Beruflich Dokumente
Kultur Dokumente
1 12 Nucleic Acid Testing To Detect HBV in Blood Donors 2011
Hochgeladen von
Putri Kusuma WardaniOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
1 12 Nucleic Acid Testing To Detect HBV in Blood Donors 2011
Hochgeladen von
Putri Kusuma WardaniCopyright:
Verfügbare Formate
The
n e w e ng l a n d j o u r na l
of
m e dic i n e
original article
Nucleic Acid Testing to Detect HBV
Infection in Blood Donors
Susan L. Stramer, Ph.D., Ulrike Wend, Daniel Candotti, Ph.D., Gregory A. Foster, B.A.,
F. Blaine Hollinger, M.D., Roger Y. Dodd, Ph.D., Jean-Pierre Allain, M.D.,
and Wolfram Gerlich, M.D.
A bs t r ac t
Background
From the Scientific Support Office, American Red Cross, Gaithersburg, MD (S.L.S.,
G.A.F.), and the Holland Laboratory, American Red Cross, Rockville, MD (R.Y.D.); the
Institute of Medical Virology, University of
Giessen, Giessen, Germany (U.W., W.G.);
the National Health Service Blood and
Transplant (D.C.) and the Department of
Haematology, University of Cambridge
(J.-P.A.) both in Cambridge, United
Kingdom; and the Eugene B. Casey Hepatitis Research Center, Baylor College of
Medicine, Houston (F.B.H.). Address reprint requests to Dr. Stramer at the
American Red Cross, Scientific Support
Office, 9315 Gaither Rd., Gaithersburg, MD
20877, or at stramers@usa.redcross.org.
N Engl J Med 2011;364:236-47.
Copyright 2011 Massachusetts Medical Society.
The detection of hepatitis B virus (HBV) in blood donors is achieved by screening
for hepatitis B surface antigen (HBsAg) and for antibodies against hepatitis B core
antigen (anti-HBc). However, donors who are positive for HBV DNA are currently
not identified during the window period before seroconversion. The current use of
nucleic acid testing for detection of the human immunodeficiency virus (HIV) and
hepatitis C virus (HCV) RNA and HBV DNA in a single triplex assay may provide
additional safety.
Methods
We performed nucleic acid testing on 3.7 million blood donations and further
evaluated those that were HBV DNApositive but negative for HBsAg and anti-HBc.
We determined the serologic, biochemical, and molecular features of samples that
were found to contain only HBV DNA and performed similar analyses of follow-up
samples and samples from sexual partners of infected donors. Seronegative HIV
and HCV-positive donors were also studied.
Results
We identified 9 donors who were positive for HBV DNA (1 in 410,540 donations),
including 6 samples from donors who had received the HBV vaccine, in whom subclinical infection had developed and resolved. Of the HBV DNApositive donors,
4 probably acquired HBV infection from a chronically infected sexual partner. Clinically significant liver injury developed in 2 unvaccinated donors. In 5 of the 6 vaccinated donors, a non-A genotype was identified as the dominant strain, whereas
subgenotype A2 (represented in the HBV vaccine) was the dominant strain in unvaccinated donors. Of 75 reactive nucleic acid test results identified in seronegative
blood donations, 26 (9 HBV, 15 HCV, and 2 HIV) were confirmed as positive.
Conclusions
Triplex nucleic acid testing detected potentially infectious HBV, along with HIV and
HCV, during the window period before seroconversion. HBV vaccination appeared
to be protective, with a breakthrough subclinical infection occurring with non-A2
HBV subgenotypes and causing clinically inconsequential outcomes. (Funded by
the American Red Cross and others.)
236
n engl j med 364;3 nejm.org january 20, 2011
The New England Journal of Medicine
Downloaded from nejm.org at UC SHARED JOURNAL COLLECTION on July 5, 2012. For personal use only. No other uses without permission.
Copyright 2011 Massachusetts Medical Society. All rights reserved.
Nucleic Acid Testing to Detect HBV in Blood
he transfusion of blood containing hepatitis B surface antigen (HBsAg) is
associated with post-transfusion infection
with hepatitis B virus (HBV). Blood that is free
of HBsAg but has high-titer antibodies against
hepatitis B core antigen (anti-HBc) in the absence
of antibodies against hepatitis B surface antigen
(anti-HBs) can also transmit HBV infection.1,2 In
1986, screening for anti-HBc was implemented
in the United States to reduce HBV transmission
and as a surrogate marker for non-A, non-B hepatitis (i.e., hepatitis C virus [HCV]).3,4 However,
a small proportion of donors with anti-HBc in
the absence of HBsAg have circulating HBV DNA
and may have a risk of infectivity.1-6
Blood that is collected during the early window period of HBV infection is highly infectious,
but this risk declines as anti-HBs develops.5,7-12
The estimated residual risk of HBV infection from
donations to the American Red Cross ranges
from 1 in 280,000 to 1 in 357,000 donations.13
After the introduction of nucleic acid testing for
screening in minipools (pools of 6 to 16 donations), the estimated yield of HBV infection ranges
from 1 in 830,000 to 1 in 2 million donations.14
However, these estimates do not capture the possibility of HBV infection in vaccinated donors
who have acute infection with low or no expression of HBsAg. HBV-seronegative but infected
donors have been identified by means of nucleic
acid testing at a rate of approximately 1 in
600,000 donations screened15 but have not been
further studied. Although the residual risk of
transmission of HBV by transfusion has decreased
progressively,13,16,17 it remains higher than the
estimated risks for human immunodeficiency
virus (HIV) and HCV (1 in 1,467,000 donations
and 1 in 1,149,000 donations, respectively).18
We conducted a study to evaluate the use of
nucleic acid testing in determining the number
of seronegative donors who have HBV DNA and
to characterize these donors according to their
risk factors and progression of molecular, serologic, and biochemical markers. We used a triplex test combining the detection of HBV DNA
with that of HIV and HCV RNA. We also evaluated donors who were seronegative for HIV and
HCV but had positive results on nucleic acid
testing.
Me thods
Screening Protocol
During 2008, the American Red Cross implemented prospective screening of all blood donations, using the Procleix Ultrio assay and the
TIGRIS automated platform10 (Gen-Probe and
Novartis) at three of its five National Testing
Laboratories. The American Red Cross collects
about 42% of the U.S. blood supply from volunteer, unpaid donors in the continental United
States and Puerto Rico. All donations were
screened by nucleic acid testing of either individual donations or 16-sample minipools. Blood
units that were released for transfusion were
negative on triplex nucleic acid testing and for all
standard blood-screening markers.18 All Ultrioreactive minipools were resolved to the reactive
individual donation, followed by testing of the
reactive individual donations (including donations
screened individually by nucleic acid testing) by
means of separate discriminatory assays for HBV,
HIV, and HCV. Any individual donation with a
positive result on nucleic acid testing was not
used for transfusion (even if the donor was subsequently determined to have a false positive result), and associated donors were deferred from
future donation. Seronegative donors with one or
multiple reactive discriminatory tests were considered potentially infected donors for further
study. For individual donations, the 95% lower
limit of detection for the HBV portion of Ultrio is
10.4 IU per milliliter (approximately 50 copies per
milliliter), as compared with approximately 30
copies per milliliter each for HIV and HCV.
The study protocol was approved by the institutional review board of the American Red Cross.
Written informed consent for follow-up studies
was obtained from donors who were reactive on
nucleic acid testing and from their partners. The
study was conducted in accordance with the provisions of the protocol.
HBV DNA Confirmation
Donors who were positive for HBV DNA on the
Ultrio assay and seronegative for HBsAg (lower
limit of detection, 0.10 ng per milliliter) and for
total (IgM and IgG) anti-HBc (HBsAg and HBcore
PRISM, Abbott Laboratories) were enrolled in
n engl j med 364;3 nejm.org january 20, 2011
The New England Journal of Medicine
Downloaded from nejm.org at UC SHARED JOURNAL COLLECTION on July 5, 2012. For personal use only. No other uses without permission.
Copyright 2011 Massachusetts Medical Society. All rights reserved.
237
The
n e w e ng l a n d j o u r na l
follow-up studies, which involved the collection
of samples at intervals of 1 to 2 weeks until seroconversion to anti-HBc occurred. Each plasma
unit from a reactive donation was retrieved for
further testing.
Additional testing that was repeated on all
index donations, as well as performed on each
follow-up sample, included duplicate Ultrio nucleic acid testing of individual donations and discriminatory testing if reactivity was observed,
followed by confirmation by means of polymer
ase-chain-reaction (PCR) assay with the use of
COBAS AmpliScreen HBV Test (Roche) with the
1-milliliter extraction method (95% lower limit
of detection, 5 IU per milliliter). In addition, the
retrieved plasma units from each donation with
reactivity on discriminatory testing were separated into aliquots and tested in replicates of 10 to
confirm reactivity. Reactivity in at least 1 of the
10 replicate tests was required for confirmation
of positive results; donations with no reactivity
were considered to have false positive results.
Serologic testing was performed on retrieved
plasma units and follow-up samples for HBsAg,
total anti-HBc, qualitative and quantitative antiHBs (Monolisa, Bio-Rad Laboratories), IgM antiHBc (ARCHITECT, Abbott), and alanine aminotransferase (Quest Diagnostics). Donors whose
HBV DNA reactivity could be confirmed in index
samples or who had serologic evidence of HBV
infection in follow-up samples were considered
to have HBV infection. The sexual partner of each
of these donors was contacted for follow-up, if
possible. Screening of a subgroup of donors for
anti-HBs was performed as an indicator of HBV
vaccine penetrance in the donor population (for
of
m e dic i n e
details, see the Supplementary Appendix, available with the full text of this article at NEJM
.org). Molecular analyses of donor and partner
samples were performed in the Geissen and
Cambridge laboratories (see the Supplementary
Appendix, available with the full text of this article at NEJM.org).
HIV and HCV RNA confirmation
Confirmation of the presence of HIV and HCV
RNA included HIV and HCV qualitative and
quantitative PCR and HCV genotyping performed
at the National Genetics Institute. Antibodies
against HIV types 1 and 2 (HIV-1/HIV-2 rDNA EIA,
Abbott Laboratories) and HCV (HCV 3.0 ELISA,
Ortho Clinical Diagnostics) were used for serologic testing of index and follow-up samples.
Serologic confirmation of reactive samples was
performed with tests licensed by the Food and
Drug Administration.18 Sexual partners were
contacted if possible, as described for HBV confirmation.
Study Oversight
The study was funded in part by Gen-Probe and
Novartis Vaccines and Diagnostics, which provided the Ultrio test kits and TIGRIS instruments. The American Red Cross provided a clinical-trial site in support of an investigational
protocol designed to determine the frequency of
donors who test HBV-seronegative but DNA-positive so that an HBV DNA blood-donation-screening claim could be justified for the Ultrio assay
performed on the TIGRIS automated platform.
The study protocol was designed and executed by
the American Red Cross and its collaborators.
Table 1. Confirmed Results on Nucleic Acid Testing and Serologic Analysis of 3,694,858 Blood Donations.*
Classification
HBV
HIV
HCV
no.
frequency
no.
frequency
no.
frequency
Positive on nucleic acid testing and
serologic analysis
426
1 in 8673
231
1 in 15,995
1426
1 in 2591
Positive on nucleic acid testing only
1 in 410,540
1 in 1,847,429
15
1 in 246,324
178
1 in 20,758
29
1 in 127,409
517
1 in 7147
Positive on serologic analysis only
* HBV denotes hepatitis B virus, HCV hepatitis C virus, and HIV human immunodeficiency virus.
Positive results for HBV on serologic analysis indicate the presence of hepatitis B surface antigen (HBsAg).
Of the 426 donations that were positive for HBV DNA and HBsAg (by neutralization), 407 (96%) were reactive to antibodies against hepatitis B core antigen (anti-HBc).
Of the 178 donations that were negative for HBV DNA and positive for HBsAg (by neutralization), 86 (48%) were reactive to anti-HBc.
238
n engl j med 364;3 nejm.org january 20, 2011
The New England Journal of Medicine
Downloaded from nejm.org at UC SHARED JOURNAL COLLECTION on July 5, 2012. For personal use only. No other uses without permission.
Copyright 2011 Massachusetts Medical Society. All rights reserved.
Nucleic Acid Testing to Detect HBV in Blood
Table 2. Characteristics of 15 Donors with HCV Infection and 2 with HIV Infection.*
Donor No.
Sex
Donor Status
Follow-up
Age
HCV RNA
days
yr
copies/ml
Genotype
55
<100
NA
3,400,000
3A
3,800,000
3A
HCV
0131
Repeat
Follow-up
Partner
11
F
NA
0031
Repeat
63
12,000
0111
First time
24
240,000
3A
0121
Repeat
77
380,000
1A
0741
First time
34
4,900,000
1A
0742
First time
24
6,600,000
1A
0743
First time
17
8,400,000
2B
0112
First time
38
11,000,000
3A
0122
Repeat
Follow-up
49
18
19,000,000
1B
370,000,000
1B
0113
Repeat
24
21,000,000
3A
0744
First time
21
31,000,000
1A
0551
Repeat
48
33,000,000
3A
0123
Repeat
52
41,000,000
3A
0541
Repeat
45
43,000,000
0191
First time
30
53,000,000
1A
0745
Repeat
16
44,000
NA
0746
Repeat
29
340,000
NA
HIV
* Donors with hepatitis C virus (HCV) or human immunodeficiency virus (HIV) are identified by a four-number designation.
The first three numbers indicate the collection site, and the number after the dash indicates the donor-sequence number
at the given site. Thus, at site 074, six seronegative, RNA-positive donors were identified. NA denotes not available.
R e sult s
Detection of HBV
In 2008, a total of 3,694,858 donations from
2,137,275 donors were screened with the use of
Ultrio. Of these samples, 576,940 donations (16%)
were screened individually by nucleic acid testing
and the remainder were screened in minipools.
After virus-specific discriminatory testing, 9 HBVseronegative donors were confirmed as having
HBV infection by additional testing (1 of 410,540
donations) (Table 1). Of the 9 infected donors,
7 (of whom 6 had been vaccinated) consented to
participate in the follow-up study, as did the sexual partners of 4 donors. The remaining 2 donors
were confirmed as having HBV infection at their
index donation from the retrieved plasma unit by
repeat nucleic acid testing. All but 1 of the 9 do-
nors with HBV infection were identified by
means of minipool nucleic acid testing; the remaining donor (019) required individual-donation nucleic acid testing for detection and tested
nonreactive by intermediate dilutions. Of the 9
donors with HBV infection, 8 were repeat donors, and 1 was a first-time donor (055). The
mean age of the infected donors was 26 years;
6 of the donors were men.
Detection of HCV and HIV
Fifteen HCV-seronegative donors had confirmed
positive results for HCV RNA on PCR assay at
their index donation. Repeat nucleic acid testing
of the retrieved plasma unit further confirmed the
index results, including identical genotypes and
similar viral loads. The 15 HCV-infected donors
are shown in order of increasing viral load at the
n engl j med 364;3 nejm.org january 20, 2011
The New England Journal of Medicine
Downloaded from nejm.org at UC SHARED JOURNAL COLLECTION on July 5, 2012. For personal use only. No other uses without permission.
Copyright 2011 Massachusetts Medical Society. All rights reserved.
239
The
n e w e ng l a n d j o u r na l
of
m e dic i n e
Table 3. Characteristics of Nine Blood Donors with Hepatitis B Virus (HBV) Infection in Index and Follow-up Samples and in Samples
from Sexual Partners.*
Donor No.
Sex
Age
Receipt of HBV
Vaccine (yr)
yr
001
Partner
003
HBV DNA
at Index
Donation
Duration of
Detected Viremia
Anti-HBs Level at Index
Donation
IU/ml
days
IU/liter
22
Yes (1992)
11
45 to 69
Negative
23
No
1.9108
NA
Negative
37
Yes (1981)
86
44 to 70
3 (ruled nonimmune)
Negative
38
No
3.610
NA
17
Yes (1998)
13
137 to 168
11
19
No
2.6108
NA
Negative
27
Yes (2001)
35
34 to 42
43
25
No
1.8106
NA
Negative
029**
19
Yes (unknown)
30
NA
96
042
28
Yes (unknown)
27
72 to 107
33
019**
44
No
21
NA
Negative
055
20
No
47
70 to >125
Negative
074
24
No
18
73 to 115
Negative
Partner
011
Partner
013
Partner
* Donors are identified by a three-number designation, indicating the collection site. At each site, there was only one seronegative, DNApositive donor. ALT denotes alanine aminotransferase, anti-HBc antibodies against hepatitis B core antigen, anti-HBs antibodies against
hepatitis B surface antigen, HBsAg hepatitis B surface antigen, and NA not available.
The number preceding the genotype, or subgenotype in donors 029 and 042, indicates the number of clones of this genotype or subgenotype in the entire quasispecies.
A value higher than 30 U per liter was considered to be elevated.
Cons indicates consensus sequence obtained by direct sequencing. The number preceding x indicates the number of clones carrying
the substitution; s indicates the location of the amino acid substitution in the HBsAg gene.
The donor became positive for anti-HBs (100 IU per liter) within 45 days, which was up to 24 days before seroconversion to IgM anti-HBc.
The donor was reactive at the index donation.
** The donor declined enrollment in the follow-up study.
The donor could not recall the year of vaccination.
index donation (median, 11 million copies per
milliliter) in Table 2. The rate of HCV RNApositive, seronegative donations was 1 in 246,324
(Table 1). Of the 15 donors, there was a nearly
even split between first-time and repeat donors,
with a mean age of 40 years; 10 of the donors were
men. The female sexual partner of donor 013-1
was available for testing; the two had the same 3A
genotype, implying infection from a common
source or through sexual transmission.
Two donors had confirmed positive results for
HIV RNA on PCR assay at their index donation,
with viral loads of 44,000 and 340,000 copies
240
per milliliter (Table 2). Testing of the plasma
unit confirmed the index test results. These two
donors, who were both seronegative, were male
repeat donors who were 16 and 29 years of age.
The HIV RNApositive donation rate was 1 in
1,847,429 donations (Table 1).
In a combined analysis of study findings,
among 75 samples from seronegative donors
that were reactive on Ultrio and discriminatory
testing, there were 26 confirmed infections (9
HBV, 15 HCV, and 2 HIV), or 1 in 153,952 donations. Thus, the positive predictive value for the
Ultrio triplex assay in seronegative samples, in-
n engl j med 364;3 nejm.org january 20, 2011
The New England Journal of Medicine
Downloaded from nejm.org at UC SHARED JOURNAL COLLECTION on July 5, 2012. For personal use only. No other uses without permission.
Copyright 2011 Massachusetts Medical Society. All rights reserved.
Nucleic Acid Testing to Detect HBV in Blood
Genotype or
Subgenotype
Days to Seroconversion
HBsAg
Anti-HBc
(IgM and
total)
ALT
Number
of Clones
Sequenced
U/liter
no.
Amino Acid
Substitutions
on S Protein
Anti-HBs
days
No
69
45
C2
7 to 16
20
20xsG145R, sV184G,
W199 stop
NA
NA
NA
C2
31
14
Cons sG145R,
3xsG145R, sV184G
No
70
20
A2
3 to 8
11
G102D, T134A
NA
NA
NA
A2
17
10
108
168
Reactive
F1
4 to 7
12
Wild type
NA
NA
NA
F1
36
11
4xsY72 stop
No
No
Reactive
B2
8 to 19
10
1xsG112R, 1xsA128T
NA
NA
NA
B2
38
Wild type
NA
NA
Reactive
7D, 4A2, 1A2/D
10
2xsQ54 frameshift
72
107
Reactive
6D, 2A2
3 to 12
sY134H, sT143A
NA
NA
NA
A2
18
15
sG112R, sT118 M,
sF134L
40
70
125
A2
9 to 640
18
C124Y, sD151L,
sW156R
No
73
115
A2
9 to 119
15
sT126A
cluding virus-specific discrimination, was 35%,
which is similar to the predictive value of other
screening assays. Two of the 26 samples required
individual-donation nucleic acid testing for detection, for a yield of 1 in 288,470 donations.
The rates of detection on serologic analysis were
higher than the rates on nucleic acid testing for
all three viruses, underscoring the need for both
nucleic acid testing and serologic screening
(Table 1).
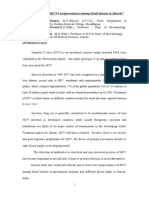
Course of HBV Infection in Index Donors
The HBV viral load was consistently low in all
index samples from the nine infected donors (11
to 86 IU per milliliter) (Table 3). Five index samples contained only HBV DNA, with no serologic
HBV markers, and four samples contained lowlevel anti-HBs (3 to 96 IU per liter), all from donors who had been vaccinated against HBV. Attempts were made to contact all nine donors.
Two donors (019 and 029) did not respond; the
other seven donors had viremia for 34 to at least
137 days but subsequently had undetectable lev-
els of HBV DNA (Table 3). Samples from these
seven donors were obtained regularly for 119 to
320 days. IgM anti-HBc (confirming acute infection) developed in all but one donor (013); this
donor had the shortest period of viremia and did
not have detectable HBsAg or total anti-HBc. One
unvaccinated donor (055) had the classic pattern
of window-period evolution accompanied by clinical signs of disease, with the presence of HBsAg
from 40 to at least 70 days, corresponding to a
peak viral load of 1.6108 IU per milliliter and an
alanine aminotransferase level of 640 U per liter.
IgM and total anti-HBc appeared on day 70, and
anti-HBs appeared on day 125 (Table 3 and Fig.
1A). Another unvaccinated donor (074) who did
not have anti-HBs at baseline became reactive to
IgM and total anti-HBc on day 73, with seroconversion to anti-HBs on day 115. Although HBsAg
was never detected, there were clinical signs of
disease, on the basis of an elevated alanine aminotransferase level (119 U per liter) on day 73.
Follow-up studies were performed for five of
the six donors with a history of HBV vaccination;
n engl j med 364;3 nejm.org january 20, 2011
The New England Journal of Medicine
Downloaded from nejm.org at UC SHARED JOURNAL COLLECTION on July 5, 2012. For personal use only. No other uses without permission.
Copyright 2011 Massachusetts Medical Society. All rights reserved.
241
The
n e w e ng l a n d j o u r na l
of
m e dic i n e
Anti-HBc (total) CO/S, HBsAg and
Anti-HBc (IgM) S/CO, Anti-HBs (IU/liter),
HBV DNA (copies/ml)
A Donor 055
109
108
107
106
105
104
103
102
HBV DNA
Anti-HBs
Anti-HBc (total)
Anti-HBc (IgM)
HBsAg
101
100
101
40
70
125
175
225
Days after Index
Anti-HBc (total) CO/S, HBsAg and Anti-HBc (IgM) S/CO, Anti-HBs (IU/liter),
HBV DNA (copies/ml)
B
Donor 013
103
Anti-HBs
104
102
HBV DNA
Anti-HBs
103
101
102
HBV DNA
Anti-HBc (total)
HBsAg
0
25
30
40
45
55
60
70
Anti-HBc (IgM)
101
100
101
Donor 042
105
75 110 125 240
Anti-HBc (total)
100
101
15
20
HBsAg
30
Days after Index
Donor 011
105
75
105
110
125
130
Donor 003
104
HBV DNA
104
HBV DNA
103
Anti-HBs
Anti-HBs
103
102
102
Anti-HBc (IgM)
101
101
Anti-HBc (total)
Anti-HBc (total)
100
101
50
Days after Index
80
100
105
120
Days after Index
135
165
100
Anti-HBc (IgM)
HBsAg
101
185
0
HBsAg
20
40
70
80
90
95
105 110 155 320
Days after Index
Figure 1. Evolution of Serologic Markers for Hepatitis B Virus (HBV) after Index Donation from Five Donors with Acute HBV Infection.
The results of follow-up analyses of virologic and serologic markers for HBV are shown for one donor who did not receive the HBV vaccine
(Panel A) and for four vaccinated donors (Panel B). Included in the analyses are values for HBV DNA (in copies per milliliter). Values for
hepatitis B surface antigen (HBsAg) and for IgM antibodies against hepatitis B core antigen (anti-HBc) are reported as signal-to-cutoff
(S/CO) ratios, where values of 1.00 or more are considered to indicate reactivity. Values for anti-HBc (total) are reported as the reciprocal of S/CO since the assay format is based on competitive inhibition. Values of 10 or more for antibodies against hepatitis B surface antigen (anti-HBs) are considered to indicate immunity. Dashed lines indicate values below the threshold of detection.
242
n engl j med 364;3 nejm.org january 20, 2011
The New England Journal of Medicine
Downloaded from nejm.org at UC SHARED JOURNAL COLLECTION on July 5, 2012. For personal use only. No other uses without permission.
Copyright 2011 Massachusetts Medical Society. All rights reserved.
Nucleic Acid Testing to Detect HBV in Blood
four of the five were positive for anti-HBs and
for HBV DNA at baseline. Transiently low levels
of HBsAg were observed in two of these donors
(011 and 042), whereas anti-HBs remained reactive (Table 3 and Fig. 1B). In these two donors,
an increase in anti-HBs corresponded to the disappearance of HBsAg. IgM and total anti-HBc became positive on day 107 in one donor (042) and
on day 168 in the other (011). Donor 013 did not
have detectable HBsAg or anti-HBc for 9 months,
but an increase in anti-HBs occurred on day 42,
when HBV DNA became undetectable (Table 3
and Fig. 1B). The fourth donor (003) had received
a plasma-derived HBV vaccine 27 years earlier; her
level of anti-HBs in the index donation (3 IU per
liter) was considered to be nonimmune. HBV
DNA remained detectable for up to 70 days, at
which time IgM and total anti-HBc appeared.
HBsAg was never detected; however, an anamnestic response for anti-HBs was observed in the
first follow-up sample (obtained on day 20). A fifth
vaccinated donor (001) was negative for anti-HBs
at baseline but had seroconversion (100 IU per
liter) within 45 days, a finding that was consistent with an anamnestic response, since it preceded the detection of total and IgM anti-HBc by
up to 24 days. Despite the detection of IgM antiHBc in four of the five vaccinated donors, no
increased levels of alanine aminotransferase
were noted, which further substantiated the inconsequential nature of these infections.
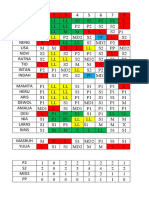
HBV genotypes or subgenotypes of the 6 vaccinated donors were C2 (in donor 001), A2 (in
donor 003), F1 (in donor 011), B2 (in donor 013),
and sequences representing both D and A2 (in
donors 029 and 042), as compared with A2 in all
unvaccinated donors (P=0.048 by Fishers exact
test, two-tailed, for the comparison between the
dominant strains in the 6 vaccinated donors and
in the 3 unvaccinated donors) (Table 3 and Fig. 2,
and the Supplementary Appendix). Figure 3 shows
the levels of anti-HBs in 520 randomly selected
donors who were not infected with HBV. Of the
231 immune donors in this subgroup (44%), more
than 65% were 29 years of age or younger, which
was consistent with the mean age of 26 years for
the 9 donors with HBV infection, of whom 6 had
also been vaccinated.
have HBV infection. In all cases, the sequences of
the presurface and surface (pre-S/S) regions of
the HBsAg gene were nearly identical at the nucleotide level (<0.1% divergence) and the amino
acid level in two laboratories, as were the full
genome sequences in donor 013 and his sexual
partner, which strongly suggests that infection
occurred between vaccinated donors and their
sexual partners who carried high viral loads
(>1.0106 IU per milliliter) (Table 3). All these
partners were highly positive for HBsAg and
anti-HBc but were negative for anti-HBs and IgM
anti-HBc, indicating chronic carriage. Three of
the four partners had mild alanine aminotransferase elevations (range, 31 to 38 U per liter),
which were consistent with chronic hepatitis B.
The transfer of a mutated minority variant to one
donor (001) from his partner further confirms
sexual transmission and immune selection. The
fifth and sixth vaccinated donors were health
care workers whose acute infections were probably the result of occupational exposure.
Discussion
Analysis of the results of blood-donor testing,
along with follow-up analyses of infected donors,
permits assessment of the details of early infection and modeling of the residual risk of infectivity from transfusion.13,18 In this study, we found
some unexpected patterns of early HBV infection
as a result of evaluating HBV nucleic acid testing
among 3.7 million blood donations. On the basis
of modeling studies, we anticipated two to four
seronegative, HBV DNApositive samples from
minipool nucleic acid testing and one seronegative,
HBV DNApositive sample from single-donation
testing.14 In fact, we found nine seronegative,
HBV DNApositive samples, and all but one were
detected on minipool nucleic acid testing, for a
total rate of 1 per 410,540 donations. Three of
the infected donors appeared to have conventional window-period infection, which was consistent with expected findings. Unexpectedly, five
of the other six infected donors had low-level
anti-HBs (3 to 96 IU per liter) or a rapid anamnestic response, attributable to the receipt of HBV
vaccine 7 to 27 years earlier. The five vaccinated
donors had a brief, transient course of infection
Origin of HBV Infection
with no evidence of disease and very low or abThe sexual partners of infected donors were sent expression of HBsAg. Viremia, which was of
traced when possible, and four were found to short duration, ranged from 11 to 86 IU per millin engl j med 364;3 nejm.org january 20, 2011
The New England Journal of Medicine
Downloaded from nejm.org at UC SHARED JOURNAL COLLECTION on July 5, 2012. For personal use only. No other uses without permission.
Copyright 2011 Massachusetts Medical Society. All rights reserved.
243
The
n e w e ng l a n d j o u r na l
ABO36920
74
61
100
100
90
A1
A3
S50225
V00866
X70185
AY233286f
Cons ARC074 ind
90
ARC074-ind-cam
ARC029-ind-cam
ARC029 cl7
ARC029 cl3
ARC029 cl1
75
Cons ARC019 ind
ARC019-ind-cam
ARC029 cl5
AB056513
AB064311
AB056515
70
97
100
100
100
100
244
m e dic i n e
M32138
Z35716
U9551
ARC042 cl6
ARC042 cl4
100
ARC042 cl3
ARC042 cl2
68 ARC042 cl7
ARC042-ind-cam
ARC042 cl9
100
X02496
ARC029 cl11
ARC029 cl9
74
100 ARC029 cl4
ARC029 cl2
ARC029 cl6
ARC042 cl12
100
ARC042 cl8
ARC029 cl10
ARC029 cl8
M54923
D23678
D50522
98
Cons ARC013 ind
100 Cons ARC013 part
ARC013-ind-cam
ARC013-part-cam
M38636
D23680
D50519
Cons ARC001 part
100
ARC001-part-cam
98
Cons ARC001 ind
M57663
74
AY934772
AY934773
AY233290
AB194949
98
AB194950
Z35717
Z72478
AB116077
ARC042 cl5
ARC042 cl1
Cons ARC003 ind
Cons ARC003 part
80
Cons ARC055 ind
ARC055-ind-cam
ARC003-ind-cam
ARC003-part-cam
100
AY090457
AY090454
Cons ARC011 part
100
ARC011-part-cam
ARC011-ind-cam
X75658
X69798
X75663
AB036910
of
AB091256
AB091255
AB106564
X75664
X75657
A2
G
E
F
Scale bar indicates
0.005 nucleotide
substitutions per site.
n engl j med 364;3 nejm.org january 20, 2011
The New England Journal of Medicine
Downloaded from nejm.org at UC SHARED JOURNAL COLLECTION on July 5, 2012. For personal use only. No other uses without permission.
Copyright 2011 Massachusetts Medical Society. All rights reserved.
Nucleic Acid Testing to Detect HBV in Blood
Figure 2 (facing page). Phylogenetic Analysis of Nine
Index Blood Donors and Their Sexual Partners in a
1200-Nucleotide Region, Including the Pre-S/S Gene.
Individual strains that are included in the study are shown
in red, and genotype references from GenBank are shown
in black. Study samples are coded as ARC (indicating the
American Red Cross), followed by a three-digit code number. The abbreviation ind indicates an index sample,
and part indicates a sample from a sexual partner of
an index donor. Sample codes ending with cam indicate consensus sequences obtained in the Cambridge
laboratory. Sample codes preceded by cons indicate
consensus of all clones obtained at the Giessen laboratory
for a particular strain. For the two samples that were identified as being coinfected with two different genotypes,
cl plus a number indicates the clone number within a
sample quasispecies. In all cases, consensus sequences
that were obtained either in Cambridge or in Giessen were
identical or differed by fewer than three nucleotides. The
letters to the right of the strains indicate the HBV genotype (B through H) or subgenotype (A1, A2, and A3). The
numbers to the left of the strains indicate genomic distance calculations (bootstrap values in percentages), in
which values of more than 70% are considered to be significantly different.
liter at donation. Four of the five vaccinated donors who were followed were also positive for
IgM anti-HBc, confirming acute infection. Smaller
studies in the United States have typically shown
approximately one HBV-infected donor per 600,000
donations screened.15 In countries where HBV infection is endemic, rates are much higher.10,19
The three acute infections among nonvaccinated donors were of subgenotype A2, which is
the most frequent genotype in the United States
and is the parent strain of the HBV vaccine. Elevations in alanine aminotransferase levels developed in two of these donors (119 and 640 U
per liter) during follow-up. In contrast, only one of
the six previously vaccinated donors was uniquely
infected with the A2 strain; she had received the
plasma-derived vaccine 27 years earlier. All other
donors were infected exclusively or predominantly with non-A2 strains. None of the vaccinated donors had any signs of elevated levels of
alanine aminotransferase. Overall, the data emphasize the protective effect of the vaccine, since
the observed infections were transient, blunted,
and without effect on liver function. Our findings thus suggest that the vaccine may be less
effective for non-A2 infections. Of interest, four
donors with acute HBV infection were discovered to have sexual partners who were chronic
HBV carriers with high viral loads of wild-type
(or in one case, mutated) HBV DNA. These infected donors had the same subgenotype and
full genome sequences compatible with transmission.
The blood of donors with acute HBV DNA
positive infection during the window period is
likely to be highly infectious in transfusion recipients.11,12 The significance of infection in
vaccinated donors is less clear. In one study,
blood donations that were positive for HBV DNA
with detectable levels of anti-HBs were not infectious in any of 22 recipients, as compared with
a rate of infection of 27% among 37 recipients
of blood that was devoid of anti-HBs.11 Similarly,
the absence of infectivity in the presence of antiHBs has been observed in other studies.2,20-23
Conversely, blood containing HBV DNA with
low-level anti-HBs (<75 IU per liter) may carry
a risk of transmission leading to acute hepatitis.24 These study findings may be relevant to
decisions about the need to implement screening
for HBV DNA among blood donors.
The rates of RNA-positive HIV and HCV infection among seronegative donations in our study
(1 in 1.85 million for HIV and 1 in 246,000 for
HCV) parallel those observed by the American
Red Cross among more than 66 million donations tested in the 10 years since the introduction of nucleic acid testing for HIV and HCV (32
HIV-positive donations, or 1 in 2 million, and
244 HCV-positive donations, or 1 in 270,000)18
and are consistent with earlier reports.25 The
characteristics of the 15 donors with HCV infection and the 2 donors with HIV infection in our
study were similar to those reported previously.18
The infrequent detection of transfusiontransmitted infection contributes to the low
cost-effectiveness of nucleic acid testing (for details, see the Supplementary Appendix).26,27 During 10 years of nucleic acid testing for HIV and
HCV in the United States, five HIV-infected donors have transmitted the virus to six of eight
living transfusion recipients. Two recipients were
infected by one donor, and two other windowperiod donors each infected one recipient. In
two cases, only one of two living recipients became infected; of these last two cases of differential transmission (i.e., in which one recipient
became infected and the other did not), one case
is unpublished.28-31 In contrast, there has been
n engl j med 364;3 nejm.org january 20, 2011
The New England Journal of Medicine
Downloaded from nejm.org at UC SHARED JOURNAL COLLECTION on July 5, 2012. For personal use only. No other uses without permission.
Copyright 2011 Massachusetts Medical Society. All rights reserved.
245
The
n e w e ng l a n d j o u r na l
of
m e dic i n e
1000
900
800
Anti-HBs (U/liter)
700
600
500
400
300
200
100
0
50
100
150
200
250
300
350
400
450
500
Donor Number
Figure 3. Levels of Antibodies against Hepatitis B Surface Antigen (Anti-HBs) in 520 Randomly Selected Samples
from U.S. Blood Donors.
Shown are results for 520 blood donors who tested negative for hepatitis B virus (HBV) DNA, hepatitis B surface
antigen (HBsAg), and antibodies against hepatitis B core antigen (anti-HBc), plotted in order of increasing level of
anti-HBs antibodies. Each symbol represents an individual donor; 44% of donors were considered to have immunity
against HBV (i.e., an anti-HBs value of 10 IU per liter or more). The arrows indicate anti-HBs levels that correspond
to values for the six HBV-vaccinated study donors who were found to be positive for HBV DNA: negative, 3, 11, 33,
43, and 96 IU per liter.
only one report of suspected transmission of HCV
through transfusion.32 For HBV, there has been
no documentation of transmission through transfusion in the United States since the introduction of ultrasensitive screening for HBsAg in
2006. The two cases of differential transmission
of HIV that were observed by the American Red
Cross, in which a high-volume plasma component transmitted the virus but packed red cells
containing low amounts of plasma did not, indicate that the sensitivity of nucleic acid testing,
even in minipools, may approach the threshold
for infection. In any event, since the implementation of nucleic acid testing and sensitive serologic assays, viral transmission by transfusion
from donors who previously had negative results
on both serologic and nucleic acid testing is a rare
finding27 (for details, see the Supplementary Appendix).
In summary, this study showed a higherthan-expected rate of HBV infection with the use
246
of triplex nucleic acid testing, mainly in donors
who had been vaccinated against HBV and who
would not have been identified by routine screening for HBsAg or anti-HBc. However, these acute
HBV infections rapidly resolved and are of inconsequential clinical significance, but their potential for transmission remains unresolved. Our
findings show the efficacy of the HBV vaccine
for the prevention of clinical disease but not
infection, and the cost of interdicting donations
that contain HBV DNA from seronegative donors
is high in the face of unknown benefit. Because
of the high cost of introducing new screening
assays for blood donors and the inability to document cost-effectiveness similar to that of other
medical interventions, the continued development of new tests either to replace older tests or
to detect newly identified agents33 is in question.
Supported by the American Red Cross, Novartis Diagnostics,
and Gen-Probe and by grants from the Eugene B. Casey Foundation and the William and Sonya Carpenter Fund (to Dr. Hollinger), from the Robert Koch Institute (to Ms. Wend and Dr.
n engl j med 364;3 nejm.org january 20, 2011
The New England Journal of Medicine
Downloaded from nejm.org at UC SHARED JOURNAL COLLECTION on July 5, 2012. For personal use only. No other uses without permission.
Copyright 2011 Massachusetts Medical Society. All rights reserved.
Nucleic Acid Testing to Detect HBV in Blood
Gerlich), and from the U.K. National Health Service Blood and
Transplant (to Dr. Candotti). Abbott Laboratories and Bio-Rad
Laboratories provided additional testing support.
Disclosure forms provided by the authors are available with
the full text of this article at NEJM.org.
We thank Rebecca L. Townsend and David E. Krysztof of the
Scientific Support Office of the American Red Cross and Jaye P.
Brodsky of Quality Analytics for managing the study database
and follow-up of donors and partners, the American Red Cross
staff and staff at Community Blood Centers of Florida for their
participation in the study, and Adrian Fisher for assistance in
the preparation of the manuscript.
References
1. Hoofnagle JH, Seeff LB, Bales ZB,
Zimmerman HJ. Type B hepatitis after
transfusion with blood containing antibody to hepatitis B core antigen. N Engl J
Med 1978;298:1379-83.
2. Mosley JW, Stevens CE, Aach RD, et
al. Donor screening for antibody to hepatitis B core antigen and hepatitis B virus
infection in transfusion recipients. Transfusion 1995;35:5-12.
3. Stevens CE, Aach RD, Hollinger FB, et
al. Hepatitis B virus antibody in blood donors and the occurrence of non-A, non-B
hepatitis in transfusion recipients: an
analysis of the Transfusion-Transmitted
Viruses Study. Ann Intern Med 1984;
101:733-8.
4. Mosley JW, Huang W, Stram DO, et al.
Donor levels of serum alanine aminotransferase activity and antibody to hepatitis B core antigen associated with recipient hepatitis C and non-B, non-C
outcomes. Transfusion 1996;36:776-81.
[Erratum, Transfusion 1997;37:109.]
5. Raimondo G, Allain JP, Brunetto MR,
et al. Statements from the Taormina expert meeting on occult hepatitis B virus
infection. J Hepatol 2008;49:652-7.
6. Hollinger FB. Hepatitis B virus infection and transfusion medicine: science and
the occult. Transfusion 2008;48:1001-26.
7. Yoshikawa A, Gotanda Y, Minegishi K,
et al. Lengths of hepatitis B viremia and
antigenemia in blood donors: preliminary
evidence of occult (HBsAg-negative) infection in the acute stage. Transfusion
2007;47:1162-71.
8. Manzini P, Abate ML, Valpreda C, et al.
Evidence of acute primary occult hepatitis
B virus infection in an Italian repeat
blood donor. Transfusion 2009;49:75764.
9. Bremer CM, Saniewski M, Wend UC,
et al. Transient occult hepatitis B virus
infection in a blood donor with high viremia. Transfusion 2009;49:1621-9.
10. Phikulsod S, Oota S, Tirawatnapong
T, et al. One-year experience of nucleic
acid technology testing for human immunodeficiency virus Type 1, hepatitis C virus, and hepatitis B virus in Thai blood
donations. Transfusion 2009;49:1126-35.
11. Satake M, Taira R, Yugi H, et al. Infectivity of blood components with low hepatitis B virus DNA levels identified in a
lookback program. Transfusion 2007;47:
1197-205.
12. Tabuchi A, Tanaka J, Katayama K, et
al. Titration of hepatitis B virus infectivity
in the sera of pre-acute and late acute
phases of HBV infection: transmission
experiments to chimeric mice with human liver repopulated hepatocytes. J Med
Virol 2008;80:2064-8.
13. Zou S, Stramer SL, Notari EP, et al.
Current incidence and residual risk of
hepatitis B infection among blood donors
in the United States. Transfusion 2009;
49:1609-20.
14. Center for Biologics Evaluation and
Research. Blood Products Advisory Committee, 94th Meeting, Gaithersburg, MD,
April 1, 2009 (transcript). (http://www.fda
.gov/downloads/AdvisoryCommittees/
CommitteesMeetingMaterials/Blood
VaccinesandOtherBiologics/BloodProducts
AdvisoryCommittee/UCM155628.pdf.)
15. Linauts S, Saldanha J, Strong DM.
PRISM HBsAg detection of hepatitis B virus minipool nucleic acid testing yield
samples. Transfusion 2008;48:1376-82.
16. OBrien SF, Xi G, Fan W, et al. Epidemiology of hepatitis B in Canadian blood
donors. Transfusion 2008;48:2323-30.
17. Daniels D, Grytdal S, Wasley A. Surveillance for acute viral hepatitis United States, 2007. MMWR Surveill Summ
2009;58:1-27.
18. Zou S, Dorsey KA, Notari EP, et al.
Prevalence, incidence, and residual risk of
human immunodeficiency virus and hepatitis C virus infections among United
States blood donors since the introduction of nucleic acid testing. Transfusion
2010;50:1495-504.
19. Hollinger FB, Sood G. Occult hepa
titis B virus infection: a covert operation.
J Viral Hepat 2010;17:1-15. [Erratum, J Viral Hepat 2010;17:600.]
20. Aach RD, Alter HJ, Hollinger FB, et al.
Risk of transfusing blood containing
a ntibody to hepatitis-B surface antigen.
Lancet 1974;2:190-3.
21. Prince AM, Lee DH, Brotman B. Infectivity of blood from PCR-positive, HBsAgnegative, anti-HBs-positive cases of resolved hepatitis B infection. Transfusion
2001;41:329-32.
22. Dreier J, Krger M, Diekmann J, Gtting C, Kleesiek K. Low-level viraemia of
hepatitis B virus in an anti-HBc- and antiHBs-positive blood donor. Transfus Med
2004;14:97-103.
23. Gerlich WH. Breakthrough of hepatitis B virus escape mutants after vaccination and virus reactivation. J Clin Virol
2006;36:Suppl 1:S18-S22.
24. Levicnik-Stezinar S, Rahne-Potokar U,
Candotti D, Lelie N, Allain JP. Anti-HBs
positive occult hepatitis B virus carrier
blood infectious in two transfusion recipients. J Hepatol 2008;48:1022-5.
25. Stramer SL, Glynn SA, Kleinman SH,
et al. Detection of HIV-1 and HCV infections among antibody-negative blood donors by nucleic acidamplification testing. N Engl J Med 2004;351:760-8.
26. Jackson BR, Busch MP, Stramer SL,
AuBuchon JP. The cost-effectiveness of NAT
for HIV, HCV, and HBV in whole-blood
donations. Transfusion 2003;43:721-9.
27. Kleinman SH, Lelie N, Busch MP. Infectivity of human immunodeficiency
virus-1, hepatitis C virus, and hepatitis B
virus and risk of transmission by transfusion. Transfusion 2009;49:2454-89.
28. Delwart EL, Kalmin ND, Jones TS,
et al. First report of human immunodeficiency virus transmission via an RNAscreened blood donation. Vox Sang 2004;
86:171-7.
29. Phelps R, Robbins K, Liberti T, et al.
Window-period human immunodeficiency
virus transmission to two recipients by an
adolescent blood donor. Transfusion 2004;
44:929-33.
30. Stramer SL, Chambers L, Page PL,
Wagner AG, Gibble J. Third reported US
case of breakthrough HIV transmission
from NAT screened blood. Transfusion
2003;43:Suppl:40A-41A. abstract.
31. Laffoon B, Crutchfield A, Levi M, et al.
HIV transmission through transfusion
Missouri and Colorado, 2008. Morb Mortal Wkly Rpt 2010;59:1335-9.
32. Taylor C, Price TH, Strong DM. Possible HCV transmission from blood
screened by pooled nucleic acid testing.
Transfusion 2002;42:Suppl:9S. abstract.
33. Stramer SL, Hollinger FB, Katz LM,
et al. Emerging infectious disease agents
and their potential threat to transfusion
safety. Transfusion 2009;49:Suppl 2:1S29S.
Copyright 2011 Massachusetts Medical Society.
n engl j med 364;3 nejm.org january 20, 2011
The New England Journal of Medicine
Downloaded from nejm.org at UC SHARED JOURNAL COLLECTION on July 5, 2012. For personal use only. No other uses without permission.
Copyright 2011 Massachusetts Medical Society. All rights reserved.
247
Das könnte Ihnen auch gefallen
- Venipuncture Course 02 10 SDokument172 SeitenVenipuncture Course 02 10 SAnton Scheepers100% (2)
- Liver Disease With PregnancyDokument115 SeitenLiver Disease With PregnancyAmro Ahmed Abdelrhman100% (3)
- Answers To Virology MCQ Paper 2Dokument8 SeitenAnswers To Virology MCQ Paper 2Idrissa ContehNoch keine Bewertungen
- Needlestick InjuryDokument24 SeitenNeedlestick InjuryAli AlisonNoch keine Bewertungen
- ThalassemiaDokument45 SeitenThalassemiaShella Novita100% (3)
- Hepatitis B in PregnancyDokument23 SeitenHepatitis B in PregnancyBrooly Denfrek100% (1)
- Hepatitis B: The Immaculate Infection: Annmarie Huysman, MD Mitul Patel, MD Douglas T. Dieterich, MDDokument7 SeitenHepatitis B: The Immaculate Infection: Annmarie Huysman, MD Mitul Patel, MD Douglas T. Dieterich, MDEnwunlu Bosso ThomasNoch keine Bewertungen
- Jana-2018-ABO & RH Blood Groups' DistributionDokument6 SeitenJana-2018-ABO & RH Blood Groups' DistributionKemo JakNoch keine Bewertungen
- Occult HBVDokument5 SeitenOccult HBVsoumenNoch keine Bewertungen
- Hepatitis B Surface Antigen Seroclearance in Patients With Chronic Hepatitis B Infection: A Clinical StudyDokument8 SeitenHepatitis B Surface Antigen Seroclearance in Patients With Chronic Hepatitis B Infection: A Clinical StudylizzykinasihNoch keine Bewertungen
- Long-Term Outcomes of Hbsag/ Anti-Hbs Double-Positive Versus Hbsag Single-Positive Patients With Chronic Hepatitis BDokument7 SeitenLong-Term Outcomes of Hbsag/ Anti-Hbs Double-Positive Versus Hbsag Single-Positive Patients With Chronic Hepatitis BTheresia IlyanNoch keine Bewertungen
- Palacios 1999Dokument6 SeitenPalacios 1999awdafeagega2r3Noch keine Bewertungen
- Medip,+1214 4749 1 CEDokument5 SeitenMedip,+1214 4749 1 CEJuliana Menara de Souza MarquesNoch keine Bewertungen
- Hepatitis B Serological Markers and Plasma DNA ConDokument9 SeitenHepatitis B Serological Markers and Plasma DNA ConSerendipity21Noch keine Bewertungen
- AhmadDokument7 SeitenAhmad성운하Noch keine Bewertungen
- Dr. Manoj KumarDokument7 SeitenDr. Manoj KumarPatna Journal of MedicineNoch keine Bewertungen
- A Rapid Immunochromatographic Assay For Hepatitis B Virus ScreeningDokument4 SeitenA Rapid Immunochromatographic Assay For Hepatitis B Virus ScreeningIcha Gaker'sNoch keine Bewertungen
- Effectiveness of Blood Donor Screening by Hiv, HCV, Hbv-Nat Assays, As Well As Hbsag and Anti-Hbc Immunoassays in Germany (2008 - 2015)Dokument8 SeitenEffectiveness of Blood Donor Screening by Hiv, HCV, Hbv-Nat Assays, As Well As Hbsag and Anti-Hbc Immunoassays in Germany (2008 - 2015)Syifa Nabila DewantyNoch keine Bewertungen
- Anti HCVDokument5 SeitenAnti HCVFaisal JamshedNoch keine Bewertungen
- The Natural History of Hepatitis C Virus Infection: Host, Viral, and Environmental FactorsDokument0 SeitenThe Natural History of Hepatitis C Virus Infection: Host, Viral, and Environmental FactorsAnis Ur RahmanNoch keine Bewertungen
- J. Clin. Microbiol.-1992-Thieme-1076-9Dokument5 SeitenJ. Clin. Microbiol.-1992-Thieme-1076-9Debby ApriliaNoch keine Bewertungen
- 2003 Theodossiades HaemophiliaDokument3 Seiten2003 Theodossiades HaemophilialeandrosarvanitakisNoch keine Bewertungen
- MR 06022Dokument3 SeitenMR 06022olfianyNoch keine Bewertungen
- Cambios en El Diagnostico de Hepatitis C-Jama 2014Dokument2 SeitenCambios en El Diagnostico de Hepatitis C-Jama 2014Joe Felipe Vera OchoaNoch keine Bewertungen
- Anti HCVDokument6 SeitenAnti HCVFaisal JamshedNoch keine Bewertungen
- Occult Hepatitis B Virus Infection: A Hidden Menace?: EditorialsDokument3 SeitenOccult Hepatitis B Virus Infection: A Hidden Menace?: EditorialsrabiaqibaNoch keine Bewertungen
- Annex 5.3 PICO 1 - How To Test (HBV) Diagnostic Accuracy of Tests To Detect Hepatitis B Surface Antigen: A Meta-Analysis and Review of The LiteratureDokument78 SeitenAnnex 5.3 PICO 1 - How To Test (HBV) Diagnostic Accuracy of Tests To Detect Hepatitis B Surface Antigen: A Meta-Analysis and Review of The LiteratureWini LugasNoch keine Bewertungen
- NIH Public Access: Author ManuscriptDokument9 SeitenNIH Public Access: Author ManuscriptNunun Utheah Udaada YgPoenyaNoch keine Bewertungen
- Oral BiologyDokument4 SeitenOral BiologyDebby ApriliaNoch keine Bewertungen
- Journal Metode - Nucleic - Acid - Amrun Kali... (TBD2001103)Dokument9 SeitenJournal Metode - Nucleic - Acid - Amrun Kali... (TBD2001103)Nada Fadhilah IryonoNoch keine Bewertungen
- Urnal Vox Sanguinis - 2023 - Pons - Prevalence of Red Blood Cell Alloantibodies Among Blood Donors in The French Military BloodDokument5 SeitenUrnal Vox Sanguinis - 2023 - Pons - Prevalence of Red Blood Cell Alloantibodies Among Blood Donors in The French Military BloodFauzan.ANoch keine Bewertungen
- Screening For Hepatitis C Virus InfectionDokument16 SeitenScreening For Hepatitis C Virus InfectionFaisal JamshedNoch keine Bewertungen
- Get PDFDokument6 SeitenGet PDFDarko MaksimovicNoch keine Bewertungen
- Inter Vens IDokument6 SeitenInter Vens Irudy bilontaloNoch keine Bewertungen
- Hepatitis C PD HDDokument7 SeitenHepatitis C PD HDAdi SuciptoNoch keine Bewertungen
- Hepatitis B and C Coinfection in A Real-Life Setting: Viral Interactions and Treatment IssuesDokument6 SeitenHepatitis B and C Coinfection in A Real-Life Setting: Viral Interactions and Treatment IssuesFiorella Portella CordobaNoch keine Bewertungen
- Incidentally Detected HBsAg Positive SubjectsDokument7 SeitenIncidentally Detected HBsAg Positive SubjectsKhumairaNoch keine Bewertungen
- Hepatitis B Testing Guide 1Dokument4 SeitenHepatitis B Testing Guide 1Piyush MalikNoch keine Bewertungen
- 1 s2.0 S120197120801374X MainDokument6 Seiten1 s2.0 S120197120801374X MainRia GandaNoch keine Bewertungen
- Lupus ActiveDokument5 SeitenLupus ActivedeliaNoch keine Bewertungen
- Management of Chronic Hepatitis B - An Overview of Practice Guidelines For Primary Care ProvidersDokument16 SeitenManagement of Chronic Hepatitis B - An Overview of Practice Guidelines For Primary Care Providersdanny17phNoch keine Bewertungen
- Hepati Tac AbstractDokument296 SeitenHepati Tac AbstractMagda MagNoch keine Bewertungen
- Hepatitis E Virus Seropositivity in An Ethnically Diverse Community Blood Donor PopulationDokument7 SeitenHepatitis E Virus Seropositivity in An Ethnically Diverse Community Blood Donor Populationadmir4Noch keine Bewertungen
- Research Papers On HCV PDFDokument5 SeitenResearch Papers On HCV PDFafmdcwfdz100% (1)
- Blood Donors and Blood CollectionDokument7 SeitenBlood Donors and Blood CollectionPritha BhuwapaksophonNoch keine Bewertungen
- Anti HCVDokument3 SeitenAnti HCVFaisal JamshedNoch keine Bewertungen
- Li2017 PDFDokument9 SeitenLi2017 PDFntnquynhproNoch keine Bewertungen
- Li 2017Dokument9 SeitenLi 2017ntnquynhproNoch keine Bewertungen
- Its Correlation With HBV DNADokument6 SeitenIts Correlation With HBV DNAbread maniacNoch keine Bewertungen
- Jurnal 1Dokument7 SeitenJurnal 1Nur Alifah Dina SNoch keine Bewertungen
- Blood Transfusion Therapy Ward Class 2020Dokument18 SeitenBlood Transfusion Therapy Ward Class 2020Sharl Bea EsmeraldaNoch keine Bewertungen
- Detection of Babesia RNA and DNA in Whole Blood Samples From US Blood DonationsDokument12 SeitenDetection of Babesia RNA and DNA in Whole Blood Samples From US Blood DonationsEnrique Salvador Padial RamosNoch keine Bewertungen
- Zheng 2014Dokument11 SeitenZheng 2014EkanshNoch keine Bewertungen
- 05 - CL Bioch 2008Dokument7 Seiten05 - CL Bioch 2008sunilpkumar18Noch keine Bewertungen
- GBV-C - HGV Infection in Hepatitis C Virus-Infected Deferred Swedish Blood Donors (Journal of Medical Virology, Vol. 54, Issue 2) (1998)Dokument5 SeitenGBV-C - HGV Infection in Hepatitis C Virus-Infected Deferred Swedish Blood Donors (Journal of Medical Virology, Vol. 54, Issue 2) (1998)Ahmed MagzoubNoch keine Bewertungen
- Keeffe 2006Dokument27 SeitenKeeffe 2006Maymay DamayNoch keine Bewertungen
- tmp4886 TMPDokument5 Seitentmp4886 TMPFrontiersNoch keine Bewertungen
- Profile of Blood Donors With Serologic Tests Reactive For The Presence of Syphilis in São Paulo, BrazilDokument7 SeitenProfile of Blood Donors With Serologic Tests Reactive For The Presence of Syphilis in São Paulo, BrazilPritha BhuwapaksophonNoch keine Bewertungen
- Pontisso1996 PDFDokument4 SeitenPontisso1996 PDFAraceli EnríquezNoch keine Bewertungen
- Heart and Lung TransplantsDokument12 SeitenHeart and Lung TransplantsferNoch keine Bewertungen
- Clinical Practice and Epidemiology in Mental HealthDokument5 SeitenClinical Practice and Epidemiology in Mental HealthMiguel Angel Arreola SotoNoch keine Bewertungen
- Correlation of Serological Biochemical and MoleculDokument6 SeitenCorrelation of Serological Biochemical and MoleculPratibha sharmaNoch keine Bewertungen
- ID Uji Saring Antigen Dan Antibodi Hepatitis C Virus Pada Darah DonorDokument6 SeitenID Uji Saring Antigen Dan Antibodi Hepatitis C Virus Pada Darah DonorIna YMNoch keine Bewertungen
- Handajani 2019 IOP Conf. Ser. Earth Environ. Sci. 217 012051 PDFDokument8 SeitenHandajani 2019 IOP Conf. Ser. Earth Environ. Sci. 217 012051 PDFCitrawati Dyah Kencono WunguNoch keine Bewertungen
- Content ServerDokument11 SeitenContent ServerRamayanaNoch keine Bewertungen
- Hepatitis B Virus and Liver DiseaseVon EverandHepatitis B Virus and Liver DiseaseJia-Horng KaoNoch keine Bewertungen
- MEIDokument27 SeitenMEIPutri Kusuma WardaniNoch keine Bewertungen
- Pengecekan Troli Zona Sebulan SekaliDokument8 SeitenPengecekan Troli Zona Sebulan SekaliPutri Kusuma WardaniNoch keine Bewertungen
- Juni Udah KeknyaDokument24 SeitenJuni Udah KeknyaPutri Kusuma WardaniNoch keine Bewertungen
- 44935Dokument12 Seiten44935Putri Kusuma WardaniNoch keine Bewertungen
- Strategic PlanningDokument19 SeitenStrategic PlanningPutri Kusuma WardaniNoch keine Bewertungen
- Coronary Artery DiseaseDokument13 SeitenCoronary Artery DiseaseChristianHanjokarNoch keine Bewertungen
- Checklist DRPDokument16 SeitenChecklist DRPPutri Kusuma WardaniNoch keine Bewertungen
- DRP DM With HTDokument20 SeitenDRP DM With HTPutri Kusuma WardaniNoch keine Bewertungen
- CDC - Concept - HrqolDokument3 SeitenCDC - Concept - HrqolPutri Kusuma WardaniNoch keine Bewertungen
- Layout SKMFDokument1 SeiteLayout SKMFPutri Kusuma WardaniNoch keine Bewertungen
- Interpretation of Hepatitis B Serologic Test ResultsDokument1 SeiteInterpretation of Hepatitis B Serologic Test ResultsMUHAMMAD JAWAD HASSANNoch keine Bewertungen
- Osteo Guidelines 2010Dokument37 SeitenOsteo Guidelines 2010Omar Castilla FariasNoch keine Bewertungen
- Project ECHO Hepatitis C Clinical GuidelinesDokument42 SeitenProject ECHO Hepatitis C Clinical GuidelinesRobert G. Gish, MDNoch keine Bewertungen
- Hepatitis b-1Dokument7 SeitenHepatitis b-1api-550162163Noch keine Bewertungen
- Cirrhosis Hepatis 1Dokument48 SeitenCirrhosis Hepatis 1Muhammad RivaileNoch keine Bewertungen
- Model Paper 9Dokument6 SeitenModel Paper 9Dr-Sanjay SinghaniaNoch keine Bewertungen
- Hepatitis B (Paush, 24)Dokument4 SeitenHepatitis B (Paush, 24)suwashNoch keine Bewertungen
- 2003 - General Medicine and Surgery For Dental Practitioners Part 5 - Liver DiseaseDokument3 Seiten2003 - General Medicine and Surgery For Dental Practitioners Part 5 - Liver DiseaseFlorence LauNoch keine Bewertungen
- Quiz Blood Born Pathogen Refresher Mix Quiz Non ECU Employees and Students and Temporary StaffDokument4 SeitenQuiz Blood Born Pathogen Refresher Mix Quiz Non ECU Employees and Students and Temporary Staffvipin khatriNoch keine Bewertungen
- The Third Factor: Effect Modification Confounding FactorDokument60 SeitenThe Third Factor: Effect Modification Confounding FactorWhina R AymaNoch keine Bewertungen
- Hepatitis D: PathophysiologyDokument2 SeitenHepatitis D: PathophysiologyYanna Habib-MangotaraNoch keine Bewertungen
- 3 s2.0 B9781455748013003301 MainDokument120 Seiten3 s2.0 B9781455748013003301 MainInzamam Ul HaqNoch keine Bewertungen
- Truenat HBVDokument2 SeitenTruenat HBVyousra zeidanNoch keine Bewertungen
- Drug Name Mechanism of Action Indication / Contraindication Adverse Effect Nursing Responsibilities Indications: CnsDokument1 SeiteDrug Name Mechanism of Action Indication / Contraindication Adverse Effect Nursing Responsibilities Indications: CnsSeno HyeonNoch keine Bewertungen
- NCM112 LP2 TransesDokument9 SeitenNCM112 LP2 TransesChristine CalleyNoch keine Bewertungen
- Tacke2016 - Treatment For Hepatitis B in Patients With Drug ResistanceDokument7 SeitenTacke2016 - Treatment For Hepatitis B in Patients With Drug ResistanceClarisa AnindyaNoch keine Bewertungen
- Ambaji Nursing College, Ganeshpura: 2 Year B.Sc. (N) Medical Surgical Nursing-IDokument2 SeitenAmbaji Nursing College, Ganeshpura: 2 Year B.Sc. (N) Medical Surgical Nursing-INEHA PANDEYNoch keine Bewertungen
- Liver FailureDokument10 SeitenLiver FailureLyra LoonNoch keine Bewertungen
- Referat: Tema: Hepatita Virală B. Abordarea de Către Organizația Mondială A Sănătății (WHO)Dokument7 SeitenReferat: Tema: Hepatita Virală B. Abordarea de Către Organizația Mondială A Sănătății (WHO)Nicanor GîscăNoch keine Bewertungen
- MPS Quick Reference Chart 1Dokument3 SeitenMPS Quick Reference Chart 1caseynolanNoch keine Bewertungen
- C-Reactive Protein: Key FactsDokument12 SeitenC-Reactive Protein: Key FactsAngel CañaresNoch keine Bewertungen
- Infectious Disease Flip ChartDokument57 SeitenInfectious Disease Flip Chartapi-373247707Noch keine Bewertungen
- Thomas Bogale TDokument64 SeitenThomas Bogale TAlemayehu KebedeNoch keine Bewertungen
- Table Virology 1Dokument28 SeitenTable Virology 1Virgil CendanaNoch keine Bewertungen
- GI Visuals From Emergency Medicine Board Review For Visual LearnersDokument40 SeitenGI Visuals From Emergency Medicine Board Review For Visual LearnersIanNoch keine Bewertungen
- History of Infections in LabDokument17 SeitenHistory of Infections in LabAslam MuhammadNoch keine Bewertungen