Beruflich Dokumente
Kultur Dokumente
Stages of Labor
Hochgeladen von
FelmerPolancoRodaOriginalbeschreibung:
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Stages of Labor
Hochgeladen von
FelmerPolancoRodaCopyright:
Verfügbare Formate
Kate Audi S.
Aclan, RN
MN- 1
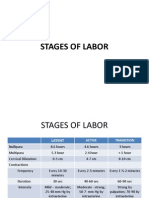
STAGES OF LABOR
Divided into three stages:
1. First Stage of Dilatation
- Which begins with the initiation of true labor contractions and ends when the cervix
is fully dilatated.
2. Second Stage
- Extending from the time of full dilatation until the infant is born.
3. Third Stage
- Also known as Placental Stage.
- Lasting from the time the infant is born until after the delivery of the placenta.
4. Fourth Stage
- The first 1 to 4 hours after birth of the placenta.
FIRST STAGE
1. LATENT PHASE ( Preparatory Phase)
- Begins at the onset of regularly perceived uterine contractions and ends when rapid
cervical dilatation begins.
- Contractions during this phase are mild and short, lasting 20 to 40 seconds.
- Cervical effacement occurs, and the cervix dilatates from 0 to 3cm.
- The phase lasts approximately 6 hours in a nullipara and 4.5 hours in a multipara.
- Cephalopelvic Disproportion a disproportion between the fetal head and pelvis.
Another reason for prolonged latent phase.
2. ACTIVE PHASE
- During this phase of labor, cervical dilatation occurs more rapidly increasing from 47cm.
- Contractions grow stronger, lasting 40-60seconds and occur approximately every 3
to 5 minutes.
- This phase last approximately 3 hours in nullipara and 2 hours for multipara.
- Show (increased vaginal secretions) and perhaps spontaneous rupture of
membranes may occur during this time.
3. TRANSITION PHASE
- Contractions reach their peak of intensity, occurring every 2 to 3 minutes with
duration of 60-90 seconds and causing maximum dilatation of 8-10cm.
- During this phase, a woman may experience intense discomfort, so strong that it is
accompanied by nausea and vomiting. Because of the intensity and intensity of the
contractions.
- May also experience a feeling of loss of control, anxiety, panic or irritability.
The peak of the transition phase can be identified by a slight slowing in the rate of
cervical dilatation when 9cm is reached (termed deceleration on a labor graph).
As woman reaches the end of this stage at 10cm of dilatation, a new sensation
occurs (i.e. an irresistible to push).
SECOND STAGE
-
Dilatation and effacement to birth of the infant.
With uncomplicated birth, this stage takes about 1hour.
THIRD STAGE
-
The placental stage, begin with the birth of the infant and ends with the delivery of
the placenta.
Two separate phases are involved:
1. PLACENTAL SEPARATION
Signs indicate that the placenta has loosened and is ready to deliver:
Lengthening of the umbilical cord
Sudden gush of vaginal blood
Change in the shape of the uterus
Firm contraction of the uterus
Appearance of the placenta at the vaginal opening
Types of Placenta
Schultze Placenta
-
Appearing shiny and glistening from the fetal membranes
Duncan Placenta
-
Looks raw, red and irregular with the ridges or cotyledons that separate blood
collection spaces showing.
Brandt- Andrews Manuever
-
push and pulling of the umbilical cord.
Up and down manuever
2. PLACENTAL EXPULSION
- After separation, the placenta is delivered either by the natural bearing down effort
of the mother or by the gentle pressure on the contracted uterine fundus by the
physician or nurse-midwife (Credes Manuever).
INTRAPARTUM PAIN EXPERIENCE
A. Overview of Pain
1. Intrapartum pain is a subjective experience of physical sensations associated with
uterine contractions, cervical dilatations and effacements, and fetal descent during
labor and birth.
2. Physiologic responses to pain may include increased blood pressure, pulse,
respirations, perspirations, pupil diameter, muscle tension (such as facial tension or
fisted hands) or muscle activity (sush as pacing, turning, or twisting)
3. Nonverbal expressions of pain may include withdrawal, hostility, fear depression.
4. 4. Verbal expressions of pain may include statement of pain, moaning and groaning.
B. Factors affecting perception of Intrapartum pain.
1. Previous experience with painful stimuli and personal expectations of the birth
experience.
2. Cultural concept of pain, specifically during childbirth, and how one should respond.
3. Rapidly progressive uterine contractions.
4. Fear, anxiety, and fatigue.
C. Physiologic causes of Intrapartum pain
1. Uterine anoxia due to compressed muscle cells during the contraction.
2. Compression of the nerve ganglia in the cervix and lower uterine segment during the
contraction.
3. Stretching of the cervix during dilation and effacement
4. Traction on, and stretching and displacement of the perineum
5. Pressure on the urethra, bladder and rectum during fetal descent
6. Distention of the lower uterine segment
7. Stretching of the uterine ligaments
Das könnte Ihnen auch gefallen
- Stages of LaborDokument23 SeitenStages of LaborPortia Dulce Toquero100% (5)
- Procedure-Assessing Fetal Heart ToneDokument1 SeiteProcedure-Assessing Fetal Heart ToneCyril Joy N. FernandoNoch keine Bewertungen
- Perineal CareDokument7 SeitenPerineal CareAna Maria Teresa H RollanNoch keine Bewertungen
- Vacuum Extraction (Ventouse)Dokument3 SeitenVacuum Extraction (Ventouse)dusty kawiNoch keine Bewertungen
- Unit VIII PRESUMPTIVE SIGNS AND SYMPTOMS OF PREGNANCYDokument5 SeitenUnit VIII PRESUMPTIVE SIGNS AND SYMPTOMS OF PREGNANCYNancy100% (1)
- PERINEAL CARE-femaleDokument17 SeitenPERINEAL CARE-femaleDarren RobertoNoch keine Bewertungen
- Esarean Ction: Cadalin, Fremelen Rose Cedamon, CarloDokument18 SeitenEsarean Ction: Cadalin, Fremelen Rose Cedamon, CarloMonette Abalos MendovaNoch keine Bewertungen
- Ballard Gestational Age AssessmentDokument8 SeitenBallard Gestational Age AssessmentgailNoch keine Bewertungen
- Complications of PostpartumDokument10 SeitenComplications of PostpartumAlverastine AnNoch keine Bewertungen
- BUBBLESHEDokument10 SeitenBUBBLESHEmaaaaarjNoch keine Bewertungen
- Stages of LaborDokument51 SeitenStages of LaborZeen_Zeen_Fern_3128100% (4)
- Multiple PregnancyDokument20 SeitenMultiple PregnancySelma FraNoch keine Bewertungen
- Determining Fetal Position with Leopold's ManeuversDokument3 SeitenDetermining Fetal Position with Leopold's ManeuversKristine Marie de MesaNoch keine Bewertungen
- Process of LabourDokument6 SeitenProcess of LabourAnnapurna Dangeti100% (1)
- Nursing Care for High-Risk Labor and DeliveryDokument170 SeitenNursing Care for High-Risk Labor and DeliveryLongyapon Sheena Stephanie100% (2)
- A. Dystocia: Problems With PowerDokument48 SeitenA. Dystocia: Problems With PowerPauline GarciaNoch keine Bewertungen
- Leopold's ManeuverDokument22 SeitenLeopold's ManeuverArlene Cerdeña Salceda100% (1)
- Partograph Monitoring Labor ProgressDokument65 SeitenPartograph Monitoring Labor ProgressAmyAgustinNoch keine Bewertungen
- Psychological Changes of PregnancyDokument6 SeitenPsychological Changes of PregnancyMarie PotayreNoch keine Bewertungen
- Theories of Labor OnsetDokument4 SeitenTheories of Labor OnsetCzarina PorciunculaNoch keine Bewertungen
- Signs of LaborDokument5 SeitenSigns of Labormarianne_07Noch keine Bewertungen
- Normal Labor: Ms. Mayuri Patel Sandra Shroff Rofel College of Nursing, VapiDokument48 SeitenNormal Labor: Ms. Mayuri Patel Sandra Shroff Rofel College of Nursing, Vapivimmy47100% (1)
- Nursing Care of The Family Experiencing A Sudden Pregnancy ComplicationDokument7 SeitenNursing Care of The Family Experiencing A Sudden Pregnancy ComplicationDacillo GailleNoch keine Bewertungen
- Midterm Notes On NCM 109 EditedDokument10 SeitenMidterm Notes On NCM 109 EditedJohn Fred100% (2)
- Excess Amniotic Fluid Causes and DiagnosisDokument2 SeitenExcess Amniotic Fluid Causes and DiagnosisAde Yonata100% (1)
- Tarlacstateuniversity College of Science Nursing DepartmentDokument5 SeitenTarlacstateuniversity College of Science Nursing DepartmentBethrice MelegritoNoch keine Bewertungen
- Notes On Obstetrics: Normal Labor (Theories of Labor Onset)Dokument22 SeitenNotes On Obstetrics: Normal Labor (Theories of Labor Onset)Jobelle Acena100% (1)
- Uterine RuptureDokument19 SeitenUterine RuptureAna Denise Quinajon0% (1)
- Breast Care and Assisting in BreastfeedingDokument7 SeitenBreast Care and Assisting in BreastfeedingBJ FernandezNoch keine Bewertungen
- Stages of Labor and DeliveryDokument7 SeitenStages of Labor and DeliveryAijem Ryan86% (7)
- Reva Rubin Maternal Role Attainment TheoryDokument4 SeitenReva Rubin Maternal Role Attainment TheoryLeonard LigutomNoch keine Bewertungen
- Nursing Care of a Toddler and FamilyDokument6 SeitenNursing Care of a Toddler and FamilyIan Mendez100% (1)
- Done LEOPOLDS MANEUVER MONICITDokument2 SeitenDone LEOPOLDS MANEUVER MONICITMoiraMaeBeridoBaliteNoch keine Bewertungen
- Leopold's Maneuvers: Assessing Fetal PositionDokument6 SeitenLeopold's Maneuvers: Assessing Fetal PositionJoeyca Shien PiolNoch keine Bewertungen
- Components of LaborDokument5 SeitenComponents of LaborJeraldine Lindo100% (4)
- Stages of LaborDokument30 SeitenStages of LaborPerrilyn Perey100% (1)
- Placental Abnormalities Normal Placenta: © Mary Andrea G. Agorilla, Ust-Con 2021 - 1Dokument3 SeitenPlacental Abnormalities Normal Placenta: © Mary Andrea G. Agorilla, Ust-Con 2021 - 1Mary AgorillaNoch keine Bewertungen
- Abdominal ExaminationDokument5 SeitenAbdominal ExaminationAnuradha MauryaNoch keine Bewertungen
- C-Section Procedure GuideDokument4 SeitenC-Section Procedure GuideKeanu ArcillaNoch keine Bewertungen
- Vaginal Speculum Delivery Tools GuideDokument25 SeitenVaginal Speculum Delivery Tools GuideMayolianne DumayNoch keine Bewertungen
- 9 Labor and DeliveryDokument6 Seiten9 Labor and DeliveryUri Perez MontedeRamosNoch keine Bewertungen
- Monitoring Labor Progress with the PartographDokument6 SeitenMonitoring Labor Progress with the Partographalyssa marie salcedo100% (1)
- NonStress TestDokument2 SeitenNonStress TestRama_ichiNoch keine Bewertungen
- Naegele's RuleDokument5 SeitenNaegele's RuleSarah Jane MaganteNoch keine Bewertungen
- Theories of Labor Onset and ProgressionDokument6 SeitenTheories of Labor Onset and ProgressionKenny NadelaNoch keine Bewertungen
- NCM 109 Care of Mother and Child at RiskDokument10 SeitenNCM 109 Care of Mother and Child at RiskMia Fe Cuaya Lorenzo100% (1)
- Stages of LaborDokument14 SeitenStages of LaborKimberly CostalesNoch keine Bewertungen
- Stages of LaborDokument5 SeitenStages of LaborGeraldine Marie Salvo100% (3)
- Maternal and Child Health Nursing: May Ann B. Allera, RNDokument16 SeitenMaternal and Child Health Nursing: May Ann B. Allera, RNmayal100% (1)
- Prenatal Management (Part 4)Dokument17 SeitenPrenatal Management (Part 4)Austine James Sabenicio PantiloNoch keine Bewertungen
- Labor and DeliveryDokument4 SeitenLabor and DeliveryJinky Teneza100% (1)
- Maternal and Child Nursing - Intrapartum PeriodDokument91 SeitenMaternal and Child Nursing - Intrapartum Periodchuppepay20% (5)
- Labor & DeliveryDokument14 SeitenLabor & DeliveryNiña Eleana FranciscoNoch keine Bewertungen
- Abortionsource 100605123737 Phpapp01Dokument38 SeitenAbortionsource 100605123737 Phpapp01Erina Erichan OtoNoch keine Bewertungen
- Maternal and Child Care Skills for Labor and DeliveryDokument61 SeitenMaternal and Child Care Skills for Labor and DeliveryboinkjilijoyNoch keine Bewertungen
- Normal Spontaneous Delivery: Reyes, Janyn Marione ADokument35 SeitenNormal Spontaneous Delivery: Reyes, Janyn Marione AJanyn Abella ReyesNoch keine Bewertungen
- Stages of Labor Delivery 2022Dokument25 SeitenStages of Labor Delivery 2022xuxi dulNoch keine Bewertungen
- Updated NCM 107 Lecture Week 7Dokument27 SeitenUpdated NCM 107 Lecture Week 7Quencee CalaycayNoch keine Bewertungen
- Stages of LaborDokument16 SeitenStages of LaborThrecia RotaNoch keine Bewertungen
- Parenting StylesDokument1 SeiteParenting StylesFelmerPolancoRodaNoch keine Bewertungen
- Safari 22 Jun 2019 at 1021 AMDokument1 SeiteSafari 22 Jun 2019 at 1021 AMFelmerPolancoRodaNoch keine Bewertungen
- Theoretical BackgroundDokument3 SeitenTheoretical BackgroundFelmerPolancoRodaNoch keine Bewertungen
- Involvement of Father in ChildbearingDokument3 SeitenInvolvement of Father in ChildbearingFelmerPolancoRodaNoch keine Bewertungen
- University dorm pass for daughterDokument1 SeiteUniversity dorm pass for daughterFelmerPolancoRodaNoch keine Bewertungen
- NSVDDokument8 SeitenNSVDFelmerPolancoRodaNoch keine Bewertungen
- Letter BingdayDokument1 SeiteLetter BingdayFelmerPolancoRodaNoch keine Bewertungen
- Ype of Statistics Which Deals With Making Conclusions. It Inferences About The Predictions For The Population. It Also Analyses The SampleDokument1 SeiteYpe of Statistics Which Deals With Making Conclusions. It Inferences About The Predictions For The Population. It Also Analyses The SampleFelmerPolancoRodaNoch keine Bewertungen
- Paternal Involvement and Childbearing Outcome Among Teenage Couple1Dokument3 SeitenPaternal Involvement and Childbearing Outcome Among Teenage Couple1FelmerPolancoRodaNoch keine Bewertungen
- Nursing Care Plan for Labor and DeliveryDokument2 SeitenNursing Care Plan for Labor and DeliveryFelmerPolancoRodaNoch keine Bewertungen
- Pre Eclampsia Case StudyDokument38 SeitenPre Eclampsia Case StudyFelmerPolancoRodaNoch keine Bewertungen
- Lecture Objectives & OutlinesDokument25 SeitenLecture Objectives & OutlinesFelmerPolancoRodaNoch keine Bewertungen
- 100514Dokument1 Seite100514FelmerPolancoRodaNoch keine Bewertungen
- Nola PenderDokument5 SeitenNola PenderFelmerPolancoRodaNoch keine Bewertungen
- SpecsDokument6 SeitenSpecsFelmerPolancoRodaNoch keine Bewertungen
- Ante PartumDokument101 SeitenAnte PartumFelmerPolancoRodaNoch keine Bewertungen
- Nursing Care Plan for Labor and DeliveryDokument2 SeitenNursing Care Plan for Labor and DeliveryFelmerPolancoRodaNoch keine Bewertungen
- Copd Final GDokument76 SeitenCopd Final GFelmerPolancoRodaNoch keine Bewertungen
- DF-650 Super Surgical Suction Unit (Digital)Dokument13 SeitenDF-650 Super Surgical Suction Unit (Digital)Fem CruzNoch keine Bewertungen
- Nola PenderDokument5 SeitenNola PenderFelmerPolancoRodaNoch keine Bewertungen
- SigDokument1 SeiteSigFelmerPolancoRodaNoch keine Bewertungen
- Demon Star orDokument3 SeitenDemon Star orFelmerPolancoRodaNoch keine Bewertungen
- LicenseDokument3 SeitenLicenseCharisse Anne M. AlbañaNoch keine Bewertungen
- Which Perform The Major Social Functions Having Locality Relevance. This Is AnotherDokument2 SeitenWhich Perform The Major Social Functions Having Locality Relevance. This Is AnotherFelmerPolancoRodaNoch keine Bewertungen
- Definition ReportDokument6 SeitenDefinition ReportFelmerPolancoRodaNoch keine Bewertungen
- Companion CD: Companion CD-ROM For Silvestri: Saunders Comprehensive Review For The NCLEX-RN®, 4th EditionDokument2 SeitenCompanion CD: Companion CD-ROM For Silvestri: Saunders Comprehensive Review For The NCLEX-RN®, 4th EditionnnaledNoch keine Bewertungen
- Integrated Management of Childhood Illness: Child Aged 2 Months Up To 5 YearsDokument44 SeitenIntegrated Management of Childhood Illness: Child Aged 2 Months Up To 5 YearsJulio Iñigo López100% (22)
- Companion CD: Companion CD-ROM For Silvestri: Saunders Comprehensive Review For The NCLEX-RN®, 4th EditionDokument2 SeitenCompanion CD: Companion CD-ROM For Silvestri: Saunders Comprehensive Review For The NCLEX-RN®, 4th EditionnnaledNoch keine Bewertungen
- Which Perform The Major Social Functions Having Locality Relevance. This Is AnotherDokument2 SeitenWhich Perform The Major Social Functions Having Locality Relevance. This Is AnotherFelmerPolancoRodaNoch keine Bewertungen
- Combined Use of Antibiotics As A Risk Factor For HDokument15 SeitenCombined Use of Antibiotics As A Risk Factor For HGemala AdillawatyNoch keine Bewertungen
- Best Homeopathic Doctor in SydneyDokument8 SeitenBest Homeopathic Doctor in SydneyRC homeopathyNoch keine Bewertungen
- A Reading On: Superior Vena Cava SyndromeDokument3 SeitenA Reading On: Superior Vena Cava SyndromeRaijenne VersolaNoch keine Bewertungen
- 236 297Dokument8 Seiten236 297Andrea KamóNoch keine Bewertungen
- Mystery Respiratory Illness Heatherwood Retirement Near Fort Detrick (July 2019)Dokument5 SeitenMystery Respiratory Illness Heatherwood Retirement Near Fort Detrick (July 2019)Kevin SteinerNoch keine Bewertungen
- NIGHTINGALE INSTITUTE OF NURSING ASSIGNMENT ON DISASTER MANAGEMENTDokument15 SeitenNIGHTINGALE INSTITUTE OF NURSING ASSIGNMENT ON DISASTER MANAGEMENTDeepti KukretiNoch keine Bewertungen
- Case Scenario CHFDokument2 SeitenCase Scenario CHFchetankumarbhumireddyNoch keine Bewertungen
- Topic 6: Microbiology, Immunity and Forensics Chapter 6B: ImmunityDokument3 SeitenTopic 6: Microbiology, Immunity and Forensics Chapter 6B: ImmunitysalmaNoch keine Bewertungen
- Abnormal Psychology Essay 2Dokument4 SeitenAbnormal Psychology Essay 2Andrew TsengNoch keine Bewertungen
- PsychDokument21 SeitenPsychطاهرة حربية AlcaldeNoch keine Bewertungen
- Week 4 Ortho TestsDokument15 SeitenWeek 4 Ortho Testsapi-468597987Noch keine Bewertungen
- (CVI) Chronic Vein InsufisiensiDokument19 Seiten(CVI) Chronic Vein Insufisiensiyessi hennyNoch keine Bewertungen
- Nutritional Problems 2023 by Chimdesa JabesaDokument32 SeitenNutritional Problems 2023 by Chimdesa JabesaTekle TayeNoch keine Bewertungen
- Reviewer in Science 4Dokument9 SeitenReviewer in Science 4Raymond ForteNoch keine Bewertungen
- Science9 Reyes, J, P Q1.W2Dokument12 SeitenScience9 Reyes, J, P Q1.W2Jeane Pineda ReyesNoch keine Bewertungen
- Understanding PterygiumDokument4 SeitenUnderstanding PterygiumBambank FarhansyahNoch keine Bewertungen
- BÀI ĐỌC ĐIỀNHIỂU VỀ COVID 19 DAP AN CHI TIET 1Dokument78 SeitenBÀI ĐỌC ĐIỀNHIỂU VỀ COVID 19 DAP AN CHI TIET 1Văn Nhân100% (1)
- Efektifitas Pemberian Kompres Tepid Water Sponge Dan Pemberian Kompres Bawang Merah Terhadap Penurunan Suhu Tubuh Anak Demam Di Banjarmasin, Kalimantan Selatan PDFDokument7 SeitenEfektifitas Pemberian Kompres Tepid Water Sponge Dan Pemberian Kompres Bawang Merah Terhadap Penurunan Suhu Tubuh Anak Demam Di Banjarmasin, Kalimantan Selatan PDFUlI SinagaNoch keine Bewertungen
- Covid 19 Dashboard 11-5-2020 DeathsDokument2 SeitenCovid 19 Dashboard 11-5-2020 DeathsRami Abou-SabeNoch keine Bewertungen
- ICD - Implantable Cardioverter DefibrillatorDokument8 SeitenICD - Implantable Cardioverter DefibrillatorJon SmithNoch keine Bewertungen
- The risks of vaping for young people (37 charactersDokument9 SeitenThe risks of vaping for young people (37 charactersMR. ARVIND BHATEWARANoch keine Bewertungen
- Case Study "John Rick Corpuz"Dokument2 SeitenCase Study "John Rick Corpuz"sir jjNoch keine Bewertungen
- Burns ActvityDokument2 SeitenBurns ActvityJoshua TercenoNoch keine Bewertungen
- Nursing Diagnosis-Readiness For Enhanced Immunization StatusDokument2 SeitenNursing Diagnosis-Readiness For Enhanced Immunization StatusMarsha Angelie75% (4)
- Hip Pain in Pregnancy GTPS - Oct19-1Dokument3 SeitenHip Pain in Pregnancy GTPS - Oct19-1Ryan CrossNoch keine Bewertungen
- Causes, Symptoms and Treatment of Pregnancy-Induced HypertensionDokument2 SeitenCauses, Symptoms and Treatment of Pregnancy-Induced HypertensionJohn Lemuel GuevarraNoch keine Bewertungen
- Patogenesis Kematian Covid19Dokument32 SeitenPatogenesis Kematian Covid19Santoto MantapNoch keine Bewertungen
- Gestational Diabetes MellitusDokument3 SeitenGestational Diabetes MellitusJustine DumaguinNoch keine Bewertungen
- Multi Sera Calibrator: Value Sheet of Mindray BS Measurement SystemDokument4 SeitenMulti Sera Calibrator: Value Sheet of Mindray BS Measurement Systemtech yuva cscNoch keine Bewertungen
- Identifikasi Biokimia Dan Aktivitas Antibakteri Isolat Bakteri Asam Laktat Dari Limbah Sayur Sawi (Brassica Juncea L.)Dokument10 SeitenIdentifikasi Biokimia Dan Aktivitas Antibakteri Isolat Bakteri Asam Laktat Dari Limbah Sayur Sawi (Brassica Juncea L.)AdeNoch keine Bewertungen