Beruflich Dokumente
Kultur Dokumente
Quiste Parauretral 2014 PDF
Hochgeladen von
AndresGómezOriginalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Quiste Parauretral 2014 PDF
Hochgeladen von
AndresGómezCopyright:
Verfügbare Formate
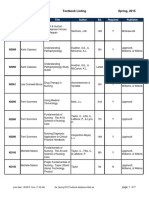
FEMALE UROLOGY
Paraurethral Cyst in Adult Women: Experience with 85 Cases
Farzaneh Sharifiaghdas, Azar Daneshpajooh,* Mahboubeh Mirzaei
Purpose: To present the clinical experience in the management of Skenes duct cysts (paraurethral cysts) in women.
Materials and Methods: A retrospective chart review of patients who have been undergone surgical treatment for
paraurethral cyst between 2002 and 2012 was performed. A total of 85 women were diagnosed with paraurethral
cyst over a 10-year period. The paraurethral cysts were detected at vaginal examination. Evaluations consisted of
urine analysis and culture and urinary tract ultrasound. The first 20 cases underwent cystourethroscopy as well. All
patients underwent surgical incision, drainage and marsupialization of the cyst. They were followed up for evidence
of any complications and recurrence.
Results: The mean follow up time was 5.5 years. Totally, 83 patients (97.6%) were cured. There were two cases of
recurrence which were treated with second surgical attempt.
Conclusion: Most paraurethral cysts in women may be diagnosed by history and physical examination alone. Simple
incision and marsupialization of the female paraurethral cyst was effective in more than 97% of our patients, without
recurrence.
Keywords: genital diseases; female; cysts; diagnosis; surgery; treatment outcome; urethral diseases.
INTRODUCTION
kenes glands, or paraurethral glands, are bilateral,
prostate homologues which are, located at the bottom of the distal urethra.(1,2) Their role is to secrete
a mucoid material, which helps to lubricate the urethral
meatus.(3) Obstruction of the ducts leads to the formation
of cyst.(1) A paraurethral cyst presents as a small, cystic
mass, just lateral or inferolateral to the urethral meatus.
Although the etiology of ductal obstruction is unknown
in neonates in adults, paraurethral cysts may be caused by
infection and inflammation.(1,4) Disorders of the Skenes
glands are rare during the prepubertal period. When a cyst
or abscess occurs, women in the third or fourth decade of
their life are most affected.(5) As Skenes ducts are embryologically derived from the urogenital sinus, these cysts
are lined by stratified squamous epithelium.(1)
Presenting symptoms include a palpable or visible mass,
pain, dyspareunia, a distorted voiding stream and vaginal discharge. Paraurethral cysts may be totally asymptomatic and are usually discovered during routine pelvic
examination.(6) The management of paraurethral cysts is
controversial.(7-9) In this article, we report our clinical experience with the diagnosis and management of paraurethral cysts.
MATERIALS AND METHODS
A retrospective chart review of patients who have been
undergone surgical treatment of paraurethral cyst in between 2002 and 2012 was performed. During a 10-year
period, more than 100 cases of paraurethral cysts have
been presented to our clinic, some of which were referred
by gynecologists or other urologists. The medical records
of all patients were reviewed. In most cases, diagnosis
was based on the patients history and physical examination. The lesions were assessed for location, mobility,
tenderness and consistency. Urine analysis, urine culture
and urinary tract ultrasound were also done in all patients.
Conservative treatments were unsuccessful in all patients.
According to the medical records, cystourethroscopy has
been performed in the first 20 cases to rule out urethral
diverticulum before surgery.
The cysts were inferolateral to the urethral meatus, displacing it to the other side (Figure 1). The patients were
operated as outpatient, under intravenous sedation or local anesthesia. At the start of the procedure, a urethral Foley catheter was inserted. Paraurethral cysts were incised,
drained (Figure 2) and marsupialized by four separated
4-0 chromic sutures (Figure 3). The anterior cyst wall
was sent for pathological examination and the posterior
cyst wall remained in situ (Figure 4). The Foley catheter
was removed at the end of the procedure.
Patients were examined postoperatively and then followed up annually for evidence of any recurrence. At
each clinical visit, they were asked questions regarding
any symptoms related to the cyst, voiding abnormality
and sexual function.
Urology and Nephrology Research Center, Labbafinejad Hospital, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
* Correspomdence: Urology and Nephrology Research Center, Labbafinejad Hospital, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
Tell: +98 21 22567222; Fax: +98 21 22567282. E-mail: azdaneshpajooh@yahoo.com.
Received April 2013 & Accepted July 2014
Female Urology 1896
Paraurethral Cyst in Women-Sharifiaghdas et al
Figure 1. The cyst has displaced urethral meatus to the other site.
Figure 2. Incision and drainage of paraurethral cyst.
RESULTS
DISCUSSION
Figure 3. Marsupialization of cyst.
Figure 4. Anterior cyst wall.
Only 85 out of 100 patients, who had marsupialization
of paraurethral cyst, were eligible to enroll in this study.
Mean age was 33.2 years (20-77 years). Of study subjects 76 were multiparous and nine were nulliparous. The
size of paraurethral cysts ranged from 0.5 to 4.5 cm. The
most common symptom was the sensation of a mass [63
(74%)]. Other symptoms were irritative urinary symptoms in 42 (49%), dyspareunia in 24 (28%) and obstructive voiding symptoms in 11 patients (13%). The mean
operation time was 10 min (range, 6-15 min). The operation was uneventful, with no postoperative complications. The patients were followed up for an average of 5.5
years (6 months to 9 years).
A total of 83 patients (97.6%) were cured, while remaining two developed recurrence of cysts after 2 and 4 years.
The second attempt of surgical marsupialization was successful and uneventful as well.
In all the specimens pathological examination revealed
benign cyst walls, lined with transitional or stratified
squamous epithelium (Figure 5). All cultures of the
drained mucous secretions were sterile.
Benign cystic lesions of the vagina are frequently encountered in gynecological and urological practice. True
cystic lesions of the vagina originate from vaginal tissues,
but lesions arising from the urethra and surrounding tissues may present as cystic lesions in the vagina as well.(1)
The differential diagnosis of vaginal wall masses are;
cysts with embryonic origin (Mullerian cysts, Gartners
duct cysts, Skenes duct cysts, Bartholins duct cysts,
vaginal adenosis, cysts of canal of Nuck), cysts with
urethral origin (urethral caruncle, urethral diverticulum),
epidermal inclusion cysts, endometriosis, ectopic ureterocele and pelvic organ prolapse. Skenes gland cysts
are very rare, the lesion typically arising secondary to the
obstruction of the duct. The cysts usually present as mass
lesions with associated pain, dyspareunia, dysuria and
distorted voiding stream.(3)
Blaivas and colleagues reported a diagnosis of paraurethral masses in 4% of their patient sample population, and
most masses were urethral diverticula (84%). Paraurethral
cysts were less commonly diagnosed, in 7% of patients.(10)
Cross and colleagues examined 140 asymptomatic wom-
Vol 11. No 05 Sept-Oct 2014 1897
Paraurethral Cyst in Women-Sharifiaghdas et al
meatus as compared with UD, which most commonly occur over the mid and proximal urethra.
After such large number of cases reported in our center,
we now believe that the preliminary diagnosis of paraurethral cysts can be easily made by physical examination in
most cases. Nevertheless, cystourethroscopy still remains
necessary to diagnosis. Also, our findings have no impact on the treatment planning. There was no need to perform a complete urological imaging palette (intravenous
urography, voiding cystourethrogram, and magnetic resonance imaging), and perhaps these evaluations should
be reserved for more complicated cysts, or cysts located
at the proximal or mid part of the urethra.
According to the literature, there is no consensus on the
treatment of paraurethral cysts. Conservative treatment
or needle aspiration is an appropriate option in the neonates,(4,14) while surgical excision is an option if the cyst
recurs or fails to resolve within a few months.(15) In adults,
several methods of management have been recommendFigure 5. Pathological characteristics of benign paraurethral cyst.
ed, including waiting for spontaneous rupture, needle
aspiration, marsupialization and complete excision of
(7-9,16)
Complete excision of the paraurethral cyst
en (mean age 41 years) by using endovaginal and perine- the cyst.
holds
the
risk of urethral injury or weakening the tiny
al sonography. A proportion of 2.9% of cases revealed
asymptomatic paraurethral cystic structures lying lateral muscle fibers around the urethra. Martin and colleagues
to the urethra, while the communication with the urethra reported the complete excision of the paraurethral cyst in
was not convincingly demonstrated in any of the cases. four patients. Two out of the four cases had urethral inju(11)
There are very few studies in the literature describ- ry, which was surgically repaired and the Foley catheter
(10)
ing the evaluation and management of paraurethral cysts remained in place for 1 week to preserve the urethra.
Lucioni
and
colleagues
reported
complete
periurethral
(7)
in adult women. We reported our first experience with
25 cases of paraurethral cysts during a 7 years interval, cyst excision in six patients, yielding an average recurbetween 1995 and 2001.(6) Therefore, this is the second rence free outcome with follow-up duration of 29 months.
24-48 hours
report from the same center with more patients and longer They also left in place the Foley catheter for
(17)
due
to
close
dissection
around
the
urethra.
Urinary infollow-up period. In our study, most of the patients were
multiparous (76 vs. 9), which indicates multiparity as a continence, urethro-vaginal fistula and urethral stricture
risk factor for paraurethral cyst. Most of the cases were in represent the other complications associated with the
the fourth and fifth decades of life. However, a few were complete excision of paraurethral cysts.
We treated all the patients by simple marsupialization of
in the post-menopausal period (4 patients, 4.7%).
the
cysts. All symptoms were completely resolved after
The position of the cyst is very important in physical exsurgery
and there was no complication such as hematoamination. The most common location of the Mullerian
cyst is along the anterolateral aspect of the vagina. Gart- ma, pain, infection, scar formation and dyspareunia. In
ners duct cysts are almost always located along the later- our first study, we reported simple marsupialization of
al wall of vagina. Bartholins duct cysts are in the lateral paraurethral cysts as a safe and effective procedure. In the
introitus, medial to the labia minora. Cysts of the canal of present study, we confirm the effectiveness of this proceNuck are generally found in the upper edge of the labia dure on a larger population and with longer follow-up.
majora or inguinal canal. The preferred region occurrence
vaginal adenosis is in the upper third of the vagina, pri- CONCLUSION
marily along the anterior wall. Epidermal inclusion cysts According to our knowledge, this is the largest case seare found at previous sites of trauma.
ries with the largest follow-up ever published concerning
The most important differential diagnosis of paraurethral female paraurethral cysts. We demonstrated that paraurecyst is the urethral diverticulum (UD). Most urethral di- thral cysts are benign lesions with excellent response to
verticula are located ventrally over the middle and prox- simple marsupialization procedure.
imal portions of the urethra, corresponding to the area of
the anterior vaginal wall 1 to 3 cm inside the introitus.(12) CONFLICT OF INTEREST
Patients with UD most commonly have anterior vaginal
wall tenderness, with or without a concomitant palpable None declared.
suburethral mass. Pressure on the mass may demonstrate
expressible purulent or bloody discharge from the UD or REFERENCES
meatus, and firmness of the area may indicate a divertic1. Eilber KS, Raz S. Benign cystic lesions of the
ular stone or neoplasm.(13) Skenes duct cysts are adjacent
vagina: a literature review. J Urol. 2003;170:717to the urethra and inferior or lateral to the urethral meatus.
22.
Differentiation from UD can often be made during phys2. Flamini MA, Barbeito CG, Gimeno EJ, Portianical examination, because these lesions are located rela
sky EL. Morphological characterization of
tively distally on the urethra, often distorting the urethral
Female Urology 1898
Paraurethral Cyst in Women-Sharifiaghdas et al
the female prostate (Skenes gland or paraure
thral gland) of Lagostomus maximus maximus.
Ann Anat. 2002;184:341-5.
3. Anderson SR. Benign vulvovaginal cysts. Diag
Histop. 2010;16:495-9.
4. Soyer T, Aydemir E, Atmaca E. Paraurethral
cysts in female newborns: role of maternal es
trogens. J Ped Adol Gynecol. 2007;20:249-51.
5. Nickles SW, Burgis JT, Menon S, Bacon JL.
Prepubertal Skenes abscess. J Ped Adol Gyne
col. 2009;22:e21-2.
6. SharifiAghdas F, Ghaderian N. Female
paraurethral cysts: experience of 25 cases. BJU
Int. 2004;93:353-6.
7. Isen K, Utku V, Atilgan I, Kutun Y. Experience
with the diagnosis and management of paraure
thral cysts in adult women. Can J Urol.
2008;15:4169-73.
8. Imamverdiev SB, Bakhyshov AA. Surgical
treatment of paraurethral cysts in women. Urol
(Moscow). 2009;2:39-41.
9. Yilmaz Y, Celik IH, Dizdar EA, et al. Paraure
thral cyst in two female newborns: Which ther
apy option?. Scand J Urol Nephrol. 2012;46:78 80.
10. Blaivas JG, Flisser AJ, Bleustein CB, Panagop
oulos G. Periurethral masses: etiology and diag
nosis in a large series of women. Obst Gyne
col. 2004;103:842-7.
11. Cross JJ, Fynes M, Berman L, Perera D. Prev
alence of cystic paraurethral structures in as
ymptomatic women at endovaginal and perineal
sonography. Clin Radiol. 2001;56:575-8.
12. Eric S, Rovner MD. Bladder and female urethral
diverticula. In: WEIN AJ, editor. Campbells
urology.10th ed. Philadelphia: Saunders; 2012.
p. 2262-89.
13. Hsiao KC, Kobashi KC. Urethral Diverticulum
and Fistula. In: Cardoz L, Staskin DR, editors.
Text Fem Urol Urogynecol. 3th ed. Lon
don: Informa healthcare; 2010. p. 971-90.
14. Fujimoto T, Suwa T, Ishii N, Kabe K. Paraure
thral cyst in female newborn: is surgery always
advocated? J Ped Surg. 2007;42:400-3.
15. Badalyan V, Burgula S, Schwartz RH. Congeni
tal paraurethral cysts in two newborn girls: dif
ferential diagnosis, management strategies,
and spontaneous resolution. J Ped Adol Gyne
col. 2012;25:e1-4.
16. Busto ML, Barguti I, Andraca AZ, Gmez
IR, Castan LB. Cyst of the skenes gland:
report of four cases and bibliographic review.
Arch Urol. 2010;63:238-42.
17. Lucioni A, Rapp DE, Gong EM, Fedunok P,
Bales GT. Diagnosis and management of peri
urethral cysts. Urol Int. 2007;78:121-5.
Vol 11. No 05 Sept-Oct 2014 1899
Das könnte Ihnen auch gefallen
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Pleural EffusionsDokument41 SeitenPleural Effusionssanjivdas100% (1)
- 2013 Fluconazole Resistant Candida Albicans.22Dokument8 Seiten2013 Fluconazole Resistant Candida Albicans.22Kala SuvarnaNoch keine Bewertungen
- Surgery CssDokument13 SeitenSurgery CssNaren ShanNoch keine Bewertungen
- ACOG Abnormal Uterine Bleeding DiagnosisDokument11 SeitenACOG Abnormal Uterine Bleeding DiagnosisJimmy Crack CornsNoch keine Bewertungen
- BFLSON Course Textbook ListingDokument7 SeitenBFLSON Course Textbook ListingWina ViqaNoch keine Bewertungen
- Narayana Hrudayalaya Cardiac Hospital Case Study LessonsDokument11 SeitenNarayana Hrudayalaya Cardiac Hospital Case Study LessonsSuhaib KhanNoch keine Bewertungen
- Presentation Syntax Score TCT 2008 PDFDokument33 SeitenPresentation Syntax Score TCT 2008 PDFElla MihNoch keine Bewertungen
- 10 1097@aog 0000000000001708Dokument20 Seiten10 1097@aog 0000000000001708oodarkfireooNoch keine Bewertungen
- Thesis T3003 PDFDokument99 SeitenThesis T3003 PDFNor HidayahNoch keine Bewertungen
- MCQDokument6 SeitenMCQalirbidiNoch keine Bewertungen
- Nle Exam SamplesDokument6 SeitenNle Exam SamplesAldrich ArquizaNoch keine Bewertungen
- Pediatric Fluid and Electrolyte AlterationsDokument51 SeitenPediatric Fluid and Electrolyte AlterationsMatthew Ryan100% (1)
- LaryngoceleDokument7 SeitenLaryngoceleM Grecu CeptureanuNoch keine Bewertungen
- NCP Epidural HemDokument32 SeitenNCP Epidural HemKatrina PonceNoch keine Bewertungen
- GlossectomyDokument68 SeitenGlossectomyRohan GroverNoch keine Bewertungen
- 11 Exercises For MyopiaDokument4 Seiten11 Exercises For MyopiaarifiqNoch keine Bewertungen
- Ventilator Wave Form and InterpretationDokument59 SeitenVentilator Wave Form and InterpretationArnab SitNoch keine Bewertungen
- Medical-Surgical Questions With Rationale 70 QuestionsDokument59 SeitenMedical-Surgical Questions With Rationale 70 QuestionsJam Torres100% (7)
- Dental and Craniomaxillofacial Implant SurgeryDokument35 SeitenDental and Craniomaxillofacial Implant SurgeryJean Carlos Barbosa FerreiraNoch keine Bewertungen
- Cauda Equina Syndrome Review: Diagnosis and TreatmentDokument9 SeitenCauda Equina Syndrome Review: Diagnosis and Treatmentabelinda100% (1)
- International Journal of Health Sciences and ResearchDokument8 SeitenInternational Journal of Health Sciences and Researchrizk86Noch keine Bewertungen
- Children of Mothers With Borderline Personality Disorder (BPD)Dokument6 SeitenChildren of Mothers With Borderline Personality Disorder (BPD)curiositykillcatNoch keine Bewertungen
- Super Arrow Flex Sheath - Brochure - EN PDFDokument3 SeitenSuper Arrow Flex Sheath - Brochure - EN PDFbiomedical_com_brNoch keine Bewertungen
- 38 The Use of Meta-Analysis in Pharmacoepidemiology: Jesse A. BerlinDokument27 Seiten38 The Use of Meta-Analysis in Pharmacoepidemiology: Jesse A. BerlinFranklin garryNoch keine Bewertungen
- Reading All That Jazz - Body ClockDokument4 SeitenReading All That Jazz - Body ClockMehran EltNoch keine Bewertungen
- Case Study Acute PancreatitisDokument62 SeitenCase Study Acute PancreatitisAilyne A. CleofeNoch keine Bewertungen
- Anamnesis & PemfisDokument81 SeitenAnamnesis & PemfisFikriYTNoch keine Bewertungen
- Case Presentatio Insomnia 1Dokument49 SeitenCase Presentatio Insomnia 1kiran mahal100% (1)
- The Role of Imaging in Primary Health CareDokument28 SeitenThe Role of Imaging in Primary Health CareishkoldNoch keine Bewertungen