Beruflich Dokumente
Kultur Dokumente
PD1011 DPT Residents
Hochgeladen von
5685630 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
3 Ansichten3 SeitenPD1011 Dpt Residents
Originaltitel
PD1011 Dpt Residents
Copyright
© © All Rights Reserved
Verfügbare Formate
PDF, TXT oder online auf Scribd lesen
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenPD1011 Dpt Residents
Copyright:
© All Rights Reserved
Verfügbare Formate
Als PDF, TXT herunterladen oder online auf Scribd lesen
0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
3 Ansichten3 SeitenPD1011 DPT Residents
Hochgeladen von
568563PD1011 Dpt Residents
Copyright:
© All Rights Reserved
Verfügbare Formate
Als PDF, TXT herunterladen oder online auf Scribd lesen
Sie sind auf Seite 1von 3
P
soriasis is a chronic relapsing skin disease that
takes on a wide spectrum of clinical morphology
and courses. The cutaneous diagnosis can usual-
ly be made by a visually literate physician, yet
deeper effects often traverse the skin and influence
both the emotional and social aspects of a patients
life.
1
This report illustrates a case of a patient who
developed erythrodermic psoriasis after a combination
of radiation treatment and a lumpectomy for breast
cancer. With minimal current publishings on this
topic, our hope is to uncover some of the enigmatic
features of psoriasis by presenting evidence and devel-
oping a foundation in which further investigation
could benefit patients.
Case Report
A 68-year-old African-American female presented to
the office with a five-week history of diffuse erythro-
derma along with orange-salmon colored erythema
and overlying scale with some islands of sparing. The
patient had noticed a greater involvement since the
onset five weeks prior and admitted to xerosis and
pruritis while denying swollen joints and nail changes.
Patient had a history of plaque psoriasis that was first
diagnosed in February 2008 and treated with etaner-
cept (Enbrel, Amgen/Pfizer) four times and topical
steroids according to the patient. Patient stated that by
the summer of 2008 her psoriasis had remitted close
to 100 percent. In December 2008, the patient was
diagnosed with breast cancer of unknown type and
subsequently treated with a lumpectomy in February
2009 followed by radiation treatment. Six weeks prior
to her current presentation, the patient had completed
radiation treatment for her breast cancer that had
been issued intermittently for approximately three to
four months. Patient has no family history of psoriasis
and past medical history is as above.
A 4mm punch biopsy was obtained from the left
forearm using both lesional and perilesional skin for
H&E and immunofluorescence studies. The biopsy
report revealed parakeratosis, a pale staining epider-
mis, hypogranulosis, psoriasiform acanthosis, superfi-
cial dilated blood vessels, and Munro microabscesses.
Patient was given Avene spray (Pierre Fabre) to be
applied twice a day for a calming and soothing effect
followed by the application of Betamethasone
Diproprionate augmented cream 0.05% applied twice
a day for two weeks and told to return in two weeks.
Upon follow up, patient was started on narrow band
UVB therapy at 350 joules, increasing at 60-joule inter-
vals two-to-three times weekly. Patient tolerated light
therapy without any complications and positive results
were seen at later appointments.
Histopathology
Skin biopsies of erythrodermic psoriasis are common-
ly unrewarding, and it can be difficult to discern an
etiologic diagnosis.
2
Classical histology findings include
a resemblance to early lesions of psoriasis with mild
epidermal hyperplasia, red blood cell extravasation in
the papillary dermis, mounds of parakeratosis with
few neutrophils, and dilated blood vessels in the upper
dermis.
2-4
Broken down into layers, the epidermis will
demonstrate mild spongiosis, moderate acanthosis,
Erythrodermic Psoriasis Post
Radiation Treatment: A Case
Presentation and Literature Review
With limited coverage in the literature, erythrodermic psoriasis post radiation deserves further study.
By Christopher Cook, DO, Khonnie Wongkittiroch, DO, Richard Miller, DO
Residents Report
36 | Practical Dermatology | October 2011
and possible psoriasiform hyperplasia.
2,3
The upper
dermis can have a considerable chronic inflammatory
cell infiltrate with occasional exocytosis of lympho-
cytes.
2,3
Discussion
Erythrodermic psoriasis is a severe, unstable, highly
labile disease that is characterized by widespread ery-
thema, edema, superficial desquamation, and systemic
signs.
3,4
Less than 2.5 percent of psoriasis cases com-
prise an erythrodermic pattern, yet there is a substan-
tial increase in risk for morbidity and mortality when
compared to the more common forms.
5
With a wide range of severity and acuity, the major-
ity of cases feature greater than 75 percent inflamma-
tion of body surface area.
6
This systemic inflammatory
response may appear as the initial manifestation of
psoriasis, however it usually occurs in patients with
previous chronic disease. The differential diagnosis
includes but is not limited to plaque psoriasis, pityria-
sis rubra pilaris, cutaneous T-cell lymphoma, pemphi-
gus foliaceous, contact dermatitis, lichen planus, and
seborrheic dermatitis.
4-6
Provocative factors range from
systemic and topical steroids to heightened emotional
stress and preceding illness, such as infection.
4
Our
case demonstrates the incidence of erythrodermic pso-
riasis post radiation therapy for breast cancer.
To date, there is a paucity of literature describing
this association, creating an uncharted path in which
we can expand our efforts to formulate more facts and
new hypotheses. Nevertheless, there is evidence of an
association between radiation therapy and cutaneous
side effects.
7
This phenomenon occurs more common-
ly in patients with incidental skin disorders and can
be traced back to 1876 when Heinrich Koebner first
described the development of psoriatic lesions follow-
ing an injury to clear skin on a patient with psoriasis.
By definition, the Koebner phenomenon is an iso-
morphic cutaneous response to trauma of normal
appearing skin.
7
It is thought that radiation therapy
may initiate skin damage and promote
Koebnerization.
7
The few case reports that exist
regarding the occurrence of psoriasis post radiation
therapy in breast cancer patients paint a portrait of a
Figs. 1-3. Patient at initial presentation.
Figs. 4-6. Patient post narrow band UVB treatment.
Fig. 1 Fig, 2 Fig. 3
Fig. 4 Fig. 5 Fig. 6
Residents Report
October 2011 | Practical Dermatology | 37
cutaneous response only locally in the irradiated
fields. One case described by Charalambous and
Bloomfield entails a patient with breast cancer that
manifested a florid erythema over the entire irradiated
breast four weeks post radiation treatment.
8
In a dif-
ferent case, Tomlinson highlights a breast cancer
patient who received a mastectomy followed by radia-
tion treatment.
9
Six weeks following the completion of
radiation therapy, the patient had a flare up of psoria-
sis in the irradiated area while the non-irradiated area
remained unblemished.
9
A third case of Koebnerization is illustrated by
Schreiber, who reported on a patient with metastatic
lung cancer to the femur.
10
Two weeks after receiving
radiotherapy of the femur, the patient experienced a
significant local psoriatic reaction.
10
Interestingly, the
majority of cases transpired between two to six weeks
post radiation therapy, a time frame that matches our
patients manifestation at six weeks. Compared to
these reports, our case is unique in that the patient
developed a generalized response instead of the afore-
mentioned local reactions.
These patients, much like those who have sustained
burns, must be treated aggressively due to an
increased risk of infection, severe dehydration, and
electrolyte imbalance. Currently, there is a lack of
quality scientific evidence on which to base a treat-
ment regimen for erythrodermic psoriasis.
5
With this
in mind, treatment considerations are centered around
the severity of disease at the time of presentation as
well as a patients comorbidities.
First line agents include the rapidly acting
cyclosporine and infliximab (Remicade, Janssen
Biotech), as well as the slower acting acitretin and
methotrexate.
5
Topical therapy should be implemented
with systemic treatment as encouraged by the medical
board.
5
Furthermore, physicians can also choose com-
bination therapy in cases that are acutely severe with
a need for urgent control or in patients that are refrac-
tory to single agents alone.
5
Combination therapy may
be more effective than monotherapy; however there is
a scarcity of data to support this.
5
Although UV light therapy is a buttress of psoriasis
management, it should be used cautiously in acute
erythrodermic cases. There are case reports of UV-
induced erythroderma as well as an increased risk of a
Koebnerization-like response.
5
There have been posi-
tive results of Psoralen plus UV therapy in erythroder-
mic psoriasis, but prudence must be taken to avoid
flare precipitation in these sensitive patients.
5
In summary, erythrodermic psoriasis is a serious
and complex disease that still requires further investi-
gation and a novel approach in regards to etiology and
treatment considerations. From a review of the litera-
ture, we believe that there is a positive correlation
between radiation therapy and psoriasis development
through a Koebnerization response. By publishing case
reports and propagating creative discussions, our
ambition is to build upon what we do know and ques-
tion what is still unknown.
The authors have no relevant disclosures.
Christopher Cook, DO is a Cutaneous Oncology Research
Assistant at Moffitt Cancer Center, Tampa, FL.
Khonnie Wongkittiroch, DO is a 3rd year Dermatology Resident
at Largo Medical Center, Largo, FL.
Richard Miller, DO is Dermatology Program Director at Largo
Medical Center, Largo, FL.
1. Jackson R. The importance of being visually literate. Observations on the art and science
of making a morphological diagnosis in dermatology. Arch Dermatol 1975;111:632-6.
2. Tomasini C, Aloi F, Solaroli C, Pippione M. Psoriatic erythroderma: a histopathologic
study of forty-five patients. Dermatology. 1997;194:102106.
3. Walsh NMG, Prokopetz R, Tron VA, et al.. Histopathology in erythroderma: review of a
series of cases by multiple observers. J Cutan Pathol. 1994;21:419423.
4. MD Consult. Erythrodermic Psoriasis. Available at http://www.mdconsult.com.ezproxylo-
cal.library.nova.edu/book/player/book.do?method=display&type=bookPage&decorator=he
ader&eid=4-u1.0-B978-0-7234-3541-9..00017-1--s0150&uniq=194100703&isbn=978-0-
7234-3541-9&sid=980718923. Accessed December 1, 2009.
5. Rosenbach, M., Hsu S., Korman N., Lebwohl M., Young M., Bebo B., Voorhees A.
Treatment of erythrodermic psoriasis: From the medical board of the National Psoriasis
Foundation. Journal of American Academy of Dermatology. 2009;
doi:10.1016/j.jaad.2009.05.048
6. Boyd, AS, Menter, A. Erythrodermic psoriasis; precipitating factors, course, and progno-
sis in 50 patients. Journal of American Academy of Dermatology. 1989;21: 985-91.
7. Ben-Yosef, R., Soyfer, V., Vexler, A. Radiation therapy in cancer patients with psoriasis.
The fractionated daily dose and the Koebner phenomenon. Radiotherapy and Oncology.
2005;74: 21-23.
8. Charalambous, H., & Bloomfield, D. Psoriasis and radiotherapy: exacerbation of psoriasis
following radiotherapy for carcinoma of the breast (the Koebner phenomenon). Clinical
Oncology (Royal College Of Radiologists (Great Britain)). 2000; 12(3), 192-193.
9. Tomlinson, M. Psoriasis and radiotherapy. Clinical Oncology (Royal College Of
Radiologists (Great Britain)). 2001; 13(2), 145.
10. Schreiber GJ, Muller-Runkel R. Exacerbation of psoriasis after megavoltage irradiation.
Cancer 1991;67: 588-9.
11. Zip C, Murray S, Walsh NMG. The specificity of histopathology in erythroderma. J Cutan
Pathol. 1993;20:393398.
Residents Report
38 | Practical Dermatology | October 2011
Das könnte Ihnen auch gefallen
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- Simply Learn Hebrew! How To Lea - Gary Thaller PDFDokument472 SeitenSimply Learn Hebrew! How To Lea - Gary Thaller PDFsuper_gir95% (22)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- Volvo FM/FH with Volvo Compact Retarder VR 3250 Technical DataDokument2 SeitenVolvo FM/FH with Volvo Compact Retarder VR 3250 Technical Dataaquilescachoyo50% (2)
- 1803 Hector Berlioz - Compositions - AllMusicDokument6 Seiten1803 Hector Berlioz - Compositions - AllMusicYannisVarthisNoch keine Bewertungen
- FraudDokument77 SeitenFraudTan Siew Li100% (2)
- Global Supplier Quality Manual SummaryDokument23 SeitenGlobal Supplier Quality Manual SummarydywonNoch keine Bewertungen
- CARET Programme1 Bennett-1Dokument10 SeitenCARET Programme1 Bennett-1TerraVault100% (3)
- Kargil Untold StoriesDokument214 SeitenKargil Untold StoriesSONALI KUMARINoch keine Bewertungen
- Julian's GodsDokument162 SeitenJulian's Godsअरविन्द पथिक100% (6)
- TCW The Global CityDokument40 SeitenTCW The Global CityAllen Carl100% (1)
- Flu Specimen Collection PosterDokument1 SeiteFlu Specimen Collection Poster568563Noch keine Bewertungen
- Tatalaksana Hipoksemia Akut CovidDokument31 SeitenTatalaksana Hipoksemia Akut CovidLilis Sumiyati100% (1)
- c05790186 PDFDokument137 Seitenc05790186 PDFAngelli GuingueNoch keine Bewertungen
- TapScanner 24-03-2021-15.19Dokument1 SeiteTapScanner 24-03-2021-15.19568563Noch keine Bewertungen
- Vertigo Blok15Dokument23 SeitenVertigo Blok15Mul YaniNoch keine Bewertungen
- 4713-7 8.16 Afzaninawati Suria YusofDokument5 Seiten4713-7 8.16 Afzaninawati Suria Yusof568563Noch keine Bewertungen
- Vol1 No1 4Dokument5 SeitenVol1 No1 4568563Noch keine Bewertungen
- List Obat BP Lanal SorongDokument3 SeitenList Obat BP Lanal Sorong568563Noch keine Bewertungen
- JaundiceDokument16 SeitenJaundicemanognaaaaNoch keine Bewertungen
- Curriculum VitaeDokument2 SeitenCurriculum Vitae568563Noch keine Bewertungen
- Risk-adjusted 30-day mortality rates after colorectal cancer surgery in EnglandDokument9 SeitenRisk-adjusted 30-day mortality rates after colorectal cancer surgery in England568563Noch keine Bewertungen
- Gastroenterol. Rep. 2014 Parikh Gastro Gou081Dokument3 SeitenGastroenterol. Rep. 2014 Parikh Gastro Gou081568563Noch keine Bewertungen
- Congestive Heart FailureDokument43 SeitenCongestive Heart Failure568563100% (1)
- Hyperbilirubinemia FinalDokument26 SeitenHyperbilirubinemia Final568563Noch keine Bewertungen
- HI! I'm Emily and Here To Tell You To Pay Attention... This Isa Really Great Talk!!!!!!!!!! Have You Seen My Brother? He's Sooooa AnnoyingDokument18 SeitenHI! I'm Emily and Here To Tell You To Pay Attention... This Isa Really Great Talk!!!!!!!!!! Have You Seen My Brother? He's Sooooa Annoying568563Noch keine Bewertungen
- Acute Decompensated Heart FailureDokument31 SeitenAcute Decompensated Heart Failure568563Noch keine Bewertungen
- Erythroderma Caused Drug Allergies: Case ReportDokument7 SeitenErythroderma Caused Drug Allergies: Case Report568563Noch keine Bewertungen
- 2013 Acc Aha Guideline On The Treatment of Blood Cholesterol To Reduce Athersclerotic Risk 2Dokument67 Seiten2013 Acc Aha Guideline On The Treatment of Blood Cholesterol To Reduce Athersclerotic Risk 2HidayadNoch keine Bewertungen
- ALS Drug SummaryDokument1 SeiteALS Drug Summary568563Noch keine Bewertungen
- PERIODE GASAL 2013/2014 Tugas: Program Studi ArsitekturDokument1 SeitePERIODE GASAL 2013/2014 Tugas: Program Studi Arsitektur568563Noch keine Bewertungen
- PERIODE GASAL 2013/2014 Tugas: Program Studi ArsitekturDokument1 SeitePERIODE GASAL 2013/2014 Tugas: Program Studi Arsitektur568563Noch keine Bewertungen
- 283 560 1 PBDokument5 Seiten283 560 1 PB568563Noch keine Bewertungen
- Combined Intravitreal Ranibizumab and Verteporfin Photodynamic Therapy Versus Ranibizumab Alone For The Treatment of Age-Related Macular DegenerationDokument5 SeitenCombined Intravitreal Ranibizumab and Verteporfin Photodynamic Therapy Versus Ranibizumab Alone For The Treatment of Age-Related Macular Degeneration568563Noch keine Bewertungen
- Bronchopleural Fistula Treatment OptionsDokument3 SeitenBronchopleural Fistula Treatment Options568563Noch keine Bewertungen
- Erythroderma: A Clinicopathological Study of 102 Cases: Original ArticleDokument6 SeitenErythroderma: A Clinicopathological Study of 102 Cases: Original Article568563Noch keine Bewertungen
- Critical Appraisal PrognosisDokument4 SeitenCritical Appraisal Prognosis568563Noch keine Bewertungen
- 68 Year Old Man Pags 71 A 75Dokument5 Seiten68 Year Old Man Pags 71 A 75568563Noch keine Bewertungen
- Short-Term Outcomes of Tonsillectomy in Adult Patients With Recurrent Pharyngitis: A Randomized Controlled TrialDokument1 SeiteShort-Term Outcomes of Tonsillectomy in Adult Patients With Recurrent Pharyngitis: A Randomized Controlled Trial568563Noch keine Bewertungen
- Short-Term Outcomes of Tonsillectomy in Adult Patients With Recurrent Pharyngitis: A Randomized Controlled TrialDokument1 SeiteShort-Term Outcomes of Tonsillectomy in Adult Patients With Recurrent Pharyngitis: A Randomized Controlled Trial568563Noch keine Bewertungen
- EB - Lecture 2 - ECommerce Revenue Models - HDokument8 SeitenEB - Lecture 2 - ECommerce Revenue Models - HXolani MpilaNoch keine Bewertungen
- UAE Cooling Tower Blow DownDokument3 SeitenUAE Cooling Tower Blow DownRamkiNoch keine Bewertungen
- Derivatives 17 Session1to4Dokument209 SeitenDerivatives 17 Session1to4anon_297958811Noch keine Bewertungen
- Sadhu or ShaitaanDokument3 SeitenSadhu or ShaitaanVipul RathodNoch keine Bewertungen
- Intel It Aligning It With Business Goals PaperDokument12 SeitenIntel It Aligning It With Business Goals PaperwlewisfNoch keine Bewertungen
- Understanding Learning Theories and Knowledge AcquisitionDokument38 SeitenUnderstanding Learning Theories and Knowledge AcquisitionKarl Maloney Erfe100% (1)
- Part 4: Implementing The Solution in PythonDokument5 SeitenPart 4: Implementing The Solution in PythonHuỳnh Đỗ Tấn ThànhNoch keine Bewertungen
- Term2 WS7 Revision2 PDFDokument5 SeitenTerm2 WS7 Revision2 PDFrekhaNoch keine Bewertungen
- Barnett Elizabeth 2011Dokument128 SeitenBarnett Elizabeth 2011Liz BarnettNoch keine Bewertungen
- Dr. Xavier - MIDokument6 SeitenDr. Xavier - MIKannamundayil BakesNoch keine Bewertungen
- It ThesisDokument59 SeitenIt Thesisroneldayo62100% (2)
- Walter Horatio Pater (4 August 1839 - 30 July 1894) Was An English EssayistDokument4 SeitenWalter Horatio Pater (4 August 1839 - 30 July 1894) Was An English EssayistwiweksharmaNoch keine Bewertungen
- Branch ListDokument65 SeitenBranch Listannamichelle1001Noch keine Bewertungen
- Solar Presentation – University of Texas Chem. EngineeringDokument67 SeitenSolar Presentation – University of Texas Chem. EngineeringMardi RahardjoNoch keine Bewertungen
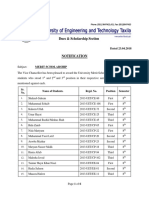
- Dues & Scholarship Section: NotificationDokument6 SeitenDues & Scholarship Section: NotificationMUNEEB WAHEEDNoch keine Bewertungen
- Coursebook 1Dokument84 SeitenCoursebook 1houetofirmin2021Noch keine Bewertungen
- Intro to Financial Management Chapter 1 SummaryDokument11 SeitenIntro to Financial Management Chapter 1 SummaryweeeeeshNoch keine Bewertungen
- Social Responsibility and Ethics in Marketing: Anupreet Kaur MokhaDokument7 SeitenSocial Responsibility and Ethics in Marketing: Anupreet Kaur MokhaVlog With BongNoch keine Bewertungen
- Reduce Home Energy Use and Recycling TipsDokument4 SeitenReduce Home Energy Use and Recycling Tipsmin95Noch keine Bewertungen
- Ivan PavlovDokument55 SeitenIvan PavlovMuhamad Faiz NorasiNoch keine Bewertungen
- Study Habits Guide for Busy StudentsDokument18 SeitenStudy Habits Guide for Busy StudentsJoel Alejandro Castro CasaresNoch keine Bewertungen