Beruflich Dokumente
Kultur Dokumente
Routine Antibiotic Use in Preterm Neonates PDF
Hochgeladen von
romeoenny41540 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
16 Ansichten5 SeitenImmature immune system of preterm neonates puts them at higher risk of sepsis. Routine antibiotic treatment was compared with no antibiotics unless clinically indicated.
Originalbeschreibung:
Originaltitel
Routine antibiotic use in preterm neonates.pdf
Copyright
© © All Rights Reserved
Verfügbare Formate
PDF, TXT oder online auf Scribd lesen
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenImmature immune system of preterm neonates puts them at higher risk of sepsis. Routine antibiotic treatment was compared with no antibiotics unless clinically indicated.
Copyright:
© All Rights Reserved
Verfügbare Formate
Als PDF, TXT herunterladen oder online auf Scribd lesen
0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
16 Ansichten5 SeitenRoutine Antibiotic Use in Preterm Neonates PDF
Hochgeladen von
romeoenny4154Immature immune system of preterm neonates puts them at higher risk of sepsis. Routine antibiotic treatment was compared with no antibiotics unless clinically indicated.
Copyright:
© All Rights Reserved
Verfügbare Formate
Als PDF, TXT herunterladen oder online auf Scribd lesen
Sie sind auf Seite 1von 5
Routine antibiotic use in preterm neonates:
a randomised controlled trial
A. Tagare*, S. Kadam, U. Vaidya, A. Pandit
Division of Neonatology, Department of Pediatrics, KEM Hospital, Rasta Peth, Pune, India
Received 22 May 2009; accepted 8 September 2009
Available online 18 November 2009
KEYWORDS
Antibiotics;
Preterm;
Routine;
Sepsis
Summary The immature immune system of preterm neonates puts them
at higher risk of neonatal sepsis. We conducted a part-blinded randomised
controlled trial to compare the effect of routine antibiotic treatment on
the incidence of clinical sepsis in pretermneonates. Pretermneonates with-
out other risk factors for infection admitted in the rst 12 h of life were ran-
domised to receive routine antibiotics or to a control group (no antibiotics
unless clinically indicated). The primary outcome variable was the inci-
dence of clinical sepsis. Secondary outcomes were the incidence of positive
blood cultures, necrotising enterocolitis (NEC) stage II or III, or death, and
the duration of hospital stay. The incidence of clinical sepsis was compara-
ble in both groups (intervention 31.9%, control 25.4%; P 0.392). Mortality
was equivalent in both groups. The control group had signicantly more pos-
itive blood cultures (P 0.002). The incidence of NEC and the duration of
hospital stay were comparable in both groups. In low risk preterm neonates
we found no evidence that routine antibiotic use has a protective effect.
2009 The Hospital Infection Society. Published by Elsevier Ltd. All rights
reserved.
Introduction
Infection is an important cause of morbidity and
mortality in neonatal intensive care units (NICUs).
Preterm infants are at higher risk of infection for
various reasons including their immature immune
response and frequent need for invasive manage-
ment. This has led to trials of routine or pro-
phylactic use of antibiotics in preterm neonates
receiving interventions such as ventilation, central
venous catheterisation and parenteral nutrition,
with variable results.
1e5
Prophylaxis using non-
absorbable enteral antibiotics has been reported
to reduce the incidence of necrotising enterocoli-
tis (NEC).
6
However, information on the role of
* Corresponding author. Address: Division of Neonatology,
Department of Pediatrics, KEM Hospital, Rasta Peth, Pune
411011, India. Tel.: 91 20 66037342; fax: 91 20 26125603.
E-mail address: docamikast@gmail.com
0195-6701/$ - see front matter 2009 The Hospital Infection Society. Published by Elsevier Ltd. All rights reserved.
doi:10.1016/j.jhin.2009.09.010
Journal of Hospital Infection (2010) 74, 332e336
Available online at www.sciencedirect.com
www.elsevierhealth.com/journals/jhin
routine systemic antibiotic use in the care of low
risk preterm neonates is limited. Hence we
designed a randomised controlled trial to compare
the incidence of clinical sepsis in preterm neo-
nates receiving antibiotics routinely with the inci-
dence in a control group.
Methods
Design and setting
A part-blinded, randomised controlled trial was
conducted between February and December 2008
in the neonatal intensive care unit at KEM Hospital,
Pune, in urban western India. This is a 40-bedded
tertiary care unit with >1200 annual admissions.
The unit caters for both inborn and outborn babies
with no segregation according to place of birth.
The unit follows strict hand-washing protocols and
has a written infection control policy. There are 11
high dependency beds. The unit has guidelines for
ventilation, parenteral nutrition and follow-up of
high risk babies.
Eligibility criteria
Preterm neonates (gestation <37 weeks) admitted
to our unit within the rst 12 h of life were eligible
for enrolment after obtaining informed parental
consent.
Exclusion criteria
(1) Maternal risk factors including leaking per
vagina for more than 24 h, fever >38
C in the
three days before delivery, foul-smelling liquor or
history of urinary tract infection; (2) fetal distress;
(3) need for resuscitation beyond positive pressure
ventilation; (4) presence of respiratory distress for
more than 6 h; (5) need for respiratory support. By
applying these exclusions our trial population con-
sisted of preterm neonates at lower risk of
infection.
Ethics approval
The study protocol was approved by the institu-
tional ethics committee.
Randomisation, allocation concealment and
blinding
Neonates eligible for enrolment were randomly
allocated either to the intervention or to the
control group using computer-generated random
numbers contained in sealed envelopes. The con-
sultant neonatologists who made clinical decisions
to initiate septic screens or antibiotics, the out-
come assessors and the statistician were masked
to the allocation status of neonates. The junior
doctors (fellows) and nursing staff were unblinded.
Intervention
Neonates in the intervention group received rst-
line intravenous antibiotics (amoxicillin clavu-
lanic acid and amikacin) for ve days from the day
of birth. The control group did not receive routine
prophylactic antibiotic treatment.
Primary outcome: incidence of sepsis
Neonates were screened for sepsis in the presence
of any four of the following clinical signs as
assessed by a neonatologist blinded to the trial
allocation: (1) sick-looking neonate; (2) tempera-
ture instability; (3) heart rate instability; (4) poor
perfusion; (5) unexplained alteration of glucose
control; (6) feed intolerance; (7) abdominal dis-
tension; (8) respiratory distress; (9) altered level
of consciousness; or (10) seizures. The sepsis
screen consisted of blood count with peripheral
smear, C-reactive protein (CRP) estimation and
blood culture. The sepsis screen was considered
positive when two or more of the following were
present: (i) total leucocyte count (TLC) <5000/mm
3
;
(ii) absolute neutrophil count <1800/mm
3
;
(iii) band to total polymorph ratio >0.2; and (iv)
CRP >1.0 mg/dL. Clinical sepsis was dened as
the presence of four or more predened clinical
features together with a positive sepsis screen.
In response to a rst episode of sepsis, in the in-
tervention group second-line antibiotics were ini-
tiated (piperacillin tazobactam and amikacin)
whereas in the control group rst-line antibiotics
were initiated (amoxicillin clavulanate and
amikacin). Antibiotics were changed according
to blood culture results. Therapeutic antibiotics
were stopped if blood cultures were negative af-
ter three days of incubation: in the intervention
group it was intended not to stop antibiotics be-
fore ve days, even if blood cultures taken in re-
sponse to clinical sepsis were negative after three
days, but in fact this situation did not arise.
Secondary outcomes
These included: (1) incidence of positive blood
cultures; (2) clinical outcomes including death,
Antibiotic use in preterm neonates 333
discharge without sepsis and treated sepsis; (3)
incidence of necrotising enterocolitis (stages II and
III by modied Bells grading);
7
and (4) duration of
hospital stay.
Sample size calculation
The incidence of clinical sepsis in our unit was 33%
overall and 25% in low risk preterm neonates. The
necessary sample size for 80% power to detect an
effect size of 20% was 63 in each limb.
Statistical methods
For statistical analysis SPSS version 11.8 was used.
ManneWhitney U-test and c
2
-test were used as
appropriate. P <0.05 were considered signicant.
Results
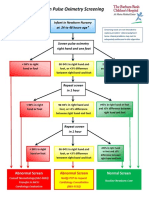
During the study period 515 preterm neonates
were admitted to the unit (Figure 1), of whom
140 were enrolled and randomised either to the
intervention (N 69) or to the control group
(N 71). Baseline characteristics (Table I) were
comparable.
The incidence of clinical sepsis was 18/71
(25.4%) in the control group and 22/69 (31.9%) in
the intervention group (P 0.392). Sepsis occurred
mainly during the rst ve days of life. Clinical
outcomes such as death, discharge without sepsis
and treated sepsis were comparable in both groups
(Table II). Two babies in each group died: three
due to NEC and one (in the control group) due to
Klebsiella pneumoniae sepsis.
We performed limited subgroup analysis accord-
ing to birth weight. Among neonates with birth
weight <1500 g the incidence of clinical sepsis was
comparable (intervention group 16/27, 59.3% vs
control group 11/26, 42.3%; P 0.217), as was
the incidence of death (intervention group 2/27,
7.4% vs control group 1/26, 3.8%; P 0.45). Among
neonates with birth weight >1500 g the incidence
of clinical sepsis was also comparable (interven-
tion group 6/42, 14.3% vs control group 7/45,
15.6%; P 0.868). Only one baby of birth weight
>1500 g died (control group).
Eleven of the 40 episodes of clinical sepsis were
associated with positive blood cultures, all of
which were deemed clinically signicant (nine
Klebsiella sp., one E. coli, one Acinetobacter bau-
mannii). However, these were not evenly distrib-
uted between the groups. Of the 18 episodes of
clinical sepsis in the control group, 10 (55.5%)
were associated with positive blood cultures,
whereas of the 22 episodes of clinical sepsis in
the intervention group only one (4.5%) was associ-
ated with positive blood cultures (P 0.002).
The duration of hospital stay was comparable in
both groups (Table II). The overall incidence of
NEC during the trial was 8.6%. In the intervention
group the incidence of NEC was 13% (9/69) while
in the control group it was 4.2% (3/71): this differ-
ence was not signicant at the 5% level (P 0.062)
but the data are compatible with the possibility
that routine antibiotics increase the incidence of
NEC.
Discussion
Before starting the study the incidence of clinical
sepsis among low risk neonates in the unit was 25%.
More than 60% of neonates admitted to this unit
are outborn and there is no segregation of inborn
and outborn neonates, which might explain the
relatively high incidence. We were keen to know
whether routine antibiotic treatment would re-
duce the incidence of sepsis. However, in this
Total no. of preterm admissions = 515
Excluded from study
Eligible for randomisation = 140
Control = 71 Intervention = 69
Age >12 h at admission = 160
Respiratory distress >6 h need for
respiratory support = 163
Resuscitation at birth = 24
Consent not requested/not given = 28
Figure 1 Distribution of study infants. Total no. of
preterm admissions 515
334 A. Tagare et al.
study, which had 80% power to detect a 20%
difference in the incidence of sepsis, neither the
incidence of clinical sepsis (31.9% vs 25.4%) nor
mortality (2.8% vs 2.9%) were signicantly differ-
ent between the intervention and control groups.
Patel et al. investigated giving postnatal peni-
cillin prophylaxis (PP) to all live-born infants.
8
This did seem to reduce the incidence of clinical
sepsis and sepsis-related deaths, mainly in neo-
nates >37 weeks of gestation and mainly due to
a reduction in group B streptococcal infection.
Most of the babies enrolled however were full
term and mothers with risk factors received ante-
natal penicillin prophylaxis, so comparison with
our trial is not appropriate.
In a randomised controlled trial involving 130
high risk neonates performed in a centre where
such babies received routine antibiotic prophy-
laxis, Auriti et al. showed that single dose ampicil-
lin and netilmicin was equivalent to a three-day
course.
9
Again this is not directly comparable
with our study, which compares routine prophy-
laxis with no routine prophylaxis in lower risk
infants, but it may be that neither of their anti-
biotic strategies was better than no antibiotics.
A notable nding in our study was that the
control group had signicantly more positive blood
cultures (10/18) than the intervention group
(1/22). A similar nding was reported when routine
penicillin prophylaxis was studied.
8
This is difcult
to explain given similar rates of clinical sepsis but
it does suggest that routine prophylaxis would
alter the positive and negative predictive values
of blood cultures, which in turn might adversely
affect decision-making in neonatal care.
Recently Cotton et al. have shown that
prolonged initial empiric antibiotic therapy in
neonates is associated with NEC.
10
In our study,
NEC occurred more frequently in the intervention
group than in the control group but this was not
statistically signicant; moreover, the study was
not powered to examine this outcome.
Table I Baseline characteristics
Parameter Control Intervention P-value
(N 71) (N 69)
Gestational age (weeks) 34.0 (29.0e36.0)
a
34.0 (27.0e36.0)
a
0.073
b
Birth weight (g) 1600 (810e2415)
a
1545 (760e2500)
a
0.812
b
Day of sepsis 4 (2e10)
a
4 (2e10)
a
0.649
b
Inborn (birth place) 45 (63.4%) 37 (53.6%) 0.241
c
Vaginal delivery 17 (23.9%) 23 (33.3%)
Elective LSCS 44 (62.0%) 36 (52.2%) 0.433
c
Emergency LSCS 10 (14.1%) 10 (14.5%)
Pregnancy-induced hypertension 36 (50.7%) 28 (40.6%)
Other maternal risk factors 20 (28.2%) 19 (27.5%) 0.118
c
No maternal risk factor 15 (21.1%) 22 (31.9%)
LSCS, lower segment caesarean section.
a
Median (range).
b
ManneWhitney U-test.
c
c
2
-Test.
Table II Secondary outcomes
Parameter Control Intervention P-value
(N 71) (N 69)
Death 2 (2.8%) 2 (2.9%)
Discharge without sepsis 53 (74.6%) 47 (68.1%) 0.678
a
Treated sepsis 16 (22.5%) 20 (29.0%)
Culture-positive sepsis 10 (14.1%) 1 (1.4%) 0.002
a
Necrotising enterocolitis 3 (4.2%) 9 (13.0%) 0.062
a
NICU stay (days) 9 (2e45)
b
9 (2e51)
b
0.932
c
NICU, neonatal intensive care unit.
a
c
2
-Test.
b
Median (range).
c
ManneWhitney U-test.
Antibiotic use in preterm neonates 335
Prophylactic antibiotics have been associated
with a lower incidence of catheter-related infec-
tions, but generally it is felt that the risk of
acquiring resistant organisms outweighs any bene-
t.
1,3,5,11
Furthermore prophylactic antibiotics did
not reduce morbidity and mortality in neonates
with central venous catheters or who were
receiving mechanical ventilation.
2,4
Antibiotic use
in NICUs is associated with the emergence of resis-
tant Gram-negative organisms such as Klebsiella
and Pseudomonas spp., whereas antenatal prophy-
laxis against group B streptococcal infection has
been shown to increase infections associated
with resistant E. coli.
12e14
Colonisation with
Gram-negative bacilli among babies in NICUs in-
creases greatly when antibiotics are continued
for more than three days, whereas antibiotics
such as ampicillin and third generation cephalo-
sporins have been shown to select for extended
spectrum b-lactamase (ESBL)-producing Gram-
negative organisms.
15e18
This phenomenon in
NICUs has been termed unnatural selection.
19
Indian NICUs are already facing antibiotic crisis,
as reected in reports of the increasing incidence
of neonatal sepsis with resistant organ-
isms.
16,17,20,21
Routine antibiotic use in the care
of preterm neonates is likely to contribute to such
problems so it is important that this strategy is criti-
cally examined. Our study suggests that in low risk
neonates routine prophylaxis is not benecial.
In conclusion, routine antibiotic use in low risk
preterm neonates does not appear to have any
protective effect. Routine antibiotic use reduces
the yield of blood cultures among babies with
clinical sepsis.
Conict of interest statement
None declared.
Funding sources
None.
References
1. Craft AP, Finer NN, Barrington KJ. Vancomycin for prophy-
laxis against sepsis in preterm neonates. Cochrane Database
Syst Rev 2004;(2):CD001971.
2. Inglis GD, Jardine LA, Davies MW. Prophylactic antibiotics to
reduce morbidity and mortality in ventilated newborn in-
fants. Cochrane Database Syst Rev 2007;(3):CD004338.
3. Harms K, Herting E, Kron M, Schiffman H, Schulz-Ehlbeck H.
Randomized, controlled trial of amoxicillin prophylaxis for
prevention of catheter-related infections in newborn in-
fants with central venous silicone elastomer catheters. J
Pediatr 1995;127:615e619.
4. Jardine LA, Inglis GDT, Davies MW. Prophylactic systemic
antibiotics to reduce morbidity and mortality in neonates
with central venous catheters. Cochrane Database Syst
Rev 2008;(1):CD006179.
5. Moller JC, Nelskamp I, Jensen R, et al. Comparison of van-
comycin and teicoplanin for prophylaxis of sepsis with coag-
ulase negative staphylococci (CONS) in very low birth
weight (VLBW) infants. J Perinat Med 1997;25:361e367.
6. Bury RG, Tudehope D. Enteral antibiotics for preventing
necrotizing enterocolitis in low birthweight or preterm in-
fants. Cochrane Database Syst Rev 2001;(1):CD000405.
7. Walsh MC, Kliegman RM. Necrotising enterocolitis: treat-
ment based on staging criteria. Pediatr Clin North Am
1986;33:179.
8. Patel DM, Rhodes PG, Le Blanc MH, Graves GR, Glick C,
Morrison J. Role of postnatal penicillin prophylaxis in pre-
vention of neonatal group B streptococcus infection. Acta
Pediatr 1999;88:874e879.
9. Auriti C, Rava` L, Di Ciommo V, Ronchetti MP, Orzalesi M.
Short antibiotic prophylaxis for bacterial infections in a neo-
natal intensive care unit: a randomized controlled trial. J
Hosp Infect 2005;59:292e298.
10. Cotten CM, Taylor S, Stoll B, et al. Prolonged duration of
initial empirical antibiotic treatment is associated with
increased rates of necrotizing enterocolitis and death for
extremely low birth weight infants. Pediatrics 2009;123:
58e66.
11. Cooke RW, Nycyk JA, Okuonghuae H, Shah V, Damjanovic V,
Hart CA. Low-dose vancomycin prophylaxis reduces coagu-
lase-negative staphylococcal bacteraemia in very low birth-
weight infants. J Hosp Infect 1997;37:297e303.
12. Arifn H, Navaratnam P, Kee TK, Balan G. Antibiotic resis-
tance patterns in nosocomial Gram-negative bacterial in-
fections in units with heavy antibiotic usage. J Trop
Pediatr 2004;50:26e31.
13. Levine EM, Ghai V, Barton JJ, Strom CM. Intrapartum anti-
biotic prophylaxis increases the incidence of gram-negative
neonatal sepsis. Infect Dis Obstet Gynecol 1999;7:210e213.
14. Hyde TB, Hilger TM, Reingold A, Farley MM, OBrien KL,
Schuchat A. Trends in incidence and antimicrobial resis-
tance of early-onset sepsis: population-based surveillance
in San Francisco and Atlanta. Pediatrics 2002;110:690e695.
15. Isaacs D. Rationing antibiotic use in the neonatal unit. Arch
Dis Child Fetal Neonatal Ed 2000;82:F1e2.
16. Jain A, Roy I, Gupta MK, Kumar M, Agarwal SK. Prevalence
of extended-spectrum beta-lactamase-producing Gram-
negative bacteria in septicaemic neonates in a tertiary care
hospital. J Med Microbiol 2003;52:421e425.
17. Krishna BVS, Patil AB, Chandrasekhar MR. Extended spec-
trum b lactamase producing Klebsiella pneumoniae in
neonatal intensive care unit. Indian J Pediatr 2007;74:
627e630.
18. Pessoa-Silva CL, Meurer Moreira B, Almeida VC, et al. Ex-
tended-spectrum beta-lactamase-producing Klebsiella
pneumoniae in a neonatal unit: risk factors for infection
and colonisation. J Hosp Infect 2003;53:198e206.
19. Isaacs D. Unnatural selection: reducing antibiotic resistance
in neonatal units. Arch Dis Child Fetal Neonatal Ed 2006;91:
F72eF74.
20. Isaacs D. Neonatal sepsis: the antibiotic crisis. Indian Pe-
diatr 2005;42:1e5.
21. Sehgal R, Gaind R, Chellani H, Agarwal P. Extended-spec-
trum beta lactamase-producing gram-negative bacteria:
clinical prole and outcome in a neonatal intensive care
unit. Ann Trop Paediatr 2007;27:45e54.
336 A. Tagare et al.
Das könnte Ihnen auch gefallen
- List of Allergens: Skin Prick Test Allergens 01/29/2016Dokument3 SeitenList of Allergens: Skin Prick Test Allergens 01/29/2016romeoenny4154Noch keine Bewertungen
- DD Viral ExantemDokument4 SeitenDD Viral Exantemsiska_mariannaNoch keine Bewertungen
- 51 Allergens Patch Test SetDokument2 Seiten51 Allergens Patch Test Setromeoenny4154Noch keine Bewertungen
- Contoh ReviewDokument6 SeitenContoh Reviewromeoenny4154Noch keine Bewertungen
- PolyarthritisDokument6 SeitenPolyarthritisromeoenny4154Noch keine Bewertungen
- Clinical Reasoning Handout: URI Symptoms Sore Throat 1) Pearls BackgroundDokument5 SeitenClinical Reasoning Handout: URI Symptoms Sore Throat 1) Pearls Backgroundromeoenny4154Noch keine Bewertungen
- Ulceration Slides 090331Dokument62 SeitenUlceration Slides 090331mumutdwsNoch keine Bewertungen
- HemophiliaDokument2 SeitenHemophiliaromeoenny4154Noch keine Bewertungen
- Dizziness in PaedDokument7 SeitenDizziness in Paedromeoenny4154Noch keine Bewertungen
- Acute Fever in Children and InfantDokument26 SeitenAcute Fever in Children and Infantromeoenny4154Noch keine Bewertungen
- Pneumonia and Respiratory Tract Infections in ChildrenDokument37 SeitenPneumonia and Respiratory Tract Infections in ChildrenjayasiinputNoch keine Bewertungen
- Febrile Seizure GuidelineDokument1 SeiteFebrile Seizure GuidelinesmileyginaaNoch keine Bewertungen
- Afebrile SeizuresDokument11 SeitenAfebrile SeizuresMai Hunny100% (1)
- Children Perio DiseasesDokument9 SeitenChildren Perio Diseasesdr parveen bathlaNoch keine Bewertungen
- Congenital Heart Disease 2014Dokument1 SeiteCongenital Heart Disease 2014romeoenny4154Noch keine Bewertungen
- Acute Stridor Diagnostic Challenges in Different Age Groups Presented To The Emergency Department 2165 7548.1000125Dokument4 SeitenAcute Stridor Diagnostic Challenges in Different Age Groups Presented To The Emergency Department 2165 7548.1000125romeoenny4154Noch keine Bewertungen
- Clinical guideline for evaluation and treatment of febrile neonatesDokument1 SeiteClinical guideline for evaluation and treatment of febrile neonatesromeoenny4154Noch keine Bewertungen
- Calvin K.W. Tong Approach To A Child With A Cough: General PresentationDokument5 SeitenCalvin K.W. Tong Approach To A Child With A Cough: General Presentationromeoenny4154Noch keine Bewertungen
- Common Anemia in Pediatric BRM - PM - V1P4 - 03Dokument12 SeitenCommon Anemia in Pediatric BRM - PM - V1P4 - 03romeoenny4154Noch keine Bewertungen
- Bronchiolitis Clinical Guideline2014Dokument2 SeitenBronchiolitis Clinical Guideline2014romeoenny4154Noch keine Bewertungen
- Approach To Acute Arthritis in Kids: Allyson Mcdonough, MD Baylor Scott & White Health Department of RheumatologyDokument35 SeitenApproach To Acute Arthritis in Kids: Allyson Mcdonough, MD Baylor Scott & White Health Department of Rheumatologyromeoenny4154Noch keine Bewertungen
- Common Anemia in Pediatric BRM - PM - V1P4 - 03Dokument12 SeitenCommon Anemia in Pediatric BRM - PM - V1P4 - 03romeoenny4154Noch keine Bewertungen
- Common Anemia in Pediatric BRM - PM - V1P4 - 03Dokument12 SeitenCommon Anemia in Pediatric BRM - PM - V1P4 - 03romeoenny4154Noch keine Bewertungen
- Clinical Reasoning Handout: URI Symptoms Sore Throat 1) Pearls BackgroundDokument5 SeitenClinical Reasoning Handout: URI Symptoms Sore Throat 1) Pearls Backgroundromeoenny4154Noch keine Bewertungen
- Guidelines Clinical Management Chikungunya WHODokument26 SeitenGuidelines Clinical Management Chikungunya WHOFábio CantonNoch keine Bewertungen
- DD Viral ExantemDokument4 SeitenDD Viral Exantemsiska_mariannaNoch keine Bewertungen
- GinggivostomatitisDokument6 SeitenGinggivostomatitisromeoenny4154Noch keine Bewertungen
- Adhd Scoring ParentDokument3 SeitenAdhd Scoring Parentromeoenny4154Noch keine Bewertungen
- Croup GuidelineDokument17 SeitenCroup Guidelineromeoenny4154Noch keine Bewertungen
- Asthma ED Clinical Guideline2014Dokument5 SeitenAsthma ED Clinical Guideline2014romeoenny4154Noch keine Bewertungen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5782)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (72)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- GBS Guideline RCOGDokument26 SeitenGBS Guideline RCOGwoihonNoch keine Bewertungen
- SOP Neonatal SepsisDokument3 SeitenSOP Neonatal SepsisEidi IdhamNoch keine Bewertungen
- Wellcogen Bacterial Antigen KitDokument6 SeitenWellcogen Bacterial Antigen KitChandra Mohan Rajendran100% (1)
- Antibiotic-Guideline-for-Neonatal SepsisDokument13 SeitenAntibiotic-Guideline-for-Neonatal SepsisNada AhmedNoch keine Bewertungen
- Early Onset Strep DiseaseDokument26 SeitenEarly Onset Strep DiseaseKez FevNoch keine Bewertungen
- Group B Streptococcus: Women's & Children's ServicesDokument7 SeitenGroup B Streptococcus: Women's & Children's ServicesYwagar YwagarNoch keine Bewertungen
- Practice Bulletin ACOG Antibiotic Prophylaxis For LabourDokument12 SeitenPractice Bulletin ACOG Antibiotic Prophylaxis For LabourLorenzo TzuNoch keine Bewertungen
- Committee Opinion No 712 Intrapartum Management.57 PDFDokument7 SeitenCommittee Opinion No 712 Intrapartum Management.57 PDFernestosandNoch keine Bewertungen
- Antenatal management and statisticsDokument64 SeitenAntenatal management and statisticsHasan Dahamsheh100% (4)
- Benzy L PenicillinDokument4 SeitenBenzy L PenicillinwenmakerdNoch keine Bewertungen
- Urinary Tract Infections During PregnancyDokument8 SeitenUrinary Tract Infections During PregnancyGloria SaldivarNoch keine Bewertungen
- Sepsis Sepsis OverviewDokument12 SeitenSepsis Sepsis OverviewFernando LopezNoch keine Bewertungen
- Neonatal Sepsis Signs, Risk Factors, and TreatmentDokument18 SeitenNeonatal Sepsis Signs, Risk Factors, and TreatmentMoe KebabNoch keine Bewertungen
- Handbook of Pediatric Infectious Disease 3rdDokument330 SeitenHandbook of Pediatric Infectious Disease 3rdPedro Jose Ramos Cabrera100% (2)
- Signs & Symptoms of Strep B in InfantsDokument59 SeitenSigns & Symptoms of Strep B in InfantsAbdul Ghaffar AbdullahNoch keine Bewertungen
- Preterm Labour: Management GuidelinesDokument44 SeitenPreterm Labour: Management Guidelinesvacha sardarNoch keine Bewertungen
- Third TrimesterDokument13 SeitenThird Trimestersingh1582Noch keine Bewertungen
- Prenatal care essentialsDokument41 SeitenPrenatal care essentialsrinkal chavdaNoch keine Bewertungen
- Ingram FilingDokument29 SeitenIngram FilingRoy S. JohnsonNoch keine Bewertungen
- Bacterial Meningitis in Children - ClinicalKeyDokument24 SeitenBacterial Meningitis in Children - ClinicalKeyRubi Gonzalez SoberanoNoch keine Bewertungen
- Systemic Complications of Streptococci in Chronic Tonsillitis: Case SeriesDokument4 SeitenSystemic Complications of Streptococci in Chronic Tonsillitis: Case SeriesIJCRM Research JournalNoch keine Bewertungen
- Respiratory Disorder in NewbornDokument13 SeitenRespiratory Disorder in NewbornDini Fajriah OmariNoch keine Bewertungen
- Ajog MFMDokument29 SeitenAjog MFMCristhian Ore HurtadoNoch keine Bewertungen
- Penicillin Skin Testing - UpToDateDokument29 SeitenPenicillin Skin Testing - UpToDateJosué Pablo Chicaiza AbadNoch keine Bewertungen
- Bacteriuria Asintomática & Embarazo - Smaill 2007Dokument12 SeitenBacteriuria Asintomática & Embarazo - Smaill 2007Rolando LaraNoch keine Bewertungen
- Clinical Features, Evaluation, and Diagnosis of Sepsis in Term and Late Preterm Infants PDFDokument27 SeitenClinical Features, Evaluation, and Diagnosis of Sepsis in Term and Late Preterm Infants PDFJonathan WelchNoch keine Bewertungen
- Group B Streptococcal Infection in Neonates and Young Infants - UpToDateDokument30 SeitenGroup B Streptococcal Infection in Neonates and Young Infants - UpToDateKöllő ArnoldNoch keine Bewertungen
- Sexually Transmitted DiseasesDokument17 SeitenSexually Transmitted DiseasesChrystele Ann Ramilo100% (1)
- Clinical Guidelines in Neonatology 1st EditionDokument958 SeitenClinical Guidelines in Neonatology 1st EditionGaby Rivera0% (1)
- DynaMed Plus - Premature Rupture of Membranes at Term (Term PROM)Dokument16 SeitenDynaMed Plus - Premature Rupture of Membranes at Term (Term PROM)LudwinNoch keine Bewertungen