Beruflich Dokumente
Kultur Dokumente
Tinea Capitis
Hochgeladen von
adityakafiberkahsmgCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Tinea Capitis
Hochgeladen von
adityakafiberkahsmgCopyright:
Verfügbare Formate
TINEA CAPITIS : A REVIEW
Abstract
Tinea capitis causes hair loss, scaling, erythema, and impetigo-like lesions. It is the
most common dermatophyte infection found in children under the age of 12, especially in
African Americans. A good knowledge and understanding of the dosages, duration, and
potential side effects of different antifungals is important for managing tinea capitis.
Introduction
The dermatophytes (tinea) are a group of fungi that invade keratinized tissue.
Depending on the type of species, the epidermis and its structures (such as nails and hair) are
infected. Dermatophyte skin infections are the most frequent clinically seen fungal infections
in the world (Abdel-Rahman et al., 2005).
Historical Perspective
The term "tinea" is an analogy to parasitic larvae, and over the years has become the
term applied to parasitic skin infections. A synonym for tinea is "ringworm," which describes
the ring-like lesions caused by that fungal infection. The term "capitis" refers to the scalp,
and hence the term "tinea capitis," identifying a ringworm infection of the scalp. The
epidemiology of finea capitis has changed with the advent of griseofulvin, and the sensitivity
of M. audouinii to this anfifungal medication. However, unlike M. audouinii, T. tonsurans
cannot be detected with the fluorescent Wood's lamp, leaving many cases undetected
(Elewski, 2000). Two separate studies showed that since the mid-1970s, both New York City
and Chicago have had an increase in T. tonsurans infections from 1% to 3%, to 90% to 96%
(Aly, 1999). By comparison, in western and eastern Europe, M. audouinii and T. schoenleinii
were the most common causes of infection, respectively. Since that time, these rates have
decreased due to the use of griseofulvin and environmental changes, such as increased
sanitation and better personal hygiene. Currently, T. violaceum is the dominant species in
eastern Europe (Aly, 1999).
Causing hair loss, scaling, erythema, and impetigo-like lesions, tinea capitis, the focus
of this article, is the most common dermatophyte infection found in children under the age of
12, especially in African Americans. Tinea capitis also occurs in adults, although this is less
common (Abdel-Rahman et al., 2005; Silverberg, Weinberg, & DeLeo, 2002). The incidence
of tinea capitis differs between gender and microorganisms. For example, Microsporum canis
infection occurs more frequently in boys, while with the Trichophyton species, boys and girls
are equally infected. Women are infected more frequently than men, perhaps due to their
care-taking role (My, 1999). Although many species can cause tinea capitis, the most
commonly occurring species are Microsporum canis, Epidermophyton floccosum,
Trichophyton mentagrophytes, Trichophyton tonsurans (mostly in the United States), and
Trichophyton rubrum (Trivino-Duran et al., 2005). In this article, a review of the historical
and clinical scope of tinea capitis, as well as new advents in the management of this common
dermatophyte infection, are presented.
Types of tinea capitis infections
Tinea capitis infections are classified into three major groups: anthropophilic,
zoophilic and geophilic. The anthropophilic infections are parasitic on humans, usually
forming larger hyphae and spores inside the hair shaft, while the zoophilic tend to be
parasitic on animals, usually forming smaller hyphae and spores outside the hair shaft. The
geophilic infections are identified by location. In immunocompetene humans, anthropophilic
spescies cause mild lesions with minimal inflammation, but geophilic and zoophilic species
may result in extensive lesions secondary to inflammation, leading to abscesses and pustules
(Krajewska-Kulak et al.,2003)
Tinea capitis types are futher divided by how dermatophytes invade the hair shaft (for
example, endothrix versus ectothrix). In endothrix, the hair shaft is filled with hyphae and
spores. Some causes of endothrix infection are T.tonsuras and T. Schoenleinii species. The
associated endothrix species also cause a black dot tinea capitis. In the ectothrix types, the
hyphae and spores cover the outside of the hair, which results in the destruction of the
cuticle. All of the microsporum spescies and T. Verrucosum are involved. Microsporum
infections (M.canis) cause a gray patch tinea capitis . ectothrix infections, un like
endothrix types, can ve identified by wood`s light. A very rare and severe form of tinea
capitis infection is favus, primarily caused by T.schoenieinii. favus results in a honeycomb-
type destruction of the hair follicle, giving the hair a yellowish collor (Kab,2006)
Clinical forms
Tinea capitis typically presents in two major forms: gray patch and black dot
Gray patch tinea capitis (GPTC). GPTC is generally found in the endemic form within the
United States, and the offending agent is typically M.canis. it is usually spread forms cats or
dogs to humans; however, person to person transmission is also possible. Initial sym ptoms
are an erythematous are on the scalp with patchy alopecia and dry scaling. The affected
area then spreads in centrifungal manner for up to a mouth, although it may persist on the
scalp for many years. These patches may coalesce, with larger patches often visible on the
scalp. Severe scaling of the scalp may result, and due to cuticle b reakage, the hair may
become brittle , with considerable b roken hair visible on the patient (Habif,2004).
Lesions may become secondarily infected with fungus or bacteria (such as
staphylococcus aureus), and will appear boggy and raised, with pus exuding. This clinical
presentation of tinea capitis is referred to as kerion, an is an immune granulomatous response
to the offending agents. There may be single or multiple plaques, and this type of
inflammation may be associated with painful episodes. Scarring will result if the kerion is not
treated appropriately. Typical treatment for this condition is the use of oral antifungais for 6
to 8 weeks; corticosteroids may be prescribed for cases of tenderness and scalp pain.
Concurrently, posteriorcervical lymphadenopathy may present as an associated symptom
(Fuller, child, midgley, & Higgins, 2003)
The use of KOH examination or Woods lamp are the main method for identifying
GPTC in patients. M. audouinii and M. canis infections appear as green blue fluorescence
under Woods light. The confirmatory diagnosis, is needed, may be obtained by culturing the
hair on sabourauds medium.
Black dot tinea capitis (BDTC). BDTC is the most common form of tinea found in
North America, and the causative agent is T. tonsurans. This form primarily affects African-
American children, typically spreading via child to child contact.beginning with an
erythematous scalling patch and scalp, BDTC progresses to single or multiple lesions. Hair is
broken off at the surface and detritus within the follicle opening gives the appearanceof a
black dot (habif, 2004). In the mostintense cases, which are accompanied by inflammation,
there may be a resemblance to pyoderma or discoid lupus erythematosus. It may also be
accompanied by lymphadenopathy (Fuller et al., 2001). If secondary infection occurs (as in
GPCT), there may be sudden shift into the kerion form. Typical treatment is oral antifungals
for 6 to 8 weeks, with the additional use of corticosteroids for tender and painful scalp. If not
of hted, the scarring may cause permanent alopecia.
BDTC is also visualized by KOH examination of hair shaft spores, and its
confirmation by culture on saborauds medium. How ever, unlike GPTC, fluorescence under
Woods light does not occur.
Favus primarily caused by schoenleinii, favus is achronic inflammatory reaction with
an infection of the outer and inner hair shafts. Initially there is erythema,followed by scutula
(yellow crust) formation. Eventually there is considerable hair loss and scarring. If left
untreated, favus will lead to permanent alopecia (matte, lopes, Melo & Beber, 1997)
Mycology
There are three genera of dermatophytes. Epidermophyton, Microsporum and
Tricophyton. There are a[pproximatelly 40 species that are either anthropophilic, zoophilic,
geophilic. Some common examples of each are anthropophilic (T. rubrum, T. tonsurans, T.
Violaceum); zoophilic (M. canis, T. Verrucosum); and geophilic (M. fulvum).
Differential Diagnosis
Tinea capitis infections are often mistaken for other more dermatologic scalp disease,
especially in older adults. Tinea capitis agents, such as M. audouinii and M. canis, can mimio
impetigo and pediculosis, or psoriasis and seborrhea, respectively. Since both causative
agents can be visualized under Woods lamp, this method should be used when the clinician
is considering the above differential diagnosis. For impetigo, the pain is generally more
severe and individual hairs do not appear to be broken. In psoriasis, the scales on the scalp
are thicker, but the hair is not brokeh off (Johnson & Nunley, 2000). Allopecia areata also
causus hair loss and may mimic T. tonsurans infections, but doesnot cause scaling of the
scalp.
Management
Before 1958, when griseofulvin was as approved by the U.S. Food and Drug
Administration (FDA) for systemic treatmen of tinea capitis, the only available treatment
were shaving the head applying mercury/sulfur to the scalp, or resorting to high fat diets
(Mahrenschlager, seidl, Ring, & Abeck, 2005). However, griseofulvin quickly became the
mainstay of treatment, and the use of terbinafine and itaconazole in patients allergic to
griseofulvin were also successful (Gupta et al, 1999: Trivino-Duran et al., 2005). In a meta
analysis study, Fleece, Gaughan, and aronoff(2004) showed terbinafine treatment for up to 4
weeks to be as effective in treating Trichophyton spp. As 8 weeks of griseofulvin treatment.
However , it is important for the patients (and parents, if the patient is a minor) to be aware
that only griseofulvin is currently approved by the FDA for treating tinea capitis, although
many physicians choose to use other systemic treatments such as terbinafine, fluconazole,
and itraconazole. Based on many successful studies (Chan & Friedlander, 2004)
One important consideration in choosing a management plan is the type of infection.
For example griseofulvin is only effective when treating Microsporum, Epidermophyton, and
Trichophyton (Chan & Friedlander, 2004). When compresed to other treatments in
Trichophyton infections, griseofulvin and terbinarfine are equally effective, but griseofulvin
is advantageous when used against Microsporum ifections(Fuller et al,2001). Moreover,
when treating Microsporum canis, the dosage and treatment lenght of systamic treatments
may need to be increased (Mahrenschlager et al., 2005), with baseline and periodic LFTs>1
month therapy and BUN/SCr for all systemic antifungal treatments, and CBC for terbinafine.
One important consideration in choosing a management plan is the type of infection.
For example, gliseofulvin is only effective when treating Microsporum, Epidermophyton, and
tricophyton( chan& Friedlander, 2004). When compared to other treatments in trycophyton
infection, griseofulvin and terbinafine are equally effective, but griseofulvin is advantageous
when used against Microsporum infection ( Fuller et al, 2001). Moreover, when treating
microsprorumcanis, the disage and treatment length of systemic treatments may need to be
increased (Mhrenschlager, 2005), with baseline and periodic LF Ts>1 month therapy and
BUN/SCr for all systemic antifungal treatments, and CBC for terbinafine.
Nursing measures
A good knowledge and understanding of the dosages, duration, and potential side
effects of different antifungals is important for the management of tneacapitis.
Griseovfulvin( Fulvion) is prescribed at 15 to 25 mg/kg/day for a period of 8
weeks or more depending on the extent of infection and the speed of recovery. This recovery
is monitored by followup examinations and the assistance of woods lamp for detecting M.
audouinii and M.canis. Griseofulvin can be taken with dairy products to increase absorption
and mask the taste of this medication for children. Patients should be cautioned about side
effects such as headache, nausea, transient rash, diarrhea, and photosensitivity. Griseovulfin
should not be used in patients with porphyria or liver disorder. It may also precipitate
systemic lupus erythematosus in some patients.
Terbinafine ( Lamisil ) is prescribed based on the weight of the patient as follows
for the treatment of tine capitis : 40 kg or more, 250 mg/day 20kg to 40kg, 125 mg/day; and
10 kg to 20 kg, 62,5 mg/day for a period up to 4 weeks, depending on the effectiveness of the
treatment. A lower dose of 3 to 6 mg/kg/day for up to 4 weeks has been sufficient in patients
with T. tonsurans infections. Patients should be warned about alopecia, erythema multiforme,
steven-johnsonyndrome, and a partial or complete loss of taste; the loss of taste is usually
reversible upon discontinuation of terbinafine. Immediate discontinuation is also warranted
with signs of neutropenia, agranulocytosis, and hepatis dysfunction.
Itraconazole (sporanox ) is given to children over 40 kg at a dose of 200 mg, 30 kg
to 40 kg at 150 mg, 20 kg to 30 kg at 100 mg, and less than 20 kg, 50 mg per day for 4 to 6
weeks to treat tineacapitis. For T.tonsurans, itraconazole can be given at 3 to 5 mg/kg/day
with meals for the same duration of time. Patients with valvular heart disease, ischemic heart
disease, pulmonary disease and renal failure should be excluded from this prescription due to
possible congestive heart failure. Patients should also be cautioned about steven-johnson
syndrome, gastrointestinal discomfort, and headaches
Fluconazole (Diflucan ) is prescribed at 5 mg/kg/day for a period up to 6 weeks
for treatment of tineacapitis. Side effects are milder than other treatment plans, and range
from gastrointestinal discomfort to abnormal liver function tests, nausea, and headache.
For specific treatment of M.canis, a longer duration of therapy is indicated for all antifungals.
Oral ketokonazole is also succesfull in treatment; however, due to its high cost and
possible hepatotoxicity, it has not been used as a first-line drug.
Treatment of carriers
Shampoos, such as a 2% ketoconazole, 1% to 2,5% selenium sulfide, 1% to 2% zinc
pyrithione, and povidone-iodine, are also used as adjuncts, along with an oral antifungal.
These shampoos may decrease scaling and itching substantially, but do not penetrate deeply
emough to be the sole treatment in patients. The shampoos are applied to the scalp at least
three times each week for 5 to 10 minutes. This also allows children to return to school when
both treatments are used together (Fleece et al, 2004).
Outcome and prognosis
The outcome and prognoses of tineacapitis is difficult to assess due to its variability
and dependence on many factors. Short-term factors, such as adherence to a drug regimen,
clean environment, screening and treatment of asymptomatic household residents are all
important factors initially. This will further depend on the rate of sensitivity of organisms to
medications, rate of re-infection, and the introduction of new organisms into the environment.
If result are not achieved and outcomes are not improved, then the medication may be
changed or the duration may be increased. Another important fact to consider is that since the
production of spores will continue, close monitoring of children and their surrounding
environment is important (Higgins, Fuller, & Smith, 2000)
Patient Education
As tineacaptis may continue as a source of infection, even asymptomatic patients,
along with adults and other siblings in the household, should be directed to use antifungals
and shampoos, such as those containing 2,5% selenium sulfide and povidone-iodine, to
prevent the spread of the carrier state. further more, young children (up to the third grade) and
the playmates of patients should also be evaluated for tineacapitis infection, since
transmission through the sharing of play toys is a common route of infection in this age
group. Those with infection or asymptomatic carriers should avoid close physical contact and
sharing of any objects until full treatment has been met with success. Prevention from
attending school is not necessary, and neither is wearing a hat or shaving the head of the child
during the course of the treatment. Complication that occur, such as severe hair loss and
scarring alopecia, may be detrimentalto the patient. Although the patient may be advised that
some of the hair loss in temporary, early proper treatment and education are absolutes.
MORE ON THIS TOPIC
Skin, benign skin lesions ( plastic surgery)
Tineacapitis ( Dermatology)
Wound healing, chronic Wounds (plastic surgery)
Nurse Practitioner Resource Center
Dermatology Nursing.2007 : 19(6);525-529.2007 Janneti Publication, inc.
The print version of this article was originally certified for CE (continuing education) credit.
For accreditation detail, please contact the publisher.
Anthony J. Janneti, inc. East Holly Avenue Box 56, Pitman, New Jersey 08071-0056
Das könnte Ihnen auch gefallen
- Tinea Capitis EmedicineDokument16 SeitenTinea Capitis EmedicineIkram IkramNoch keine Bewertungen
- BAHAN Tinea CapitisDokument28 SeitenBAHAN Tinea CapitisYorika HafelaniNoch keine Bewertungen
- Tinea CapitisDokument7 SeitenTinea Capitismufidah nurfajNoch keine Bewertungen
- Tinea Capitis: Audouinii), Which Give A Typical Green Fluorescence. T. Rubrum, The Commonest Cause of TineaDokument10 SeitenTinea Capitis: Audouinii), Which Give A Typical Green Fluorescence. T. Rubrum, The Commonest Cause of TineaSyamsul ArifinNoch keine Bewertungen
- Tinea CapitisDokument7 SeitenTinea CapitisNadya LiemNoch keine Bewertungen
- Tinea Corporis Pedia-1Dokument11 SeitenTinea Corporis Pedia-1Denso Antonius LimNoch keine Bewertungen
- The Diagnosis and Management Of: Tinea CapitisDokument4 SeitenThe Diagnosis and Management Of: Tinea CapitisQuraisy jamal sahilNoch keine Bewertungen
- Tinea Capitis Q & ADokument2 SeitenTinea Capitis Q & Aandre yuindartantoNoch keine Bewertungen
- The Diagnosis and Management of Tinea CapitisDokument4 SeitenThe Diagnosis and Management of Tinea CapitisKeyla Kehara PutriNoch keine Bewertungen
- The Kerion An Angry Tinea Capitis PBDokument7 SeitenThe Kerion An Angry Tinea Capitis PBprajnamitaNoch keine Bewertungen
- Tinea Capitis in AdultsDokument7 SeitenTinea Capitis in Adultsdimasarya671Noch keine Bewertungen
- Tinea Capitis: Current Review of The Literature: EpidemiologyDokument7 SeitenTinea Capitis: Current Review of The Literature: EpidemiologyameliaNoch keine Bewertungen
- DERMATOMYCOSISDokument114 SeitenDERMATOMYCOSISQonita Qurrota AyunNoch keine Bewertungen
- Diagnosis and Management of Common Tinea InfectionsDokument23 SeitenDiagnosis and Management of Common Tinea InfectionsGiovanni AnggastaNoch keine Bewertungen
- Medical MycologyDokument14 SeitenMedical Mycologyhawkar omerNoch keine Bewertungen
- DermatophyteDokument8 SeitenDermatophyteBhuvana RajNoch keine Bewertungen
- E Tra: Diagnosis and Management of Cutaneous Tinea InfectionsDokument8 SeitenE Tra: Diagnosis and Management of Cutaneous Tinea InfectionsFuad hadyanNoch keine Bewertungen
- Tinea - The DermatophytesDokument67 SeitenTinea - The Dermatophytesmansoor aliNoch keine Bewertungen
- 2003, Vol.21, Issues 3, Antifungal TherapyDokument186 Seiten2003, Vol.21, Issues 3, Antifungal TherapyRizweta DestinNoch keine Bewertungen
- Tinea Capitis Favus-Like Appearance: Problem of Diagnosis: Dwi Ratna Adisty, Linda AstariDokument7 SeitenTinea Capitis Favus-Like Appearance: Problem of Diagnosis: Dwi Ratna Adisty, Linda AstarihaningpradyNoch keine Bewertungen
- Derma To Phyto SesDokument5 SeitenDerma To Phyto SesNia Sari Nastiti LubisNoch keine Bewertungen
- Ringworm (Tinea Capitis)Dokument15 SeitenRingworm (Tinea Capitis)farmasi_hmNoch keine Bewertungen
- Dermatophytosis: EtiologyDokument6 SeitenDermatophytosis: EtiologyTheresia FalentinaNoch keine Bewertungen
- Title of The LecDokument22 SeitenTitle of The LecWeird BoiNoch keine Bewertungen
- CL Head Lice - Diagnosis and TherapyDokument7 SeitenCL Head Lice - Diagnosis and TherapyMaya Asharie HarahapNoch keine Bewertungen
- Fungal Skin Infections ملزمةDokument6 SeitenFungal Skin Infections ملزمةعبدالرحمن طارق عبدالله صالحNoch keine Bewertungen
- Chapter 4Dokument103 SeitenChapter 4tenaw100% (1)
- DefinitionDokument12 SeitenDefinitionHassan kamalNoch keine Bewertungen
- Elewski 2000Dokument20 SeitenElewski 2000mgalihwbNoch keine Bewertungen
- Kata PengantarDokument21 SeitenKata PengantarKartika RosyahNoch keine Bewertungen
- Tinea CapitisDokument7 SeitenTinea Capitisمحمد عبدالواسع المسنيNoch keine Bewertungen
- Dermatomycosis Periode 2 Maret - 5 JuniDokument128 SeitenDermatomycosis Periode 2 Maret - 5 JuniDevy KurniawatiNoch keine Bewertungen
- Tinea Corporis, Tinea Cruris, Tinea Nigra, and Piedra: Dermatologic Clinics August 2003Dokument7 SeitenTinea Corporis, Tinea Cruris, Tinea Nigra, and Piedra: Dermatologic Clinics August 2003Dicky KurniawanNoch keine Bewertungen
- Tinea Barbae Is A Rare Dermatophytic Infection That Is Limited To The Bearded Areas of The FaceDokument3 SeitenTinea Barbae Is A Rare Dermatophytic Infection That Is Limited To The Bearded Areas of The FaceMardiah Nurul HasanahNoch keine Bewertungen
- Super Ficial Fungal Infections: Key PointsDokument4 SeitenSuper Ficial Fungal Infections: Key PointsBagus Putra KurniawanNoch keine Bewertungen
- Dermatophytosis: LectureDokument35 SeitenDermatophytosis: LectureGideon MukalaziNoch keine Bewertungen
- TineaDokument4 SeitenTineaFenni OktoberryNoch keine Bewertungen
- Topical Treatment of Common Superficial Tinea InfectionsDokument8 SeitenTopical Treatment of Common Superficial Tinea InfectionsColate LocoNoch keine Bewertungen
- Pediculus Humanus Capitis: An Update: Characteristics of LiceDokument11 SeitenPediculus Humanus Capitis: An Update: Characteristics of LiceRizkaKhaerunnisaNoch keine Bewertungen
- Cutaneous Mycoses MikologiDokument10 SeitenCutaneous Mycoses MikologisherinaNoch keine Bewertungen
- Fungal Infection of The SkinDokument74 SeitenFungal Infection of The Skinary_puraNoch keine Bewertungen
- M13 - Dermatology - Chapter 5Dokument11 SeitenM13 - Dermatology - Chapter 5Idham BaharudinNoch keine Bewertungen
- Fungal InfectionDokument5 SeitenFungal InfectionFiras HamidehNoch keine Bewertungen
- Pharmaceutical Microbiology and Parasitology (PHMP211)Dokument59 SeitenPharmaceutical Microbiology and Parasitology (PHMP211)Crisamor Rose Pareja ClarisaNoch keine Bewertungen
- Superficial Fungal InfectionsDokument40 SeitenSuperficial Fungal InfectionsMarimuthu PrabhakaranNoch keine Bewertungen
- Tinea Capitis: Review ArticleDokument33 SeitenTinea Capitis: Review ArticleABhinav GangwarNoch keine Bewertungen
- Clinical Review - FullDokument6 SeitenClinical Review - Fullilham thohirNoch keine Bewertungen
- A Study of Tinea Capitis in ChildrenDokument4 SeitenA Study of Tinea Capitis in ChildrenTantriSaptennoPattiradjawaneNoch keine Bewertungen
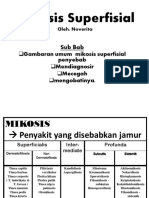
- Mikosis SuperfisialDokument46 SeitenMikosis SuperfisialAdipuraAtmadjaEgokNoch keine Bewertungen
- Dermatophyte InfectionDokument59 SeitenDermatophyte Infectionحسين طاهر حاتم طاهرNoch keine Bewertungen
- Acral Manifestations of Fungal InfectionsDokument21 SeitenAcral Manifestations of Fungal InfectionsanwarNoch keine Bewertungen
- Tinea Barbae Is A Rare Dermatophytic Infection That Is Limited To The Bearded Areas of The FaceDokument5 SeitenTinea Barbae Is A Rare Dermatophytic Infection That Is Limited To The Bearded Areas of The Facemardiah nurulNoch keine Bewertungen
- Palmoplantar PustulosisDokument6 SeitenPalmoplantar PustulosisputraimanullahNoch keine Bewertungen
- Bur, 2012Dokument16 SeitenBur, 2012Jessica VanyaNoch keine Bewertungen
- Gray Patch Tinea Capitis Caused by Microsporum Canis PDFDokument4 SeitenGray Patch Tinea Capitis Caused by Microsporum Canis PDFAnonymous hxXpvZdZNoch keine Bewertungen
- DermatophytosisDokument5 SeitenDermatophytosisRadovan Miki RadovanovicNoch keine Bewertungen
- Mycology Lecture FinalDokument258 SeitenMycology Lecture FinalBahaa Shaaban100% (1)
- Lesson 2 Superficial Cutaneous Mycosis HandoutsDokument8 SeitenLesson 2 Superficial Cutaneous Mycosis HandoutsKhay Mae DonascoNoch keine Bewertungen
- Viral Vistas: Insights into Infectious Diseases: The Invisible War: Decoding the Game of Hide and Seek with PathogensVon EverandViral Vistas: Insights into Infectious Diseases: The Invisible War: Decoding the Game of Hide and Seek with PathogensNoch keine Bewertungen
- Advocating For The Nursing RoleDokument6 SeitenAdvocating For The Nursing Rolemp1757100% (1)
- Jadwal Pelatihan Bonels Pro EmergencyDokument2 SeitenJadwal Pelatihan Bonels Pro Emergencyburhan100% (1)
- MCQs in PediatricsDokument4 SeitenMCQs in Pediatricsarun babu93% (15)
- Team Atlas BrochureDokument2 SeitenTeam Atlas Brochureapi-375843571Noch keine Bewertungen
- 15 National Comprehensive Training On Standards of Nursing PracticeDokument272 Seiten15 National Comprehensive Training On Standards of Nursing Practicednebiyu03Noch keine Bewertungen
- Family & Home NursingDokument77 SeitenFamily & Home NursingNancy SinghNoch keine Bewertungen
- WHO Operational Handbook On Tuberculosis 2020Dokument136 SeitenWHO Operational Handbook On Tuberculosis 2020Hanifah HanifahNoch keine Bewertungen
- Sultanate of Oman Ministry of Health: Requirements For Health EstablishmentsDokument15 SeitenSultanate of Oman Ministry of Health: Requirements For Health Establishmentsazamk saidNoch keine Bewertungen
- Rheumatic Fever Is AnDokument7 SeitenRheumatic Fever Is AnHamza SaeedNoch keine Bewertungen
- Medical Problem That Needs Antibiotic ProphylaxisDokument6 SeitenMedical Problem That Needs Antibiotic ProphylaxisPing KyNoch keine Bewertungen
- Study Guide Beh SciencesDokument38 SeitenStudy Guide Beh SciencesFawad KhanNoch keine Bewertungen
- Participants Midwifery Obstetrics PDFDokument177 SeitenParticipants Midwifery Obstetrics PDFNathaniel Cabatuan SalimbagatNoch keine Bewertungen
- FESS ComplicationsDokument17 SeitenFESS ComplicationsJoe NumberNoch keine Bewertungen
- Hannah Shaddock - Virtual Autopsy LabDokument7 SeitenHannah Shaddock - Virtual Autopsy LabHannah ShaddockNoch keine Bewertungen
- Phenylketonuria: Martha Blair Gwaltney Medical Genetics R Ostrowski, Phd. and L. Mcnally, M.S. July 13, 2002Dokument8 SeitenPhenylketonuria: Martha Blair Gwaltney Medical Genetics R Ostrowski, Phd. and L. Mcnally, M.S. July 13, 2002Luisa Gadis Tri WahyuniNoch keine Bewertungen
- Nutrition Month 2019Dokument37 SeitenNutrition Month 2019Czerwin JualesNoch keine Bewertungen
- Wiltshire HRT Guidance 2014Dokument5 SeitenWiltshire HRT Guidance 2014andrewmmwilmot100% (1)
- Risk Management Review ArticleDokument31 SeitenRisk Management Review Articlemohamed fathi abdel aalNoch keine Bewertungen
- Handbook of Qualitative Health Research For Evidence-Based PracticeDokument569 SeitenHandbook of Qualitative Health Research For Evidence-Based PracticeMariana LepinskyNoch keine Bewertungen
- Priority Nursing Diagnosis NutritionDokument5 SeitenPriority Nursing Diagnosis NutritionAnonymous h2EnKyDbNoch keine Bewertungen
- Team Communication: It's About Patient Safety: by Susan B. Childress, RN, MN, OCNDokument4 SeitenTeam Communication: It's About Patient Safety: by Susan B. Childress, RN, MN, OCNAnna Zhifa AbNoch keine Bewertungen
- KKM Otorhinolaryngology Patient Information LeafletDokument156 SeitenKKM Otorhinolaryngology Patient Information LeafletIzzudin Tarmizi100% (1)
- Ih - Osha 2022Dokument15 SeitenIh - Osha 2022Nursyafiq Ali Shibramulisi100% (1)
- Sts Module 8 - BacuetesDokument5 SeitenSts Module 8 - BacuetesbacuetesjustinNoch keine Bewertungen
- Unilag MSC PUBLIC HealthDokument2 SeitenUnilag MSC PUBLIC HealthImona Ohihon100% (1)
- Choose The Best AnswerDokument27 SeitenChoose The Best AnswerHusseini ElghamryNoch keine Bewertungen
- Case LabirinitisDokument5 SeitenCase LabirinitisAnaNoch keine Bewertungen
- Philippine Dental Association Covid 19 Monitoring FormDokument1 SeitePhilippine Dental Association Covid 19 Monitoring Formrhusolano rhusolanoNoch keine Bewertungen
- A Descriptive Study To Assess The Oral Health Status and Knowledge Regarding Oral Health Hazards Among Tobacco Consuming Adults of Selected Communities at Rewa, (M. P.)Dokument4 SeitenA Descriptive Study To Assess The Oral Health Status and Knowledge Regarding Oral Health Hazards Among Tobacco Consuming Adults of Selected Communities at Rewa, (M. P.)International Journal of Innovative Science and Research TechnologyNoch keine Bewertungen
- Cart Cardiac Arrest Risk TriageDokument8 SeitenCart Cardiac Arrest Risk TriageAlexeiLópezCarbonellNoch keine Bewertungen