Beruflich Dokumente
Kultur Dokumente
Copd Guideline Acp Ats Ers Accp Abstract
Hochgeladen von
RESCATEURCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Copd Guideline Acp Ats Ers Accp Abstract
Hochgeladen von
RESCATEURCopyright:
Verfügbare Formate
Diagnosis and Management of Stable Chronic Obstructive Pulmonary Dis...
1 of 3
http://www.annals.org/content/155/3/179.abstract#.TwMzI3I6LvE.email
Annals of Internal Medicine
www.annals.org
Ann Intern Med
August 2, 2011
vol. 155 no. 3 179-191
Clinical Guidelines
Diagnosis and Management of Stable Chronic Obstructive Pulmonary
Disease: A Clinical Practice Guideline Update from the American College of
Physicians, American College of Chest Physicians, American Thoracic Society,
and European Respiratory Society
Amir Qaseem, MD, PhD, MHA; Timothy J. Wilt, MD, MPH; Steven E. Weinberger, MD; Nicola A. Hanania, MD, MS; Gerard Criner, MD;
Thys van der Molen, PhD; Darcy D. Marciniuk, MD; Tom Denberg, MD, PhD; Holger Schnemann, MD, PhD, MSc; Wisia Wedzicha, PhD;
Roderick MacDonald, MS; and Paul Shekelle, MD, PhD, for the American College of Physicians, the American College of Chest
Physicians, the American Thoracic Society, and the European Respiratory Society *
+ Author Affiliations
Abstract
Description: This guideline is an official statement of the American College of Physicians (ACP), American College of Chest Physicians (ACCP),
American Thoracic Society (ATS), and European Respiratory Society (ERS). It represents an update of the 2007 ACP clinical practice guideline on
diagnosis and management of stable chronic obstructive pulmonary disease (COPD) and is intended for clinicians who manage patients with COPD.
This guideline addresses the value of history and physical examination for predicting airflow obstruction; the value of spirometry for screening or
diagnosis of COPD; and COPD management strategies, specifically evaluation of various inhaled therapies (anticholinergics, long-acting -agonists,
and corticosteroids), pulmonary rehabilitation programs, and supplemental oxygen therapy.
Methods: This guideline is based on a targeted literature update from March 2007 to December 2009 to evaluate the evidence and update the 2007
ACP clinical practice guideline on diagnosis and management of stable COPD.
Recommendation 1: ACP, ACCP, ATS, and ERS recommend that spirometry should be obtained to diagnose airflow obstruction in patients with
respiratory symptoms (Grade: strong recommendation, moderate-quality evidence). Spirometry should not be used to screen for airflow obstruction
in individuals without respiratory symptoms (Grade: strong recommendation, moderate-quality evidence).
Recommendation 2: For stable COPD patients with respiratory symptoms and FEV1 between 60% and 80% predicted, ACP, ACCP, ATS, and ERS
suggest that treatment with inhaled bronchodilators may be used (Grade: weak recommendation, low-quality evidence).
Recommendation 3: For stable COPD patients with respiratory symptoms and FEV1 <60% predicted, ACP, ACCP, ATS, and ERS recommend
treatment with inhaled bronchodilators (Grade: strong recommendation, moderate-quality evidence).
Recommendation 4: ACP, ACCP, ATS, and ERS recommend that clinicians prescribe monotherapy using either long-acting inhaled anticholinergics
or long-acting inhaled -agonists for symptomatic patients with COPD and FEV1 <60% predicted. (Grade: strong recommendation, moderate-quality
evidence). Clinicians should base the choice of specific monotherapy on patient preference, cost, and adverse effect profile.
Recommendation 5: ACP, ACCP, ATS, and ERS suggest that clinicians may administer combination inhaled therapies (long-acting inhaled
anticholinergics, long-acting inhaled -agonists, or inhaled corticosteroids) for symptomatic patients with stable COPD and FEV1<60% predicted
(Grade: weak recommendation, moderate-quality evidence).
Recommendation 6: ACP, ACCP, ATS, and ERS recommend that clinicians should prescribe pulmonary rehabilitation for symptomatic patients with
an FEV1 <50% predicted (Grade: strong recommendation, moderate-quality evidence). Clinicians may consider pulmonary rehabilitation for
symptomatic or exercise-limited patients with an FEV1 >50% predicted. (Grade: weak recommendation, moderate-quality evidence).
Recommendation 7: ACP, ACCP, ATS, and ERS recommend that clinicians should prescribe continuous oxygen therapy in patients with COPD who
have severe resting hypoxemia (Pa O2 55 mm Hg or SpO2 88%) (Grade: strong recommendation, moderate-quality evidence).
Related articles
Letter:
A Clinical Practice Guideline Update on the Diagnosis and Management of Stable Chronic Obstructive Pulmonary Disease
Robert P. Young and Raewyn J. Hopkins
Ann Intern Med January 3, 2012 156:68-69;
1/3/2012 12:42 PM
Das könnte Ihnen auch gefallen
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- 2017 AMI-STEMI Slide-Set Final For WebDokument94 Seiten2017 AMI-STEMI Slide-Set Final For WebRESCATEURNoch keine Bewertungen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- 2017 DAPT Slide-SetDokument55 Seiten2017 DAPT Slide-SetRESCATEURNoch keine Bewertungen
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- DAPTDokument48 SeitenDAPTRESCATEURNoch keine Bewertungen
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- 2017 STEMI Ehx393 - Web Addenda - For WEBDokument8 Seiten2017 STEMI Ehx393 - Web Addenda - For WEBRESCATEURNoch keine Bewertungen
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Standardisation of Lung Function Testing: The Authors' Replies To Readers' CommentsDokument3 SeitenStandardisation of Lung Function Testing: The Authors' Replies To Readers' CommentsRESCATEURNoch keine Bewertungen
- 2016 Cardio-Oncology Slide-SetDokument18 Seiten2016 Cardio-Oncology Slide-SetRESCATEURNoch keine Bewertungen
- American Thoracic Society Statement On Research Priorities in Respiratory NursingDokument8 SeitenAmerican Thoracic Society Statement On Research Priorities in Respiratory NursingRESCATEURNoch keine Bewertungen
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- Stem CellDokument3 SeitenStem CellRESCATEURNoch keine Bewertungen
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Integrating Coordinating Efforts Copd Guideline DevelopmentDokument96 SeitenIntegrating Coordinating Efforts Copd Guideline DevelopmentRESCATEURNoch keine Bewertungen
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Multi MorbidityDokument10 SeitenMulti MorbidityRESCATEURNoch keine Bewertungen
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Case Presentation: Daguio / Dianalan / Ebrahim / EddingDokument29 SeitenCase Presentation: Daguio / Dianalan / Ebrahim / EddingnsdnNoch keine Bewertungen
- Resume Ogechi UkachuDokument3 SeitenResume Ogechi UkachuSlahuddin KhanNoch keine Bewertungen
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Surgery Made Easy V1 PDFDokument125 SeitenSurgery Made Easy V1 PDFطلال العمريNoch keine Bewertungen
- Orahex Oral SolutionDokument1 SeiteOrahex Oral SolutionconanmarcNoch keine Bewertungen
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
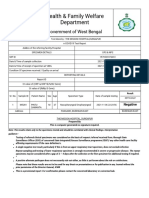
- Health & Family Welfare Department: Government of West BengalDokument2 SeitenHealth & Family Welfare Department: Government of West BengalAnkit JhaNoch keine Bewertungen
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- Breast Self Examination 1Dokument36 SeitenBreast Self Examination 1zehan iraniNoch keine Bewertungen
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- Roleplay FastfoodDokument9 SeitenRoleplay FastfoodIndra DarmaNoch keine Bewertungen
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- Infection Control Management Plan: PurposeDokument6 SeitenInfection Control Management Plan: PurposeRekhaNoch keine Bewertungen
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Diagnosis and Management of Intrahepatic Cholangiocarcinoma: A Comprehensive Update For The RadiologistDokument22 SeitenDiagnosis and Management of Intrahepatic Cholangiocarcinoma: A Comprehensive Update For The RadiologistNadia HamdaniNoch keine Bewertungen
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Chapter 12Dokument16 SeitenChapter 12Ruthleen May Simeon100% (1)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Neurologic ProblemsDokument11 SeitenNeurologic ProblemsFilipino Nurses Central67% (3)
- WEBSTER, J.G. Medical Instrumentation: Application and Design. New York: John Wiley & Sons, 1998Dokument2 SeitenWEBSTER, J.G. Medical Instrumentation: Application and Design. New York: John Wiley & Sons, 1998Virgilio MagaldeNoch keine Bewertungen
- G4 - SCI Summative Test in Science IV (Chapters 14 - 19)Dokument4 SeitenG4 - SCI Summative Test in Science IV (Chapters 14 - 19)Ador Isip100% (2)
- Compartment-Syndrome PPT GADAR 2Dokument20 SeitenCompartment-Syndrome PPT GADAR 2meikha tari batjun0% (1)
- Phlebtomy Guidelines and Order of DrawDokument3 SeitenPhlebtomy Guidelines and Order of Drawohemgee wowNoch keine Bewertungen
- Kesehatan Indonesia. 2016.: Daftar PustakaDokument2 SeitenKesehatan Indonesia. 2016.: Daftar PustakaSiti Raudatus SolihahNoch keine Bewertungen
- Presentation Resuscitation - Power PointDokument45 SeitenPresentation Resuscitation - Power PointRouquia ManzoorNoch keine Bewertungen
- White FungusDokument279 SeitenWhite FungusDjsjsbNoch keine Bewertungen
- Performance Indicators For Hospitals: Niladri MajumderDokument34 SeitenPerformance Indicators For Hospitals: Niladri MajumderNiladri Majumder100% (15)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- KNH 411 Final ExamDokument12 SeitenKNH 411 Final Examapi-301897220Noch keine Bewertungen
- 03 Klasifikasi Penyakit Dan Keadaan Yang Mempengaruhi Jaringan PeriodontiumDokument16 Seiten03 Klasifikasi Penyakit Dan Keadaan Yang Mempengaruhi Jaringan PeriodontiumFloba Ika SianturiNoch keine Bewertungen
- S1.01. Dental ErgonomicsDokument72 SeitenS1.01. Dental ErgonomicsYasser Al WasifiNoch keine Bewertungen
- Poison and Antidote ChartDokument5 SeitenPoison and Antidote ChartSusanne Mae Gonzales50% (2)
- Nursing Pharmacology Immunity Study GuideDokument18 SeitenNursing Pharmacology Immunity Study GuideChelsea SmithNoch keine Bewertungen
- SDMS ID: P2010/0496-001 2.9/09WACS Title: Management of Postpartum HaemorrhageDokument11 SeitenSDMS ID: P2010/0496-001 2.9/09WACS Title: Management of Postpartum HaemorrhageYwagar YwagarNoch keine Bewertungen
- Department ListDokument6 SeitenDepartment Listzubair waliNoch keine Bewertungen
- Per Rectal Bleeding CompiledDokument33 SeitenPer Rectal Bleeding CompiledRajhmuniran Kandasamy100% (1)
- Historical Development of Psychiatric Social Work and Role of Psychiatric Social Worker in SocietyDokument9 SeitenHistorical Development of Psychiatric Social Work and Role of Psychiatric Social Worker in SocietyZubair Latif100% (7)
- CABGDokument14 SeitenCABGClaudette CayetanoNoch keine Bewertungen
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Spiritual Healing Chants - Opt PDFDokument11 SeitenSpiritual Healing Chants - Opt PDFAmit Govilkar100% (1)