Beruflich Dokumente
Kultur Dokumente
1 MacDougall - Wright ICFCY and GAS 2009
Hochgeladen von
ec16043Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
1 MacDougall - Wright ICFCY and GAS 2009
Hochgeladen von
ec16043Copyright:
Verfügbare Formate
Disability and Rehabilitation, 2009; 31(16): 13621372
REHABILITATION IN PRACTICE
The ICF-CY and Goal Attainment Scaling: Benefits of their combined
use for pediatric practice
JANETTE MCDOUGALL1 & VIRGINIA WRIGHT2
1
Research Program, Thames Valley Childrens Centre, London, Ontario, Canada and 2Research Program, Bloorview Research
Institute, Toronto, Ontario, Canada
Downloaded By: [University of Western Ontario] At: 19:51 7 July 2009
Accepted October 2008
Abstract
Purpose. There is much heterogeneity and disconnect in the approaches used by service providers to conduct needs
assessments, set goals and evaluate outcomes for clients receiving pediatric rehabilitation services. The purpose of this article
is to describe how the International Classification of Functioning, Disability and Health-Child and Youth (ICF-CY) can be
used in combination with Goal Attainment Scaling (GAS), an individualised measure of change, to connect the various
phases of the therapeutic process to provide consistent clinical care that is family-centred, collaborative, well directed and
accountable.
Method. A brief description of both the ICF-CY and GAS as they pertain to pediatric rehabilitation is provided as
background. An explanation is given of how the ICF-CY offers a framework through which clients, families and service
providers can together identify the areas of clients needs. In addition, the article discusses how the use of GAS facilitates
translation of clients identified needs into distinct, measurable goals set collaboratively by clients, their families and service
providers. Examples of integrated GAS goals set for the various components of the ICF-CY are provided. The utility of GAS
as a measure of clinical outcomes for individual clients is also discussed.
Conclusions. Used in combination, the ICF-CY and GAS can serve to coordinate, simplify and standardise assessment and
outcome evaluation practices for individual clients receiving pediatric rehabilitation services.
Keywords: ICF, ICF-CY, goal attainment scaling, children, rehabilitation, disability
Introduction
Goal setting has been described as the identification
of and agreement on a target among a client, his/her
family and service provider(s) followed by working
towards the target over a specific period of time [1].
The focus of rehabilitation has recently broadened to
promote enhanced social participation, in addition to
encouraging improved physical function and better
performance in activities of daily living [2]. The
importance of improving environmental supports to
enhance client functioning has also been recently
recognised. At any one point in time, a client may
have needs that require setting goals for change
across diverse aspects of functioning, as well as for
modifications to the environment. Unfortunately,
needs are often assessed and goals set without an
overarching frame of reference that can help clients
and service providers: (a) to identify the specific
aspects of individual functioning and the environmental factors that a clients goals should target for
change, and; (b) to understand how goals are
meaningful and interrelated within the overall context of the clients life and long-term development.
Furthermore, goals are often loosely set and broadly
defined, meaning that change cannot be accurately
or sensitively measured.
Clinical observation, the use of standardised
measures, and parent, client, teacher or other service
provider reports/interviews are among the most
common approaches used by rehabilitation service
providers of various disciplines (i.e. occupational
therapists, physical therapists, speech language
pathologists, social workers, recreational therapists,
Correspondence: Janette McDougall, Research Program, Thames Valley Childrens Centre, 779 Base Line Road East, London, Ontario, N6C 5Y6 Canada.
E-mail: janettem@tvcc.on.ca
ISSN 0963-8288 print/ISSN 1464-5165 online 2009 Informa UK Ltd.
DOI: 10.1080/09638280802572973
Downloaded By: [University of Western Ontario] At: 19:51 7 July 2009
The ICF-CY and GAS
behavioural therapists, nurses and others) for evaluating change in clients goal-based outcomes [3].
Both clinical observation, particularly by an expert
service provider, and reports/interviews may be quite
insightful and provide useful information for both
needs assessment and estimating change in childrens goals [4]. However, for accountability purposes, these approaches may need to be
supplemented with the use of goal setting and rating
techniques that can provide sound measurement,
and efficient documentation of client outcomes.
Standardised measures may be used to assess a
client at intake and to measure change in the clients
functional goals following service delivery. However,
standardised measures typically focus on selected
aspects of health and frequently do not include items
that directly reflect a clients unique needs and goals.
In such instances, the instrument will not be an
overly sensitive measure of change for the clients
goals. Moreover, service providers often report
modifying standardised measures to obtain an
accurate appraisal of the clients distinct situation
[5]. Unfortunately, modifying a standardised test can
seriously affect the psychometric properties of the
instrument [5]. Another issue with using standardised measures to evaluate change in clients goals is
that many are discriminative tools designed to
measure status at a single point in time and have
not been validated with respect to their ability to be
responsive to clinically important change [3,6].
In addition, up until recently few measures have
been available to assess a clients social participation
[7].
Studies have shown that, although families value
the types of functional changes typically reflected in
standardised measures, they place more value on
aspects of functioning that are not readily captured
by these types of measures, such as social participation [8,9]. In addition, standardised measures, in
general, do not facilitate a process whereby clients,
families and multiple service providers can work
collaboratively to set and evaluate childrens progress
on their goals. Research suggests that enhanced
collaboration among service providers and families
leads to positive service provider and client outcomes [10].
The purpose of this article is to describe how the
International classification of functioning, disability
and health-child and youth version (ICF-CY) [11]
can be employed by service providers in pediatric
rehabilitation practice to help clients and families
identify the needs related to all aspects of child
functioning and the environment. In addition, this
article will explain how this needs assessment process
can facilitate the collaborative setting of measurable,
individualised, functional goals using Goal Attainment Scaling (GAS), thus providing a quantifiable,
1363
reliable and valid assessment of change in individual
client outcomes following service delivery. The
article will also make clear why GAS is an ideal
individualised measurement approach to use with the
ICF-CY. Descriptions of the ICF-CY and GAS and
their utility with respect to collaborative service
delivery in pediatric rehabilitation practice are
provided below as background to each.
The ICF-CY
Published in 2001, the ICF [12] has been accepted
as the International standard for conceptualising
health and disability of people and populations and
for coding and collecting functional data [13]. It also
provides a system for coding and documenting the
impact of the social and physical environment on
human functioning. The ICF-CY, published in
October 2007 is based on the ICF, but is designed
specifically for use with children and youth and
allows more developmental aspects of functioning to
be coded. In addition, it focusses greater attention on
learning and child-specific environmental factors
[14]. The ICF and the ICF-CY classification systems
are designed for use with the long-standing international classification of diseases and related health
problems, tenth revision (ICD-10) [15] to provide a
comprehensive picture of the health of people and
populations [12]. Table I provides a list of the
chapters or domains of the ICF and the ICF-CY
and their level-one codes that are the foundation
for the proposed link with goal setting. The ICF
and ICF-CY also include more detailed codes at
levels two through four that can be used for
identifying needs and setting goals of greater
specificity.
In addition to providing classification systems, the
ICF and ICF-CY share a conceptual framework for
understanding functioning and disability that is
based on a biopsychosocial perspective of health. In
this framework, functioning is an umbrella term that
encompasses all body functions, activities and
participation. Disability is an umbrella term for
impairments, activity limitations and participation
restrictions. Impairments are defined as problems
in body function or structure; activity limitations
are difficulties a person may have in carrying out
daily activities; and participation restrictions are
problems a person may experience when involved in
life or social situations. A persons functioning and
disability, including a persons participation in life,
are depicted as arising from the interaction among
health conditions and environmental (e.g. air quality,
peer relationships, service availability) and personal
(e.g. age, gender, lifestyle, etc.) factors [12] (see
Figure 1).
1364
J. McDougall & V. Wright
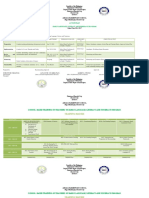
Table I. List of chapters in the ICF and ICF-CY and their levelone codes [13].
Body functions and structures
b1
b2
b3
b4
Downloaded By: [University of Western Ontario] At: 19:51 7 July 2009
b5
b6
b7
b8
s1
s2
s3
s4
s5
s6
s7
s8
Mental functions
Sensory functions and pain
Voice and speech functions
Functions of the cardiovascular, hematological, immunological and respiratory systems
Functions of the digestive, metabolic and endocrine systems
Genitourinary and reproductive functions
Neuormusculoskeletal and movement-related functions
Functions of the skin and related structures
Structures of the nervous system
Eye, ear and related structures
Voice and speech related structures
Cardiovascular, immunological and respiratory related
structures
Digestive, metabolic and endocrine related structures
Genitourinary and reproductive related structures
Structures related to movement
Skin and related structures
Activity and participation
d1
d2
d3
d4
d5
d6
d7
d8
d9
Learning and applying knowledge
General tasks and demands
Communication
Mobility
Self-care
Domestic life
Interpersonal relationships
Major life areas
Community, social and civic life
Natural environment and human-made changes to environment
e1
e2
e3
e4
e5
Products and technology
Natural environment
Support and relationships
Attitudes
Services, systems and policies
The ICF and ICF-CY classification systems and
shared conceptual framework are intended for use
within and across multiple sectors, such as health
promotion, rehabilitation, education, insurance, policy and statistics [16]. Within each sector, the ICF
and ICF-CY can be used for multiple purposes in
clinical (e.g. needs assessment), research (e.g. outcome measurement) and statistical areas (e.g. data
collection) [12]. However, neither the ICF nor the
ICF-CY operationalise the dimensions of disability,
that is they are not in and of themselves outcome
measures. Critical foundational work is being done
to assess the extent to which current standardised
measures capture the various domains of the ICF
[1721] and the ICF-CY [22]. In tandem with this is
the development and validation of suitable measures
of outcomes that will address measurement gaps
identified by the ICF [17]. There have also been
initiatives to assemble a selection of these measures
into a core set of outcome measures [23,24]. The
main contribution of the ICF and ICF-CY to such
efforts has been to provide an agenda of items that
should be taken into account for the development
and selection of outcome measures. Another significant use of the items included in the ICF has
been the development of core sets of items that can
be employed to generate individual profiles of
functioning for persons with various chronic conditions [25].
The extent of knowledge and practice-based
utilisation of the ICF by the providers of pediatric
rehabilitation services remains limited despite its
strong presence in the research literature [26].
However, service providers have indicated that the
ICF could be useful as a framework to guide their
practice and to facilitate collaboration with families
and other service providers. Indeed, a number of
publications have described how the ICF is starting
to be used as a framework for facilitating collaborative service delivery in pediatric rehabilitation practice [1,2734]. The ICF-CY is expected to be of
even greater relevance for this purpose than the
current ICF. Initial research has indicated that
participation and environmental factors are taken
into account more often when an assessment tool
based on the ICF-CY is used [32].
Goal Attainment Scaling
There are two main reasons for measuring outcomes
in the field of pediatric therapy: (a) to evaluate
outcomes for a specific child (to improve services to
that child); and (b) to determine the effectiveness of
a service or programme as a whole [6]. The
importance of measuring childrens progress towards
their individual functional goals is becoming increasingly recognised [35]. Individualised approaches can
demonstrate whether clients have achieved their
specific intervention goals. GAS is one of the most
widely used individualised approaches. GAS was first
developed in the 1960s by Kiresuk and Sherman [36]
and has been used to evaluate health services,
educational programmes and social services [37
39]. In the past 20 years, GAS has been used in
research work on the effects of pediatric therapy
services for children with developmental, physical
and communication needs [4050]. In those studies,
service providers of various rehabilitation disciplines
have employed GAS successfully. However, the use
of GAS for clinical purposes in pediatric practice
appears still to be limited [3,5].
GAS goals must meet six requirements. They need
to be: relevant, understandable, measurable, behavioural, attainable and time-related [51]. The GAS
procedure involves: (a) defining a unique set of goals
for each child, (b) specifying a range of possible
outcomes for each goal (on a scale recommended to
Downloaded By: [University of Western Ontario] At: 19:51 7 July 2009
The ICF-CY and GAS
1365
Figure 1. The World Health Organisations model of functioning and disability [13].
contain five levels, from 72 to 2) [52] and (c)
using the scale to evaluate the childs change after a
specified intervention period. A score of 72 on a
GAS scale (typically the childs baseline level)
represents improvement that is much less than the
expected level of attainment after intervention,
71 represents improvement that is less than the
expected level of attainment after intervention, 0
represents the expected (targeted) level of attainment
after intervention and 1 and 2 represent levels of
attainment that exceed expectations but represent
outcomes that the child is thought to be capable of
achieving under extremely favourable conditions.
The aim is to have clinically equal intervals between
all scale levels.
Improvement should be measured using only one
variable of change per scale, keeping other variables
constant. If, in doing so, the goal does not remain
clinically meaningful, two (or more) variables could
change within in a single scale, provided that
improvement is not expected to occur simultaneously on these variables. For a complete description of how to write GAS goals for clients receiving
pediatric rehabilitation services, see King et al. [6].
Several key issues related to the psychometric
properties of GAS have been debated particularly
with respect to conducting programme evaluation
and research, where multivariate data analysis
techniques are used [35,53]. Although these issues
are less relevant when using GAS for clinical
purposes, a very brief discussion of its validity and
reliability follows. For a detailed discussion of using
GAS for programme evaluation purposes, see King
et al. [6], and for discussions of psychometric issues
related to GAS, see Cardillo and Smith [52,54],
Smith and Cardillo [55] and Tennant [53].
Pediatric studies provide considerable evidence of
no more than low to moderate concurrent validity
between GAS and standardised measures [6,35,48].
However, this may be advantageous when GAS is
used for clinical purposes, because GAS has been
indicated to be more sensitive to change than normreferenced measures [35]. The lack of a higher
order construct underlying GAS and the ordinal
level of measurement of GAS scales, have also been
identified as problematic [53]. Although the idiosyncratic nature of GAS may pose a threat to validity for
group comparisons, in clinical contexts, it offers an
opportunity to measure exactly what needs to be
measured [35]. Moreover, the original developers of
GAS argue that it is not the content of each specific
GAS scale that is comparable or the higher order
construct, but the perceived ability to change in a
particular domain [51]. It has been suggested that
building up item banks of goals (e.g. comparing
goals within components of the ICF), which can be
calibrated onto a unidimensional scale would allow
for an individualised yet generalisable and more
efficient approach when using GAS for group
comparisons [53].
Downloaded By: [University of Western Ontario] At: 19:51 7 July 2009
1366
J. McDougall & V. Wright
GAS has been criticised due to its potential for
bias [52]. Unintentional bias can occur in goal
scaling (e.g. goals are overly easy to attain) or in goal
rating (e.g. showing that a child make improvements
that are not in fact real). Reliability can be improved,
however, by comprehensive training of service
providers with respect to goal setting and rating,
adequate definitions of the levels of goal attainment
and the use of multiple raters [38]. When carefully
implemented, inter-rater reliability of GAS between
two independent service providers rating goals on the
same occasion can be very high (ICC 0.98) [6].
Some of the processes of clinical service delivery in
pediatric settings can naturally reduce the possibility
and extent of bias in goal scaling and rating. A
collaborative goal-setting model helps to ensure that
goal areas and levels are relevant and that ratings are
valid, because both are based on a consensus
involving several individuals who are knowledgeable
about the child and invested in helping the child to
achieve real gains [5658].
Although GAS can be a time-consuming procedure, with scale development requiring up to 45 min
per child [35,59], all articles included in a review of
GAS use in pediatric rehabilitation reported high
family and service provider satisfaction with the
procedure [35]. Considering its acceptable social
validity [60] and the clinical benefits described
above, it appears to be worth the additional time
and effort and may be associated with greater
efficiency of treatment by leading to a more
streamlined, focussed intervention approach.
The combined use of the ICF-CY and GAS
It is important to note that, although the extent of
knowledge and practice-based utilisation of the ICF
and ICF-CY by rehabilitation service providers is
limited, research indicates that the types of goals set
for clients reflect ICF and ICF-CY content [3,22].
That is goals are typically set for clients across all
components of the ICF/ICF-CY (i.e. impairments,
activity limitations and participation restrictions and
environmental factors). However, service providers
tend to focus on impairment-based goals while, as
stated earlier, clients and families are more interested
in achieving goals related to activity and participation
[61]. Indeed, client goals are significantly more often
impairment or activity based than participation based
[3]. Service providers report that, even though
participation is an important outcome, it is typically
not the area that they feel is going to be immediately
influenced by the treatment they are providing [3].
As initial research suggests [32], using a needs
assessment tool based on the ICF-CY may lead to
more participation and environmental-based goals
being set for clients. Collaborative needs assessment
and goal identification using the ICF-CY can
facilitate a dialogue among clients, families and
service providers that helps to merge the two
perspectives. Moreover, because goals at the impairment and activity limitation level tend to be short
term and discipline specific, participation and
environmental-based goals may also increase as
developmental, community-based approaches to
pediatric service delivery [62] and interprofessional
collaboration [10] exert a greater influence on daily
practice.
When an initial assessment is conducted, the
domains of the ICF-CY can act as a good starting
point to help clients and families collaborate to
identify functional concerns, and can also ensure all
aspects of an individuals life are effectively addressed, as appropriate [1,32]. Visual tools [1],
developmentally structured interviews [63] or abbreviated and modified checklists similar to the ICF
checklist [64] that include a core set of codes
appropriate for use in pediatric rehabilitation settings
[27] are formats that can be used to present the ICF/
ICF-CY classification system in a manner that will
allow clients needs to be identified efficiently yet
comprehensively. Recently, developmental core
sets for four age groups have been identified from
the ICF-CY that could be useful when conducting
needs assessments for children and youth with
disabilities [65]. Some authors have provided examples of how a specific intervention-based ICF
framework model could be developed with families
during needs assessment and goal identification to
help clarify discussions about modifiable factors and
outcome possibilities across ICF (or ICF-CY)
domains [34,66] (see Figure 2 for an example of an
intervention-based model).
The ICF encourages acceptance of variation and
difference in ability, and the setting of self-defined
goals that are accomplished in whatever way is best
for each individual [32]. Once the client and his/her
family, in collaboration with rehabilitation service
providers, have identified areas requiring intervention using the ICF-CY, GAS could then be used to
transform clients broad, self-defined goals into
distinct, measurable goals.
The ICF-CY and GAS are complementary to each
other in a number of ways. Like the ICF-CY, GAS
allows for difference in ability by facilitating the
setting of goals that are unique to an individual. Also,
like the ICF-CY, GAS facilitates the assessment of
childrens development over time. Moreover, GAS
can be adapted to any ICF-CY domain [60]. Indeed,
the use of GAS allows the integration of impairment,
activity, participation or environmental goals within
the same evaluation template [3]. Goals may be
written that target change in impairment, activity
Downloaded By: [University of Western Ontario] At: 19:51 7 July 2009
The ICF-CY and GAS
1367
Figure 2. Intervention-based ICF/ICF-CY framework model used to identify needs and set broad goals.
limitations or the environment as short-term goals
with change in participation as a longer-term goal
(see Table II). For example, rehabilitation service
providers (e.g. school liaison, social worker, clinician, etc.) may help a client meet the goal of
participating in school-related tasks and duties by
collaborating with the clients family and a school
team to ensure a support worker is appropriately in
place, and that the child is provided with the
necessary time to practice the functional activities
required to meet his/her participation goal.
In addition to setting short- and long-term goals
within the same evaluation template, a concurrent set
of goals could be written to permit the examination
of how changes in impairments, activity limitations
and participation restrictions are related at a given
point in time [66]. Moreover, a set of goals targeting
change in an individuals functioning and change in
the environment could be set with the same
intervention time line, and could help ascertain
how modifications to the environment impact on
child functional outcomes within that given time line
(see Table III). For example, providers of schoolbased rehabilitation services could help a client to
meet the participation goal of playing with classmates at recess by simultaneously working to
enhance the supportiveness of the social environment in the classroom for the client. This could be
done by providing information to classroom teachers
and students about disabilities, by organising classroom presentations that can help change attitudes
toward disabilities, by modelling appropriate behaviour for interacting with the client and by encouraging teachers to set up situations where the client can
come together with classmates more often (e.g.
creating learning centres that encourage interaction,
changing seating positions), all of which may
encourage child-initiated interactions at recess.
1368
J. McDougall & V. Wright
Table II. Example of goals written for different components of the ICF-CY across a time line (facilitating examination of how changes in
shorter-term goals related to the environment and activity limitations influence changes in longer-term goals related to participation).
Downloaded By: [University of Western Ontario] At: 19:51 7 July 2009
Goal attainment scaling goals
Targeted ICF-CY
goal areas
Goal 1: Support from health
professionals (e355)
Goal 2: Moving around using
equipment (d465)
Goal 3: School life and related activities
(d835)
ICF-CY Component
Environmental factors
Activity limitations
Participation restrictions
Time line
1 Month
2 Months
5 Months
Level of attainment
72 (much less than
expected)
71 (somewhat less
than expected)
0 (expected level
of outcome)
1 (somewhat more
than expected)
No arrangements made for support
worker
Support worker available to work
with client h per day
Support worker available to work
with client 1 h per day
Support worker available to work
with client 1 h per day
Cannot walk with walker in
school hallway
Can walk with walker 250 m in
school hallway in 8 min
Can walk with walker 250 m in
school hallway in 6 min
Can walk with walker 250 m in
school hallway in 4 min
2 (much more
than expected)
Support worker available to work
with client 2 h per day
Can walk with walker 250 m in
school hallway in 2 min
Does not participate in hall monitoring
duties with other students at recess
Participates in hall monitoring duties for
the time at recess once a week
Participates in hall monitoring duties for
the time at recess twice a week
Participates in hall monitoring duties for
the time at recess once a week and
for entire recess once a week
Participates in hall monitoring duties for
entire recess twice a week
Comments:
If attainment falls between scale levels, goal will be rated at lower level
Table III. Example of goals written for different components of the ICF-CY with same time line (facilitating examination of reciprocal
relationship between goals targeting change in the environment and goals targeting change in child functioning).
Goal attainment scaling goals
Targeted ICF-CY
goal areas
ICF-CY Component
Goal 1: Support and relationships with
peers (e325)
Environmental factors
Goal 2: Engagement in play (d880)
Time line
5 Months
5 Months
Level of attainment
72 (much less than
expected)
71 (somewhat less
than expected)
0 (expected level
of outcome)
1 (somewhat more
than expected)
2 (much more
than expected)
Classmates do not interact* at all with
client in the classroom
Classmates interact with client once or
twice a day in the classroom
Classmates interact with client 3 times a
day in the classroom
Classmates interact with client 4 times a
day in the classroom
Classmates interact with client 5 or more
times a day in the classroom
Does not participate in child-initiated playground activities
with classmates at recess
Participates in child-initiated playground activities with
classmates at recess for about of the time on a typical day
Participates in child-initiated playground activities with
classmates at recess for about of the time on a typical day
Participates in child-initiated playground activities with
classmates at recess for about 3=4 of the time on a typical day
Participates in child-initiated playground activities with
classmates for the full recess on a typical day
Comments:
Participation restrictions
*Interaction may include any typical classroom behaviour expected between students such as: working together
on an assignment, help with completing a task, spending free time together playing a board game, etc.
If attainment falls between scale levels, goal will be rated at lower level
In addition, it is possible within a single goal to
target a variable for change at both the individual
functional level and the level of the environment
(as mentioned, GAS only allows one variable of
change per scale level, but more than one variable
can change within an entire scale) [6] (see
Table IV). This allows goals for environmental
modification to be directly linked with goals of the
client and family for functional change in the child,
thereby facilitating practice that is holistic and
family-centred [3].
When setting goals, the 0 (expected level) and
the 72 level (often the baseline) of goal attainment
should be set initially with clients (where appropriate) and their families [6]. Input at this stage from
families with respect to the other three goal levels
would also be beneficial. Service providers could
then use their GAS training and clinical expertise to
The ICF-CY and GAS
1369
Table IV. Example of a single goal that includes two variables of change.
Downloaded By: [University of Western Ontario] At: 19:51 7 July 2009
Goal attainment scaling goals
Targeted ICF-CY goal areas
Goal 1: Learning to write (d145) with support from a health professional (e355)
ICF-CY Component
Activity limitations and environmental factors
Time line
6 Months
Level of attainment
72 (much less than expected)
71 (somewhat less than expected)
0 (expected level of outcome)
1 (somewhat more than expected)
2 (much more than expected)
Can
Can
Can
Can
Can
Comments:
If attainment falls between scale levels, goal will be rated at lower level
print 4 of 8 letters of first name with hands on assistance and verbal cueing
print 6 of 8 letters of first name with hands on assistance and verbal cueing
print 8 of 8 letters of first name with hands on assistance and verbal cueing
print 8 of 8 letters of first name with verbal cueing
print 8 of 8 letters of first name independently
complete the GAS scaling process. Peer review of the
scaling is also an option to enhance reliability and
validity [6]. Clients and families should then be
consulted before finalising the goal scaling. As stated,
for clinical purposes, goal rating at predetermined
review times should be undertaken as a collaborative
process between clients, families and service providers, facilitating reflection on the ongoing therapeutic process.
Some caveats
It should be made clear that it is not the authors
intention to suggest that a comprehensive ICF-CYbased initial assessment is required for all clients who
receive pediatric rehabilitation services. Often, clients are seen short term for a very specific issue (e.g.
minor speech or fine motor difficulties) that does not
necessitate an expansive ICF-CY-based assessment
at intake. In many of these cases, the evaluation
needs only to focus on the most relevant components
of the ICF-CY for that client. However, when it is
expected that a client with a complex condition will
have multiple service needs that require ongoing
intervention, a complete assessment using an ICFCY-based tool would be of great benefit.
Neither is it the authors intention to suggest that
the use of standardised measures in pediatric
rehabilitation practice should be abandoned. Indeed,
a toolbox of standardised tools should be seen as an
important part of client assessment for evaluation of
impairment and activity limitations, as these have
been found to be integral to the determination of
clients/families strengths and needs, and for setting
goals [3]. This toolbox should, whenever possible,
contain measures that have been designed for
evaluation of change [21]. Supplementation of
GAS with standardised measures that provide more
conventional estimates of post-treatment status is
also suggested to give a comprehensive assessment of
outcome, especially when evaluating outcomes for a
group of children [6,38]. For example, change at
the impairment level has been measured using a
standardised measure and then compared with
change at the participation level using GAS [67].
In addition, other individualised measures have their
own benefits for pediatric rehabilitation practice and
can provide information that differs in focus from
GAS. For example, the Canadian Occupational
Performance Measure (COPM) [68] can provide
information about a clients progress on goals in the
areas of self-care, productivity and leisure. The COPM
may be less time-consuming than GAS, and may be a
better choice when time efficiency is paramount and
clients goals fall within the three above-named areas.
GAS, however, provides complete flexibility for setting
any type of goal in any area of the ICF-CY and for
simultaneously assessing goals related to changes in
both the client and the environment.
Another option is to use components of the
COPM in combination with GAS. The COPM
provides an assessment of families satisfaction with
childrens goal attainment [3]. Used together, GAS
could provide quantifiable results on actual attainment of goals based on observable criteria
whereas the COPM could offer the clients/families
perspective on performance and its value (i.e.
satisfaction) [69].
Future considerations
In conclusion, considering the benefits, it is worth
the effort to use the ICF-CY together with GAS in
pediatric clinical practice. Given the newness of the
ICF (and ICF-CY), service providers may still lack
substantial knowledge of this framework and
classification system and few apply it in everyday
practice [26]. Therefore, pediatric centres may
first need to provide training to staff regarding the
ICF/ICF-CY. Additional information about and
Downloaded By: [University of Western Ontario] At: 19:51 7 July 2009
1370
J. McDougall & V. Wright
training materials for the ICF can be accessed from
the ICFs home page [11]. Also, recent work is
available that describes three systematic programmes
for teaching service providers to use the ICF, along
with efforts to evaluate their effectiveness [70].
As stated, research indicates that providers of
pediatric rehabilitation services rarely use validated,
individualised approaches such as GAS for clinical
purposes [3,5]. Because of the lack of general
knowledge about GAS as well as the importance of
conducting the GAS procedure accurately to reduce
bias, pediatric centres interested in using GAS will
need to provide GAS training to service providers.
Specific guidelines for GAS training within the
pediatric rehabilitation context can be found in King
et al. [6].
Finally, because both the use of an ICF-CY-based
assessment tool and GAS are the added steps to the
existing therapeutic process, it is important for
managers and administrators to support the restructuring of assessment and evaluation sessions to
permit the successful integration of these procedures
into everyday practice.
Acknowledgements
Dr. Wright is supported by a Career Development
Award (2007 to 2011) through the Canadian Child
health Clinician Scientist Program, a Canadian
Institutes of Health Research Strategic Training
Initiative.
References
1. Bornman J, Murphy J. Using the ICF in goal setting: clinical
applications using Talking Mats1. Disabil Rehabil Assist
Technol 2006;1:145154.
2. Sakzewski L, Boyd R, Ziviana J. Clinimetric properties of
participation measures for 5- to 13-year old children with
cerebral palsy: a systematic review. Dev Med Child Neurol
2007;49:232240.
3. Wright V. From clinical observation to outcome measurement. 2007. Electronic Citation. http://www.oacrs.com/
News/Conference2007/TA7ClinicalObservationToOutcome
Measurement.ppt. Last accessed April 2008.
4. King G, Currie M, Bartlett D, Gilpin M, Willoughby C,
Tucker MA, Strachan D, Baxter D. The development of
expertise in pediatric rehabilitation therapists: changes in
approach, self-knowledge, and use of enabling and customizing strategies. Dev Neurorehabil 2007;10:223240.
5. Hanna S, Russell D, Bartlett D, Kertoy M, Rosenbaum P,
Wynn K. Measurement practises in pediatric rehabilitation: a
survey of physical therapists, occupational therapists, and
speech-language pathologists in Ontario. Phys Occup Ther
Pediatr 2007;27:2542.
6. King G, McDougall J, Palisano R, Gritzan J, Tucker MA.
Goal attainment scaling: its use in evaluating pediatric therapy
programs. Phys Occup Ther Pediatr 1999;19:3152.
7. Wade D. Outcome measures for clinical rehabilitation trials:
impairment, function, quality of life, or value? Am J Phys Med
Rehabil 2003;82:S26S31.
8. Cohn E. Parent perspectives of occupational therapy using a
sensory integration approach. Am J Occup Ther 2001;55:
285294.
9. Cohn E, Miller L, Tickle-Degnen L. Parent hopes for therapy
outcomes: Children with sensory modulation disorders. Am J
Occup Ther 2000;54:3643.
10. Barrett J, Curran V, Glynn L, Godwin M. CHSRF Synthesis:
interprofessional collaboration and quality primary healthcare.
Ottawa, ON: Canadian Health Services Research Foundation;
2007.
11. World Health Organization. International classification of
functioning, disability and healthchild and youth version.
Geneva, Switzerland: World Health Organization; 2007.
12. World Health Organization. International classification of
functioning, disability and health. Geneva, Switzerland; 2001.
13. World Health Organization. International classification of
functioning, disability and health, Internet. Electronic Citation.
http://www.who.int/classifications/icf/site/onlinebrowser/../index.
cfm. Last accessed February 2008.
14. Lollar D, Simeonsson R. Diagnosis to function: classification
for children and youth. J Dev Behav Pediatr 2005;26:
323330.
15. World Health Organization. International statistical classification of diseases and related health problems, 10th revision,
Vol 1. Geneva, Switzerland: World Health Organization; 1992.
stun
16. Stucki G, Cieza A, Ewert T, Kostanjsek N, Chaterji S, U
T. Application of the International classification of functioning, disability and health (ICF) in clinical practice. Disabil
Rehabil 2002;24:281282.
17. McConachie H, Colver A, Forsyth R, Jarvis S, Parkinson K.
Participation of disabled children: how should it be characterized and measured? Disabil Rehabil 2006;28:11571164.
18. Cieza A, Brockow T, Ewert T, Amman E, Kolleritis B,
stun T, Stucki G. Linking health-status
Chatterji S, U
measurements to the International classification of functioning, disability and health. J Rehabil Med 2002;34:205210.
19. Cieza A, Stucki G. Content comparison of health-related
quality of life (HRQOL) instruments based on the International classification of functioning, disability and health (ICF).
Qual Life Res 2005;14:12251237.
20. Dijkers M, Whiteneck G, El-Jaroudi R. Measures of social
outcomes in disability research. Arch Phys Med Rehabil
2000;81:S63S77.
21. Salter K, Jutai J, Teasell R, Foley N, Bitensky J, Bailey M.
Issues for selection of outcome measures in stroke rehabilitation: ICF participation. Disabil Rehabil 2005;79:506528.
22. Nijhuis B, Reindeers-Messelink H, deBlecourt A, Ties J,
Boonstra A, Groothoff J, Nakken H, Postema K. Needs,
problems, and rehabilitation goals of young children with
cerebral palsy as formulated in the rehabilitation activities
profile for children. J Rehabil Med 2008;40:347354.
23. Demers L, Desrosiers J, Ska B, Wolfson C, Nikolova R,
Pervieux I, Auger C. Assembling a toolkit to measure geriatric
rehabilitation outcomes. Am J Phys Med Rehabil 2005;84:
460472.
24. Rentsch H, Bucher P, Nyffeler D, Wolf C, Hefti H, Fluri E,
Wenger U, Walti C, Boyer I. The implementation of the
International classification of functioning, disability and
health (ICF) in daily practice of neurorehabilitation: an
interdisciplinary project at the Kantonsspital of Lucerne,
Switzerland. Disabil Rehabil 2003;25:411421.
stun B, Chatterji S, Kostanjsek N, Stucji
25. Cieza A, Ewert T, U
G. Development of ICF core sets for patients with chronic
conditions. J Rehabil Med 2004;Suppl 44:911.
26. Farrell J, Anderson S, Hewitt K, Livingston M, Stewart D. A
survey of occupational therapists in Canada about their
knowledge and use of the ICF. Can J Occup Ther 2007;74:
S221S232.
Downloaded By: [University of Western Ontario] At: 19:51 7 July 2009
The ICF-CY and GAS
27. McDougall J, Horgan K, Baldwin P, Tucker MA. Employing
the International classification of functioning, disability, and
health (ICF) to enhance services for children and youth with
chronic physical health conditions and disabilities. Paediatr
Child Health 2008;13:173178.
28. Campbell W, Skarakis-Doyle E. School-aged children with
SLI: the ICF as a framework for collaborative service delivery.
J Commun Disord 2007;40:513535.
29. McLeod S, Bleile K. The ICF: a framework for setting goals
for children with speech impairment. Child Lang Teach Ther
2004;20:199219.
30. Darzins P, Fone S, Darzins S. The International
classification of functioning, disability, and health can help
structure and evaluate therapy. Aust Occup Ther J 2006;53:
127131.
31. Palisano R. A collaborative model of service delivery
for children with movement disorders: a framework for
evidence-based decision making. Phys Ther 2006;86:
12951305.
kesson E.
32. Raghavendra P, Bornman J, Granlund M, Bjorck-A
The World Health Organizations International classification
of functioning, disability and health: implications for clinical
and research practice in the field of augmentative and
alternative communication. Augment Altern Commun 2007;
23:349361.
33. Rosenbaum P, Stewart D. The World Health Organization
International classification of functioning, disability and
health: a model to guide clinical thinking, practice, and
research in the field of cerebral palsy. Semin Pediatr Neurol
2004;11:510.
34. Steiner W, Ryser L, Huber E, Uebelhart D, Aeschlimann A,
Stucki G. Use of the ICF as a clinical problem-solving tool in
physical therapy and rehabilitation medicine. Phys Ther
2002;82:10981107.
35. Steenbeek D, Ketelaar M, Galama K, Gorter J. Goal
attainment scaling in paediatric rehabilitation: a critical
review of the literature. Dev Med Child Neurol 2007;49:
550556.
36. Kiresuk T, Sherman R. Goal attainment scaling: a general
method for evaluating comprehensive community mental
health programs. J Community Ment Health 1968;4:
443453.
37. Cytrynbaum S, Ginath Y, Birdwell J, Brandt L. Goal
attainment scaling: a critical review. Eval Q 1974;3:540.
38. Kiresuk T, Smith A, Cardillo J. Goal attainment scaling:
applications, theory, and measurement. Hillsdale, New Jersey:
Lawrence Erlbaum Associates; 1994.
39. MacKay G, Somerville W, Lundie J. Reflections on goal
attainment scaling (GAS): cautionary notes and proposals for
development. Educ Res 1996;38:161172.
40. Palisano R, Haley S, Brown D. Goal attainment scaling as a
measure of change in infants with motor delays. Phys Ther
1992;72:432437.
41. Ashford S, Turner-Stokes L. Goal attainment for spasticity
management using botulinum toxin. Physiother Res Int
2006;11:2434.
42. Brown D, Effgen S, Palisano R. Performance following
ability-focused physical therapy intervention in individuals
with severely limited physical and cognitive abilities. Phys
Ther 1996;78:934947.
43. Cook A, Bentz B, Lynch C, Miller B. School-based use of a
robotic arm system by children with disabilities. IEEE Trans
Neural Syst Rehabil Eng 2005;13:452460.
44. Ekstrom L, Johansson E, Granat T, Carlsberg E. Functional
therapy for children with cerebral palsy: an ecological
approach. Dev Med Child Neurol 2005;47:613619.
45. King G, McDougall J, Tucker MA, Gritzan J, Malloy-Miller
T, Alambets P, Gregory K, Thomas K, Cunning D. An
46.
47.
48.
49.
50.
51.
52.
53.
54.
55.
56.
57.
58.
59.
60.
61.
62.
63.
1371
evaluation of functional, school-based therapy services for
children with special needs. Phys Occup Ther Pediatr 1999;
19:529.
King G, Tucker MA, Alambets P, Gritzan J, McDougall J,
Ogilvie A, Husted K, OGrady S, Malloy-Miller T, Brine M.
The evaluation of functional, school-based therapy services for
children with special needs: a feasibility study. Phys Occup
Ther Pediatr 1998;18:127.
Oren T, Ogletree B. Program evaluation in classrooms
for students with autism: student outcomes and program
processes. Focus Autism Dev Disabil 2000;15:170175.
Palisano R. Validity of goal attainment scaling with infants
with motor delays. Phys Ther 1993;73:651658.
Steenbeek D, Meester-Delver A, Becher J, Lankhorst G. The
effect of botulinum toxin type A treatment of the lower
extremity on the level of functional abilities in children with
cerebral palsy: evaluation with goal attainment scaling. Clin
Rehabil 2005;19:274282.
Stephens T, Haley S. Comparison of two methods for
determining change in motorically handicapped children.
Phys Occup Ther Pediatr 1991;11:117.
Ottenbacher K, Cusick A. Discriminative versus evaluative
assessment: some observations on goal attainment scaling. Am
J Occup Ther 1993;47:349354.
Cardillo J, Smith A. Psychometric issues. In: Kiresuk T,
Smith A, Cardillo J, editors. Goal attainment scaling:
applications, theory, and measurement. Hillsdale, NJ:
Lawrence Erlbaum Associates; 1994. pp 173212.
Tennant A. Goal attainment scaling: current methodological
challenges. Disabil Rehabil 2007;29:15831588.
Cardillo J, Smith A. Reliability of goal attainment scores.
In: Kiresuk T, Smith A, Cardillo J, editors. Goal attainment
scaling: applications, theory, and measurement. Hillsdale,
NJ: Lawrence Erlbaum Associates; 1994. pp 213242.
Smith A, Cardillo J. Perspectives on validity. In: Kiresuk T,
Smith A, Cardillo J, editors. Goal attainment scaling:
applications, theory, and measurement. Hillsdale, NJ:
Lawrence Erlbaum Associates; 1994. pp 243272.
Mitchell T, Cusick A. Evaluation of a client-centred paediatric
rehabilitation programme using goal attainment scaling. Aust
Occup Ther J 1998;45:717.
Clark M, Caudrey D. Evaluation of rehabilitation services:
the use of goal attainment scaling. Int Rehabil Med 1983;5:
4145.
Smith A. Introduction and overview. In: Kiresuk T, Smith A,
Cardillo J, editors. Goal attainment scaling: applications,
theory, and measurement. Hillsdale, NJ: Lawrence Erlbaum
Associates; 1994. pp 114.
Cusick A, McIntyre S, Novak I, Lannin N, Lowe K. A
comparison of goal attainment scaling and the Canadian
occupational performance measure for paediatric research.
Paediatr Rehabil 2006;9:149157.
Schlosser R. Goal attainment scaling as a clinical measurement technique in communication disorders: a critical review.
J Commun Disord 2003;37:217239.
Soberg H, Finsel A, Roise O, Bautz-Holtzer E. Identification and comparison of rehabilitation goals after multiple
injuries: an ICF analysis of the patients, physiotherapists,
and other allied professionals goals. J Rehabil Med 2008;
40:340346.
King G, Tucker MA, Baldwin P, LaPorta J. Bringing the life
needs model to life: implementing a service delivery model for
pediatric rehabilitation. Phys Occup Ther Pediatr 2006;26:
4370.
Kronk R, Ogonowski J, Rice C, Feldman H. Reliability in
assigning ICF codes to children with special health care needs
using a developmentally structured interview. Disabil Rehabil
2005;27:977983.
1372
J. McDougall & V. Wright
Downloaded By: [University of Western Ontario] At: 19:51 7 July 2009
64. World Health Organization. ICF checklist. Geneva, Switzerland; 2001.
65. Simeonsson R. ICF-CY next steps: developmental core sets.
Electronic Citation. http://apha.confex.com/alpha/134am/
techprogram/paper_130610.htm. Last accessed September
2008.
66. Wright V, Rosenbaum P, Goldsmith C, Law M, Fehlings D.
How do changes in body functions, activity, and participation
relate in children with cerebral palsy? Dev Med Child Neurol
2008;50:283289.
67. Mall V, Heinman F, Siebal A, Bertram C, Hafkemeyer U,
Wissel J, Berweck S, Haverkamp F, Nass G, Breitbach-Faller
N, Schulte-Mattler W, Korinthenberg R. Treatment of
adductor spasticity with BTX-A in children with CP: a
randomized, double-blind, placebo-controlled study. Dev
Med Child Neurol 2006;48:1013.
68. Law M, Baptiste S, McColl M, Opzoomer A, Polatajko H,
Pollack N. The Canadian occupational performance measure:
an outcome measure for occupational therapy. Can J Occup
Ther 1990;57:8287.
69. Trombly C, Radomski M, Trexel C, Burnett-Smith S.
Occupational therapy and achievement of self-identified goals
by adults with traumatic brain injury: Phase II. Am J Occup
Ther 2002;56:489498.
70. Reed G, Dilfer K, Bufka L, Scherer M, Kotze P,
Tshivhase M, Stark S. Three model curricula for teaching
clinicians to use the ICF. Disabil Rehabil 2008;30:
927941.
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5795)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1091)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Chapter - 13 - Cardiovascular - Responses - Exercise Physiology For Health Fitness and PerformanceDokument32 SeitenChapter - 13 - Cardiovascular - Responses - Exercise Physiology For Health Fitness and Performanceec16043Noch keine Bewertungen
- Adding A Post-Training FIFA 11+ Exercise Program To The Pre-Training FIFA 11+ Injury Prevention Program Reduces Injury Rates AmongDokument8 SeitenAdding A Post-Training FIFA 11+ Exercise Program To The Pre-Training FIFA 11+ Injury Prevention Program Reduces Injury Rates Amongec16043Noch keine Bewertungen
- Trigger Point FinderDokument160 SeitenTrigger Point Finderec16043Noch keine Bewertungen
- What Does Best Practice Care For Musculoskeletal Pain Look LikeDokument10 SeitenWhat Does Best Practice Care For Musculoskeletal Pain Look Likeec16043Noch keine Bewertungen
- A Current Review of An Unsolved PuzzleDokument3 SeitenA Current Review of An Unsolved Puzzleec16043Noch keine Bewertungen
- DR Shahin Pourgol - Osteopathy Vs Chiropractic Vs Physical Therapy Vs Massage TherapyDokument9 SeitenDR Shahin Pourgol - Osteopathy Vs Chiropractic Vs Physical Therapy Vs Massage Therapyec16043Noch keine Bewertungen
- 2010 Handbook Survey ResearchDokument51 Seiten2010 Handbook Survey Researchec16043Noch keine Bewertungen
- Why Don't Most Runners Get Knee Osteoar... (Med Sci Sports ExercDokument2 SeitenWhy Don't Most Runners Get Knee Osteoar... (Med Sci Sports Exercec16043Noch keine Bewertungen
- Writing Lesson Plan - ZOMNIADokument5 SeitenWriting Lesson Plan - ZOMNIAJenniferHamiltonNoch keine Bewertungen
- Metric System Lesson Plan 2015Dokument22 SeitenMetric System Lesson Plan 2015api-283334442Noch keine Bewertungen
- Epse 432 - Reflection PaperDokument5 SeitenEpse 432 - Reflection Paperapi-260661724Noch keine Bewertungen
- What Is Instructional System Design?Dokument2 SeitenWhat Is Instructional System Design?coy aslNoch keine Bewertungen
- Greek Gods Family Tree ChartDokument14 SeitenGreek Gods Family Tree ChartJohn Perseus LeeNoch keine Bewertungen
- Action Plan Early Language, Literacy and Numeracy Program: Abkasa Elementary SchoolDokument3 SeitenAction Plan Early Language, Literacy and Numeracy Program: Abkasa Elementary Schoolenimsay somarNoch keine Bewertungen
- The Real Filipino TimeDokument2 SeitenThe Real Filipino TimeMilxNoch keine Bewertungen
- V Interpretation Construction (ICON) Design ModelDokument23 SeitenV Interpretation Construction (ICON) Design ModelSakshi SadhanaNoch keine Bewertungen
- Presentation The Smart School in Malaysia'Dokument8 SeitenPresentation The Smart School in Malaysia'sha aprellNoch keine Bewertungen
- Grade 9 The Canadian Atlas Online - WeatherDokument9 SeitenGrade 9 The Canadian Atlas Online - Weathermcmvkfkfmr48gjNoch keine Bewertungen
- Precalculus PDFDokument28 SeitenPrecalculus PDFRosanna Lombres83% (6)
- MSTA 2003 Conference ProgDokument31 SeitenMSTA 2003 Conference ProgchaddorseyNoch keine Bewertungen
- Grammar - PET For SchoolsDokument10 SeitenGrammar - PET For SchoolsRuth100% (1)
- Lozanov and The Teaching TextDokument33 SeitenLozanov and The Teaching TextPhạm Thái Bảo NgọcNoch keine Bewertungen
- Percent Lesson PlanDokument1 SeitePercent Lesson Planapi-344760154Noch keine Bewertungen
- M7NS Ia 1Dokument6 SeitenM7NS Ia 1jennelyn malayno0% (1)
- Lesson PlanDokument2 SeitenLesson Planapi-237655947Noch keine Bewertungen
- HCM Course HandbookDokument22 SeitenHCM Course HandbookAlex ForryanNoch keine Bewertungen
- IQ and The Problem of Social AdjustmentDokument4 SeitenIQ and The Problem of Social AdjustmentCarlos ContrerasNoch keine Bewertungen
- Development Plan Rpms Sy 2018 2019Dokument8 SeitenDevelopment Plan Rpms Sy 2018 2019Gideon Salino Gasulas BunielNoch keine Bewertungen
- Beaumont Job Shadow All Interview Ty NoteDokument12 SeitenBeaumont Job Shadow All Interview Ty Noteapi-358423274Noch keine Bewertungen
- Developing An Invisible Message About Relative Acidities of Alcohols in The NaturDokument4 SeitenDeveloping An Invisible Message About Relative Acidities of Alcohols in The NaturDhiman BasuNoch keine Bewertungen
- Article On The Importance of Elementary EducationDokument3 SeitenArticle On The Importance of Elementary EducationNITISHSN100% (1)
- Terminal Report English Fair 2019Dokument8 SeitenTerminal Report English Fair 2019Brandy BitalanNoch keine Bewertungen
- CalculatinghalflifeDokument5 SeitenCalculatinghalflifeapi-256503273Noch keine Bewertungen
- Teaching Models Transmission TransactionDokument3 SeitenTeaching Models Transmission TransactionMark BorresNoch keine Bewertungen
- Locker GameDokument3 SeitenLocker GameYashmeeta SharmaNoch keine Bewertungen
- Week 32 Q4Dokument9 SeitenWeek 32 Q4Jacquelyn Buscano DumayhagNoch keine Bewertungen
- 2017 Fbms Tlac Strategies OverviewDokument2 Seiten2017 Fbms Tlac Strategies Overviewapi-332018399Noch keine Bewertungen
- Music of Mindoro DLLDokument2 SeitenMusic of Mindoro DLLkarla joy 05100% (1)