Beruflich Dokumente
Kultur Dokumente
Basalioma
Hochgeladen von
ditanovrianaOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Basalioma
Hochgeladen von
ditanovrianaCopyright:
Verfügbare Formate
Spontaneous regression
M Gupta et al
262
Manuchehri K, Loo A, Ramchandani M, Kirby GR. Acute
suprachoroidal haemorrhage in a patient treated with
streptokinase for myocardial infarction. Eye 1999; 13(3):
685686.
Alexandrakis G, Chaudhry NA, Liggett PE, Weitzman M.
Spontaneous suprachoroidal haemorrhage in
age-related macular degeneration presenting as
angle-closure glaucoma. Retina 1998; 18(5):
485486.
T Hammam and C Madhavan
Princess Margaret Hospital
Okus Road
Swindon SN1 4JU, UK
Figure 2
vessel wall rupture by an apparently excessive pressure
gradient across the vessel wall.3
A spontaneous suprachoroidal haemorrhage can result
in angle closure glaucoma and corneal oedema
secondary to forward displacement of the irislens
diaphragm.5 In our case the angle was open at the time of
examination.
Typically, patients experience a sudden onset of severe
ocular pain with a subsequent loss of vision. Headache,
nausea and vomiting may also accompany the ocular
pain.1
Suprachoroidal haemorrhage after valsalva manoeuvre
has been reported in patients either on systemic anticoagulants, treated with streptokinase or in eyes with
previous ocular surgery (scleral buckle).25
To our knowledge, this is the first reported case of
spontaneous choroidal haemorrhage in an individual
who is not on any anticoagulants or has had no past
history of ocular surgery.
References
1
2
Eye
Chu TG, Green RL. Suprachoroidal haemorrhage. Surv
Ophthalmol 1999; 43(6): 471486.
van Meur JC, van den Bosch WA. Suprachoroidal
haemorrhage following a valsalva manoeuvre. Arch
Ophthalmol 1993; 111: 10251026.
Meyers SM, Foster RE. Choroidal haemorrhage after
valsalvas manoeuvre in eyes with a previous scleral buckle.
Ophthalm Surg 1995; 26(4): 216217.
Correspondence: T Hamman
Tennent Institute of Ophthalmology
Gartnaval General Hospital
Great Western Road
Glasgow G4 0SF, UK
Tel: 0141 344 1109
Fax: 0141 211 2054
E-mail: tarek12uk@yahoo.co.uk
Sir,
Complete spontaneous regression of a basal cell
carcinoma
Eye (2003) 17, 262263. doi:10.1038/sj.eye.6700303
A case of spontaneous regression of a basal cell
carcinoma is presented.
Case report
A 76-year-old man under review for glaucoma in the
right eye presented to the eye clinic with a large
lesion on the medial aspect of the right lower lid in
January 1997. The lesion had a maximum horizontal
diameter of 11 mm and a vertical diameter of 12 mm. It
had a central ulcerated crater with a raised pearly
rolled edge (Figure 1a). Based on the location and
clinical appearance of the lesion, a provisional diagnosis
of basal cell carcinoma (nodular) was made and an
incisional biopsy was performed. Histology was
consistent with an adenoid basal cell carcinoma. The
patient was put on the waiting list for excision of the
basal cell carcinoma with a skin graft in February 1997.
When reviewed in March 1997 the lesion had become
smaller in size, so surgery was postponed. On
subsequent follow-up in June 1997, it had disappeared
completely (Figure 1b). The patient has been under
follow-up for 4 years with no evidence of recurrence of
the basal cell carcinoma.
Allergic reaction to hyaluronidase
HS Ahluwalia et al
263
T lymphocytes through the release of cytokines6,7 has
been postulated to be the causative mechanism. Partial
regression of basal cell carcinomas has been reported in
about 50% of skin lesion;5 however, a complete
regression of the lesion as in the present instance has, to
the best of our knowledge, never been reported in
ophthalmic literature.
References
1
7
Figure 1 (a) The basal cell carcinoma on the lower lid as seen
on presentation in January 1997. (b) Complete spontaneous
regression of the basal cell carcinoma in July 1997.
Discussion
Basal cell carcinoma (rodent ulcer), the most common
tumour affecting the eyelids, is responsible for
considerable morbidity owing to its locally invasive
nature.1 Arising from the basal layer of the epidermis, it
is responsible for 8590% of lid malignancies, two-thirds
of which are seen in the lower lid.1,2
Diagnosis is made on the clinical appearance and
confirmed by histology, the adenoid and metatypical
types being the most common differentiated forms.3 The
usual course of the disease is a gradual enlargement of
the lesion with underlying tissue destruction
necessitating treatment. Treatment options include
cryotherapy, radiation, chemotherapy, laser ablation and
electrodessication, but surgical excision is the most
widely accepted treatment of choice.4
Regression of epithelial skin tumours like
keratoacanthoma, familial self-healing epithelioma,
melanoma and basal cell carcinoma has been reported in
dermatology.5,6 An immune response mediated by CD4+
Marco CE, Waltz K. Basal cell carcinoma of the eyelid
and periocular skin. Survey Ophthalmol 1993; 38:
169192.
Cotsarelis G, Cheng S, Dong D. Existence of slow cycling
limbal epithelial basal cells that can be preferentially
stimulated to proliferate: implications on epithelial stem
cells. Cell 1989; 57: 201209.
Borel DM. Cutaneous basosquamous carcinoma. Review
of literature and report of 35 cases. Arch Pathol 1973; 95:
293297.
Warren RC, Nerad JA, Carter KD. Punch biopsy technique
for the ophthalmologist. Arch Ophthalmol 1990; 108:
778779.
Barnetson RS, Halliday GM. Regression in skin tumors: a
common phenomenon. Australas J Dermatol 1997; 38:
563565.
Halliday GM, Patel A, Hunt MJ et al. Spontaneous
regression of human melanoma/nonmelanoma skin
cancer: association with infiltrating CD4+ T cells. World J
Surg 1995; 19(3): 352358.
Wong DA, Bishop GA, Lowes MA et al. Cytokine
profiles in spontaneously regressing basal cell
carcinomas. Br J Dermatol 2000; 143(1): 9198.
M Gupta, P Puri, A Kamal and ME Nelson
Department of Ophthalmology
Royal Hallamshire Hospital
Glossop Road
Sheffield S10 2JF, UK
Correspondence: M Gupta
Tel: 07786 893 563
Fax: 0114 271 3747
E-mail: mohiteye@yahoo.co.uk
Sir,
Delayed allergic reaction to hyaluronidase: a rare
sequel to cataract surgery
Eye (2003) 17, 263266. doi:10.1038/sj.eye.6700243
Peribulbar anaesthesia using lignocaine or bupivicaine is
frequently used in ophthalmic surgery. Hyaluronidase is
often used as an adjunct to aid dispersal of these
agents.14 We report a case of orbital inflammation
secondary to delayed postoperative hyaluronidase
allergy leading to visual loss.
Eye
Das könnte Ihnen auch gefallen
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Effect of Nasal Obstruction Surgery On Middle Ear VentilationDokument5 SeitenEffect of Nasal Obstruction Surgery On Middle Ear VentilationditanovrianaNoch keine Bewertungen
- Early Syphilis: Serological Treatment Response To Doxycycline/tetracycline Versus Benzathine PenicillinDokument5 SeitenEarly Syphilis: Serological Treatment Response To Doxycycline/tetracycline Versus Benzathine PenicillinditanovrianaNoch keine Bewertungen
- Forensic Pregnancy Diagnostics With Placental mRNA Markers: Original ArticleDokument5 SeitenForensic Pregnancy Diagnostics With Placental mRNA Markers: Original ArticleditanovrianaNoch keine Bewertungen
- Forensic Stomatological Identification of A MurdererDokument5 SeitenForensic Stomatological Identification of A MurdererditanovrianaNoch keine Bewertungen
- Sex Determination From Metacarpal and PhalangDokument8 SeitenSex Determination From Metacarpal and PhalangditanovrianaNoch keine Bewertungen
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- BSBHRM405 Support Recruitment, Selection and Induction of Staff KM2Dokument17 SeitenBSBHRM405 Support Recruitment, Selection and Induction of Staff KM2cplerkNoch keine Bewertungen
- Commercial Private Equity Announces A Three-Level Loan Program and Customized Financing Options, Helping Clients Close Commercial Real Estate Purchases in A Few DaysDokument4 SeitenCommercial Private Equity Announces A Three-Level Loan Program and Customized Financing Options, Helping Clients Close Commercial Real Estate Purchases in A Few DaysPR.comNoch keine Bewertungen
- Packing List Night at Starlodge Adventure SuitesDokument2 SeitenPacking List Night at Starlodge Adventure SuitesArturo PerezNoch keine Bewertungen
- 6401 1 NewDokument18 Seiten6401 1 NewbeeshortNoch keine Bewertungen
- Thomas HobbesDokument3 SeitenThomas HobbesatlizanNoch keine Bewertungen
- Pda Teachers GuideDokument2 SeitenPda Teachers Guidepeasyeasy100% (2)
- A Practical Guide To Transfer Pricing Policy Design and ImplementationDokument11 SeitenA Practical Guide To Transfer Pricing Policy Design and ImplementationQiujun LiNoch keine Bewertungen
- Lindenberg-Anlagen GMBH: Stromerzeugungs-Und Pumpenanlagen SchaltanlagenDokument10 SeitenLindenberg-Anlagen GMBH: Stromerzeugungs-Und Pumpenanlagen SchaltanlagenБогдан Кендзер100% (1)
- Notice: Grant and Cooperative Agreement Awards: Public Housing Neighborhood Networks ProgramDokument3 SeitenNotice: Grant and Cooperative Agreement Awards: Public Housing Neighborhood Networks ProgramJustia.comNoch keine Bewertungen
- Financial Performance Report General Tyres and Rubber Company-FinalDokument29 SeitenFinancial Performance Report General Tyres and Rubber Company-FinalKabeer QureshiNoch keine Bewertungen
- Prof. Monzer KahfDokument15 SeitenProf. Monzer KahfAbdulNoch keine Bewertungen
- Ulster Cycle - WikipediaDokument8 SeitenUlster Cycle - WikipediazentropiaNoch keine Bewertungen
- National Rural Employment Guarantee Act, 2005Dokument17 SeitenNational Rural Employment Guarantee Act, 2005praharshithaNoch keine Bewertungen
- 2 Lista Total de Soportados 14-12-2022Dokument758 Seiten2 Lista Total de Soportados 14-12-2022Emanuel EspindolaNoch keine Bewertungen
- Pasahol-Bsa1-Rizal AssignmentDokument4 SeitenPasahol-Bsa1-Rizal AssignmentAngel PasaholNoch keine Bewertungen
- Queen of Hearts Rules - FinalDokument3 SeitenQueen of Hearts Rules - FinalAudrey ErwinNoch keine Bewertungen
- MGT 601-Smes Management MCQ For Final Term Preparation: ProductionDokument80 SeitenMGT 601-Smes Management MCQ For Final Term Preparation: ProductionSajidmehsudNoch keine Bewertungen
- Executive SummaryDokument3 SeitenExecutive SummarySofia ArissaNoch keine Bewertungen
- Tesmec Catalogue TmeDokument208 SeitenTesmec Catalogue TmeDidier solanoNoch keine Bewertungen
- Phylogenetic Tree: GlossaryDokument7 SeitenPhylogenetic Tree: GlossarySab ka bada FanNoch keine Bewertungen
- Durst Caldera: Application GuideDokument70 SeitenDurst Caldera: Application GuideClaudio BasconiNoch keine Bewertungen
- Kutune ShirkaDokument11 SeitenKutune ShirkaAnonymous CabWGmQwNoch keine Bewertungen
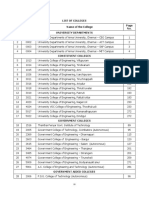
- TNEA Participating College - Cut Out 2017Dokument18 SeitenTNEA Participating College - Cut Out 2017Ajith KumarNoch keine Bewertungen
- Cryptography Practical 1Dokument41 SeitenCryptography Practical 1Harsha GangwaniNoch keine Bewertungen
- Damodaram Sanjivayya National Law University VisakhapatnamDokument6 SeitenDamodaram Sanjivayya National Law University VisakhapatnamSuvedhya ReddyNoch keine Bewertungen
- German Lesson 1Dokument7 SeitenGerman Lesson 1itsme_ayuuNoch keine Bewertungen
- Seangio Vs ReyesDokument2 SeitenSeangio Vs Reyespja_14Noch keine Bewertungen
- Best Interior Architects in Kolkata PDF DownloadDokument1 SeiteBest Interior Architects in Kolkata PDF DownloadArsh KrishNoch keine Bewertungen
- Reflection On An American ElegyDokument2 SeitenReflection On An American ElegyacmyslNoch keine Bewertungen
- 1b SPC PL Metomotyl 10 MG Chew Tab Final CleanDokument16 Seiten1b SPC PL Metomotyl 10 MG Chew Tab Final CleanPhuong Anh BuiNoch keine Bewertungen