Beruflich Dokumente
Kultur Dokumente
Iseases and Is An Important Cause of Mortality and Morbidity Worldwide
Hochgeladen von
Annette CraigOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Iseases and Is An Important Cause of Mortality and Morbidity Worldwide
Hochgeladen von
Annette CraigCopyright:
Verfügbare Formate
iseases and is an important cause of mortality and morbidity worldwide.
Essential update: Survival benefits of azithromycin outweigh MI risk in
elderly patients with pneumonia
Although recent research suggests that azithromycin may be associated with increased
cardiovascular events, Mortensen and colleagues found that in elderly patients hospitalized
with community-acquired pneumonia, early survival benefits with azithromycin greatly
exceeded the risk of nonfatal MI. Their retrospective cohort study included 73,690 veterans
most of them men and all of them 65 years of age or olderwho received guidelinerecommended combination antibiotic therapy.[1, 2]
In the study, 90-day mortality was significantly lower in patients whose treatment included
azithromycin than in those whose treatment did not include azithromycin (17.4% vs 22.3%).
within the first 90 days of hospitalization, treatment with azithromycin averted seven deaths
for every nonfatal MI. Patients treated with azithromycin had a small but significant
increased risk of MI compared with those who received other treatments (5.1% vs 4.4%), but
did not have a significantly increased risk of experiencing any cardiac event, cardiac
arrhythmias, or heart failure.[1, 2]
Presentation and pathogens in typical CAP
Typical bacterial CAP pathogens include Streptococcus pneumoniae, Haemophilus
influenzae, and Moraxella catarrhalis; these 3 pathogens account for approximately 85% of
CAP cases. Patients with bacterial CAP typically present with fever, usually with a
productive cough and often with pleuritic chest pain. Other pulmonary findings on physical
examination are as follows:
Purulent sputum is characteristic
Rales are heard over the involved lobe or segment
Increased tactile fremitus, bronchial breathing, and E-to-A change may be present if
consolidation has occurred
Decreased tactile fremitus and dullness on chest percussion may result from pleural
effusion (usually due to H influenzae infection) or empyema
Particular patient settings and the specific CAP pathogens that are most often associated with
them include the following:
Most common overall: S pneumoniae
Exacerbation of chronic bronchitis leading to CAP that requires hospitalization: M
catarrhalis
Influenza[3] : Staphylococcus aureus
Atypical CAPs
The clinical presentation of atypical CAP is often subacute. In addition, patients with CAP
due to atypical CAP pathogens present with a variety of pulmonary and extrapulmonary
findings (eg, CAP plus diarrhea). Atypical CAP includes the following:
Psittacosis
Q fever
Tularemia
Mycoplasma pneumonia
Legionnaires disease
Chlamydophila (Chlamydia) pneumonia
Extrapulmonary signs and symptoms seen in some forms of atypical CAP may include the
following:
Mental confusion
Prominent headache
Myalgias
Ear pain
Abdominal pain
Diarrhea
Rash (Horder spots in psittacosis; erythema multiforme in Mycoplasma pneumonia)
Nonexudative pharyngitis
Hemoptysis
Splenomegaly
Relative bradycardia
Pleural effusion in a patient with CAP and extrapulmonary manifestations should suggest
Legionella infection. Pleural effusion with appropriate epidemiologic history findings, such
as contact with a rabbit or deer, may suggest tularemia.
Workup
Laboratory studies for CAP are as follows:
Chest radiography
Sputum Gram stain and/or culture (do not send the sputum of patients with COPD for
Gram stain or culture, because these specimens invariably demonstrate a mixed or
normal flora)
Blood cultures
Other laboratory tests
If atypical CAP is suspected, because of extrapulmonary findings, the workup may include
the following:
Serum transaminase levels
Serum phosphorus levels
Urinalysis
Ferritin levels
Creatine phosphokinase (CPK) levels
C-reactive protein (CRP) levels
Procalcitonin levels
Cold agglutinin titers
Otherwise unexplained early, transient, and slight increases in serum transaminases in a
patient with CAP suggest the presence of psittacosis, Q fever, or Legionella pneumonia.[4]
Otherwise unexplained hypophosphatemia or microscopic hematuria in a patient with CAP
suggests Legionnaires disease.[5]
Chest radiography
Obtain chest radiographs in all patients with suspected CAP to exclude conditions that mimic
CAP and to confirm the presence of an infiltrate compatible with the presentation of CAP.[6, 7]
Patients presenting very early with CAP may have negative findings on chest radiography. In
these patients, repeat chest radiography within 24 hours. Serial chest radiography can be used
to observe the progression of CAP.
Hospital admission
Although patients with mild CAP may be treated in an ambulatory setting, patients with CAP
who are moderately to severely ill should be hospitalized.[8] Patients with severe CAP who
require invasive ventilation require admission to an intensive care unit (ICU).[9, 10, 11, 12, 13, 14]
Antibiotic Therapy
CAP may be treated with monotherapy or combination therapy. Effective monotherapy
antibiotics include the following[15, 16, 17, 18] :
Doxycycline
Respiratory quinolones
Combination therapy usually consists of ceftriaxone plus doxycycline or azithromycin.
Immunocompromised hosts who present with CAP are treated in the same manner as
otherwise healthy hosts but may require a longer duration of therapy.
Inpatient therapy for CAP is usually with IV antibiotics, followed by an oral course of
therapy for a total of 14 days.[19, 20, 21, 22] Patients who are severely ill or who are unable to
tolerate or absorb oral medications require a longer duration of IV therapy before switching
to an oral antibiotic.[23]
Mild to moderately ill patients with CAP may be treated entirely via the oral route, either on
an inpatient or outpatient basis.
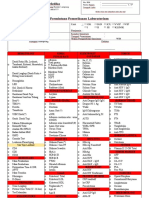
Image library
Gram stain showing Streptococcus pneumoniae.
Das könnte Ihnen auch gefallen
- This Site Is Intended For Healthcare ProfessionalsDokument17 SeitenThis Site Is Intended For Healthcare ProfessionalsAnnette CraigNoch keine Bewertungen
- This Site Is Intended For Healthcare ProfessionalsDokument17 SeitenThis Site Is Intended For Healthcare ProfessionalsAnnette CraigNoch keine Bewertungen
- PhysicalDokument1 SeitePhysicalAnnette CraigNoch keine Bewertungen
- Effect of MRB Solution Immersion on Steel HardnessDokument3 SeitenEffect of MRB Solution Immersion on Steel HardnessAnnette CraigNoch keine Bewertungen
- PtuDokument3 SeitenPtuAnnette CraigNoch keine Bewertungen
- What Is BrachialgiaDokument1 SeiteWhat Is BrachialgiaAnnette CraigNoch keine Bewertungen
- Family Circle: Pak Darli S RizkyDokument1 SeiteFamily Circle: Pak Darli S RizkyAnnette CraigNoch keine Bewertungen
- The SymptomsDokument1 SeiteThe SymptomsAnnette CraigNoch keine Bewertungen
- Effect of MRB Solution Immersion on Steel HardnessDokument3 SeitenEffect of MRB Solution Immersion on Steel HardnessAnnette CraigNoch keine Bewertungen
- Journal ReadingDokument1 SeiteJournal ReadingAnnette CraigNoch keine Bewertungen
- PtuDokument3 SeitenPtuAnnette CraigNoch keine Bewertungen
- SummaryDokument2 SeitenSummaryAnnette CraigNoch keine Bewertungen
- GambarDokument1 SeiteGambarAnnette CraigNoch keine Bewertungen
- Practice Essentials: Essential Update: Telavancin Approved For Bacterial PneumoniaDokument12 SeitenPractice Essentials: Essential Update: Telavancin Approved For Bacterial PneumoniaAnnette CraigNoch keine Bewertungen
- Heart Failure Develops When The HeartDokument17 SeitenHeart Failure Develops When The HeartAnnette CraigNoch keine Bewertungen
- Liver So RosDokument5 SeitenLiver So RosAnnette CraigNoch keine Bewertungen
- Early Syphilis: Serological Treatment Response To Doxycycline/tetracycline Versus Benzathine PenicillinDokument5 SeitenEarly Syphilis: Serological Treatment Response To Doxycycline/tetracycline Versus Benzathine PenicillinAnnette CraigNoch keine Bewertungen
- SummaryDokument2 SeitenSummaryAnnette CraigNoch keine Bewertungen
- Eficacy, Safety and Toxicity of The Traditional Medicines: By: Prof. Dr. ARMENIA, MS. AptDokument37 SeitenEficacy, Safety and Toxicity of The Traditional Medicines: By: Prof. Dr. ARMENIA, MS. AptAnnette CraigNoch keine Bewertungen
- Determination of Lipid Oxidation Products in Vegetable Oils and Marine OmegaDokument14 SeitenDetermination of Lipid Oxidation Products in Vegetable Oils and Marine OmegaAnnette CraigNoch keine Bewertungen
- Early Syphilis: Serological Treatment Response To Doxycycline/tetracycline Versus Benzathine PenicillinDokument4 SeitenEarly Syphilis: Serological Treatment Response To Doxycycline/tetracycline Versus Benzathine PenicillinAnnette CraigNoch keine Bewertungen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5784)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Soi 2016-17Dokument280 SeitenSoi 2016-17venkat_nsnNoch keine Bewertungen
- Nurse Np1 Board CramsheetDokument8 SeitenNurse Np1 Board CramsheetZero TwoNoch keine Bewertungen
- Vaccination in PregnancyDokument7 SeitenVaccination in PregnancyNoraNoch keine Bewertungen
- Referat: Department Dermato - Venereologist Faculty of Medicine Universitas Al-Khairaat Palu 2017Dokument27 SeitenReferat: Department Dermato - Venereologist Faculty of Medicine Universitas Al-Khairaat Palu 2017Elvis HusainNoch keine Bewertungen
- AAHA Canine Vaccination GuidelinesDokument23 SeitenAAHA Canine Vaccination GuidelinesRaniah DahlanNoch keine Bewertungen
- Rife's Original Basic FrequenciesDokument38 SeitenRife's Original Basic FrequenciesVeljko Nikolic100% (1)
- IT 3 - GAS Infection - ZKA - BLOK 27 - 2017Dokument20 SeitenIT 3 - GAS Infection - ZKA - BLOK 27 - 2017Archita WicesaNoch keine Bewertungen
- Immunization EPI Huda 201212Dokument5 SeitenImmunization EPI Huda 201212Aerish TupazNoch keine Bewertungen
- ManevreDokument447 SeitenManevreIoana MorariuNoch keine Bewertungen
- Kuliah Biokimia-Imunokimia FK UNDIPDokument19 SeitenKuliah Biokimia-Imunokimia FK UNDIPPutri HapsariNoch keine Bewertungen
- Hairy Leukoplakia As An Early OralDokument4 SeitenHairy Leukoplakia As An Early OralJessicaLisaNugrohoNoch keine Bewertungen
- PathophysiologyDokument2 SeitenPathophysiologySarahlaine BrazasNoch keine Bewertungen
- Clsi Ila02 ADokument36 SeitenClsi Ila02 ACristian Gutiérrez VeraNoch keine Bewertungen
- Pro-Inflammatory Effects of Hypoglycemia in Humans With or Without DiabetesDokument32 SeitenPro-Inflammatory Effects of Hypoglycemia in Humans With or Without Diabetestitin setya ningsihNoch keine Bewertungen
- Hav Igm CTKDokument2 SeitenHav Igm CTKGu AleXanderNoch keine Bewertungen
- MHC Antigens: Rakesh Sharda Department of Veterinary Microbiology NDVSU College of Veterinary Science & A.H., MhowDokument18 SeitenMHC Antigens: Rakesh Sharda Department of Veterinary Microbiology NDVSU College of Veterinary Science & A.H., MhowMuskanpreet kaurNoch keine Bewertungen
- 14 HF-Limfoma GI TractDokument27 Seiten14 HF-Limfoma GI TractNur akilaNoch keine Bewertungen
- Form Lab RSBM NewDokument2 SeitenForm Lab RSBM NewKiki OlivianaNoch keine Bewertungen
- Respiratory Diseases in Children GuideDokument86 SeitenRespiratory Diseases in Children Guidemurugesh1969100% (1)
- ELISADokument32 SeitenELISAAAnneMichelleP.CruzNoch keine Bewertungen
- MMI4804 Quiz 5Dokument16 SeitenMMI4804 Quiz 5Ham Mad0% (1)
- Red Eyes Guide: Causes and TreatmentsDokument45 SeitenRed Eyes Guide: Causes and TreatmentsDavidVictoriousLukas100% (1)
- Bacte03 NEISSERIA AND MORAXELLADokument11 SeitenBacte03 NEISSERIA AND MORAXELLAAngelic AngelesNoch keine Bewertungen
- NCP Burn Risk InfectionDokument1 SeiteNCP Burn Risk InfectionBraingie Racho50% (4)
- Viral Diseases MechanismsDokument105 SeitenViral Diseases MechanismspolypeptideNoch keine Bewertungen
- MICROPARA LEC Chapter 14 ReviewerDokument11 SeitenMICROPARA LEC Chapter 14 ReviewerRen “Shel” ManaloNoch keine Bewertungen
- Top Diagnosis from Count of DiagnosisDokument356 SeitenTop Diagnosis from Count of DiagnosisdartosNoch keine Bewertungen
- Employee Health and Personal Hygiene HandbookDokument45 SeitenEmployee Health and Personal Hygiene HandbookAsma OmarNoch keine Bewertungen
- BC Lioton SKDokument71 SeitenBC Lioton SKAlejandra Cale Radowitz0% (1)
- CEFSK1 Aspergillus (Eng, Ital, Span, Ger, Fre) KD 12-13Dokument3 SeitenCEFSK1 Aspergillus (Eng, Ital, Span, Ger, Fre) KD 12-13fcincilaNoch keine Bewertungen