Beruflich Dokumente
Kultur Dokumente
Silicone Lymphadenopathy - An Unexpected Cause
Hochgeladen von
entgo8282Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Silicone Lymphadenopathy - An Unexpected Cause
Hochgeladen von
entgo8282Copyright:
Verfügbare Formate
Silicone lymphadenopathy: an unexpected cause
of neck lumps
E OMAKOBIA
1
, G PORTER
1
, S ARMSTRONG
2
, K DENTON
3
Departments of
1
ENT,
2
Radiology, and
3
Histopathology, Southmead Hospital, Bristol, UK
Abstract
Objective: To report a rare case of silicone lymphadenopathy solely affecting the left supraclavicular lymph nodes.
Case report: Our patient presented with a painless swelling in the left supraclavicular region. Notably, she had
previously undergone cosmetic breast augmentation using silicone-containing implants. Radiological imaging and
subsequent excisional biopsy of the swelling produced findings consistent with a silicone foreign body reaction
secondary to bilateral breast implant rupture.
Conclusion: Silicone lymphadenopathy following breast augmentation primarily affects the axillary nodes.
Supraclavicular lymph node involvement is unusual. To our knowledge, this is the first report in the English
language literature of silicone lymphadenopathy manifesting solely in the supraclavicular lymph nodes.
Although the need to exclude malignancy in such cases is of the utmost importance, silicone lymphadenopathy
should also be considered in the differential diagnosis. Fine needle aspiration cytology is a useful initial
investigation, which may be followed up by excisional biopsy and histological analysis for further confirmatory
diagnostic information.
Key words: Breast Implants; Mammoplasty; Silicone; Lymphadenopathy; Neck
Introduction
Silicone lymphadenopathy is defined as the presence of
silicone in a lymph node, and is an uncommon compli-
cation of using silicone prostheses for either joints or
plastic surgical procedures, specifically breast augmen-
tation or reconstruction.
1,2
Such cases pose a diagnostic
challenge as malignancy is often the initial consider-
ation. In this report, we discuss a rare case of silicone
lymphadenopathy occurring in the supraclavicular
lymph nodes of a patient with a prior history of cos-
metic augmentation mammoplasty with silicone
implants. In such cases, fine needle aspiration cytology
(FNAC) is a useful initial investigation and may be suf-
ficient for diagnosis. If inconclusive, excisional biopsy
of the affected lymph node for histological analysis
should also be performed.
3
Case report
A 52-year-old woman presented to the ENT out-patient
clinic with a two-month history of a non-tender lump in
the left supraclavicular region, having been referred by
her general practitioner. There was no history of dys-
phagia, dysphonia or otalgia, and on questioning she
reported no weight loss, poor appetite, feverishness or
night sweats. She had a 10 pack-year smoking
history. She reported having undergone bilateral
breast augmentation for cosmetic purposes 13 years
earlier, and was currently being treated for hyperthyr-
oidism, but there was no other past medical history of
note.
Clinical examination confirmed a well circum-
scribed, firm, non-tender, 2 cm lump in the left supra-
clavicular fossa. No lymphadenopathy was noted
elsewhere, and examination of the ears, nose and
throat was otherwise unremarkable.
An initial ultrasound scan of the neck revealed
several areas of abnormal, increased echogenicity in
the left supraclavicular fossa (Figure 1). A 0.5 cm, ill-
defined nodule in the thyroid isthmus was also noted,
which was initially thought to be the primary site of
pathology. Fine needle aspiration of the thyroid
lesion unfortunately yielded an insufficient specimen
for diagnosis; hence, further investigations were per-
formed. The differential diagnoses considered at this
stage included primary head and neck malignancy,
metastasis, lymphoma and reactive lymphadenopathy
secondary to infection such as tuberculosis.
A subsequent magnetic resonance imaging scan of
the neck demonstrated a cluster of abnormal left level
IV lymph nodes (Figure 2).
The patient was recalled for fine needle aspiration of
one of these lymph nodes. Cytological examination
Accepted for publication 29 March 2012 First published online 7 June 2012
The Journal of Laryngology & Otology (2012), 126, 970973. CLINICAL RECORD
JLO (1984) Limited, 2012
doi:10.1017/S0022215112001089
showed a background of lymphocytes, numerous
clusters of adipocytes, and a significant number of mul-
tinucleate giant cells with ingested fatty material. No
features of malignancy were seen (Figure 3).
Since no definitive cytological diagnosis could be
made, the patient was scheduled for direct endoscopy
of the upper aerodigestive tract and excisional biopsy
of the enlarged left supraclavicular lymph node. On
macroscopic inspection, the specimen was solid and
grey-white in colour. Endoscopy of the pharynx,
larynx and upper oesophagus was unremarkable.
Histological analysis identified a lymph node which
had largely been replaced by foreign material
masses, with a pronounced foreign body response
(Figure 4). No evidence of malignancy was seen. It
was concluded that the appearances were in keeping
with a foreign body response to silicone from a
leaking breast implant. Tissue culture yielded no
growth and no acid-alcohol-fast bacilli were seen on
direct staining, making a diagnosis of tuberculosis
unlikely.
Subsequent computed tomography (CT) scanning of
the neck, thorax, abdomen and pelvis revealed no lung
or mediastinal lesions. Apart from small nodes in the
porta hepatis, which were deemed to be within normal
limits, no other areas of lymphadenopathy were seen.
Hence, a diagnosis of lymphoma was very unlikely.
The CT images were later reviewed by a breast radiol-
ogist who noted irregularity of the capsule of both
breast implants, consistent with bilateral rupture (this is
termed the linguine sign) (Figure 5).
The patient was reassured that malignancy had not
been detected. She was referred back to the plastic
surgeon who had performed the original breast aug-
mentation, with a view to further assessment of
leakage or rupture of the silicone breast prostheses.
FIG. 1
Ultrasound scan of the neck showing abnormally increased echo-
genicity in the left supraclavicular fossa. In retrospect, this is the
classically described snowstorm appearance of silicone in lymph
nodes.
FIG. 2
Coronal magnetic resonance imaging scan of the neck demonstrat-
ing a cluster of abnormal left level IV lymph nodes.
FIG. 3
Photomicrograph of fine needle aspiration cytology specimen from
the abnormal left level IV lymph nodes, showing multinucleate
giant cells together with macrophages containing clear material.
(May Grunwald Giemsa stain; 400)
FIG. 4
Photomicrograph of left enlarged supraclavicular lymph node fol-
lowing excisional biopsy, showing that normal lymph node contents
have been displaced by multinucleate giant cells and clear globular
areas (where the silicone is located). (H&E; 200)
CLINICAL RECORD 971
Discussion
Silicone lymphadenopathy, involving a foreign body
reaction to silicone, is a well documented complication
of breast augmentation using silicone-containing
materials.
1,4
It has been postulated that silicone can migrate
through tissues via two distinct mechanisms: firstly,
through rupture or erosion of a silicone-containing
surface; or secondly, through continued leakage
through an intact surface.
5,6
When silicone tissue
migration occurs via either of these mechanisms, fibro-
sis and foreign body granulomatous reactions can
occur.
7
Silicone particles may be transported to
regional lymph nodes via macrophages in the reti-
culo-endothelial system.
3
The resulting foreign body
reaction may produce local swelling of the involved
lymph node, such as the left supraclavicular lymph
nodes in the case reported.
Silicone lymphadenopathy following breast
augmentation primarily affects the axillary nodes,
5,8
but there have been reported cases involving intramam-
mary,
4
internal mammary
9
and supraclavicular lymph
nodes.
10
The current case is particularly unusual in
that, to our knowledge, it is the first reported case of
silicone lymphadenopathy manifesting solely in a
supraclavicular lymph node in a patient with no prior
history of breast cancer. Shipchandler et al. described
a similar case of supraclavicular lymphadenopathy
due to silicone breast implants in 2007; however, this
patient later developed bilateral axillary silicone
lymphadenopathy.
Silicone lymphadenopathy poses important clinical
considerations in the approach to the patient with a
lump in the neck or axilla and a prior history of silicone
augmentation mammoplasty. Although the clinicians
initial priority should be to exclude malignancy, it is
important to note whether there is any prior history of
breast augmentation using silicone-containing
materials. If not considered in the initial differential
diagnosis, silicone foreign body reaction is a difficult
diagnosis to arrive at. Furthermore, in patients who
have had breast cancer treated with mastectomy fol-
lowed by reconstructive mammoplasty using silicone
gel implants, the possibility of metastatic breast
cancer should obviously be high in the differential
diagnosis; however, silicone lymphadenopathy should
not be disregarded. For the majority of individuals
who have had silicone augmentation mammoplasty
purely for cosmetic purposes, silicone lymphadenopa-
thy should be considered, in addition to a possible
new diagnosis of malignancy.
Once a silicone foreign body reaction is suspected,
FNAC of the affected lymph node has been shown to
be a cost-effective and accurate initial investigation to
aid diagnosis.
3,11
In such cases, FNAC shows a
foreign body reactive, lymphoid background with
numerous giant cells, as in the case described. If
there is clinical suspicion of silicone lymphadenopathy,
FNAC alone may be sufficient for a definitive diagno-
sis. However, if FNAC is inconclusive, or if other,
more sinister diagnoses are suspected, a conservative
excisional lymph node biopsy is advisable to provide
a histological diagnosis and to exclude concomitant
malignancy.
3
Silicone lymphadenopathy is a rare
complication of procedures involving silicone
Axillary lymph nodes are the most commonly
affected after silicone mammoplasty
Supraclavicular lymph nodes are very rarely
involved
Malignancy is the most important differential
diagnosis
Diagnosis is by fine needle aspiration
cytology, plus excisional biopsy histology if
needed
Plastic or breast surgeons should assess
implant leakage or rupture before
considering removal
Here, we describe a rare case of supraclavicular lym-
phadenopathy secondary to silicone foreign body reac-
tion. In patients with a prior history of silicone
augmentation mammoplasty, silicone lymphadenopa-
thy should be considered in the differential diagnosis
of supraclavicular neck lumps. However, the initial pri-
ority in such cases should be to exclude malignancy.
Fine needle aspiration cytology may be sufficient for
diagnosis, but in the absence of conclusive findings
excisional biopsy should also be performed to
provide a histological diagnosis.
FIG. 5
Axial, arterial phase, soft tissue window, computed tomography
scan of the thorax, demonstrating irregularity of the capsule of
both breast implants (the linguine sign) consistent with bilateral
rupture.
E OMAKOBIA, G PORTER, S ARMSTRONG et al. 972
Conclusion
Silicone lymphadenopathy is a rare but recognised
complication of procedures involving the use of sili-
cone. In the case of silicone augmentation mammo-
plasty, the axillary lymph nodes are the most
commonly affected site; very rarely, the supraclavicular
lymph nodes may be involved. In such cases, malig-
nancy is the most important differential diagnosis, but
silicone lymphadenopathy should also be considered.
Although fine needle aspiration cytology alone may
be sufficient for definitive diagnosis, in doubtful
cases lymph node excisional biopsy should also be per-
formed for histological analysis. Affected patients
should be referred to a plastic or breast surgeon for
assessment of implant leakage or rupture before
removal is considered.
References
1 Truong LD, Cartwright J Jr, Goodman MD, Woznicki D.
Silicone lymphadenopathy associated with augmentation mam-
moplasty. Morphologic features of nine cases. Am J Surg Pathol
1988;12:48491
2 Christie AJ, Weinberger KA, Dietnich M. Silicone lymphadeno-
pathy and synovitis: complications of silicone elastomer finger
joint prostheses. JAMA 1977;237:14634
3 Tabatowski K, Elson CE, Johnston WW. Silicone lymphadeno-
pathy in a patient with mammary prosthesis. Fine needle aspira-
tion cytology, histology and analytical electron microscopy.
Acta Cytol 1990;34:1014
4 Rivero MA, Schwartz DS, Mies C. Silicone lymphadenopathy
involving intramammary lymph nodes: a new complication of
silicone mammoplasty. AJR Am J Roentgenol 1994;162:
108990
5 Adams ST, Cox J, Rao GS. Axillary silicone lymphadenopathy
presenting with a lump and altered sensation in the breast: a case
report. J Med Case Reports 2009;3:6442
6 Hausner RJ, Schoen FJ, Mendez-Fernandez MA, Henly WS,
Geis RC. Migration of silicone gel to axillary lymph nodes
after prosthetic mammoplasty. Arch Pathol Lab Med 1981;
105:3712
7 Van Diest PJ, Beekman WH, Hage JJ. Pathology of silicone
leakage from breast implants. J Clin Pathol 1998;51:4937
8 Kulber DA, MacKenzie D, Steiner JH, Glassman H, Hopp D,
Hiatt JR et al. Monitoring the axilla in patients with silicone
gel implants. Ann Plast Surg 1995;35:5804
9 Kao CC, Rand RP, Holt CA, Pierce RH, Timmons JH, Wood
DE. Internal mammary silicone lymphadenopathy mimicking
recurrent breast cancer. Plast Reconstr Surg 1997;99:2259
10 Shipchandler TZ, Lorenz RR, McMahon J, Tubbs R.
Supraclavicular lymphadenopathy due to silicone breast
implants. Arch Otolaryngol Head Neck Surg 2007;133:8302
11 Santos-Briz A Jr, Lopez-Rios F, Santos-Briz A, De Agustin PP.
Granulomatous reaction to silicone in axillary lymph nodes a
case report with cytologic findings. Acta Cytol 1999;43:11635
Address for correspondence:
Dr Eugene Omakobia,
ENT Clinical Fellow,
ENT Department,
Southmead Hospital,
Bristol BS10 5NB, UK
Fax: +44 (0)117 323 5850
E-mail: eugeneomakobia@doctors.org.uk
Dr E Omakobia takes responsibility for the integrity
of the content of the paper
Competing interests: None declared
CLINICAL RECORD 973
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Case Presentation SiliconomaDokument24 SeitenCase Presentation Siliconomaentgo8282Noch keine Bewertungen
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- Complications After Facial Contour Augmentation With Injectable Silicone. Diagnosis and Treatment. Report of A Severe CaseDokument6 SeitenComplications After Facial Contour Augmentation With Injectable Silicone. Diagnosis and Treatment. Report of A Severe Caseentgo8282Noch keine Bewertungen
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Silicone Migration To The Contralateral Axillary Lymph Nodes and Breast After Highly Cohesive Silicone Gel Implant FailureDokument3 SeitenSilicone Migration To The Contralateral Axillary Lymph Nodes and Breast After Highly Cohesive Silicone Gel Implant Failureentgo8282Noch keine Bewertungen
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (894)
- Posterior TympanotomyDokument6 SeitenPosterior Tympanotomyentgo8282Noch keine Bewertungen
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Simultaneous Presentation of Silicone and Silica GranulomaDokument4 SeitenSimultaneous Presentation of Silicone and Silica Granulomaentgo8282Noch keine Bewertungen
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Fitting and Modifying Hearing InstrumentsDokument32 SeitenFitting and Modifying Hearing Instrumentsentgo8282Noch keine Bewertungen
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Neck Lymphadenitis Due To Silicone Granuloma After MammaryDokument6 SeitenNeck Lymphadenitis Due To Silicone Granuloma After Mammaryentgo8282Noch keine Bewertungen
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Cutaneous Silicone Granuloma Mimicking Breast Cancer After Ruptured Breast ImplantDokument4 SeitenCutaneous Silicone Granuloma Mimicking Breast Cancer After Ruptured Breast Implantentgo8282Noch keine Bewertungen
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- Silicone Granuloma of The Facial TissuesDokument9 SeitenSilicone Granuloma of The Facial Tissuesentgo8282Noch keine Bewertungen
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- Silicone Granuloma of The Face Treated With MinocyclineDokument4 SeitenSilicone Granuloma of The Face Treated With Minocyclineentgo8282Noch keine Bewertungen
- Locoregional Silicone Spread After High Cohesive Gel Silicone Implant RuptureDokument2 SeitenLocoregional Silicone Spread After High Cohesive Gel Silicone Implant Ruptureentgo8282Noch keine Bewertungen
- Granulomatous Reaction To Silicone InjectionDokument4 SeitenGranulomatous Reaction To Silicone Injectionentgo8282Noch keine Bewertungen
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- 5 (1) (1) .Compression of DilonDokument63 Seiten5 (1) (1) .Compression of Dilonentgo8282Noch keine Bewertungen
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- H 2 02 (1) (1) .FeedbackDokument8 SeitenH 2 02 (1) (1) .Feedbackentgo8282Noch keine Bewertungen
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Please Answer The Following Questions Based On This ScaleDokument1 SeitePlease Answer The Following Questions Based On This Scaleentgo8282Noch keine Bewertungen
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Orocraniofacial Features Clinical ScaleDokument1 SeiteOrocraniofacial Features Clinical Scaleentgo8282Noch keine Bewertungen
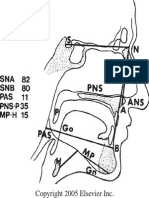
- Standard Cephalometric TracingDokument1 SeiteStandard Cephalometric Tracingentgo8282Noch keine Bewertungen
- Treatment PhilosophyDokument1 SeiteTreatment Philosophyentgo8282Noch keine Bewertungen
- Acute supraglottitis의 치료Dokument4 SeitenAcute supraglottitis의 치료entgo8282Noch keine Bewertungen
- Thyroid Isthmusectomy - A Critical AppraisalDokument4 SeitenThyroid Isthmusectomy - A Critical Appraisalentgo8282Noch keine Bewertungen
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- - 에 기침하면서 어지럼증 발생하여 앞으로 서러지고 glabella 부위 수상 택시 타고 내리다가 안면부수상Dokument14 Seiten- 에 기침하면서 어지럼증 발생하여 앞으로 서러지고 glabella 부위 수상 택시 타고 내리다가 안면부수상entgo8282Noch keine Bewertungen
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- 2010KoreanGuideline pediatricOM forSMEDDokument109 Seiten2010KoreanGuideline pediatricOM forSMEDentgo8282Noch keine Bewertungen
- BPPV in The ElderlyDokument5 SeitenBPPV in The Elderlyentgo8282Noch keine Bewertungen
- Basics of Sleep Staging CMPDokument25 SeitenBasics of Sleep Staging CMPentgo8282Noch keine Bewertungen
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- BPPV-마산, 창원 신경과Dokument38 SeitenBPPV-마산, 창원 신경과entgo8282Noch keine Bewertungen
- Case Presentation김봉태Dokument12 SeitenCase Presentation김봉태entgo8282Noch keine Bewertungen
- The Maxilla-Premaxilla Approach To Extensive Nasal Septum SurgeryDokument13 SeitenThe Maxilla-Premaxilla Approach To Extensive Nasal Septum Surgeryentgo8282100% (1)
- BPPV and Long-Term Follow-UpDokument4 SeitenBPPV and Long-Term Follow-Upentgo8282Noch keine Bewertungen
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- Case Presentation-Bilateral Peritonsillar AbscessDokument29 SeitenCase Presentation-Bilateral Peritonsillar Abscessentgo8282Noch keine Bewertungen
- Cima Do Patamar - Um Exercico de Raciocinio ClinicoDokument5 SeitenCima Do Patamar - Um Exercico de Raciocinio ClinicoFrederico PóvoaNoch keine Bewertungen
- Limci Gupta Valerie Thomas JaysoDokument285 SeitenLimci Gupta Valerie Thomas JaysoNaima TariqNoch keine Bewertungen
- Endobronchial Ultrasound: What Is It and When Should It Be Used?Dokument6 SeitenEndobronchial Ultrasound: What Is It and When Should It Be Used?Legenda AkNoch keine Bewertungen
- CUE Case History of 56 Year Old Smoker with Penile CancerDokument26 SeitenCUE Case History of 56 Year Old Smoker with Penile CancerAnil Kumar GowdaNoch keine Bewertungen
- Data Sheet 2Dokument3 SeitenData Sheet 2survery analysisNoch keine Bewertungen
- Scrofula in A Child: Insights and ImagesDokument1 SeiteScrofula in A Child: Insights and Imagesmawarni siahaanNoch keine Bewertungen
- Why Does My Patient Limphadenopathy or Splenomegaly?Dokument14 SeitenWhy Does My Patient Limphadenopathy or Splenomegaly?lacmftcNoch keine Bewertungen
- Lymphadenopathy)Dokument63 SeitenLymphadenopathy)Jaifred Christian F. LopezNoch keine Bewertungen
- Breast ExaminationDokument15 SeitenBreast ExaminationStanca GabrielNoch keine Bewertungen
- Systematic Evaluation That Produces The Ideal Treatment and The Best PrognosisDokument54 SeitenSystematic Evaluation That Produces The Ideal Treatment and The Best PrognosisKeith Mark AlmarinesNoch keine Bewertungen
- Artificial Intelligence Based Diagnosis For Cervical Lymph Node Malignancy Using The Point-Wise Gated Boltzmann MachineDokument12 SeitenArtificial Intelligence Based Diagnosis For Cervical Lymph Node Malignancy Using The Point-Wise Gated Boltzmann MachineDr.K.Meena Jeyanthi ecestaffNoch keine Bewertungen
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Background LimfadenitisDokument29 SeitenBackground LimfadenitisWahyu Permata LisaNoch keine Bewertungen
- Case Report: Yafanita Izzati Nurina, Usman HadiDokument8 SeitenCase Report: Yafanita Izzati Nurina, Usman HadiZuraidaNoch keine Bewertungen
- Masa CervicalDokument9 SeitenMasa CervicalMdacNoch keine Bewertungen
- Sesap16 Volume 1Dokument459 SeitenSesap16 Volume 1Kamil Hanna0% (1)
- Tuberculous Lymphadenitis & Lymphoma: Prof - Dr.S.P.Gayathre Chief of General Surgery Madras Medical CollegeDokument51 SeitenTuberculous Lymphadenitis & Lymphoma: Prof - Dr.S.P.Gayathre Chief of General Surgery Madras Medical CollegeAashmi ChandrikaaNoch keine Bewertungen
- Linfadenopatia Cervical 2018 PediatricsDokument13 SeitenLinfadenopatia Cervical 2018 PediatricsCarlos VegaNoch keine Bewertungen
- IV Surgery PDFDokument265 SeitenIV Surgery PDFاللهم أصلح أمريNoch keine Bewertungen
- Q2 GPA Diseases of WBCs Lymph Nodes Spleen and ThymusDokument7 SeitenQ2 GPA Diseases of WBCs Lymph Nodes Spleen and ThymusAdrian CaballesNoch keine Bewertungen
- Case Taking Proforma - Respiratory SystemDokument7 SeitenCase Taking Proforma - Respiratory SystemK Haynes Raja100% (11)
- General Inspection: ContusionDokument4 SeitenGeneral Inspection: ContusionJohnson ThomasNoch keine Bewertungen
- Tuberculous LymphadenitisDokument16 SeitenTuberculous LymphadenitisA. PathakNoch keine Bewertungen
- Lymph Nodes Normal Anatomy Major ZonesDokument5 SeitenLymph Nodes Normal Anatomy Major ZoneschristianNoch keine Bewertungen
- Diagnosing Lymphadenopathy: Approaches and ConsiderationsDokument45 SeitenDiagnosing Lymphadenopathy: Approaches and ConsiderationsYUFFANoch keine Bewertungen
- Lymphadenopathy: Lymphadenopathy Is A Term Meaning "Disease of TheDokument3 SeitenLymphadenopathy: Lymphadenopathy Is A Term Meaning "Disease of TheAbay AesculapianoNoch keine Bewertungen
- 1 - General Assessment 2023Dokument12 Seiten1 - General Assessment 2023Mohned AlhababiNoch keine Bewertungen
- Patho QuestDokument4 SeitenPatho QuestRosel Ann BontiaNoch keine Bewertungen
- Lymphadenopathy in ChildrenDokument5 SeitenLymphadenopathy in ChildrenMaria PaulaNoch keine Bewertungen
- Lymph Node EnlargementDokument6 SeitenLymph Node Enlargementlucas mansanoNoch keine Bewertungen
- Journal Benjolan Di LeherDokument9 SeitenJournal Benjolan Di LeherStase IPD SoedarsoNoch keine Bewertungen
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionVon EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionBewertung: 4 von 5 Sternen4/5 (402)
- Why We Die: The New Science of Aging and the Quest for ImmortalityVon EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityBewertung: 3.5 von 5 Sternen3.5/5 (2)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisVon EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisBewertung: 4 von 5 Sternen4/5 (1)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedVon EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedBewertung: 5 von 5 Sternen5/5 (78)
- The Age of Magical Overthinking: Notes on Modern IrrationalityVon EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityBewertung: 4 von 5 Sternen4/5 (13)