete
with multiple
grammatical errors.
Terminology/spelling is
often incorrect.. Reader
can follow assessment
only with effort. Some
content is not clear.
Organization seems
haphazard.
(4-0 points)
___/10
20
Section VI
References
Literature sources
sited
APA Format
Three professional
references
Compelling evidence is
given to support content
and is clear and well
represented. Three
references are provided.
APA format is used
accurately and consistently.
(5 points)
References to support
content are generally
present. Three references
are provided.
APA format is used with
minor violations.
(4 points)
Although occasional
references support content,
the minimum of 3
references is not evident.
Format of reference list
reflects incomplete
knowledge of APA format
(3 points)
References are not
cited to support
content.
Format of reference list
is not recognizable as
APA format.
(2-0 points)
___/5
Section VII
Paper Submitted on
designated day
2 point deduction
per each day late
Date Due: ______
Submitted: _____
The paper is submitted on
the assigned day.
(5 points)
The paper is submitted one
day past assigned day.
(3 points)
The paper is submitted two
days past assigned day.
(1points)
The paper is submitted
three days past
assigned day.
(0 to -1 points, etc. per
additional days late)
____/5
Total:
___/100
Date: _________ Instructor ________________________________________________ Grade ______
Comments:
21
Das könnte Ihnen auch gefallen
- Head To Toe AssessmentDokument3 SeitenHead To Toe AssessmentCatherine Drew Sims100% (6)
- Pead 3 - Abdominal Pain and VommitingDokument22 SeitenPead 3 - Abdominal Pain and Vommitingbbyes100% (1)
- Acute Abdominal PainDokument11 SeitenAcute Abdominal Painone_2_nv100% (1)
- Assessing Neurologic FunctionsDokument10 SeitenAssessing Neurologic FunctionsDenise DizonNoch keine Bewertungen
- Fluids Electrolytes and Acid Base ImbalancesDokument8 SeitenFluids Electrolytes and Acid Base ImbalancesSamantha Bernardo UndaNoch keine Bewertungen
- GI Signs and SymptomsDokument40 SeitenGI Signs and SymptomsJohnny BeeNoch keine Bewertungen
- Nursing Assessment Form: A. Demographic DataDokument5 SeitenNursing Assessment Form: A. Demographic Datacat_w0m4nNoch keine Bewertungen
- Ms Reviewer Renal UrinaryDokument5 SeitenMs Reviewer Renal UrinaryAlyssa Nicole CajayonNoch keine Bewertungen
- Nursing Care Health Assessment Form: Instructions For CompletionDokument6 SeitenNursing Care Health Assessment Form: Instructions For CompletionJM RomiasNoch keine Bewertungen
- Pain LectureDokument13 SeitenPain LectureDale BuckmanNoch keine Bewertungen
- Physical AssessmentDokument29 SeitenPhysical AssessmentTheSweetpea501100% (1)
- Assessment and Management of Patients With Endocrine DisordersDokument46 SeitenAssessment and Management of Patients With Endocrine Disordersamal100% (1)
- Health, Stress, and CopingDokument43 SeitenHealth, Stress, and CopingKar Gayee100% (1)
- Pharmacy CalculationsDokument39 SeitenPharmacy CalculationsEbookGlobal100% (5)
- RAC US Exam QuestionsDokument5 SeitenRAC US Exam QuestionsNikki Bella0% (1)
- Oncologic EmergenciesDokument3 SeitenOncologic EmergenciesMiguel Cuevas DolotNoch keine Bewertungen
- General Appearance: Ital SignDokument4 SeitenGeneral Appearance: Ital SignLiza Estrabo100% (1)
- Weekly Clinical Prep Packet 12 REVISEDDokument12 SeitenWeekly Clinical Prep Packet 12 REVISEDMei SarteNoch keine Bewertungen
- Health Assessment Proforma of School StudentsDokument4 SeitenHealth Assessment Proforma of School StudentsMantu Roy100% (1)
- The Origin and Nature of Sorcery-Pharmakeia-Pharmaceutical ExplainedDokument40 SeitenThe Origin and Nature of Sorcery-Pharmakeia-Pharmaceutical ExplainedArnulfo Yu LanibaNoch keine Bewertungen
- Anxiety Disorder FarazDokument36 SeitenAnxiety Disorder FarazFaraz HodaNoch keine Bewertungen
- Niversity of The Philippines Manila: Nursing Health History Date of Interview: (Input) A. Biographic DataDokument4 SeitenNiversity of The Philippines Manila: Nursing Health History Date of Interview: (Input) A. Biographic DataConstance Isabelle MercadoNoch keine Bewertungen
- Heath Assessment ToolDokument8 SeitenHeath Assessment ToolHouda Hayek100% (1)
- Stroke - Final ReportDokument16 SeitenStroke - Final ReportgolokipokNoch keine Bewertungen
- A2 Chemistry Revision NotesDokument13 SeitenA2 Chemistry Revision NotesJobe Bryer50% (4)
- GIT Examination - Clinical Skills With DRDokument8 SeitenGIT Examination - Clinical Skills With DRNaveen KovalNoch keine Bewertungen
- Eating DisordersDokument9 SeitenEating DisordersFatin Nurina Mohd NazemiNoch keine Bewertungen
- DELIRIUM PresentationDokument26 SeitenDELIRIUM PresentationAnkush Sharma100% (1)
- History and Physical ExaminationDokument17 SeitenHistory and Physical ExaminationNur Fatima SanaaniNoch keine Bewertungen
- Aspirn 4Dokument2 SeitenAspirn 4salwaNoch keine Bewertungen
- Pharmaceutical Inorganic Chemistry QB Sem 1 B PharmDokument8 SeitenPharmaceutical Inorganic Chemistry QB Sem 1 B PharmAshish SinghNoch keine Bewertungen
- History Taking Cheat SheetDokument1 SeiteHistory Taking Cheat SheetLaura ForsythNoch keine Bewertungen
- Health History Documentation Form ChristinaDokument6 SeitenHealth History Documentation Form Christinaapi-545542584Noch keine Bewertungen
- Autoimmune DisordersDokument13 SeitenAutoimmune Disordersinah krizia lagueNoch keine Bewertungen
- Nursing Process Diagnosis Plan Implementation EvaluationDokument59 SeitenNursing Process Diagnosis Plan Implementation EvaluationYemaya84Noch keine Bewertungen
- Complete Physical Examination ChecklistDokument5 SeitenComplete Physical Examination Checklistapi-641836481Noch keine Bewertungen
- Drug Study - SalbutamolDokument2 SeitenDrug Study - SalbutamolryanNoch keine Bewertungen
- Malaria MEQDokument6 SeitenMalaria MEQMuvenn KannanNoch keine Bewertungen
- The Roadmap Report Teacher's Notes: Unit 1: Social Screen Time Corresponds With Lessons 1A& 1BDokument20 SeitenThe Roadmap Report Teacher's Notes: Unit 1: Social Screen Time Corresponds With Lessons 1A& 1BrunnermnNoch keine Bewertungen
- IV Flow Rate QuizDokument6 SeitenIV Flow Rate QuizKannanNoch keine Bewertungen
- Pharma CompaniesDokument7 SeitenPharma Companiesshaishav_86100% (2)
- PE Form - NeonateDokument3 SeitenPE Form - NeonateStef ReyesNoch keine Bewertungen
- Physical Assessment ChecklistDokument3 SeitenPhysical Assessment ChecklistMaria PunoNoch keine Bewertungen
- GangreneDokument6 SeitenGangreneMohammad Yordan GandaraNoch keine Bewertungen
- Anxiety and Stress-Related DisordersDokument26 SeitenAnxiety and Stress-Related Disordersunpredictable_stoneNoch keine Bewertungen
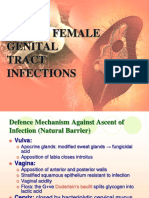
- 12 Lower Female Genital Tract InfectionsDokument42 Seiten12 Lower Female Genital Tract InfectionsAwal Sher khanNoch keine Bewertungen
- Gangrene Is The Death of TissueDokument2 SeitenGangrene Is The Death of TissuerahulbafnaeNoch keine Bewertungen
- PancreatitisDokument12 SeitenPancreatitismardsz100% (5)
- Communicable Disease ChartDokument1 SeiteCommunicable Disease ChartArlan AbraganNoch keine Bewertungen
- MS InstrumentsDokument3 SeitenMS InstrumentsFreeNursingNotesNoch keine Bewertungen
- Batt Exam PharmaDokument56 SeitenBatt Exam PharmaJoana Grace CortezNoch keine Bewertungen
- Management of OADokument15 SeitenManagement of OARudy HsNoch keine Bewertungen
- Most Question That The "Psychiatrist" Would Ask?Dokument1 SeiteMost Question That The "Psychiatrist" Would Ask?Chayantorn NimmanwathanaNoch keine Bewertungen
- HemiplegiaDokument17 SeitenHemiplegiaStefany CelineNoch keine Bewertungen
- LALA Megatable DermaDokument39 SeitenLALA Megatable DermaJorelle MarquezNoch keine Bewertungen
- Delirium, Dementia, PsychosisDokument2 SeitenDelirium, Dementia, PsychosisLagente EstalocaNoch keine Bewertungen
- OB Gyne Assessment ToolDokument5 SeitenOB Gyne Assessment ToolKyla CsyNoch keine Bewertungen
- Head InjuryDokument9 SeitenHead InjuryRaveen mayiNoch keine Bewertungen
- Need Motivates The Behaviour of A Person.: Human Needs TheoryDokument8 SeitenNeed Motivates The Behaviour of A Person.: Human Needs TheoryDan Ataniel EnsaladaNoch keine Bewertungen
- SAMDokument108 SeitenSAMAlimyon Abilar MontoloNoch keine Bewertungen
- Iabetic Europathy: DR Saumya H Mittal Neurologist Sharda Hospital & Health CityDokument39 SeitenIabetic Europathy: DR Saumya H Mittal Neurologist Sharda Hospital & Health CityGhea SugihartiNoch keine Bewertungen
- Neurosis: Department of Psychology The First Affiliated Hospital of ZZU Huirong GuoDokument132 SeitenNeurosis: Department of Psychology The First Affiliated Hospital of ZZU Huirong GuoIván BernalNoch keine Bewertungen
- Oral Revalida - NCM 417 2014 MidtermDokument10 SeitenOral Revalida - NCM 417 2014 MidtermMae DacerNoch keine Bewertungen
- DR Ashiq Tutorials Pre-Krok 1222Dokument66 SeitenDR Ashiq Tutorials Pre-Krok 1222Praveen KpNoch keine Bewertungen
- (MED1) 3.04 Approach To Hypertension (Dr. Bago-Azares)Dokument11 Seiten(MED1) 3.04 Approach To Hypertension (Dr. Bago-Azares)NoreenNoch keine Bewertungen
- Hyporeninemic HypoaldosteronismDokument12 SeitenHyporeninemic HypoaldosteronismCésar Augusto Sánchez SolisNoch keine Bewertungen
- Cagayan de Oro City College of Nursing Assessment Form General InformationDokument11 SeitenCagayan de Oro City College of Nursing Assessment Form General Informationdjanggo18Noch keine Bewertungen
- Notes Pages 2Dokument1 SeiteNotes Pages 2runnermnNoch keine Bewertungen
- Unit Test 7BDokument2 SeitenUnit Test 7BrunnermnNoch keine Bewertungen
- Homework:: They Align With The Requirements For Your Target Role, You're Ready To Move Your Job Search ForwardDokument1 SeiteHomework:: They Align With The Requirements For Your Target Role, You're Ready To Move Your Job Search ForwardrunnermnNoch keine Bewertungen
- Ability Can Could Pages 1Dokument1 SeiteAbility Can Could Pages 1runnermnNoch keine Bewertungen
- How To Uncover Job Opportunities: Understand Your Target RoleDokument1 SeiteHow To Uncover Job Opportunities: Understand Your Target RolerunnermnNoch keine Bewertungen
- Unit Test 1ADokument2 SeitenUnit Test 1Arunnermn100% (1)
- The Roadmap Report: Unit 2: The Return of The Milkman Corresponds With Lesson 2ADokument2 SeitenThe Roadmap Report: Unit 2: The Return of The Milkman Corresponds With Lesson 2ArunnermnNoch keine Bewertungen
- Unit Test 4BDokument2 SeitenUnit Test 4BrunnermnNoch keine Bewertungen
- RM C1 Video Worksheets ContentsDokument1 SeiteRM C1 Video Worksheets ContentsrunnermnNoch keine Bewertungen
- Phrasal Verbs - EnglishDokument4 SeitenPhrasal Verbs - EnglishrunnermnNoch keine Bewertungen
- Employment Law: Religious Discrimination and Racial Harassment: What Ever Happened To Marshawn Demur?Dokument12 SeitenEmployment Law: Religious Discrimination and Racial Harassment: What Ever Happened To Marshawn Demur?runnermnNoch keine Bewertungen
- Oxford Practice Grammar Advanced Tests Pages 5 6Dokument2 SeitenOxford Practice Grammar Advanced Tests Pages 5 6runnermnNoch keine Bewertungen
- Task 1. Continuous AspectDokument1 SeiteTask 1. Continuous AspectrunnermnNoch keine Bewertungen
- Acculturation TasksDokument2 SeitenAcculturation TasksrunnermnNoch keine Bewertungen
- Applying Agile Learning To Teaching English For Specific PurposesDokument22 SeitenApplying Agile Learning To Teaching English For Specific PurposesrunnermnNoch keine Bewertungen
- Medication Generic/Brand Classification Nursing Implications (3) Dosage Route Schedule /time Desired Effect Side Effects (3) TeachingDokument5 SeitenMedication Generic/Brand Classification Nursing Implications (3) Dosage Route Schedule /time Desired Effect Side Effects (3) TeachingrunnermnNoch keine Bewertungen
- Key Ideas: Factors That Affect Language Learning - MotivationDokument2 SeitenKey Ideas: Factors That Affect Language Learning - MotivationrunnermnNoch keine Bewertungen
- 5 Practical PYP TipsDokument1 Seite5 Practical PYP TipsrunnermnNoch keine Bewertungen
- Can and Can't: Things You Can Do and Eight Things You Can't Do. Examples: Ride A BicycleDokument1 SeiteCan and Can't: Things You Can Do and Eight Things You Can't Do. Examples: Ride A BicyclerunnermnNoch keine Bewertungen
- Singular Plural Escriba La Forma Correcta Del Verbo "To Be": Luis LedesmaDokument1 SeiteSingular Plural Escriba La Forma Correcta Del Verbo "To Be": Luis LedesmarunnermnNoch keine Bewertungen
- VerbtobeDokument1 SeiteVerbtoberunnermnNoch keine Bewertungen
- A Nurse Educator Is Reviewing With A Group of Nursing Students The Actions and Thought ProcessesDokument4 SeitenA Nurse Educator Is Reviewing With A Group of Nursing Students The Actions and Thought ProcessesrunnermnNoch keine Bewertungen
- School Nurse Schedule Spring 2015: Renee Mathews 641-751-1156 Susan Gallo 641-236-2750 Gloria Dielschneider 641-366-2810Dokument1 SeiteSchool Nurse Schedule Spring 2015: Renee Mathews 641-751-1156 Susan Gallo 641-236-2750 Gloria Dielschneider 641-366-2810runnermnNoch keine Bewertungen
- Hba1c 2018 Dr. Suryani DaulayDokument34 SeitenHba1c 2018 Dr. Suryani DaulayAnonymous K0ykZ9siQNoch keine Bewertungen
- Sepha White Paper Non Destructive VisionScanDokument12 SeitenSepha White Paper Non Destructive VisionScananshulNoch keine Bewertungen
- Regulatory Requirements For Clinical Trials in IndiDokument8 SeitenRegulatory Requirements For Clinical Trials in IndiMahendran NNoch keine Bewertungen
- Kardex 4Dokument3 SeitenKardex 4Juviely PremacioNoch keine Bewertungen
- Chemical EngineeringDokument83 SeitenChemical EngineeringQuynh Mai DoNoch keine Bewertungen
- Fibrosis QuisticaDokument6 SeitenFibrosis QuisticaFernanda Del ValleNoch keine Bewertungen
- Cetrimide Agar Base (European Pharmacopoeia) : CAT Nº: 1102Dokument2 SeitenCetrimide Agar Base (European Pharmacopoeia) : CAT Nº: 1102Tatjana MarkovicNoch keine Bewertungen
- Repositioning Dabur: Case Details: PriceDokument7 SeitenRepositioning Dabur: Case Details: Pricechakri5555Noch keine Bewertungen
- OHA Response To Governor Vaping 2019Dokument2 SeitenOHA Response To Governor Vaping 2019Mark FurmanNoch keine Bewertungen
- Term Paper On Investment Management: Presented byDokument42 SeitenTerm Paper On Investment Management: Presented byChinmoy Prasun GhoshNoch keine Bewertungen
- Dokumen - Tips - List of Pharma Companies in GujaratDokument22 SeitenDokumen - Tips - List of Pharma Companies in Gujaratbhavyapanchalv4Noch keine Bewertungen
- A Study of Over The Counter Medication Use, Among Patients Presenting To Family Physicians, at A Teaching Hospital in KarachiDokument12 SeitenA Study of Over The Counter Medication Use, Among Patients Presenting To Family Physicians, at A Teaching Hospital in KarachiSamruddhi ZambareNoch keine Bewertungen
- Abilify Maintena Epar Public Assessment Report enDokument70 SeitenAbilify Maintena Epar Public Assessment Report enWara RizkyNoch keine Bewertungen
- Australia Medical Carriage RequirementsDokument28 SeitenAustralia Medical Carriage Requirementsdoğancan uzunNoch keine Bewertungen
- PCE Pharmacode Guide V04-05 enDokument19 SeitenPCE Pharmacode Guide V04-05 enMaximo FerreiraNoch keine Bewertungen
- BaruDokument7 SeitenBaruKoasNoch keine Bewertungen
- Article 017Dokument10 SeitenArticle 017Digambar GondvaleNoch keine Bewertungen
- Elastomer Brochure 2010Dokument52 SeitenElastomer Brochure 2010mlombardiTONoch keine Bewertungen
- Bioterp Partners PETX Long ThesisDokument31 SeitenBioterp Partners PETX Long ThesisZack100% (1)
- Physician Care ManagerDokument3 SeitenPhysician Care Managerkman0722Noch keine Bewertungen
- UNIT3 Communication in Drug Safety Crisis ManagementDokument4 SeitenUNIT3 Communication in Drug Safety Crisis Managementworkvasudha18Noch keine Bewertungen
- Case Study 3Dokument2 SeitenCase Study 3金霄Noch keine Bewertungen