Beruflich Dokumente
Kultur Dokumente
Does Preoperative Predictive Lung Functions Correlates With Post Surgical Lung Functions in Lobectomy?
Hochgeladen von
Editor_IAIMOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Does Preoperative Predictive Lung Functions Correlates With Post Surgical Lung Functions in Lobectomy?
Hochgeladen von
Editor_IAIMCopyright:
Verfügbare Formate
Preoperative and post surgical lung
l
functions in lobectomy
ISSN: 2394-0026 (P)
ISSN: 2394-0034 (O)
Original Research Article
Does preoperative predictive lung functions
correlates with post surgical lung functions
in lobectomy?
Mushtaq Ahmad Mir, Mohammad Akbar Bhat, Farooq Ahmad
Ganie*, Ghulam Nabi Lone, Hafeez ulla Lone
Department of Cardiovascular and Thoracic Surgery, Sher-i-Kashmir
Kashmir Institute of Medical Sciences
(SKIMS), Jammu and Kashmir, India
*Corresponding author email: farooq.ganie@ymail.com
How to cite this article: Mushtaq Ahmad Mir, Mohammad Akbar Bhat, Farooq Ahmad Ganie,
Ghulam Nabi Lone, Hafeez ulla Lone.
Lone Does preoperative predictive lung functions correlates with
post surgical lung functions in lobectomy? IAIM, 2015; 2(3): 126-133.
Available online at www.iaimjournal.com
Received on: 22-02-2015
Accepted on: 07-03-2015
Abstract
Background: Patients with normal pulmonary function tolerate removal of an entire lung without
respiratory problems. In patients with
wit impaired pulmonary function, post resectional function is of
importance for the assessment of surgical risk. This necessitates the ability to measure the relative
contribution of the parenchyma to be resected
ted to the total lung function and the predicted
p
postoperative lung functions.
Objective: To determine preoperative lung functions as assessed with split lung functions and
correlates with postsurgical lung functions and to determine the effect of lung resections on
spirometric lung function.
Material and methods: All those patients planned for lung resection surgery were included in the
study. Predicted postoperative FEV1 and FVC were calculated. Preoperative
Preoperativ spirometry was
performed within
in a week before surgery. Predicted postoperative values were calculated.
Postoperative spirometry was performed at the end of first month, third month, and sixth month for
each patient. The relationship between potential predictors and postoperative complications were
assessed. The predicted values were correlated with measured values (actual values) during the
postoperative follow up.
Results: Lobectomy was donee in 64 persons. The predicted postoperative
postopera
FEV1 and FVC correlated
well with observed FEV1 and FVC in lobectomy (p<.05). The mean preoperative FEV1/L were 1.8 and
the mean predicted postoperative
ostoperative (L) FEV1 were 1.4. The mean FEV1 at 1 month follow up were 1.6
and the mean FEV1 at 3 month follow up were 179.8.
International Archives of Integrated Medicine, Vol. 2, Issue 3, March, 2015.
Copy right 2015,, IAIM, All Rights Reserved.
Rese
Page 126
Preoperative and post surgical lung
l
functions in lobectomy
ISSN: 2394-0026 (P)
ISSN: 2394-0034 (O)
Conclusion: Our study showed that simple calculations based on preoperative pulmonary
pulmonar function
studies correlated well with the actual postoperative FEV1 and FVC forr patients undergoing
lobectomy. This calculation, however, underestimates the actual postoperative FEV1 and FVC by 230
ml in lobectomy.
Key words
Lobectomy, Spirometry, Pulmonary
ulmonary function.
Introduction
The lobar arrangement is defined early in fetal
life. Right lung is divided into three lobes
l
(upper, middle and lower). Left is divided into
two lobes (upper and lower lobes). The right
lung has 10 bronchopulmonary segments and
left lung has 9 bronchopulmonary segments [1].
Lung resection is a therapeutic procedure for
variety of pulmonary diseases that
tha was
introduced by Tuffier in 1891 [2].
Lungs are composed of sections called lobes;
right has three and left has two. When a
complete lobe of lung is removed, it is known as
lobectomy. When entire lung is removed,
removed it is
known as pneumonectomy. The Indications of
lobectomy
includes
Lung
abscess,
Bronchiectasis, Drug resistant tuberculosis,
Mycetoma, Emphysema, Hemoptysis, AV
malformation, Sequestration of lobe/lung,
Adenomyomatosis and
nd Malignant [3, 4] like
Non-small cell carcinoma, Small cell carcinoma,
Metastatic tumours and others.
The pulmonary function tests are done with the
help of spirometer [5, 6]. Spirometry
Spirom
is an
expiratory maneuver. It measures exhaled
volume or vital capacity but does not measure
residual volume, functional residual capacity
capacit or
total lung capacity (TLC). Vital capacity (VC) is a
simple measure of lung volume usually reduced
re
in restrictive disorders. VC is an indirect measure
of other lung volumes. Other tests such a
residual volume, gas diffusion tests,
t
inhalation
challenge test, and exercise
xercise stress tests may also
be performed to determine lung function.
Studies on pulmonary function testing in the
preoperative evaluation for the lung resection
surgery indicate that the following criteria are
predictive
of
increased
postoperat
postoperative
complications
lications and mortality. For lobectomy,
FEV1 <1 L; MVV <40% of predicted; FEF 25-75%
<0.6 L/second and DLCO <50% of predicted.
There is general agreement that at least, the
preoperative pulmonary testing of patients of
whom lung resection is being considered
consider should
include spirometry and arterial blood gases [7].
Split lung function studies [8] showed patients
with normal pulmonary function tolerate
removal of an entire lungg without respiratory
problems. In patients with
th impaired pulmonary
function, however, knowledge of post
resectional function is of importance for the
assessment of surgical risk. This necessitates the
ability to measure the relative contribution of
the parenchyma to be resected to the total lung
function. Kearney, et al.. [9] found the predicted
postoperative FEV1, the only independent
predictor of postoperative complications.
Zeiher, et al. obviates the need for a perfusion
scan by the formula used as below [1, 2, 3, 4, 5,
6, 7, 8, 9, 10].
Predicted postoperative FEV1 or FVC =
preoperative
operative FEV1 or FVC x (1-S
(1 x 1/19).
International Archives of Integrated Medicine, Vol. 2, Issue 3, March, 2015.
Copy right 2015,, IAIM, All Rights Reserved.
Rese
Page 127
Preoperative and post surgical lung
l
functions in lobectomy
Predicted postoperative FEV1 or FVC =
preoperative FEV1 or FVC x (1-S
(1
x
0.0526).
Predicted postoperative FEV1 or FVC =
preoperative FEV1 or FVC x (1-S
(1
x
5.26/100) (where S is the number of
bronchopulmonary
chopulmonary segments to be
removed and 19 the total number of
bronchopulmonary segments)
Postoperative complications were defined as
those occurring within 30 days after surgery
[11]. Present study was aimed to determine
preoperative lung functions as assessed with
split lung functions and correlates with
postsurgical lung functions and to determine the
effect of lung resections on spirometric lung
function.
Material and methods
The
he study was conducted in the Department of
Cardiovascular and Thoracic Surgery,
S
SKIMS,
Srinagar, Kashmir, India on 64 patients. All those
patients who were planned for lung resection
surgery in the Department of Cardiovascular
ardiovascular and
Thoracic Surgery
urgery were included in the study
protocol prospectively. Informed consent was
taken from all cases enrolled for the study.
Besides
routine
investigations,
specific
investigations include pulmonary specific
evaluation (pulmonary function tests) were
done.
Pulmonary specific evaluation was performed in
graded manner to meet the cited goals and
help-risk stratifies the
he patients prior to
anticipate surgery. The first stage of assessment
was spirometry. Spirometeric indices that were
commonly used and have been extensively
ex
studied include FEV1, FVC, FEV1/FVC% and MVV.
Out of all these indices, FEV1 and FVC were
regarded as best for predicting complications of
ISSN: 2394-0026 (P)
ISSN: 2394-0034 (O)
lung resection and were most commonly used
for decision making.
Predicted postoperative FEV1 and FVC were
calculated as per the formulae given below.
Predicted
postoperative
FEV1 =
preoperative FEV1 X [1-(S x 0.0526)]
S = No. of bronchopulmonary segments
resected.
Predicted
redicted
postoperative
FVC
=
preoperative FVC X [1-(S x 0.0526)].
S = No. of bronchopulmonary segments
resected.
Calculation of predicted postoperative FEV1 and
FVC were performed using
ng preoperative data
and information on the number of
bronchopulmonary segments resected was
predicted on the basis of preoperative radiologic
studies (chest X-ray
ray and computed tomography
of chest). Number of bronchopulmonary
segments resected was recorded for each
patient.
Preoperative spirometryy was performed within
with a
week before surgery. Predicted postoperative
values
were
calculated.
Postoperative
spirometry was performed at the end of first
month, third month, and sixth month for each
patient. The relationship
ationship between potential
predictors and postoperative complications
were assessed. The predicted values were
correlated with measured values (actual values)
during the postoperative follow up.
The data was subjected to statistical analysis
using parametric and non-parametric
parametric tests for
comparative evaluation. Besides correlation and
regression, we also assessed the sensitivity of
the predicted postoperative lung functions to
predicted/infer the postoperative complications.
International Archives of Integrated Medicine, Vol. 2, Issue 3, March, 2015.
Copy right 2015,, IAIM, All Rights Reserved.
Rese
Page 128
Preoperative and post surgical lung
l
functions in lobectomy
ISSN: 2394-0026 (P)
ISSN: 2394-0034 (O)
Results
Discussion
The age range of our study of 64 patients was 14
years to 75 years with mean age of 54.6 years.
Most of the patients were farmer by occupation
(41.7%) and student least common (2.9%). The
most common
ommon symptom was cough (73.8%),
(73.8%) the
most common co-morbidity
morbidity was hypertension in
(19.4%)
19.4%) and (76.7%) had history of smoking.
This
his study was conducted in the Department of
Cardiovascular and Thoracic Surgery, Sher-iSher
Kashmir Institute of Medical Sciences, Srinagar,
Srinagar
India, which is the onlyy tertiary care institute of
Jammu and kashmir State. The preoperative
evaluation off patients having lung diseases is a
complex and perplexing problem. It is important
not only to identify the patients with potentially
resectable lung disease, but also to identify
those patients who can or cant tolerate lung
resection. The predicted postoperative
pos
FEV1 and
FVC are the frequently used criteria for defining
physiologic operability.
The most common procedure performed
perfor
was
lower lobectomy (29.1%) and
nd the commonest
indication was squamous cell carcinoma (84%)
and the least common was carcinoid (1.5%). The
most common complication was breathlessness
breathle
(95%). The other complications were
bronchopleural fistula (3.1%), prolonged air leak
(1.6%), pneumonia (1.6%), arrhythmia and death
(1.6%) as per Table 1.
Complications
cations as per predicted values
The most common complication breathlessness
was seen in patients with predicted
postoperative FEV1 <1.45 L and predicted
postoperative FVC <1.67 L (p <0.01).
Bronchopleural fistula, prolonged air leak,
pneumonia, arrhythmia or death was seen in
patients with predicted postoperative FEV1
<0.66 L and predicted
icted postoperative FVC <0.70 L
(p<0.01).
Correlations of predicted postoperative FEV1
with observed FEV1 in lobectomy
Predicted postoperative FEV1 correlated with
observed FEV1 at 1st (r = 0.996),
.996), 3rd (r = 0.995)
and 6th (r = 0.998)
.998) month in the post operative
follow up.
Correlations of predicted postoperative FVC
with observed FVC in lobectomy
Predicted postoperative FVC correlated with
observed FVC at 1st (r = 0.989), 3rd (r = 0.990) and
6th (r = 0.990)
.990) month in the post operative follow
up.
Age distribution and sex distribution
The age range in our series of 64 patients were
14 years to 75 years with a mean age of 54.6
years, study population comprised
compr
of 50 males
and 14 females with a male to female ratio of 4:
1.This corresponds
sponds to the study of Nakahara K
[12] and Zeiher BG, et al. [10
10].
Occupation, presenting
nting symptoms and coco
morbidity
43 patients (67%) were farmer (most common)
and the least common students (4%). The most
common symptom was cough (73.8%) and the
least common was weight loss (1.9%). 19.4%
were hypertensive
ensive and 76.7% were smokers.
This corresponds to the study conducted by
Camili, et al. [13].
Indications
The most common indication for surgery was
squamous cell carcinoma lung (56 patients i.e.
i.e
87%) and the
he least common was carcinoid (1
patient only).
). This is consistent with the study
of Zeiher BG, et al. [10] in which lung resections
were performed forr neoplastic conditions of
lung in majority of cases (56%), lung abscess in
1, tuberculosis in 1 and carcinoid in 4 patients.
International Archives of Integrated Medicine, Vol. 2, Issue 3, March, 2015.
Copy right 2015,, IAIM, All Rights Reserved.
Rese
Page 129
Preoperative and post surgical lung
l
functions in lobectomy
Procedure
Lower lobectomy was performed in 30 patients
(46%) and upper lobectomy in 20 patients (31%)
while middle lobectomy in 5 patients (7.8%).
This corresponds to the study conducted by
Zeiher BG, et al. [10] in which 13
pneumonectomies,
41
lobectomies,
7
bilobectomies and 1 wedge resection were
performed. This is also corresponds to the study
conducted by Markos J, et al.. [5]
[ in which 18
pneumonectomies,
29
lobectomies,
6
thoracotomy without
out resection were performed.
Lung function parameters in lobectomy
Lobectomy was performed in 64 patients. The
measurement of spirometric indices FEV1 and
FVC
was
done
preoperatively
and
postoperatively. The predicted postoperative
FEV1 and FVC were calculated by using simple
segment counting technique given by juhl and
Frost. The actual postoperative FEV1 and FVC
measurement was done at 1, 3 and 6 month.
The mean preoperative FEV1 was 1.8 L. The
mean predicted postoperative FEV1 was 1.4 L,
the mean observed FEV1 at 1 month was 1.6 L,
at 3 month 1.6 L and at 6 months 1.6 L. The
predicted postoperative value FEV1 was
compared with the postoperative measured
values FEV1 att 1 month, 3 month and 6 month.
The predicted postoperative value FEV1
consistently
ntly
underestimated
the
actual
postoperative FEV1 by approximately 158 ml at 1
month (p <0.0001), 180 ml at 3 month (p
<0.0001), and 230.8 mll at 6 month (p<0.0001).
The mean predicted postoperative FVC was 1.6 L
and the mean observed FVC value at 1 month, at
3 month and at 6 month was 1.8 L, 1.8 L and 1.8
L respectively. The predicted postoperative FVC
was compared with the
postoperative
measured
ured values at 1 month, 3 month and at 6
month, the predicted postoperative value FVC
consistently underestimated the mean actual
postoperative FVC by approximately 124 ml at 1
month (p<0.0001), 147 ml at 3 month
ISSN: 2394-0026 (P)
ISSN: 2394-0034 (O)
(p<0.0001) and 185 ml att 6 month (p<0.0001).
(p<0.0001)
This study corresponds to the study conducted
by Zeiher BG, et al. [10] in which predicted
postoperative values were calculated and were
compared with postoperative measured values.
The predicted postoperative FEV1 and FVC
consistently
underestimated
the
actual
postoperative FEV1 and FVC by approximately
250 ml. Our study is consistent with the study
conducted by the Bolliger CT,
CT et al. [14] and
Brunelli, et al. [15] in which predicted
postoperative FEV1 and FVC were compared
with the postoperative measured FEV1 and FVC
values. Both the studies documented
underestimation of postoperative FEV1 and FVC
by 250 ml and 200 ml when predicted
postoperative lung functions were evaluated in
patients of lung resections.
Complications
as
per
the
predicted
postoperative FEV1 and FVC
The most common complication was
breathlessness (grade I and grade II) in 61
patients (95%). The other complications were
bronchopleural fistula, prolonged air leak,
pneumonia, arrhythmiaa or death.
death Breathlessness
(grade II) was seen in patients with predicted
postoperative FEV1 1.4 L (p <0.0001) and
predicted postoperative FVC 1.67 L (p <0.0001).
Bronchopleural fistula, prolonged air leak,
pneumonia, arrhythmia or deaths were seen in
patients
tients with predicted postoperative FEV1
0.66L (p <0.0001) and predicted postoperative
FVC 0.70 L (p <0.0001). This study corresponds
the study conducted by Markos J,
J et al. [5] in
which predicted postoperative FEV1 and FVC
were predictive of postoperative
postoperati complications
indicating death and respiratory failure, the best
predictor of death was predicted postoperative
FEV1.
Bechard, et al. [16] conducted a study in which
criterion for surgical resection included an FEV1
>1.7 L for pneumonectomy, >1.2
> L for lobectomy
International Archives of Integrated Medicine, Vol. 2, Issue 3, March, 2015.
Copy right 2015,, IAIM, All Rights Reserved.
Rese
Page 130
Preoperative and post surgical lung
l
functions in lobectomy
and greater than 0.9 L for wedge resection.
Busch, et al. [17] conducted a study in which
pulmonary complications
tions occurred in 82%
patients. This study is consistent with the study
of Olsen GN, et al. [18] in which predicted
postoperative FEV1 <0.8 L was associated with
complications. Markos J, et al.. [5] reported that
low predicted postoperative FEV1 was
associated with higher mortality and morbidity.
Fujiu K, et al. [19] conducted a study in which
postoperative complications were divided
divide into
two
groups;
oups;
respiratory
complications
(pneumonia/atelectasis))
and
other
complications
ations (bronchopleural fistula/prolonged
fistula/p
air leak/arrhythmia etc.). Postoperative
mortality of 3.9% was reported to be associated
with predicted postoperative FEV1 <40%. The
maximum number of lobectomy patients (94%)
developed breathlessness postoperatively.
postope
Two
patients had bronchopleural fistula, 1 had
prolonged air leak, 1 had pneumonia
pneumon and 1 died
due
to
respiratory
failure.
Among
pneumonectomy
patients,
5
developed
breathlessness, 6 had bronchopleural fistula,
fistu 5
had prolonged air leak, 1 had pneumonia, 1 had
arrhythmia and 4 died
ed due to respiratory failure.
Three patients developed breathlessness in
segmentectomy and 5 patients developed
breathlessness in wedge resection patients. This
study corresponds to the study conducted by
Kearney DJ, et al. [9] in which complications
were seen in 39% of patients undergoing
pneumonectomy, 19% patients undergoing
lobectomy. Our study wass in conformity with
the study of Busch E, et al. [17]] who reported 6
deaths in the entire series of 103 patients, 2 of
which were directly caused by a pulmonary
complication and 1 was due to a contributing
factor. Fujiu K, et al. [19] documented 27%
postoperative respiratory complications in
pneumonectomy patients.
ISSN: 2394-0026 (P)
ISSN: 2394-0034 (O)
Correlations of predicted postoperative FEV1
and FVC with measured postoperative FEV1 and
FVC in lobectomy
The predicted postoperative FEV1 correlated
well with postoperative FEV1 measured values at
1 month (r = 0.996, p <0.001), 3 month (r =
0.995, p <0.0001) and 6 month (r = 0.998, p
<0.0001)
001) in patients of lobectomy. The predicted
postoperative FVC correlated well with
postoperative measured FVC values at 1 month
(r = 0.989, p <0.0001), 3 month (r = 0.990, p
<0.0001) and 6 month (r = 0.998, p <.0001) in
patients of lobectomy. This study corresponds to
the study conducted by Zeiher BG,
BG et al. [10] in
which the actual postoperative FEV1 and FVC
correlated well with the predicted postoperative
FEV1 and FVC for patients undergoing lobectomy
lo
(r = 0.867 and r = 0.832 respectively). Winthida,
et al. [20] conducted a study in which there was
statistically significant correlation (p <0.01)
between the predicted postoperative FEV1 and
FVC and actual postoperative FEV1 and FVC.
Markos J, et al. [5] conducted a study in which
the predictions of postoperative function
correlated well with the measured values at 3
month. For FEV1, r = 0.89 in lobectomy (p
<0.001). This present study establishes beyond
doubt the correlation of predicted postoperative
postopera
FEV1 and FVC with the actual postoperative lung
functions. There
here is direct correlation between
the predicted postoperative lung function with
the incidence/ prevalence of postoperative
complications. These findings hold true
especially for major lung resections.
Conclusion
Our study showed that simple calculations based
on preoperative pulmonary
pulmonar function studies
correlated well with the actual postoperative
FEV1 and FVC forr patients undergoing
lobectomy.
This calculation, however,
underestimates the actual postoperative FEV1
and FVC by 230 ml in lobectomy.
International Archives of Integrated Medicine, Vol. 2, Issue 3, March, 2015.
Copy right 2015,, IAIM, All Rights Reserved.
Rese
Page 131
Preoperative and post surgical lung
l
functions in lobectomy
References
1. Beccaria M, Corisco A, Fulgoni P,
P et al.
Lung cancer resection: The prediction of
postsurgical outcomes should include
long term functional results. Chest,
2001; 120: 37-42.
2. Tuffier T. De le resection du sommet du
poumon. Semin Med Paris, 1891; 2:
202.
3. Weber A, Stammberger U, Dutly A, et al.
Thoracoscopic lobectomy for benign
diseases. Eur J Cardiothorac Surg., 2001;
20: 443-448.
4. Yim APC. VATS major pulmonary
resection revisited. Ann Thorac Surg.,
2002; 74: 615-623.
5. Markos J, Mullan BP, Hillman DR, et al.
Preoperative assessment as a predictor
of mortality and morbidity after lung
resection. Am Rev Respir Dis., 1989;
139: 902-916.
6. Crapo
rapo RO. Pulmonary function testing.
N Eng J Med., 1994; 331: 25-30.
25
7. Datta D, Lahiri B.
Preoperative
evaluation of patients undergoing lung
resection surgery. Chest, 2003; 123(6):
2096-2103.
8. Bolliger CT, Perruchoud AP. Functional
evaluation of the lung
lu
resection
candidate. Eur Respir J., 1998; 11: 198198
212.
9. Kearney DJ, Lee TH, Reilly JJ, et al.
Assessment of operative risk in patients
undergoing lung resection. Chest, 1994;
105: 753-759.
10. Zeiher BG, Gross TJ, Keru JA, et al.
Predicting postoperative pulmonary
functions in patients undergoing lung
resection. Chest, 1995; 108: 68-72.
68
11. Stolz A, Schutzner J, Simonek J, et al.
Comparison
of
postoperative
complications of 60 and 70 year old
ISSN: 2394-0026 (P)
ISSN: 2394-0034 (O)
patients after lung surgery. Interactive
Cardiovascular and Thoracic
Thora
Surgery,
2003; 2: 620-623.
12. Nakahara K, Monden Y, Ohno K, et al. A
method for predicting postoperative
lung function and its relation to
postoperative complications in patients
with lung cancer. Ann Thorac Surg.,
1985; 39: 260-265.
13. Camilli AE, Burrows B, Kndudson RJ, et
al.
Longitudinal changes in forced
expiratory volume in one second in
adults. Am Rev Respir Dis., 1987; 135:
794-799.
14. Bolliger CT, Guckel C, Eugel H, et al.
Prediction of function reserve after lung
resection;
comparision
between
quantitative, computed tomography,
scinitigraphy and anatomy. Respiration,
2002; 69: 482-489.
15. Brunelli A, Refai M, Salati M, et al.
Predicted versus observed FEV1 and
DLCO after major lung resection: A
prospective evaluation at different
postoperative
tive periods. Ann Thorac Surg.,
2007; 83: 1134-1139.
1139.
16. Bechard D, Wetstein Lewis. Assessment
of exercise oxygen consumption as
preoperative criterion for lung resection.
Ann Thorac Surg., 1987; 44: 344-349.
344
17. Busch E, Verazin G, Anthowiak JG, et al.
Pulmonary
ry complications in patients
undergoing thoracotomy for lung
carcinoma. Chest, 1994; 105: 760-766.
760
18. Olsen GN, Block AJ, Tobias JA.
Prediction of post pneumonectomy
pulmonary function using quantitative
macroaggregate
regate lung scanning. Chest,
1974; 66: 13-16.
19. Fujiu K, Kanno R, Suzuki H, et al.
Preoperative pulmonary function as a
predictor of repiratory complications
and mortality in patients under lung
International Archives of Integrated Medicine, Vol. 2, Issue 3, March, 2015.
Copy right 2015,, IAIM, All Rights Reserved.
Rese
Page 132
Preoperative and post surgical lung
l
functions in lobectomy
ISSN: 2394-0026 (P)
ISSN: 2394-0034 (O)
undergoing lobectomy.
Ann Thorac
Surg., 2004; 78: 1215-1218.
1215
cancer resection. Fukushima J Med Sci.,
2003; 49(2): 117-127.
20. Winthida, Laroche CM, Groves AM, et al.
Use of quantitative lung scintigraphy to
predict
postoperative
pulmonary
function in lung cancer patients
Source of support: Nil
Conflict of interest: None declared.
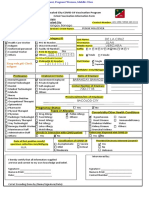
Table - 1:: Lung function parameters in the lobectomy subjects. (n = 64)
FEV1
FVC
Preoperative (L)
Predicted postoperative (L)
1 month follow up (L)
3 month follow up (L)
6 month follow up (L)
Difference at 1 month (ml)
Difference at 3 month (ml)
Difference at 6 month (ml)
Preoperative
Predicted postoperative
1 month follow up
3 month follow up
6 month follow up
Difference at 1 month (ml)
Difference at 3 month (ml)
Difference at 6 month (ml)
min
0.4
0.29
0.4
0.5
0.54
80
70
130
0.5
0.36
0.5
0.6
0.61
-200
-180
-180
max
3.3
2.5
2.7
2.72
2.75
230
250
250
3.5
2.94
2.74
2.76
2.8
250
250
250
Mean
1.8
1.4
1.6
1.6
1.6
157.9
179.8
230.8
2.2
1.6
1.8
1.8
1.8
124.5
147.1
185.8
SD
0.6
0.5
0.5
0.5
0.5
47.6
53.1
29.5
0.7
0.6
0.6
0.6
0.6
98.2
100.9
106.3
p value
a: p = 0.000*,
b: p = 0.000*,
c: p = 0.000*,
d: p = 0.000*,
e: p = 0.000*,
f: p = 0.000*,
Fredmans test
P = 0.000*
a: p = 0.000*,
b: p = 0.000*,
c: p = 0.000*,
d: p = 0.000*,
e: p = 0.000*,
f: p = 0.000*,
Fredmans test
p = 0.000*
a: Predicted postoperative FEV1 or FVC in comparison to FEV1 or FVC - 1 month follow up
b: Predicted postoperative FEV1 or FVC in comparison to FEV1 or FVC - 3 month follow up
c: Predicted postoperative FEV1 or FVC in comparison to FEV1 or FVC - 6 month follow up
d: FEV1 or FVC - 1 month follow up
u in comparison to FEV1 or FVC - 3 month follow up
e: FEV1 or FVC - 1 month follow up in comparison to FEV1 or FVC - 6 month follow up
f: FEV1or FVC - 3 month follow up in comparison to FEV1 or FVC - 6 month follow up
F: Overall change in FEV1 or FVC
p value flagged by asterisk mark indicates significant difference of compared groups
International Archives of Integrated Medicine, Vol. 2, Issue 3, March, 2015.
Copy right 2015,, IAIM, All Rights Reserved.
Rese
Page 133
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Vegetarian Diets: Health Benefits and Associated RisksDokument5 SeitenVegetarian Diets: Health Benefits and Associated RisksEditor_IAIMNoch keine Bewertungen
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- Biliopleural Fistula - A Rare Complication of Blunt Thoracoabdominal TraumaDokument4 SeitenBiliopleural Fistula - A Rare Complication of Blunt Thoracoabdominal TraumaEditor_IAIMNoch keine Bewertungen
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Zip Injuries: A Simple SolutionDokument3 SeitenZip Injuries: A Simple SolutionEditor_IAIMNoch keine Bewertungen
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Incidentally Detected Carcinoma in Situ in A Fibroadenoma of Breast in A Postmenopausal Woman: A Case ReportDokument6 SeitenIncidentally Detected Carcinoma in Situ in A Fibroadenoma of Breast in A Postmenopausal Woman: A Case ReportEditor_IAIMNoch keine Bewertungen
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Diagnosis of Anaplastic Thyroid Carcinoma On Fine Needle Aspiration Cytology - A Rare Case ReportDokument5 SeitenDiagnosis of Anaplastic Thyroid Carcinoma On Fine Needle Aspiration Cytology - A Rare Case ReportEditor_IAIMNoch keine Bewertungen
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Malignant Gastrointestinal Stromal Tumors (GISTs) of The Duodenum - A Rare Occurrence: Case ReportDokument5 SeitenMalignant Gastrointestinal Stromal Tumors (GISTs) of The Duodenum - A Rare Occurrence: Case ReportEditor_IAIMNoch keine Bewertungen
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Three Port Laparoscopic Cholecystectomy in Situs Inversus Totalis: A Case ReportDokument4 SeitenThree Port Laparoscopic Cholecystectomy in Situs Inversus Totalis: A Case ReportEditor_IAIMNoch keine Bewertungen
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- A Rare Case Report of Ectopic Cervical ThymomaDokument4 SeitenA Rare Case Report of Ectopic Cervical ThymomaEditor_IAIMNoch keine Bewertungen
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Case Report: Localized Nodular Synovitis of Knee JointDokument6 SeitenCase Report: Localized Nodular Synovitis of Knee JointEditor_IAIMNoch keine Bewertungen
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- Epidermal Nevus Syndrome Associated With Ocular Symblepharon and Gum Hypertrophy - A Rare VariantDokument4 SeitenEpidermal Nevus Syndrome Associated With Ocular Symblepharon and Gum Hypertrophy - A Rare VariantEditor_IAIMNoch keine Bewertungen
- Adenosquamous Carcinoma of Stomach: A Rare Entity - Case ReportDokument4 SeitenAdenosquamous Carcinoma of Stomach: A Rare Entity - Case ReportEditor_IAIMNoch keine Bewertungen
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Oral Rehabilitation Through Preventive Approach: Overdenture and Fenestrated DentureDokument6 SeitenOral Rehabilitation Through Preventive Approach: Overdenture and Fenestrated DentureEditor_IAIMNoch keine Bewertungen
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- Cervical and Vaginal Agenesis - A Rare Case ReportDokument5 SeitenCervical and Vaginal Agenesis - A Rare Case ReportEditor_IAIMNoch keine Bewertungen
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Lung Resection For Extensive Lung Injury Causing Severe HemorrhageDokument4 SeitenLung Resection For Extensive Lung Injury Causing Severe HemorrhageEditor_IAIMNoch keine Bewertungen
- Cardiac Troponin-T Levels in Heart Blood As A Marker To Diagnose Postmortem Myocardial InfarctionDokument11 SeitenCardiac Troponin-T Levels in Heart Blood As A Marker To Diagnose Postmortem Myocardial InfarctionEditor_IAIMNoch keine Bewertungen
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Changing Trends in Cesarean DeliveryDokument7 SeitenChanging Trends in Cesarean DeliveryEditor_IAIMNoch keine Bewertungen
- Detection of High Molecular Weight IgG Fibronectin Complexes in Various Types of Acute Myeloid Leukemia - A Study in Third World CountryDokument7 SeitenDetection of High Molecular Weight IgG Fibronectin Complexes in Various Types of Acute Myeloid Leukemia - A Study in Third World CountryEditor_IAIMNoch keine Bewertungen
- Couvelaire Uterus - A Case ReportDokument4 SeitenCouvelaire Uterus - A Case ReportEditor_IAIMNoch keine Bewertungen
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- Introduction To Cadavers - A Student's PerspectiveDokument8 SeitenIntroduction To Cadavers - A Student's PerspectiveEditor_IAIMNoch keine Bewertungen
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Laparoscopic Appendicectomy Surgery Using Spinal AnesthesiaDokument5 SeitenLaparoscopic Appendicectomy Surgery Using Spinal AnesthesiaEditor_IAIMNoch keine Bewertungen
- A Comparative Study of Fascial Sheath Interposition Versus No Fascial Sheath Interposition in No Scalpel VasectomyDokument6 SeitenA Comparative Study of Fascial Sheath Interposition Versus No Fascial Sheath Interposition in No Scalpel VasectomyEditor_IAIMNoch keine Bewertungen
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- A Comparative Study Between Conventional System and The Bethesda System Applied For Reporting Thyroid CytopathologyDokument9 SeitenA Comparative Study Between Conventional System and The Bethesda System Applied For Reporting Thyroid CytopathologyEditor_IAIMNoch keine Bewertungen
- Departmental Equipment Maintenance System in Government Medical CollegeDokument8 SeitenDepartmental Equipment Maintenance System in Government Medical CollegeEditor_IAIMNoch keine Bewertungen
- Role of Antibiotic Prophylaxis in Open Inguinal Hernioplasty - A Prospective Randomized Clinical TrialDokument11 SeitenRole of Antibiotic Prophylaxis in Open Inguinal Hernioplasty - A Prospective Randomized Clinical TrialEditor_IAIMNoch keine Bewertungen
- Sonographic Measurement of Renal Size in Normal North Indian ChildrenDokument7 SeitenSonographic Measurement of Renal Size in Normal North Indian ChildrenEditor_IAIMNoch keine Bewertungen
- Evidentiary Value and Effects of Contaminants On Blood Group Factors in Medico-Legal GroundsDokument5 SeitenEvidentiary Value and Effects of Contaminants On Blood Group Factors in Medico-Legal GroundsEditor_IAIMNoch keine Bewertungen
- White Blood Cell (WBC) As A Diagnostic Parameter in Acute Appendicitis in Pediatric Patients - A Retrospective StudyDokument3 SeitenWhite Blood Cell (WBC) As A Diagnostic Parameter in Acute Appendicitis in Pediatric Patients - A Retrospective StudyEditor_IAIMNoch keine Bewertungen
- The Use of Controller Medications in The Management of Pediatric Bronchial Asthma - Dynamic Patterns of LTRA (Montelukast) UseDokument7 SeitenThe Use of Controller Medications in The Management of Pediatric Bronchial Asthma - Dynamic Patterns of LTRA (Montelukast) UseEditor_IAIMNoch keine Bewertungen
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Comparative clinical and radiographic evaluation of autogenous bone grafts and demineralized freeze dried bone xenograft (Osseograft) combined with PRP in the treatment of human periodontal intra-osseous defects – 6 months studyDokument12 SeitenComparative clinical and radiographic evaluation of autogenous bone grafts and demineralized freeze dried bone xenograft (Osseograft) combined with PRP in the treatment of human periodontal intra-osseous defects – 6 months studyEditor_IAIMNoch keine Bewertungen
- D10W (Anything D5W) - 3% Normal Saline ( 0.9% Hypertonic) - Mannitol - Parenteral NutritionDokument6 SeitenD10W (Anything D5W) - 3% Normal Saline ( 0.9% Hypertonic) - Mannitol - Parenteral NutritionAlec Anon100% (1)
- Lab Policies Alkaline Phosphatase C311 Lab 8803Dokument4 SeitenLab Policies Alkaline Phosphatase C311 Lab 8803Valdez Francis ZaccheauNoch keine Bewertungen
- Role of Atypical Pathogens in The Etiology of Community-Acquired PneumoniaDokument10 SeitenRole of Atypical Pathogens in The Etiology of Community-Acquired PneumoniaJaya Semara PutraNoch keine Bewertungen
- Prostate Cancer Between Prognosis and Adequate/proper TherapyDokument8 SeitenProstate Cancer Between Prognosis and Adequate/proper TherapyGabriel NguyenNoch keine Bewertungen
- Bài Tập Tự Luyện Unit 2: Your Body And You (Lesson 1) #hasuenglishclassDokument4 SeitenBài Tập Tự Luyện Unit 2: Your Body And You (Lesson 1) #hasuenglishclassThu Tra NguyenNoch keine Bewertungen
- Systemic Lupus Erythematosus AssignmentDokument6 SeitenSystemic Lupus Erythematosus AssignmentnehaNoch keine Bewertungen
- SV300 Ventilator Product BrochureDokument6 SeitenSV300 Ventilator Product BrochureabnerkalilNoch keine Bewertungen
- ManitolDokument20 SeitenManitolkr PadmanabhanNoch keine Bewertungen
- 901-Article Text-1856-1-10-20221129Dokument6 Seiten901-Article Text-1856-1-10-20221129Made NujitaNoch keine Bewertungen
- Emergence of Multidrug Resistant Acinetobacter Baumannii As Nosocomial Pathogen: Clinical Significance and Antimicrobial SensitivityDokument5 SeitenEmergence of Multidrug Resistant Acinetobacter Baumannii As Nosocomial Pathogen: Clinical Significance and Antimicrobial SensitivityIOSRjournalNoch keine Bewertungen
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Herbs or Natural Products CancerDokument16 SeitenHerbs or Natural Products CancerANGELO NHAR100% (1)
- Guardian - Dental PPO Plan Summary 2022Dokument4 SeitenGuardian - Dental PPO Plan Summary 2022Jessi ChallagullaNoch keine Bewertungen
- Annotated BibliographyDokument5 SeitenAnnotated Bibliographyapi-286443025Noch keine Bewertungen
- Case Study NCP - Forcep BirthDokument4 SeitenCase Study NCP - Forcep BirthKent CruzNoch keine Bewertungen
- Colorectal Disease - 2023 - Suarez Pazos - Step by Step Surgical Technique For Robotic Kono S Anastomosis After Small BowelDokument2 SeitenColorectal Disease - 2023 - Suarez Pazos - Step by Step Surgical Technique For Robotic Kono S Anastomosis After Small BowelCLINIC SURGERY 17THNoch keine Bewertungen
- CH 5 Providing Psychosocial CareDokument79 SeitenCH 5 Providing Psychosocial CareKevin FacunNoch keine Bewertungen
- Milk Ring TestDokument25 SeitenMilk Ring TestDilhan Anuradha Wimalaratne71% (7)
- Bacteremia Fungemia, and Blood Cul Tures-V1Dokument53 SeitenBacteremia Fungemia, and Blood Cul Tures-V1Alok MishraNoch keine Bewertungen
- Annex 8. Viral Transport Media (VTM)Dokument2 SeitenAnnex 8. Viral Transport Media (VTM)deancoksNoch keine Bewertungen
- Ministry Health Medicines Formulary 1 2015Dokument371 SeitenMinistry Health Medicines Formulary 1 2015David Lim Su ShenNoch keine Bewertungen
- Cancer Incidence Estimates For 2022 Projection.99848Dokument13 SeitenCancer Incidence Estimates For 2022 Projection.99848Kittur AkshayNoch keine Bewertungen
- R-5656-02-V02 CA360B DFU Eng 20120320Dokument89 SeitenR-5656-02-V02 CA360B DFU Eng 20120320Ana ObradovicNoch keine Bewertungen
- Case Study On DehydrationDokument4 SeitenCase Study On DehydrationDustin Dela CruzNoch keine Bewertungen
- COPD ExacerbationDokument2 SeitenCOPD ExacerbationjusthoangNoch keine Bewertungen
- EBUS Kazuhiro YasufukuDokument27 SeitenEBUS Kazuhiro YasufukuOrion JohnNoch keine Bewertungen
- ACLS Megacode Testing ScenariosDokument12 SeitenACLS Megacode Testing Scenariosealm10100% (2)
- Thesis Related To Breast Self ExaminationDokument6 SeitenThesis Related To Breast Self Examinationfjfyj90y100% (3)
- Immunology Review For FPGEEDokument8 SeitenImmunology Review For FPGEEMina MinawyNoch keine Bewertungen
- Vaccination Form (Sample)Dokument1 SeiteVaccination Form (Sample)Godfrey Loth Sales Alcansare Jr.Noch keine Bewertungen
- Opioid-Free AnesthesiaDokument8 SeitenOpioid-Free AnesthesiaPaulina LugoNoch keine Bewertungen
- The Obesity Code: Unlocking the Secrets of Weight LossVon EverandThe Obesity Code: Unlocking the Secrets of Weight LossBewertung: 4 von 5 Sternen4/5 (6)
- The Age of Magical Overthinking: Notes on Modern IrrationalityVon EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityBewertung: 4 von 5 Sternen4/5 (28)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsVon EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNoch keine Bewertungen
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeVon EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeBewertung: 2 von 5 Sternen2/5 (1)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDVon EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDBewertung: 5 von 5 Sternen5/5 (2)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionVon EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionBewertung: 4 von 5 Sternen4/5 (404)