Beruflich Dokumente
Kultur Dokumente
1 s2.0 S0090825804003610 Main PDF
Hochgeladen von
Ririn WahyuniOriginalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
1 s2.0 S0090825804003610 Main PDF
Hochgeladen von
Ririn WahyuniCopyright:
Verfügbare Formate
Gynecologic Oncology 94 (2004) 575 577
www.elsevier.com/locate/ygyno
Case Report
Pregnancy after trachelectomy: a high-risk condition of preterm delivery.
Report of a case and review of the literature
Patrick Petignat, a,* Catalin Stan, a Eric Megevand, a and Daniel Dargent b
a
Gynecologic Oncology Service, University Hospitals of Geneva, Geneva, Switzerland
b
Department of Gynecologic Surgery, Hospital Edouard Herriot, Lyons, France
Received 4 August 2003
Available online 2 July 2004
Abstract
Background. Trachelectomy is a conservative but locally radical procedure associated with a high risk of preterm delivery.
Case. A 28-year-old patient with cervical cancer FIGO stage IB1 was treated with laparoscopic pelvic lymphadenectomy followed by
trachelectomy. Three years later, she conceived spontaneously. In consideration of the high risk of preterm delivery, the cervical status was
evaluated by transvaginal ultrasonography. At 16 weeks gestation, we observed the cerclage suture correctly placed at the level of the
internal cervical os and a neo-cervical segment length of 1.5 cm. Thereafter, serial ultrasound measurements showed preservation of the
cervical competence. The patient achieved an uneventful pregnancy and delivered by elective cesarean section at 37 weeks.
Conclusion. Transvaginal scans to evaluate the competence of the neo-cervix may contribute to the management and counseling of
patients after trachelectomy.
D 2004 Elsevier Inc. All rights reserved.
Keywords: Cervical cancer; Fertility; Laparoscopic lymphadenectomy; Pregnancy; Trachelectomy
Introduction
Case report
Women with early stage cervical cancers are usually
managed by radical hysterectomy and have to forego
their desire for future fertility. The issue of having
children after cervical cancer is important as the disease
affects primarily young women and many of them before
childbearing is completed. Vaginal trachelectomy is a
locally radical procedure which allows preservation of
the body of the uterus, but is associated with a high risk
of preterm delivery in pregnancy (Table 1) [1 10].
In a woman with a stage IB1 cervical cancer who
desired to preserve her childbearing potential, we performed laparoscopic pelvic lymph node dissection followed by a radical trachelectomy. Three years later, the
patient had a successful pregnancy and term delivery.
A 28-year-old woman, gravida 3, para 1, with no medical
or surgical history apart from one normal pregnancy and
delivery, presented to our colposcopic clinic for evaluation
of a high-grade squamous intraepithelial lesion identified on
her Papanicolaou smear. A cervical biopsy showed a cervical intraepithelial neoplasia (CIN) III, and the patient was
treated with large loop electrosurgical excision of the transformation zone. Histologic examination showed invasive,
well-differentiated squamous cell carcinoma measuring 9
mm laterally and infiltrated to a depth of 7 mm, without the
presence of lymph vascular space involvement.
The patient was assessed by magnetic resonance imaging of the pelvis and abdomen and examination under
anesthesia to determine the extension of the disease and
was staged FIGO IB1. She was informed of the standard
management in this situation, including radical hysterectomy. However, because the patient strongly desired to
preserve her fertility, she was counseled as to the possibility of radical trachelectomy and informed of the known
risks and complications of the procedure, including the
possibility of compromised fertility.
* Corresponding author. Department of Gynecology and Obstetrics,
University Hospitals of Geneva, Boulevard de la Cluse 30, 1211 Geneva,
14 Switzerland. Fax: +41-22-382-42-24.
E-mail address: patrick-petignat@hcuge.ch (P. Petignat).
0090-8258/$ - see front matter D 2004 Elsevier Inc. All rights reserved.
doi:10.1016/j.ygyno.2004.05.039
576
P. Petignat et al. / Gynecologic Oncology 94 (2004) 575577
Table 1
Pregnancy outcome and gestational age at delivery after radical trachelectomy
Authors (years)
Number
of patients
Number of
pregnancies
Gestational age
at delivery (weeks)
N (%) deliveries at
z36 weeks gestation
Roy et al. [1]
Martin et al. [2]
Covens et al. [3]
Dargent et al. [4]
Burnham et al. [5]
Shepherd et al. [6]
Alexopoulos et al. [7]
Rodriguez et al. [8]
Schlaerth et al. [9]
Burnett et al. [10]
Total
4
1
4
13
1
8
1
1
4
3
40
5
1
5
20
1
14
1
1
4
3
55
25; 34; 38; 39
27
2 miscarriages; 28; 2 at z36
10 miscarriages or fetal deaths; 10 at z36
37
4 miscarriages; 25; 26; 28; 31; 35; 35; 4 at z36
25
39
24; 26; 32; 38
20; 24; >36
38*
2
0
2
10
1
4
0
1
1
1
22
(50%)
(66%)*
(NA)*
(40%)*
(25%)
(33%)
(58%)*
Miscarriage (<20 weeks gestation); *miscarriages have been excluded; NA = not available.
Laparoscopic pelvic lymphadenectomy was performed
which revealed no lymph node metastases. We then proceeded with radical vaginal trachelectomy, as previously
described [4]. In addition, a single monofilament non-absorbable (1 nylon) suture was inserted into the lower segment
of the uterus to form a cerclage; the knot was hidden in the
isthmo-vaginal suture after a Sturmdorf closure. The vaginal
mucosa was approximated to the isthmic mucosa (squamocolumnar junction) to leave a permeable cervical canal. At the
end of the procedure, the cervical canal was measured and
showed a neo-cervix of 1.2 cm length below the isthmus.
The patient then resumed normal menses; follow-up by
colposcopy and Papanicolaou smear repeatedly tested negative. Three years later, she conceived spontaneously. Transvaginal ultrasound measurement of cervical length was
performed at 16, 20, 24, 28, and 34 weeks of gestation to
assess the stability and competence of the cervix (Fig. 1).
The cerclage placement was located at the internal os with a
cervical length of 1.5 cm throughout the pregnancy.
At 37 weeks gestation, a low transverse cesarean section
was performed under rachis anesthesia, and a live healthy
female child weighing 2700 g was delivered. The mother
and child were discharged 6 days post delivery.
Discussion
The most important issue for the patient and her physician following a treatment for cancer is the cure rate. The
available data in terms of survival after trachelectomy are
scant because the number of patients treated by this procedure remains small. However, it seems that the control of the
disease and survival are comparable to traditional surgical
procedures for early-stage cervical cancer [3,4,6,10].
The second important issue is the fertility and pregnancy
outcome. Even if the body of the uterus is preserved, this
therapeutic approach may alter the reproductive function
and expose those women to a high risk of preterm labor. To
the best of our knowledge, 10 reports regrouping 40 women
and 55 pregnancies have been published in the literature to
date (Medline search: 1966 to April 2003). Among those
women with a pregnancy of more than 20 weeks gestation,
42% delivered z36 weeks gestation (Table 1).
Preterm delivery may occur as a result of lack of
mechanical support of the residual cervix or ascending
infection followed by chorioamnionitis. Given the large
amount of cervix surgically removed, most authors recommend the insertion of a prophylactic cerclage to
provide sufficient mechanical support. A second potentially effective prevention strategy (not performed in our
case) is a total cervico-vaginal occlusion using the Saling
technique, which should be performed between 12 and 14
weeks of pregnancy in an effort to reduce the risk of
chorioamnionitis [4,11].
To date, no data exist in the literature on the cervical
status and competence during pregnancy following trachelectomy. However, it can be assumed that early detection of
preterm labor in these women might be difficult given the
Fig. 1. Endovaginal ultrasonography of cervix after radical trachelectomy (34 weeks gestation). Calipers mark the internal and external os. The distance
between the calipers was considered as the neocervical length (1.5 cm). The cerclage can be seen in cross-sections.
P. Petignat et al. / Gynecologic Oncology 94 (2004) 575577
risk of painless and progressive dilation of their residual
uterine cervix. Usual approaches used to detect preterm
delivery are regular digital cervical examinations, sterile
speculum examinations or ultrasonographic examination.
After trachelectomy, digital cervical and speculum examinations have a limited reliability due to the markedly
modified anatomy caused by the suture of the vaginal
mucosa to the neo-cervix, except in cases presenting with
advanced cervical dilatation or prolapsed of the membranes.
Transvaginal ultrasonographic follow-up may present a
significant advantage over digital or speculum examination
to evaluate the neo-cervix and the endocervical canal, and
to identify women truly at risk of preterm delivery. The
clinician performing the scan should be aware of the
anatomical modifications induced by the surgery, as the
narrowing of the upper part of the vagina due to its
approximation to the isthmic mucosa and should avoid an
excessive pressure on the vaginal probe which could potentially disturb the neo-cervix. In our case, we inserted the
probe slightly into the vagina until it met resistance, visualized the cerclage in the sagittal plane and manipulated the
probe until the entire cervical canal has been visualized.
Neither suture displacement nor significant cervical shortening was observed during the complete pregnancy.
What is the appropriate management if an ultrasonographic diagnosis of cervical incompetence is established?
First and foremost, antenatal interventions should be performed such as a transfer to a facility with a neonatal
intensive unit and the administration of corticosteroids to
the mother to hasten lung maturation. Other approaches
such as the Saling procedure or a second vaginal cerclage
performed in an emergency status would seem to us to be
considered as perilous.
We conclude that serial vaginal ultrasound assessment
of the neo-cervix in patients after trachelectomy allows
the determination of its competence and subsequently
contributes to the management and counseling of the
patient. The effective benefit of this procedure has not
yet been established by evidence-based scientific proof
because of the rarity of these cases, but this attitude may
577
be considered as a likely contributing factor to the efficient
clinical care of these patients.
Acknowledgment
We thank Mrs. Rosemary Sudan for editorial assistance.
References
[1] Roy M, Plante M. Pregnancies after radical vaginal trachelectomy for
early-stage cervical cancer. Am J Obstet Gynecol 1998;179:1494 6.
[2] Martin XJ, Golfier F, Romestaing P, Raudrant D. First case of pregnancy after radical trachelectomy and pelvic irradiation. Gynecol
Oncol 1999;74:286 7.
[3] Covens A, Shaw P, Murphy J, DePetrillo D, Lickrish G, Lafranboise
S, et al. Is radical trachelectomy a safe alternative to radical hysterectomy for patients with stage IA B carcinoma of the cervix? Cancer
1999;86:2273 9.
[4] Dargent D, Martin X, Sacchetoni A, Mathevet P. Laparoscopic vaginal radical trachelectomy. A treatment to preserve the fertility of
cervical carcinoma patients. Cancer 2000;88:1877 82.
[5] Burnham A, Venkitaraman U, Street P. Successful pregnancy following trachelectomy and laparoscopic pelvic lymphadenectomy for cervical cancer. Gynaecol Endosc 2000;9:73 4.
[6] Shepherd JH, Mould T, Oram DH. Radical trachelectomy in early
stage carcinoma of the cervix: outcome as judged by recurrence and
fertility rates. BJOG 2001;108:882 5.
[7] Alexopoulos E, Efkarpidis S, Fay TN, Williamson KM. Pregnancy
following radical trachelectomy and pelvic lymphadenectomy for
Stage I cervical adenocarcinoma. Acta Obstet Gynecol Scand 2002;
81:791 2.
[8] Rodriguez M, Guimares O, Rose PG. Radical abdominal trachelectomy and pelvic lymphadenectomy with uterine conservation and
subsequent pregnancy in the treatment of early invasive cervical
cancer. Am J Obstet Gynecol 2001;185:370 4.
[9] Schlaerth JB, Spirtos NM, Schlaerth AC. Radical trachelectomy and
pelvic lymphadenectomy with uterine preservation in the treatment of
cervical cancer. Am J Obstet Gynecol 2003;188:29 34.
[10] Burnett AF, Roman LD, OMeara AT, Morrow CP. Radical vaginal
trachelectomy and pelvic lymphadenectomy for preservation of fertility in early cervical carcinoma. Gynecol Oncol 2003;88:419 23.
[11] Saling E. Der fruhe totale Muttermundsverschluss zur Vermeidung
habitueller Aborte und Fruhgeburten. Z Geburtshilfe Perinatol 1981;
1852:259 61.
Das könnte Ihnen auch gefallen
- Life Style Wellness Coaching PDFDokument275 SeitenLife Style Wellness Coaching PDFSundar Prabhu71% (7)
- Work Life Balance WLB QuestionnaireDokument3 SeitenWork Life Balance WLB QuestionnairetarisaiNoch keine Bewertungen
- MRSADokument44 SeitenMRSAMarion PerniaNoch keine Bewertungen
- Reaching OutDokument353 SeitenReaching OutDebayan NandaNoch keine Bewertungen
- Beyond Cervical Length: Association Between Postcerclage Transvaginal Ultrasound Parameters and Preterm BirthDokument8 SeitenBeyond Cervical Length: Association Between Postcerclage Transvaginal Ultrasound Parameters and Preterm BirthMariana HernandezNoch keine Bewertungen
- A First Trimester Scan May Reveal The Presence of Placenta Accreta. Absence of The Anterior Uterine Wall During Caesarean Section: An Unexpected Placenta Accreta That Was Treated ConservativelyDokument3 SeitenA First Trimester Scan May Reveal The Presence of Placenta Accreta. Absence of The Anterior Uterine Wall During Caesarean Section: An Unexpected Placenta Accreta That Was Treated ConservativelyBOHR International Journal on GynaecologyNoch keine Bewertungen
- Placenta Increta Causing Um in The 26th Week of Pregnancy 2Dokument3 SeitenPlacenta Increta Causing Um in The 26th Week of Pregnancy 2Kester ApostolNoch keine Bewertungen
- 2014 179 0 Successful Treatment of Cervical Incompetence Using A Modified Laparoscopic Cervical Cerclage Technique A Cohort StudyDokument5 Seiten2014 179 0 Successful Treatment of Cervical Incompetence Using A Modified Laparoscopic Cervical Cerclage Technique A Cohort Studyalifiah nabillaNoch keine Bewertungen
- Surgical Treatment of Cesarean Scar Ectopic PregnancyDokument7 SeitenSurgical Treatment of Cesarean Scar Ectopic PregnancyIndRa KaBhuomNoch keine Bewertungen
- Girija BS, Sudha TR: AbstractDokument4 SeitenGirija BS, Sudha TR: AbstractALfuNoch keine Bewertungen
- Managment of Scar PregnancyDokument43 SeitenManagment of Scar Pregnancyvacha sardarNoch keine Bewertungen
- Laparoscopic Appendectomy During PregnancyDokument4 SeitenLaparoscopic Appendectomy During PregnancypsychobillNoch keine Bewertungen
- Complete Septate Uterus in PregnancyDokument6 SeitenComplete Septate Uterus in PregnancyfitriamarizkaNoch keine Bewertungen
- Normal Vaginal Delivery at Term After Expectant Management of Heterotopic Caesarean Scar Pregnancy: A Case ReportDokument3 SeitenNormal Vaginal Delivery at Term After Expectant Management of Heterotopic Caesarean Scar Pregnancy: A Case Reportdiaaabdallah209Noch keine Bewertungen
- Case Report Large Uterine Fibroids in Pregnancy With Successful Caesarean MyomectomyDokument4 SeitenCase Report Large Uterine Fibroids in Pregnancy With Successful Caesarean MyomectomyChidimma VictoryNoch keine Bewertungen
- Placenta Previa 1Dokument2 SeitenPlacenta Previa 1Gunther MirandaNoch keine Bewertungen
- PIIS0015028219304844Dokument2 SeitenPIIS0015028219304844nighshift serialsleeperNoch keine Bewertungen
- Antenatal Diagnosis of Uterine Incarceration: Surgical Role of MRI and Intraoperative Transmyometrium UltrasoundDokument6 SeitenAntenatal Diagnosis of Uterine Incarceration: Surgical Role of MRI and Intraoperative Transmyometrium UltrasoundAndy WahyudiNoch keine Bewertungen
- Successful Conservative Treatment of Microinvasive Cervical Cancer During PregnancyDokument3 SeitenSuccessful Conservative Treatment of Microinvasive Cervical Cancer During PregnancyEres TriasaNoch keine Bewertungen
- Case Report: Retained Intrauterine Device (IUD) : Triple Case Report and Review of The LiteratureDokument9 SeitenCase Report: Retained Intrauterine Device (IUD) : Triple Case Report and Review of The LiteratureYosie Yulanda PutraNoch keine Bewertungen
- Recurrent Cornual Ectopic Pregnancy - A Case Report: Article InfoDokument2 SeitenRecurrent Cornual Ectopic Pregnancy - A Case Report: Article InfoeditorijmrhsNoch keine Bewertungen
- 2011 9 PDFDokument6 Seiten2011 9 PDFRamesh Kumar SNoch keine Bewertungen
- Scar Ectopic Case ReportDokument6 SeitenScar Ectopic Case ReportMominah MayamNoch keine Bewertungen
- ContentServer - Asp 70Dokument12 SeitenContentServer - Asp 70kookiescreamNoch keine Bewertungen
- Uncomplicated Term Vaginal Delivery Following Magnetic Resonance-Guided Focused Ultrasound Surgery For Uterine FibroidsDokument4 SeitenUncomplicated Term Vaginal Delivery Following Magnetic Resonance-Guided Focused Ultrasound Surgery For Uterine FibroidsMangku Liong GuanNoch keine Bewertungen
- Prediction of Preterm Delivery in Twins by Cervical Assessment at 23 WeeksDokument4 SeitenPrediction of Preterm Delivery in Twins by Cervical Assessment at 23 WeeksBudi Darmawan DiswanNoch keine Bewertungen
- Placenta Percreta Dan Ligasi Arteri Internal IlliakaDokument4 SeitenPlacenta Percreta Dan Ligasi Arteri Internal IlliakaNyoman TapayanaNoch keine Bewertungen
- Anesthetic Management of An Undiagnosed Advanced Extrauterine Pregnancy Under Combined Spinal-Epidural AnesthesiaDokument4 SeitenAnesthetic Management of An Undiagnosed Advanced Extrauterine Pregnancy Under Combined Spinal-Epidural AnesthesiaHanayuki VizureiNoch keine Bewertungen
- Third Trimester Fetoscopic Laser Ablation of Type II Vasa PreviaDokument5 SeitenThird Trimester Fetoscopic Laser Ablation of Type II Vasa PreviaSol MancipeNoch keine Bewertungen
- Cervical IncompetenceDokument28 SeitenCervical IncompetenceHoney May Rollan Vicente100% (1)
- Management of AUB in A Bicornuate Uterus - Endometrial Ablation in A CompDokument1 SeiteManagement of AUB in A Bicornuate Uterus - Endometrial Ablation in A Comptipu42Noch keine Bewertungen
- Clinical Medicine Insights: Case ReportsDokument4 SeitenClinical Medicine Insights: Case ReportsJer KelNoch keine Bewertungen
- Journal of Medical Case ReportsDokument4 SeitenJournal of Medical Case ReportsAna Di JayaNoch keine Bewertungen
- 9.radha Et Al.Dokument3 Seiten9.radha Et Al.International Journal of Clinical and Biomedical Research (IJCBR)Noch keine Bewertungen
- Interesting Case FinalDokument33 SeitenInteresting Case Finalazenith dumlaoNoch keine Bewertungen
- Plprevia PDFDokument3 SeitenPlprevia PDFAtikah RahmadhaniNoch keine Bewertungen
- Anterior Cervical Wall Rupture As A Result of Induced AbortionDokument4 SeitenAnterior Cervical Wall Rupture As A Result of Induced AbortionnawriirwanNoch keine Bewertungen
- Case Reports in Women's HealthDokument4 SeitenCase Reports in Women's Healthowadokunquick3154Noch keine Bewertungen
- Cornual Ectopic PregnancyDokument1 SeiteCornual Ectopic PregnancyPavani NallaluthanNoch keine Bewertungen
- Primary Ovarian Abscess in Pregnancy: Case ReportDokument3 SeitenPrimary Ovarian Abscess in Pregnancy: Case ReportVinnyRevinaAdrianiNoch keine Bewertungen
- Uterine VaricesDokument3 SeitenUterine VaricesCindy AuliaNoch keine Bewertungen
- Gynecology and Minimally Invasive Therapy: Shahul Hameed Mohamed Siraj, Bernard Su Min ChernDokument3 SeitenGynecology and Minimally Invasive Therapy: Shahul Hameed Mohamed Siraj, Bernard Su Min ChernIrvin MarcelNoch keine Bewertungen
- Uterine Adherence To Anterior Abdominal Wall After Caesarean SectionDokument3 SeitenUterine Adherence To Anterior Abdominal Wall After Caesarean SectionGladstone AsadNoch keine Bewertungen
- Cervical Assessment at The Routine 23 W Scan UOG 2001Dokument3 SeitenCervical Assessment at The Routine 23 W Scan UOG 2001Arturo Eduardo Dowell DelgadoNoch keine Bewertungen
- A Case Report Abdominal Pregnancy MRI Vs USG RevisedDokument14 SeitenA Case Report Abdominal Pregnancy MRI Vs USG Revisedarnovareswari28Noch keine Bewertungen
- Cervical IncompetenceDokument30 SeitenCervical IncompetenceSignor ArasNoch keine Bewertungen
- Farman Bhai TreatmentDokument4 SeitenFarman Bhai TreatmentDr-Noor Muhammad KhanNoch keine Bewertungen
- Prolaps UteriDokument39 SeitenProlaps UteriVita DesriantiNoch keine Bewertungen
- Cervicval Shortening / Cervical Insufficiency: EtiologyDokument3 SeitenCervicval Shortening / Cervical Insufficiency: EtiologyMiska RaihanaNoch keine Bewertungen
- Ultrasound Study of Ovarian Cysts in Pregnancy Prevalence and SignificanceDokument4 SeitenUltrasound Study of Ovarian Cysts in Pregnancy Prevalence and SignificanceDavid Eka PrasetyaNoch keine Bewertungen
- Ectopic Pregnancy: by Amielia Mazwa Rafidah Obstetric and Gynecology DepartmentDokument43 SeitenEctopic Pregnancy: by Amielia Mazwa Rafidah Obstetric and Gynecology DepartmentAlrick AsentistaNoch keine Bewertungen
- 1 s2.0 S1028455911001823 MainDokument6 Seiten1 s2.0 S1028455911001823 MainFatimah AssagafNoch keine Bewertungen
- tmp7DB6 TMPDokument78 Seitentmp7DB6 TMPFrontiersNoch keine Bewertungen
- Rupture of The Cervix During Pregnancy After Cervical Pessary Insertion For Preventing Preterm BirthDokument4 SeitenRupture of The Cervix During Pregnancy After Cervical Pessary Insertion For Preventing Preterm BirthNuril AzizahNoch keine Bewertungen
- Abrasio PlacentaDokument3 SeitenAbrasio Placentamuhammad azamNoch keine Bewertungen
- Effectiveness of Using of Single Dose of Methotrexate in Management of Cervical Ectopic PregnancyDokument3 SeitenEffectiveness of Using of Single Dose of Methotrexate in Management of Cervical Ectopic PregnancyasclepiuspdfsNoch keine Bewertungen
- Laparoscopic Management of Rudimentary Uterine Horn Pregnancy: Case Report and Literature ReviewDokument4 SeitenLaparoscopic Management of Rudimentary Uterine Horn Pregnancy: Case Report and Literature ReviewCamacho OmarNoch keine Bewertungen
- Case Report: AIM MethodDokument3 SeitenCase Report: AIM Methoddrskjain2005Noch keine Bewertungen
- Khing Journal...Dokument5 SeitenKhing Journal...Khing AbatNoch keine Bewertungen
- Case Report: Ruptured Ectopic Pregnancy in Caesarean Section Scar: A Case ReportDokument3 SeitenCase Report: Ruptured Ectopic Pregnancy in Caesarean Section Scar: A Case ReportEga MegawatiNoch keine Bewertungen
- Heterotopic Pregnancy Cervical and TubalDokument9 SeitenHeterotopic Pregnancy Cervical and Tubalvictorubong404Noch keine Bewertungen
- Ovarian Ectopic Pregnancy: A Rare Case: Iran J Reprod Med Vol. 12. No. 4. PP: 281-284, April 2014Dokument4 SeitenOvarian Ectopic Pregnancy: A Rare Case: Iran J Reprod Med Vol. 12. No. 4. PP: 281-284, April 2014alif bagusNoch keine Bewertungen
- MC Seminar - CFA Standard: Coonsboro Calvin CoonidgeDokument14 SeitenMC Seminar - CFA Standard: Coonsboro Calvin CoonidgeRirin Wahyuni100% (1)
- Peripartum CardiomyopathyDokument1 SeitePeripartum CardiomyopathyRirin WahyuniNoch keine Bewertungen
- Hemodynamic Effects of Spinal Anesthesia For Cesarean Section Are Equivalent in Severely Preeclamptic and Healthy ParturientsDokument21 SeitenHemodynamic Effects of Spinal Anesthesia For Cesarean Section Are Equivalent in Severely Preeclamptic and Healthy ParturientsRirin WahyuniNoch keine Bewertungen
- Total Pelvic ExenterationDokument13 SeitenTotal Pelvic ExenterationRirin Wahyuni100% (1)
- Luka Bakar: Nama: Melvin Andrean NIM: 112018161 Pembimbing: Kpt. Dr. Anwar Lewa, SP - BP-RE, M.BiomedDokument47 SeitenLuka Bakar: Nama: Melvin Andrean NIM: 112018161 Pembimbing: Kpt. Dr. Anwar Lewa, SP - BP-RE, M.BiomedIpd CengkarengNoch keine Bewertungen
- HorlicksDokument5 SeitenHorlicksAdalberto MacdonaldNoch keine Bewertungen
- Missed Myocardial InfarctionDokument2 SeitenMissed Myocardial InfarctionHARITH RAJAH100% (1)
- You Exec - Coronavirus Management Kit FreeDokument25 SeitenYou Exec - Coronavirus Management Kit FreeNidaNoch keine Bewertungen
- UntitledDokument22 SeitenUntitledBenjamin Swami100% (7)
- Assignment No 1 bt502 SeminarDokument15 SeitenAssignment No 1 bt502 SeminarMashal WakeelaNoch keine Bewertungen
- Device Related Error in Patient Controlled.17Dokument6 SeitenDevice Related Error in Patient Controlled.17Ali ÖzdemirNoch keine Bewertungen
- Puskesmas Wanggudu Raya: Dinas Kesehatan Kabupaten Konawe UtaraDokument6 SeitenPuskesmas Wanggudu Raya: Dinas Kesehatan Kabupaten Konawe UtaraicaNoch keine Bewertungen
- Cupuncture: Victor S. SierpinaDokument6 SeitenCupuncture: Victor S. SierpinaSgantzos MarkosNoch keine Bewertungen
- Background Info: ThesisDokument3 SeitenBackground Info: ThesisCITLALI RAMIREZ MEDINANoch keine Bewertungen
- SS20120100010 42491076 PDFDokument6 SeitenSS20120100010 42491076 PDFRishiraj JaiswalNoch keine Bewertungen
- A Prospective Study On The Practice of Conversion of Antibiotics From IV To Oral Route and The Barriers Affecting ItDokument3 SeitenA Prospective Study On The Practice of Conversion of Antibiotics From IV To Oral Route and The Barriers Affecting ItInternational Journal of Innovative Science and Research TechnologyNoch keine Bewertungen
- Primitive ReflexesDokument10 SeitenPrimitive Reflexesbun_yulianaNoch keine Bewertungen
- Revision: Assumption: I. Find The Assumptions in The Following CasesDokument4 SeitenRevision: Assumption: I. Find The Assumptions in The Following CasesHiển NguyễnNoch keine Bewertungen
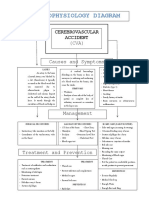
- Pathophysiology DiagramDokument1 SeitePathophysiology Diagramzebzeb STEMANoch keine Bewertungen
- BibliographyDokument2 SeitenBibliographyelvie21Noch keine Bewertungen
- Crown & Bridge RemovalDokument1 SeiteCrown & Bridge RemovalCamilaNoch keine Bewertungen
- 1 TTP Mozambique - STE EIS Vol - I - Submitted - For - Disclosure - 0Dokument227 Seiten1 TTP Mozambique - STE EIS Vol - I - Submitted - For - Disclosure - 0Luciana MirandaNoch keine Bewertungen
- The Customer Is Always Right Right? Is That Not What Companies Always Claim?Dokument6 SeitenThe Customer Is Always Right Right? Is That Not What Companies Always Claim?faith mutsambiriNoch keine Bewertungen
- Disturbed Sleep Pattern Related To Environmental FactorsDokument9 SeitenDisturbed Sleep Pattern Related To Environmental Factorsalaisah dimaporoNoch keine Bewertungen
- Iep Forms EngDokument23 SeitenIep Forms EngElsa PimentelNoch keine Bewertungen
- CL489F Physiotherapy Reassessment ReportDokument4 SeitenCL489F Physiotherapy Reassessment ReportnaeemullahNoch keine Bewertungen
- Liposuction: Immediately After SurgeryDokument1 SeiteLiposuction: Immediately After SurgeryScott J. Zevon, MD, FACSNoch keine Bewertungen
- Suchita Srivastava & Anr Vs Chandigarh Administration On 28 August 2009Dokument11 SeitenSuchita Srivastava & Anr Vs Chandigarh Administration On 28 August 2009Disability Rights AllianceNoch keine Bewertungen
- CSHP TEMPLATE (1) - NewDokument14 SeitenCSHP TEMPLATE (1) - NewLucky JavellanaNoch keine Bewertungen
- Guidance For Industry: Clinical Pharmacology Data To Support A Demonstration of Biosimilarity To A Reference ProductDokument18 SeitenGuidance For Industry: Clinical Pharmacology Data To Support A Demonstration of Biosimilarity To A Reference ProductBrian WilliamsNoch keine Bewertungen