Beruflich Dokumente
Kultur Dokumente
Wellens SDR
Hochgeladen von
tufis02Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Wellens SDR
Hochgeladen von
tufis02Copyright:
Verfügbare Formate
Diagnostics
Electrocardiographic Manifestations of
Wellens Syndrome
JOSEPH RHINEHARDT,* WILLIAM J. BRADY, MD,* ANDREW D. PERRON, MD,*
AND AMAL MATTU, MD
Wellens syndrome is a pattern of electrocardiographic T-wave changes
associated with critical, proximal left anterior descending (LAD) artery
stenosis. The syndrome is also referred to as LAD coronary T-wave
syndrome. Syndrome criteria include T-wave changes plus a history of
anginal chest pain without serum marker abnormalities; patients lack Q
waves and signicant ST-segment elevation; such patients show normal
precordial R-wave progression. The natural history of Wellens syndrome is anterior wall acute myocardial infarction. The T-wave abnormalities are persistent and may remain in place for hours to weeks; the
clinician likely will encounter these changes in the sensation-free patient. With denitive management of the stenosis, the changes resolve
with normalization of the electrocardiogram. It is vital that the physician
recognize these changes and the association with critical LAD obstruction and signicant risk for anterior wall myocardial infarction. (Am J
Emerg Med 2002;20:638-643. Copyright 2002, Elsevier Science (USA). All
rights reserved.)
When evaluating patients in the emergency department
(ED), emergency physicians (EP) must be capable and
procient in the interpretation of the electrocardiogram
(ECG). Among the many electrocardiographic ndings indicative of acute coronary syndromes, the EP must be
familiar with the characteristics of the preinfarction stage of
coronary artery disease known as Wellens syndrome.
Wellens syndrome consists of T-wave abnormalities in the
anterior chest leads. These changes are associated with
signicant obstruction in the proximal left anterior descending (LAD) coronary artery. Patients with Wellens syndrome are at high risk for the development of an extensive
myocardial infarction of the anterior wall and death.1 Although medical management may provide symptomatic improvement at rst, the natural history of this syndrome is
anterior wall myocardial infarction that, if not aborted,
results in signicant left ventricular dysfunction and/or
From the *Department of Emergency Medicine, University of Virginia, Charlottesville, VA; and the Department of Emergency Medicine, University of Maryland, Baltimore, MD.
Manuscript received and accepted December 10, 2001.
Reprints are not available.
Address correspondence to William Brady, MD, Department of
Emergency Medicine, Box 523-21, University of Virginia Medical
Center, Charlottesville, VA 22908. E-mail: wb4z@virginia.edu
Key Words: Electrocardiogram, T-wave inversion, T wave,
Wellens Syndrome.
Copyright 2002, Elsevier Science (USA). All rights reserved.
0735-6757/02/2007-0014$35.00/0
doi:10.1053/ajem.2002.34800
638
death. Once Wellens syndrome has been recognized, urgent coronary angiographynot stress imagining of any
sortis required to evaluate the need for early angioplasty
or coronary bypass surgery.2 This article discusses the electrocardiographic ndings suggestive of this potentially fatal
condition.
CASE PRESENTATIONS
Case 1
A 49-year-old man presented to the ED with chest pain of
4 hours duration that was associated with diaphoresis.
Emergency medical technicians treated the patient with
nitrates, morphine, and aspirin; he was sensation-free on
arrival to the ED. The examination was unremarkable. The
12-lead ECG (Fig 1), performed when the patient was free
of discomfort, showed deeply inverted T waves in leads V2
to V6; the ST segments were minimally elevated and convex in morphology in leads V2 to V4. The electrocardiographic pattern in a pain-free patient raised the possibility of
LAD coronary T-wave syndrome. Serum markers were
negative for myocardial infarction. The patient was admitted to a cardiology service for cardiac catheterization, which
revealed a 95% proximal LAD artery occlusion. Angioplasty with stent placement was performed successfully.
Case 2
A 54-year-old woman presented to the ED with chest
pain associated with diaphoresis and nausea. The examination was remarkable for diaphoresis. Before performing the
ECG the patients pain resolved. The ECG (Fig 2) showed
biphasic T-wave inversions in leads V2 to V4; the T waves
were biphasic in leads V2 and V3. She remained pain free
in the ED; the initial serum marker was normal. She was
admitted to the coronary care unit where the pain recurred
approximately 6 hours later, associated with the development of obvious ST-segment elevation in leads V2 to V4
consistent with acute myocardial infarction (AMI). She
received a thrombolytic agent with reperfusion conrmed
by resolution of the pain and the ST-segment elevation.
Cardiac catheterization revealed a near-complete proximal
LAD lesion that was successfully opened and stented.
Case 3
A 54-year-old man presented via ambulance to the ED
with chest pain. Examination revealed diaphoresis. He was
RHINEHARDT ET AL MANIFESTATIONS OF WELLENS SYNDROME
639
FIGURE 1. Case 1, normal
sinus rhythm with inverted T
waves in leads V2 to V6. The
T waves are deeply inverted.
Note the abrupt angle of the
descending limb of the T
wave, accounting for its
marked negative amplitude
(ie, deeply inverted). Also
note the minimal ST-segment
elevation in leads V2 to V4
with a convex contour.
given nitrates and morphine with resolution of his pain. At this
point, an ECG (Fig 3) showed normal sinus rhythm with
biphasic T-wave inversions in the anterior distribution (leads
V1-V4). The initial serum marker was negative for myocardial
infarction. The patients primary care physician examined the
patient in the ED; a stress test was performed. Approximately
1 minute into the test, the patient developed severe pain in the
midchest accompanied by diaphoresis and dizziness. The ECG
revealed ST-segment elevation in the anterior leads consistent
with anterior wall AMI (Fig 4). He was taken to the catheterization laboratory where a proximal LAD lesion was found and
successfully opened via angioplasty.
DISCUSSION
de Zwann et al1 rst described a subgroup of patients
hospitalized for unstable angina that were at high risk for
FIGURE 2. Case 2, normal
sinus rhythm with biphasic Twave inversions in leads V2
and V3 as well as T-wave inversion in lead V4. The ST
segment is also elevated in
leads V2 and V3 with a concave morphology.
640
AMERICAN JOURNAL OF EMERGENCY MEDICINE Volume 20, Number 7 November 2002
FIGURE 3. Case 3, normal
sinus rhythm with biphasic Twave inversions in leads V1
to V4 and concave ST-segment elevation.
the development of an anterior wall myocardial infarction.
This subgroup could be recognized by characteristic STsegmentT-wave changes in the precordial leads. These
changes involve the T wave with occasional involvement of
the ST segment. Two basic patterns of electrocardiographic
change are encountered: (1) isoelectric or minimally elevated (ie, less than 1 mm) ST segment with a straight or
convex morphology that leads into a negative (inverted) T
wave at an angle of 60 to 90 (Figs 1 and 5);2 (2) biphasic
T waves in the right to midprecordial leads (Figs 2, 3,
and 5).3
In Wellens rst study, 26 of 145 patients admitted for
unstable angina (18%) had this electrocardiographic pattern.1 In a second prospective study, 180 of 1,260 hospitalized patients (14%) showed the characteristic electrocardiographic changes.2 Furthermore, all of these patients had
signicant disease of the proximal LAD. In the rst study,
12 of 16 patients (75%) with electrocardiographic changes
who did not receive coronary revascularization developed
an extensive anterior wall infarction within a few weeks
after admission.1 In the second study, urgent coronary angiography was implemented, and all of the 180 patients with
FIGURE 4. Case 3, acute
ST-segment elevation myocardial infarction of the anterior wall.
electrocardiographic changes were found to have blockage
of the LAD, varying from 50% to complete obstruction.2
Early detection of these electrocardiographic changes is
also important because of the clinical presentation of a
patient with Wellens syndrome. The characteristic electrocardiographic pattern often develops when the patient is not
experiencing angina. In fact, during an attack of chest pain,
the ST-segmentT-wave abnormalities usually normalize or
develop into ST-segment elevation.2 Cardiac serum markers
are often normal or minimally elevated. In Wellens prospective study, only 21 of 180 patients (12%) with electrocardiographic changes had elevated cardiac enzymes. These
elevations were always less than twice the upper limit of
normal.2 Therefore, the ECG may be the only indication of
an impending extensive anterior wall myocardial infarction
in an otherwise asymptomatic patientas seen in Case 3
(Figs 3 and 4).
The electrocardiographic ndings include signicant involvement of the T wave with occasional alterations of the
ST segment. The ST segment itself is often normal (ie,
isoelectric); if abnormal, it is minimally elevated, usually
less than 1 mm with a high take-off of the ST segment from
the QRS complex. If the ST segment is elevated, it is either
RHINEHARDT ET AL MANIFESTATIONS OF WELLENS SYNDROME
FIGURE 5. The T-wave inversions of Wellens syndrome, the
more common pattern of (A-C) deeply inverted T wave and the
(D-F) less common biphasic T wave. (B-F) ST-segment elevation
is present.
convex in contour (Figs 1 and 5) or obliquely straight in
appearance (Figs 1 and 3); concave morphologies are also
seen (Figs 2, 3, and 5).1 T-wave ndings, the key features of
this electrocardiographic syndrome, may take the form of 1
of 2 patterns of T-wave changes. In the more common
pattern, which comprises approximately 75% of cases, the T
wave is deeply inverted (Figs 1 and 5A-5C). As the ST
segment terminates, the T wave assumes a very negative
angle relative to the isoelectric baseline; this angle may
approach 90. The inverted T wave is symmetric in contour.
The less common variant, comprising 25% of Wellens
syndrome cases, presents with biphasic T waves (Figs 2, 3,
and 5D-5E).1,2
The ST-segment and T-wave changes are present in leads
V2 and V3; in certain cases, the changes may also involve
leads V1 and V4. In Wellens prospective study, approxi-
641
mately two thirds of patients also had these changes in lead
V1 and three quarters in lead V4. Patients with abnormalities in lead V4 occasionally will show similar abnormalities
in leads V5 or V6.2 The electrocardiographic pattern often
develops when the patient is not experiencing angina, and
the ST-segmentT-wave abnormalities usually normalize or
develop into ST-segment elevation during an attack of chest
pain. In Wellens study, 60% of patients diagnosed with
Wellens syndrome had the characteristic electrocardiographic changes on admission. After admission, 56 (31%)
developed the changes within 24 hours, 10 (5%) within 2
days, 5 (2.8%) within 3 days, and 1 (0.6%) within 5 days.2
Electrocardiographic T-wave inversions may be related
to a number of clinical syndromes, ranging from life-threatening events such as acute coronary ischemia, pulmonary
embolism, and central nervous system injury, to entirely
benign presentations such as persistent juvenile T-wave
pattern and the digitalis effect. The list of differential possibilities of the inverted T wave is quite extensive, including acute coronary ischemia (non-Wellenoid ischemia,
Wellens presentation, and nonST-segment elevation
AMI), past myocardial infarction, persistent juvenile Twave pattern, left ventricular hypertrophy, bundle branch
block, digitalis effect, acute myocarditis, pre-excitation syndromes, acute pulmonary embolism, cerebrovascular accident, and later stages of pericarditis.4 If the EP considers the
following criteria in the interpretation of the ECG with
T-wave inversion, the differentiation of Wellens T waves
from other causes of inverted T waves will be easily accomplished (Table 1).3,5-7
The chest pain patient who presents with a convincing
clinical description of acute coronary syndrome and manifests electrocardiographic change involving the T wave in
the anterior distribution will likely be managed in appropriate fashion in terms of initial therapy, diagnostic studies,
and dispositionnitrates, aspirin, and -adrenergic blockade, among other agents coupled with repeat ECGs and
serum markers ending in an inpatient admission. Morphologically, Wellens T waves are either deeply inverted or
biphasic both congurations are highly characteristic of
the syndrome and unlike other T-wave inversions related to
acute confusional state (Fig 6). The major issue here is the
recognition of the syndrome and its relation to high-grade,
proximal LAD obstructionwith the natural history of extensive anterior wall AMI. The avoidance of provocative
testing, including stress imaging, is key in that such testing
may precipitate an AMI with signicant acute sequelae.
Continuing on in the differential, such T-wave changes can
TABLE 1. Clinical and Electrocardigraphic Criteria for Wellens
Syndrome
Symmetric and deeply inverted T waves, in leads V2 and V3,
occasionally in leads V1, V4, V5, and V6;
or
Biphasic T wave in leads V2 and V3;
plus
Isoelectric or minimally elevated (1 mm) ST segment
No precordial Q waves
History of angina
Pattern present in pain-free state
Normal or slightly elevated cardiac serum markers.
642
AMERICAN JOURNAL OF EMERGENCY MEDICINE Volume 20, Number 7 November 2002
FIGURE 6. A comparison of abnormal T-wave inversions in
acute ischemic heart disease. (A) Deeply inverted T wave of
Wellens syndrome. (B) Biphasic T wave of Wellens syndrome.
(C) Non-Wellens ischemic T-wave inversion. (D) Non-Wellens
ischemic T-wave inversion. The common feature that is useful in
distinguishing between these 2 types of inverted T waves and the
related clinical syndrome is the depth of the inverted T wave
considerably more so in Wellens syndrome.
occur owing to past myocardial infarction; once again, the
morphology of such T-wave changes (inverted symmetrically with minimal negative amplitude) is quite distinct
from the Wellens T waves.
Considering noncoronary causes of T-wave inversions,
the left ventricular hypertrophy and bundle branch block
patterns should be readily recognized by their signicant
coexistent ndings. For left ventricular hypertrophy, the
presence of prominent electric forces in the QRS complexes
of leads V1 to V6 is required to make the electrocardiographic diagnosis of left ventricular hypertrophy by voltage
criteria. The EP must also realize that such repolarization
change in left ventricular hypertrophy is usually limited to
leads I, aVl, V5, and V6. Regarding the bundle branch block
pattern, the widened QRS complex and characteristic morphologies of both right and left bundle branch block are
obvious clues to its presence. Left bundle branch block
pattern does not include T-wave inversion in leads V1 to
V4; right bundle branch block pattern does include such
T-wave changes.
From the perspective of electrocardiographically similar
T-wave inversions, those changes associated with acute
central nervous system insults are the most comparable.8
These T-wave changes are so similar, in fact, that they are
described as Wellenoid in appearance (Fig 7). These Twave changes are often very deeply inverted and/or biphasic
in morphology. Of course, the clinical presentation of the
patient (cephalgia, focal neurologic examination, and/or altered mental status) is likely to suggest the appropriate
diagnosis and solve the electrocardiographic differential
quandary.
Digitalis effect can be diagnosed electrocardiographically, of course, when the patient is using a digitalis compound. These T-wave changes most often are associated
with diffuse ST-segment depression and have the characteristic gradual descending limb of the T wave with a rapid
return to the baseline of the ascending portion. Acute pulmonary embolism, acute myocarditis, and pericarditis all
have characteristic historic and examination ndings that
will suggest the appropriate clinical diagnosis.
CONCLUSION
Wellens syndrome is a preinfarction stage of coronary
artery disease. Patients with this syndrome present with
FIGURE 7. ECG showing
extensive T-wave inversions
with biphasic morphology in
leads V2 to V6. This ECG
was obtained in a 54-year-old
patient who presented with altered mental status; cranial
computed tomography scan
showed extensive subarachnoid hemorrhage.
RHINEHARDT ET AL MANIFESTATIONS OF WELLENS SYNDROME
characteristic electrocardiographic ndings in the precordial leads. These changes are associated with obstruction
in the proximal LAD coronary artery. Two patterns of
electrocardiographic changes are encountered, the deeply
inverted T wave and the biphasic T wave. Once Wellens
syndrome has been recognized, cardiology consultation
for possible coronary angiography is likely necessary to
further evaluate the patient. Unless performed under the
supervision of a cardiologist, stress imaging is strongly
discouraged.
REFERENCES
1. de Zwann C, Bar FW, Wellens HJJ: Characteristic electrocardiographic pattern indicating a critical stenosis high in left anterior
descending coronary artery in patients admitted because of impending myocardial infarction. Am Heart J 1982;103:730-736
643
2. de Zwann C, Bar FW, Janssen JH, et al: Angiographic and
clinical characteristics of patients with unstable angina showing an
ECG pattern indicating critical narrowing of the proximal LAD coronary artery. Am Heart J 1989;117:657-665
3. Tandy TK, Bottomy DP, Lewis JG: Wellens Syndrome. Ann
Emerg Med 1999;33:347-351
4. Aufderheide TP, Brady WJ, Gibler B: Acute coronary ischemic
syndromes, in Marx J, Hockberger R, Walls R (eds): Rosens Emergency MedicineConcepts and Clinical Practice (ed 5). St. Louis,
MO, Mosby, Inc., 2001
5. Ondrusek RS: Spotting an MI before its an MI. RN 1996;59:
26-30
6. Kahn EC, Keller KB: Wellens syndrome in the emergency
department. J Emerg Nurs 1991;17:80-84
7. Paul S, Johnson P: Early recognition of critical stenosis high in
the left anterior descending coronary artery. Heart Lung 1990;19:
27-29
8. Perron AD, Brady WJ: Electrocardiographic manifestations of
CNS events. Am J Emerg Med 2000;18:715-720
Das könnte Ihnen auch gefallen
- Red Cell Morphology in Peripheral Smear and Automated Counter 2019 PDFDokument6 SeitenRed Cell Morphology in Peripheral Smear and Automated Counter 2019 PDFtufis02Noch keine Bewertungen
- Abnormal WBC Scattergram A Clue To The Diagnosis of MalariaDokument6 SeitenAbnormal WBC Scattergram A Clue To The Diagnosis of Malariatufis02Noch keine Bewertungen
- Utility - of - Scatterplot - Patterns - of - Automated - Hematology Analysers 2020Dokument6 SeitenUtility - of - Scatterplot - Patterns - of - Automated - Hematology Analysers 2020tufis02Noch keine Bewertungen
- Interpretation-Of-Histograms PresentationDokument46 SeitenInterpretation-Of-Histograms Presentationtufis02Noch keine Bewertungen
- A Specific Abnormal Scattergram of Peripheral Blood Leukocytes That May Suggest Hairy Cell LeukemiaDokument4 SeitenA Specific Abnormal Scattergram of Peripheral Blood Leukocytes That May Suggest Hairy Cell Leukemiatufis02Noch keine Bewertungen
- XN Training ManualDokument135 SeitenXN Training Manualtufis02100% (2)
- Hematology Discussion 2011 KPBDokument10 SeitenHematology Discussion 2011 KPBtufis02Noch keine Bewertungen
- Reticulated Platelets - Clinical Application and FDokument13 SeitenReticulated Platelets - Clinical Application and Ftufis02Noch keine Bewertungen
- Serous Effusions 2018Dokument303 SeitenSerous Effusions 2018tufis02Noch keine Bewertungen
- Hiperfibrinogenoliza Path-Upmc-Edu-Cases-Case264-Dx-HtmlDokument1 SeiteHiperfibrinogenoliza Path-Upmc-Edu-Cases-Case264-Dx-Htmltufis02Noch keine Bewertungen
- Dan Matei Abandoned Forts and Their Civi PDFDokument19 SeitenDan Matei Abandoned Forts and Their Civi PDFtufis02Noch keine Bewertungen
- Open or Close BOOKMARKS - : Ken Grauer, MD-KG/EKG Press (Gainesville, FL 600 Pages - 2014)Dokument15 SeitenOpen or Close BOOKMARKS - : Ken Grauer, MD-KG/EKG Press (Gainesville, FL 600 Pages - 2014)tufis02Noch keine Bewertungen
- Peripheral Smear Examination PDFDokument91 SeitenPeripheral Smear Examination PDFtufis02Noch keine Bewertungen
- Learning The Nodal Stations in The AbdomenDokument9 SeitenLearning The Nodal Stations in The Abdomentufis02Noch keine Bewertungen
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- 10 General Anatomy of The Cardiovascular SystemDokument140 Seiten10 General Anatomy of The Cardiovascular SystemSuzana VoiculescuNoch keine Bewertungen
- Betarie Anum Almira - RMIK (A) - Praktik KSPK 11Dokument1 SeiteBetarie Anum Almira - RMIK (A) - Praktik KSPK 11Betarie Anum AlmiraNoch keine Bewertungen
- NCP Preeclampsia and EclampsiaDokument16 SeitenNCP Preeclampsia and EclampsiaBiway Regala100% (1)
- JURNAL Diseksi AortaDokument3 SeitenJURNAL Diseksi AortaNurhidayantiAyaMSNoch keine Bewertungen
- Cardiomyopathy KonoDokument150 SeitenCardiomyopathy KonoValerian BîcosNoch keine Bewertungen
- Acute Myocardial Infarction Pa Tho Physiology Amp Schematic DiagramDokument6 SeitenAcute Myocardial Infarction Pa Tho Physiology Amp Schematic DiagramPeArl PeraltaNoch keine Bewertungen
- WBI11 01 Que 20220108Dokument28 SeitenWBI11 01 Que 20220108Hammodshan 7Noch keine Bewertungen
- Blood Supply of The Neck and HeadDokument56 SeitenBlood Supply of The Neck and HeadAdrianaNoch keine Bewertungen
- Cardiac Arrest: Signs and SymptomsDokument7 SeitenCardiac Arrest: Signs and SymptomsWebster The-TechGuy LunguNoch keine Bewertungen
- Data - Second Annual Data Science Bowl - KaggleDokument3 SeitenData - Second Annual Data Science Bowl - KaggleRVPNoch keine Bewertungen
- Umbilical Catheterization in ServiceDokument11 SeitenUmbilical Catheterization in ServiceLucian CaelumNoch keine Bewertungen
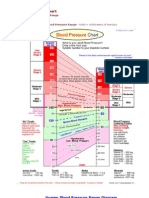
- Bloodpressure 2Dokument4 SeitenBloodpressure 2Yousuf Azhar AlamiaNoch keine Bewertungen
- Practical Checklist PD CVS OnlyDokument6 SeitenPractical Checklist PD CVS OnlyardiandawoodNoch keine Bewertungen
- Peran Perawat Pada Pemeriksaan Penunjang IVUS, OCT (Imaging)Dokument31 SeitenPeran Perawat Pada Pemeriksaan Penunjang IVUS, OCT (Imaging)Miftahul HudaNoch keine Bewertungen
- 2014-Brochure LeaderflexDokument2 Seiten2014-Brochure LeaderflexRaji VeeramalluNoch keine Bewertungen
- Blood Pressure ChartDokument5 SeitenBlood Pressure Chartmahajan1963100% (1)
- Ten Questions ICU Specialists Should Address When Managing Cardiogenic Acute Pulmonary OedemaDokument4 SeitenTen Questions ICU Specialists Should Address When Managing Cardiogenic Acute Pulmonary OedemaFarmacia Del Bosque100% (1)
- Circulatory SystemDokument49 SeitenCirculatory SystemBrent ValdespinaNoch keine Bewertungen
- Lymphatic System 2Dokument31 SeitenLymphatic System 2cardos cherryNoch keine Bewertungen
- Electrocardiogram: Dr. Yasser El-WazirDokument21 SeitenElectrocardiogram: Dr. Yasser El-WazirSalah Salah 201-901-341Noch keine Bewertungen
- Chest Pain Protocol in EDDokument3 SeitenChest Pain Protocol in EDshahidchaudharyNoch keine Bewertungen
- Pediatric Nursing Reviewer CardiovascularDokument4 SeitenPediatric Nursing Reviewer CardiovascularJemy Lorane TemporalNoch keine Bewertungen
- Heart Failure LCDokument14 SeitenHeart Failure LCgalih suharnoNoch keine Bewertungen
- Vitamin E Book For Ailing and Healthy Hearts - Wilfrid Shute PDF (Orthomolecular Medicine)Dokument212 SeitenVitamin E Book For Ailing and Healthy Hearts - Wilfrid Shute PDF (Orthomolecular Medicine)Anonymous gwFqQcnaX80% (5)
- Journal Coartation AortaDokument6 SeitenJournal Coartation AortaMangaismeNoch keine Bewertungen
- RBSE Class 8 Science Notes Chapter 7 Blood Circulation - RBSE GuideDokument3 SeitenRBSE Class 8 Science Notes Chapter 7 Blood Circulation - RBSE GuideAlpine AcademiaNoch keine Bewertungen
- Structured Oral Examination in Clinical Anaesthesia Practice Ex NDokument578 SeitenStructured Oral Examination in Clinical Anaesthesia Practice Ex Nkaran27091% (11)
- Nursing Care Plan For Client With Ineffective Tissue PerfusionDokument2 SeitenNursing Care Plan For Client With Ineffective Tissue PerfusionThe Right WayNoch keine Bewertungen
- Path-09 CARDIODokument18 SeitenPath-09 CARDIOCarlos Fernando Banegas FloresNoch keine Bewertungen
- Easy Rhythm Strip AnalysisDokument24 SeitenEasy Rhythm Strip Analysisheldai1100% (4)