Beruflich Dokumente
Kultur Dokumente
Orthognatic Surgery: Mandible III
Hochgeladen von
Hendy Nurahadi0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
14 Ansichten1 Seiteortho
Originaltitel
ortho 3
Copyright
© © All Rights Reserved
Verfügbare Formate
PDF, TXT oder online auf Scribd lesen
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenortho
Copyright:
© All Rights Reserved
Verfügbare Formate
Als PDF, TXT herunterladen oder online auf Scribd lesen
0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
14 Ansichten1 SeiteOrthognatic Surgery: Mandible III
Hochgeladen von
Hendy Nurahadiortho
Copyright:
© All Rights Reserved
Verfügbare Formate
Als PDF, TXT herunterladen oder online auf Scribd lesen
Sie sind auf Seite 1von 1
Oral Presentations
Wednesday, 13 September 2006, 14.3015.40
Orthognatic surgery: mandible III
Hall 8
77
the risk of serious intraoperative and postoperative complications
in the tretment of mandibular prognathism.
Orthognatic surgery: mandible III
O.274 Change of condyle angulation after BSSO
M. Szalwinski1,2 , J. Piekarczyk1 , M. Jagielak1 , P. Piekarczyk1 .
1 2nd Department of MaxilloFacial Surgery, 2 Department of
Anatomy, Medical University of Warsaw, Poland
The aim of our study was to evaluate potential changes in
mandible condyle and ramus angulation after bilateral sagittal
split osteotomies.
The material contained 30 dry specimens of human mandibles
and their digital photographs before and after BSSO.
The method: Each mandible was photographed in three different
aspects from behind, laterally and from above. The position
of mandibles in front of camera objective was always constant,
and so was the distance for statistic recurrence. Using standard
surgical equipment sagittal osteotomies were performed due to
mandibular prognathism 15 cases and retrogenia 15 cases. Diameter between condyles was maintained. Digital photographs
were processed in DICOM. Using computer software followed
data were reported: angulation of mandible ramus to frontal,
transversal and sagittal plane, angulation of condyles to each
other.
Changes in the condyle angulation depending on the osteotomy
method were reported. No signicant role of osteotomy method
were reported. However, osteotomy plane may be signicant. Although results of our study performed in vitro, without occlusion
with maxilla could be disputable, we cannot deny inuence on
temporo-mandibular joint.
O.275 Modications in surgical treatment of
mandibular prognathism Own experiences
M. Baran, T. Tomaszewski, J. Wojciechowicz. Maxillofacial
Surgery, University Hospital, Lublin, Poland
Introduction: The most frequently utilized technique for surgical
treatment of mandibular deformities is bilateral sagittal split osteotomy (BSSO), originally described by Obwegeser and Trauner.
To this technique that is modied by Dal Pont and Hunsuck,
several changes were added in our Department. The changes aim
at limiting the soft tissues dissection, obtaining stable bone union
and elimination of possible complications: excessive bleeding,
unfavourable fractures, facial palsy.
Methods: The orthodontic decompensation and the third molars
previous removal are essential. The medial osteotomy is performed with 45 angulation to the medial plane of ramus. The
osteotomy does not cross the mandibular foramen, is led down
and forward across temporal crest, does not reach the oblique
ridge and in most cases ends half a way between them. To
straighten the osteotomy line, the connecting osteotomy passes
smoothly on both the medial and lateral osteotomy, performed at
the second molar level. The lateral osteotomy passes through both
the lateral and inferior cortex of the horizontal ramus reaching
lingual surface. The split is begun in the superior part, then in
retromolar area and is completed in lateral osteotomy area.
Results: Between years 1993 and 2006, described BSSO was
performed in 97 patients with excellent outcomes. Complications
such as relapse, facial palsy, dangerous hemorrhage or pseudoarthrosis, were not observed.
Conclusions: The modied osteotomy line and removal of the
third molars bring larger thickness of bone segments. The treatment results show that the proposed BSSO modications decrease
O.276 Endoscopic-assisted rigid xation in intra-oral
vertical subsigmoid osteotomy: A preliminary
study
L.O. John, L.K. Cheung. Oral & Maxillofacial Surgery, Faculty
of Dentistry, The University of Hong Kong, China
Introduction: Intra-oral vertical subsigmoid osteotomy (IVSO)
is a mandibular ramus osteotomy technique used to correct
mandibular prognathism. It is an easily learned surgical procedure executed transorally, and results in fewer neurosensory
disturbances than sagittal split osteotomy. However, the intra-oral
route limits visibility and makes access to the application of rigid
xation difcult. Post-operative intermaxillary xation (IMF) for
several weeks is mandatory to ensure stability for bone healing.
Objectives: (1) To illustrate the clinical technique of endoscopeassisted rigid xation in intra-oral vertical subsigmoid osteotomy
(VSO); and (2) to report on early post-operative morbidities.
Material and Methods: Six patients presenting with Class 3
skeletal prole were recruited. The osteotomy was performed
through an intra-oral route. Rigid xation was achieved with a
3 mm stab incision located inferior to the ear pinna allowing
access to the transbuccal trocar. A rigid endoscope was introduced intra-orally to improve visibility during xation. Patients
preoperative and 3-month post-operative radiographs and clinical morbidities (neurosensory status & temporomandibular joint
(TMJ) function) were assessed.
Results: 83.3% of patients fully recovered inferior alveolar nerve
function, and 66.6% recovered TMJ function. The scar from the
stab incision was effectively camouaged by the ear pinna, and
was not noticeable by the patients.
Conclusion: This preliminary study conrms that the application
of endoscope-assisted rigid xation in intra-oral VSO is clinically feasible. All the patients presented with minimal clinical
morbidities and good stability at the early post-operative period.
O.277 Facial palsy after mandibular bilateral split
osteotomy Analysis of a rare and seldom
complication
E.-L. Barth, N.-C. Gellrich, P. Brachvogel. Department for
Cranio-Maxillofacial Surgery, Hannover Medical School,
Carl-Neuberg-Str. 1, 30625 Hannover, Germany
Introduction and Objectives: Since Obwegeser introduced his
operation technique in the 1950s, it had become, with slight
modications (DAL PONT, EPKER, HUNSUCK), the most
used surgical procedure to treat mandibular growth anomalies.
Although it is a highly standard procedure with calculable risks,
the literature shows many reports about facial nerve palsies as a
rare and seldom complication.
Material, Methods and Results: In a retrospective survey
over 23 years (19832006) we followed up 1826 patients who
underwent orthognathic surgery in our department. In 9 patients
a facial palsy occurred post-operatively (0.49%) In 8 cases it was
transient, in 1 case a permanent facial nerve paralysis. The aim
of the study was to analyse the dependent factors which led to
the nerve injury and how it is possible to prevent such a serious
complication.
Conclusions: However orthognathic surgery is a kind of elective
surgery in healthy people, the appearance of a postoperative
facial palsy is nearly the worst case for both sides, patient and
surgeon, because quality of life, especially social interaction, is
signicantly reduced.
Das könnte Ihnen auch gefallen
- Orthognatic Surgery: Mandible IDokument1 SeiteOrthognatic Surgery: Mandible IHendy NurahadiNoch keine Bewertungen
- Variations in Impacted Mandibular Permanent MolarsDokument9 SeitenVariations in Impacted Mandibular Permanent MolarsHendy NurahadiNoch keine Bewertungen
- Texture Analysis of CT Images in The Characterization of OralDokument7 SeitenTexture Analysis of CT Images in The Characterization of OralHendy NurahadiNoch keine Bewertungen
- Pps 2Dokument5 SeitenPps 2Hendy NurahadiNoch keine Bewertungen
- Palatal Abses IbnuDokument3 SeitenPalatal Abses IbnuHendy NurahadiNoch keine Bewertungen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- J of Cosmetic Dermatology - 2023 - Palauro - Innovation of The Protocol For The Application of Cryolipolysis Effects andDokument9 SeitenJ of Cosmetic Dermatology - 2023 - Palauro - Innovation of The Protocol For The Application of Cryolipolysis Effects andPaolaNoch keine Bewertungen
- Current issues and advances in postoperative pain managementDokument17 SeitenCurrent issues and advances in postoperative pain managementAmade DeaNoch keine Bewertungen
- 33 - Nasal Fractures PDFDokument15 Seiten33 - Nasal Fractures PDFcarlosNoch keine Bewertungen
- Research Forehead FillerDokument5 SeitenResearch Forehead FillerNavaphon ChanbangNoch keine Bewertungen
- Gifted HandsDokument8 SeitenGifted HandsMichelle Arellano67% (3)
- Apendicits NiñosDokument25 SeitenApendicits NiñosArturo SantiagoNoch keine Bewertungen
- Case Study Dr. Sisk LCA Gene Therapy MC 0005054 21NOV2022Dokument6 SeitenCase Study Dr. Sisk LCA Gene Therapy MC 0005054 21NOV2022SALAH YOUNISNoch keine Bewertungen
- Ambulatory Hysteroscopy - Creating Certainty: The Solution For Diagnostics and Treatment in An Ambulatory SettingDokument2 SeitenAmbulatory Hysteroscopy - Creating Certainty: The Solution For Diagnostics and Treatment in An Ambulatory Settingreta.rose92Noch keine Bewertungen
- Emergency Airway Management in Patients With COVID-19: A Prospective International Multicenter Cohort StudyDokument12 SeitenEmergency Airway Management in Patients With COVID-19: A Prospective International Multicenter Cohort Studyluisfernandoamaya89Noch keine Bewertungen
- Boh Luli 2019Dokument3 SeitenBoh Luli 2019Francisco ChourioNoch keine Bewertungen
- Pediatric TracheostomyDokument45 SeitenPediatric Tracheostomytsega tilahunNoch keine Bewertungen
- Tirumala Tirupati Devasthanams: TirupatiDokument3 SeitenTirumala Tirupati Devasthanams: Tirupativenkatraju.YNoch keine Bewertungen
- Causes and Management of Upper GI BleedingDokument4 SeitenCauses and Management of Upper GI BleedingRazi HaiderNoch keine Bewertungen
- Hernia: Information For PatientsDokument2 SeitenHernia: Information For Patientsrianrifaldi123_98497Noch keine Bewertungen
- 153Dokument8 Seiten153Hélder MouraNoch keine Bewertungen
- Semiology of Insular Lobe SeizuresDokument6 SeitenSemiology of Insular Lobe SeizuresViviana Torres BallesterosNoch keine Bewertungen
- Graston TechniqueDokument8 SeitenGraston TechniqueSvetlana PolyakovaNoch keine Bewertungen
- Unintentional Trauma During Gynaecological Surgery: I. Z. MackenzieDokument8 SeitenUnintentional Trauma During Gynaecological Surgery: I. Z. Mackenziemuhammadnurul asmiNoch keine Bewertungen
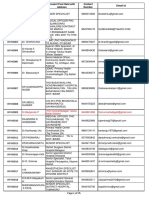
- Contact details of medical officers in KarnatakaDokument25 SeitenContact details of medical officers in KarnatakaShweta jain100% (1)
- Classification of Mandibular Condylar Fractures: David B. Powers, MD, DMD, FRCS (Ed)Dokument10 SeitenClassification of Mandibular Condylar Fractures: David B. Powers, MD, DMD, FRCS (Ed)Mashood AhmedNoch keine Bewertungen
- Irish Tatler Emface 1674483099 OriginalDokument1 SeiteIrish Tatler Emface 1674483099 OriginalFelicia BuenoNoch keine Bewertungen
- Syntax Score Calculation SimulationDokument66 SeitenSyntax Score Calculation SimulationTahari Bargas PrakosoNoch keine Bewertungen
- Advances in Facial Rejuvenation Botox, HA Dermal Fillers, & Combination TherapyDokument26 SeitenAdvances in Facial Rejuvenation Botox, HA Dermal Fillers, & Combination Therapybluestes100% (1)
- Pterygium Pinguecula Post-Op GuideDokument4 SeitenPterygium Pinguecula Post-Op GuideBrandon ChienNoch keine Bewertungen
- Anatomical Shoulder Fracture System Surgical Technique PDFDokument24 SeitenAnatomical Shoulder Fracture System Surgical Technique PDFAdrian TudorNoch keine Bewertungen
- SERVO-Air Presentation Indonesia Rev SlideDokument32 SeitenSERVO-Air Presentation Indonesia Rev SlideSamsulNoch keine Bewertungen
- Total Shoulder Arthroplasty, An Overview, Indicatins and Prosthetic OptionsDokument4 SeitenTotal Shoulder Arthroplasty, An Overview, Indicatins and Prosthetic OptionsYafiahnaf FirdausNoch keine Bewertungen
- Removable Partial Denture Occlusion: John R. Ivanhoe, DDS, Kevin D. Plummer, DDSDokument17 SeitenRemovable Partial Denture Occlusion: John R. Ivanhoe, DDS, Kevin D. Plummer, DDSAna MaríaNoch keine Bewertungen
- What Happens After The Cystoscopy ProcedureDokument2 SeitenWhat Happens After The Cystoscopy ProcedureStepyn SalvadorNoch keine Bewertungen
- Female Urinary Catheter Insertion GuideDokument9 SeitenFemale Urinary Catheter Insertion GuideVinz Khyl G. CastillonNoch keine Bewertungen