Beruflich Dokumente
Kultur Dokumente
Testosterone and Erectile Function An Unresolved Enigma
Hochgeladen von
Yeti MaretaOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Testosterone and Erectile Function An Unresolved Enigma
Hochgeladen von
Yeti MaretaCopyright:
Verfügbare Formate
european urology 52 (2007) 2628
available at www.sciencedirect.com
journal homepage: www.europeanurology.com
Editorial
referring to the article published on pp. 5470 of this issue
Testosterone and Erectile Function: An Unresolved Enigma
Konstantinos Hatzimouratidis, Dimitrios Hatzichristou *
2nd Department of Urology, Papageorgiou General Hospital and Center for Sexual and Reproductive Health,
Aristotle University of Thessaloniki, Greece
Erectile function depends on a complex interrelationship between psychological, neurologic, vascular,
and endocrine factors. It is well known that androgens play a critical role in the physiology of erectile
function. This statement was based on several
clinical observations: (1) castration is associated with
a decline in sexual interest and erectile function,
although some potency may be maintained; (2)
antiandrogens result in erectile dysfunction (ED),
although sexual interest may persist; and (3) androgen supplementation improves sexual function in
hypogonadal men. However, the underlying
mechanisms by which androgens regulate erectile
function are poorly defined [1]. In their in depth and
thoughtful review article, Traish et al provide an
extensive analysis of the cellular, molecular, and
physiologic mechanisms of androgens in erectile
physiology and try to incorporate current evidence
into clinical practice [2]. Several questions are raised
from this article that stimulate discussion and
provide guidance for future research.
1.
Do we have hard data that androgens are
critical for erectile function?
Preclinical studies provide evidence that androgens
modulate erectile function in several ways [1].
Testosterone may regulate central and peripheral
mechanisms of penile erection. Androgen deficiency
is associated with structural changes in the cavernous nerves consistent with nerve atrophy and
androgen supplementation may reverse these
changes resulting in nerve regeneration. Although
these data remain to be proved in humans, they may
explain the lack of clinical response with androgen
therapy in men. The expression and activity of
nitrous oxide synthase (NOS) isoforms in the corpus
cavernosum is reduced after castration and these
changes are reversed with androgen administration.
Because smooth muscle relaxation and erection
depend on NO, they are believed to be androgen
dependent too. Furthermore, castration has been
shown to reduce the expression and activity of
phosphodiesterase type 5 (PDE5) and androgen
supplementation has been shown to up-regulate
the expression and activity of PDE5. These data are
consistent with the clinical evidence that although
PDE5 administration may improve erectile function
in hypogonadal men or men with low testosterone
levels, erectile response is maximized following
androgen supplementation. Finally, androgen deprivation significantly reduces trabecular smooth muscle content and increases connective tissue
deposition. Furthermore, smooth muscle appears
disorganized, with a large number of cytoplasmic
vacuoles, whereas cellular structures resembling
adipocytes have been identified in the subtunical
region of the corpus cavernosum. These observations
are also consistent with basic research and clinical/
pathologic evidence showing that reduced cavernosal smooth muscle content is associated with venoocclusive dysfunction. Although most data are based
on animal studies that cannot be extrapolated to
DOI of original article: 10.1016/j.eururo.2007.02.034
* Corresponding author.
E-mail address: hatzichr@med.auth.gr (D. Hatzichristou).
0302-2838/$ see back matter # 2007 Published by Elsevier B.V. on behalf of European Association of Urology.
doi:10.1016/j.eururo.2007.03.025
european urology 52 (2007) 2628
humans, a growing body of evidence supports the
important role of androgens in erectile function.
In humans, androgens are critical for the development and growth of secondary sexual organs
including the penis. Children with androgen deficiency develop micropenis, whereas this is not the
case after attainment of sexual maturity. Androgen
ablation in patients with prostate cancer significantly
reduces frequency, duration, and rigidity of nocturnal
erections based on nocturnal penis tumescence and
rigidity (NPTR) recordings. Furthermore, erectile
function domain scores on the International Index
of Erectile Function (IIEF) are reduced in hypogonadal
men, whereas testosterone administration is able to
reverse the abnormal NPTR recordings and improve
erectile function. The high prevalence of hypogonadism and ED in metabolic syndrome and its components is another field of current research [3]. Low
testosterone is strongly associated with the metabolic syndrome and ED is highly associated with the
metabolic syndrome and comorbidities associated
with it; hypogonadism is a predictor of type 2
diabetes and androgen-deprivation therapy for
prostate cancer is associated with increased risk
of diabetes, coronary heart disease, myocardial
infarction, sudden cardiac death, and worsening of
existing diabetes. Besides that, testosterone therapy
may improve insulin sensitivity and reduce abdominal obesity. However, it remains unclear whether
hypogonadism contributes to the pathogenesis
of the metabolic syndrome or the reverse is true.
2.
Which is the appropriate work-up in
hypogonadal men with ED?
Prevalence rates of androgen insufficiency and
ED vary from 1.7% to 35% in different studies,
depending on the study sample and setting. Lateonset hypogonadism (LOH) is a clinical and biochemical syndrome frequently associated with
advancing age and characterized by a deficiency
in serum androgen levels, with or without changes
in receptor sensitivity to androgens. It may affect
the function of multiple organ systems and result
in significant detriment in the quality of life,
including major alterations in sexual function.
Sexual dysfunction may be the presenting symptom but depression, irritability, cognition and sleep
disturbances, increase in visceral fat, decrease in
body hair, and skin alterations must not be
neglected in history-taking and clinical assessment. Biochemical determination of low androgen
levels must accompany clinical evidence for androgen insufficiency.
27
Medical and sexual history, incorporating
physical examination findings, will usually reveal
suspicious cases of hypogonadism. Screening
questionnaires (Androgen Deficiency in the Aging
Male [ADAM], Aging Males Symptoms, [AMS] and a
structured interview [ANDROTEST]) are relatively
nonspecific and they are not recommended in
clinical practice [4]. Testosterone assessment
remains a major point of debate. Total testosterone
values follow the circadian rhythm and measurement in the early morning is recommended, despite
the fact that this circadian rhythm is lost with aging
and morning assessment may not be as important as
it was thought to be. But should we measure total
testosterone? Due to the fact that only unbound
testosterone is active and sex hormone-binding
globulin (SHBG) is increasing with age, total testosterone assessment is considered today unreliable.
Bioavailable and free testosterone assessments are
recommended. Although measurement of bioavailable testosterone is reliable, this is not the case for
free testosterone. Therefore, the most accessible and
reliable assays to establish the presence of hypogonadism are the measurement of bioavailable testosterone or the calculated free testosterone (cFT). This
assessment is incorporated in basic evaluation of the
patient with ED in almost all current guidelines [5,6].
3.
Why is erectile function preserved in some
men with low androgen levels?
It seems that there is a testosterone threshold value
(about 10% of the normal values), below which
erectile function declines in a dose-dependent fashion [7]. Androgen-dependent tissues have varying
sensitivities to circulating testosterone levels. Androgen receptor polymorphism may play a key role. This
means that an individual with low testosterone
values may maintain erections due to the high
activity of androgen receptor and vice versa. In
addition, testosterone is not the only androgen
associated with erectile function but dihydrotestosterone (DHT), adrenal androgens (such as dehydroepiandrosterone [DHEA] and DHEA sulfate [DHEA-S]),
estrogens, and conjugated metabolites are also
important. Should we measure all these hormones?
The answer is no for the routine clinical practice, but
in some specific cases this assessment may be of
value although these determinations are complex
and not yet standardized. These may include
patients treated with 5a-reductase inhibitors or
those for whom there is no clear reason for the lack
of response to testosterone. Similarly, traditional
hormonal assessment including follicle-stimulating
28
european urology 52 (2007) 2628
hormone (FSH), luteinizing hormone (LH), thyroidstimulating hormone (TSH), and prolactin is not
indicated in the uncomplicated evaluation of ED
associated with LOH, but must considered when
systemic endocrine disorders are suspected or when
androgen supplementation fails to restore hypogonadism and erectile function.
4.
How should we treat the hypogonadal man
with ED?
Although several testosterone formulations are
available, testosterone topical gel and long-term
depot injections are the preferred treatment
options today, due to their favorite pharmacokinetic profile characterized by relatively constant
plasma levels, avoiding wide fluctuations and
minimal side effects. A point of debate is the
presence of borderline testosterone levels. Testosterone supplementation in these patients is generally justified especially in those not responding to
PDE5 inhibitors (PDE5-Is). The therapeutic role of
other treatments (such as DHEA, aromatase inhibitors, or clomiphene citrate) is not supported by
rigorous data and may be considered only in
selected cases with complex endocrine disorders.
PDE5-Is are today the first treatment option for men
with ED. Although as many as 75% of hypogonadal
men with ED may respond to a PDE5-I alone,
response is maximized after combination treatment [8]. Another point of interest is patients with
borderline or abnormal testosterone levels do not
respond to PDE5-Is; in such patients LOH may be the
cause, and physicians should be aware that coadministration of testosterone supplementation with
a PDE5-I may reverse non-responders to responders. Initial studies have shown that up to 58% of
patients converted to responders with this combination treatment [9]. However, because several
other risk factors for ED may be present in elderly
men, testosterone supplementation may not
restore erectile function despite normalization of
testosterone levels.
Finally, attention should be paid to the follow-up
protocol for patients receiving testosterone supplementation. Testosterone assessment, hematologic
examinations (hematocrit and hemoglobin), liver
function tests, bone density, and a lipid profile must
be periodically evaluated although there is no
consensus on optimal time intervals. Digital rectal
examination (DRE) and determination of serum
prostate-specific antigen (PSA) are mandatory in
men over the age of 45 yr as baseline measurements
of prostate health prior to therapy with testosterone,
at quarterly intervals for the first 12 mo, and yearly
thereafter. Although it is commonly believed that
testosterone causes enhanced growth of prostate
cancer, this association is poorly defined [10]. No
large, long-term studies of testosterone replacement
therapy have been performed. The prostate cancer
rates in published studies are approximately 1%,
similar to the cancer detection rate in prostate
cancer screening trials. While we wait for largescale, well-designed studies with high-level evidence, patients receiving testosterone replacement
therapy need close medical monitoring.
References
[1] Traish AM, Guay AT. Are androgens critical for penile
erections in humans? Examining the clinical and preclinical evidence. J Sex Med 2006;3:382404, discussion 4047.
[2] Traish AM, Goldstein I, Kim NN. Testosterone and erectile
function: from basic research to a new clinical paradigm
for managing men with androgen insufficiency and erectile dysfunction. Eur Urol 2007;52:5470.
[3] Kupelian V, Shabsigh R, Araujo AB, ODonnell AB, McKinlay JB. Erectile dysfunction as a predictor of the metabolic
syndrome in aging men: results from the Massachusetts
Male Aging Study. J Urol 2006;176:2226.
[4] Morley JE, Perry III HM, Kevorkian RT, Patrick P. Comparison of screening questionnaires for the diagnosis of
hypogonadism. Maturitas 2006;53:4249.
[5] Nieschlag E, Swerdloff R, Behre HM, et al. Investigation,
treatment and monitoring of late-onset hypogonadism in
males. ISA, ISSAM, and EAU recommendations. Eur Urol
2005;48:14.
[6] Wespes E, Amar E, Hatzichristou D, et al. EAU guidelines
on erectile dysfunction: an update. Eur Urol 2006;49:806
15.
[7] Montorsi F, Oettel M. Testosterone and sleep-related erections: an overview. J Sex Med 2005;2:77184.
[8] Guay AT, Perez JB, Jacobson J, Newton RA. Efficacy and
safety of sildenafil citrate for treatment of erectile dysfunction in a population with associated organic risk
factors. J Androl 2001;22:7937.
[9] Shabsigh R, Kaufman JM, Steidle C, Padma-Nathan H.
Randomized study of testosterone gel as adjunctive therapy to sildenafil in hypogonadal men with erectile dysfunction who do not respond to sildenafil alone. J Urol
2004;172:65863.
[10] Morgentaler A. Testosterone and prostate cancer: an historical perspective on a modern myth. Eur Urol 2006;50:
9359.
Das könnte Ihnen auch gefallen
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Mastertop 1230 Plus PDFDokument3 SeitenMastertop 1230 Plus PDFFrancois-Noch keine Bewertungen
- Grade 7 ExamDokument3 SeitenGrade 7 ExamMikko GomezNoch keine Bewertungen
- Analysis of Electric Machinery Krause Manual Solution PDFDokument2 SeitenAnalysis of Electric Machinery Krause Manual Solution PDFKuldeep25% (8)
- Snapdragon 435 Processor Product Brief PDFDokument2 SeitenSnapdragon 435 Processor Product Brief PDFrichardtao89Noch keine Bewertungen
- Pe 03 - Course ModuleDokument42 SeitenPe 03 - Course ModuleMARIEL ASINoch keine Bewertungen
- German Atv-Dvwk Rules and StandardsDokument25 SeitenGerman Atv-Dvwk Rules and StandardsMehmet Emre Bastopcu100% (1)
- DNA ReplicationDokument19 SeitenDNA ReplicationLouis HilarioNoch keine Bewertungen
- WL-80 FTCDokument5 SeitenWL-80 FTCMr.Thawatchai hansuwanNoch keine Bewertungen
- MRBR ATR 72 Rev18Dokument424 SeitenMRBR ATR 72 Rev18Juan Forero OrtizNoch keine Bewertungen
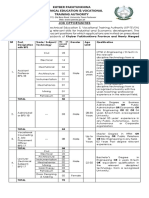
- KP Tevta Advertisement 16-09-2019Dokument4 SeitenKP Tevta Advertisement 16-09-2019Ishaq AminNoch keine Bewertungen
- Global Geo Reviewer MidtermDokument29 SeitenGlobal Geo Reviewer Midtermbusinesslangto5Noch keine Bewertungen
- Equivalent Fractions Activity PlanDokument6 SeitenEquivalent Fractions Activity Planapi-439333272Noch keine Bewertungen
- An Exploration of The Ethno-Medicinal Practices Among Traditional Healers in Southwest Cebu, PhilippinesDokument7 SeitenAn Exploration of The Ethno-Medicinal Practices Among Traditional Healers in Southwest Cebu, PhilippinesleecubongNoch keine Bewertungen
- Vendor Information Sheet - LFPR-F-002b Rev. 04Dokument6 SeitenVendor Information Sheet - LFPR-F-002b Rev. 04Chelsea EsparagozaNoch keine Bewertungen
- 11-03 TB Value Chains and BPs - WolfDokument3 Seiten11-03 TB Value Chains and BPs - WolfPrakash PandeyNoch keine Bewertungen
- Retailing in IndiaDokument11 SeitenRetailing in IndiaVinod MalkarNoch keine Bewertungen
- Hdfs Default XML ParametersDokument14 SeitenHdfs Default XML ParametersVinod BihalNoch keine Bewertungen
- Powerpoint Speaker NotesDokument4 SeitenPowerpoint Speaker Notesapi-273554555Noch keine Bewertungen
- Online Extra: "Economists Suffer From Physics Envy"Dokument2 SeitenOnline Extra: "Economists Suffer From Physics Envy"Bisto MasiloNoch keine Bewertungen
- Rockaway Times 11818Dokument40 SeitenRockaway Times 11818Peter J. MahonNoch keine Bewertungen
- Tetralogy of FallotDokument8 SeitenTetralogy of FallotHillary Faye FernandezNoch keine Bewertungen
- Psychological Contract Rousseau PDFDokument9 SeitenPsychological Contract Rousseau PDFSandy KhanNoch keine Bewertungen
- C C C C: "P P P P PDokument25 SeitenC C C C: "P P P P PShalu Dua KatyalNoch keine Bewertungen
- MASONRYDokument8 SeitenMASONRYJowelyn MaderalNoch keine Bewertungen
- Corrosion Fatigue Phenomena Learned From Failure AnalysisDokument10 SeitenCorrosion Fatigue Phenomena Learned From Failure AnalysisDavid Jose Velandia MunozNoch keine Bewertungen
- Strucure Design and Multi - Objective Optimization of A Novel NPR Bumber SystemDokument19 SeitenStrucure Design and Multi - Objective Optimization of A Novel NPR Bumber System施元Noch keine Bewertungen
- Report Card Grade 1 2Dokument3 SeitenReport Card Grade 1 2Mely DelacruzNoch keine Bewertungen
- Dynamics of Machinery PDFDokument18 SeitenDynamics of Machinery PDFThomas VictorNoch keine Bewertungen
- Working With Difficult People Online WorksheetDokument4 SeitenWorking With Difficult People Online WorksheetHugh Fox IIINoch keine Bewertungen
- Evaluation TemplateDokument3 SeitenEvaluation Templateapi-308795752Noch keine Bewertungen