Beruflich Dokumente
Kultur Dokumente
Is Obesity A Risk Factor For Clostridium Difficile Infection?
Hochgeladen von
zernikevictoriaOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Is Obesity A Risk Factor For Clostridium Difficile Infection?
Hochgeladen von
zernikevictoriaCopyright:
Verfügbare Formate
Obesity Research & Clinical Practice (2015) 9, 5054
ORIGINAL ARTICLE
Is obesity a risk factor for Clostridium
difcile infection?
Emma Punni a, Jaime L. Pula b, Fady Asslo c,
Walid Baddoura a,c, Vincent A. DeBari a,d,
a
Department of Medical Education, St. Josephs Regional Medical Center, Paterson,
NJ, USA
b Department of Pediatrics, St. Josephs Regional Medical Center, Paterson, NJ, USA
c Division of Gastroenterology, St. Josephs Regional Medical Center, Paterson, NJ,
USA
d Department of Internal Medicine, School of Health and Medical Sciences, Seton Hall
University, South Orange, NJ, USA
Received 29 October 2013 ; received in revised form 13 December 2013; accepted 13 December 2013
KEYWORDS
Clostridium difcile
infection;
Obesity;
Epidemiology;
Risk factors;
Body mass index
Summary
Background: The epidemiology of Clostridium difcile infection (CDI) has become
an important area of investigation, especially in light of the global increase in both
hospital-acquired (HA) and community-acquired (CA) CDI. Recently, obesity was
found to be associated with CDI and was suggested to represent an independent
risk factor for it.
Objective: We undertook a casecontrol study to examine obesity as an exposure
for both HA and CA cases in adults (age 18 years) admitted to a tertiary, universityafliated, acute care medical facility in the northeastern United States.
Methods: During the period January 2012July 2013, we examined cross-sectional
BMI data on 189 cases of CDI and 189 contemporaneous age and gender-matched
controls.
Results: We were unable to detect a statistically signicant difference between
the two groups; in fact, the BMI values for both groups were substantially equivalent (cases: median = 26.5 kg/m, IQR: 22.132.5; controls: median = 26.0, IQR:
22.731.0; p = 0.696). Odds ratios (and 95% condence intervals), evaluated at BMI
of 25, 30 and 35 kg/m2 , did not demonstrate statistical signicance.
Conclusion: These data suggest that obesity, as described by BMI, may not be a risk
factor for CDI in all populations.
2013 Asian Oceanian Association for the Study of Obesity. Published by Elsevier
Ltd. All rights reserved.
Corresponding author at: Department of Internal Medicine, School of Health and Medical Sciences, Seton Hall University, South
Orange, NJ, USA. Tel.: +1 908 309 3939.
E-mail address: Vincent.debari@shu.edu (V.A. DeBari).
1871-403X/$ see front matter 2013 Asian Oceanian Association for the Study of Obesity. Published by Elsevier Ltd. All rights reserved.
http://dx.doi.org/10.1016/j.orcp.2013.12.007
Is obesity a risk factor for Clostridium difcile infection?
Introduction
Clostridium difcile infection (CDI) has become
an important nosocomial cause of morbidity and
mortality in the healthcare facility setting [1].
The result of CDI is diarrhoea, although the disease may progress to pseudomembranous colitis, a
severe inammation of the colon [2]. Because of
the scope and severity of CDI, its epidemiology and
potential therapeutic approaches to dealing with
it have achieved prominence over the past decade
[3,4].
Among the better known risk factors, antibiotic
use has come to be recognised as an exposure that
is independently associated with CDI. Studies have
also implicated the use of proton pump inhibitors
(PPI) [5,6], chronic renal failure [7], older age [8],
and chemotherapy-induced immunosuppression [9]
as risk factors. Hypoalbuminemia has also been
associated with CDI [10], and, along with diabetes mellitus, may be a risk factor for recurrence
[11].
A recent clinical investigation from Israel found
a strong association of obesity with CDI. In a
retrospective, casecontrol study, Bishara et al.
[12] found that the mean body mass index (BMI)
for a group of 146 cases of CDI (33.6 kg/m2 ,
SD: 4.3) was signicantly (p < 0.001) higher than
a matched control group (28.9 5.4 kg/m2 ). This
report has been the only such report to show
an association between obesity and CDI. We
sought to examine the possibility of obesity, as
evidenced by increased BMI, being an independent risk factor in our population of recent CDI
cases.
Methods
Setting
The study was conducted at St. Josephs Regional
Medical Center, a 700 bed, university-afliated,
tertiary care, teaching hospital in the northeastern
United States. The protocol was submitted to the
Institutional Review Board and was granted exempt
status.
Subjects and protocol
Subjects were enrolled retrospectively during the
late summer of 2013 and included cases of CDI
observed during the period January 2012July
2013, inclusive. We included presumed cases of
CDI, based on clinical manifestation (diarrhoea)
51
and both the presence of C. difcile antigen
(glutamate dehydrogenase) and toxins A and B
as detected by the C.diff Quik Chek Complete
assay system (TechLab Inc., Blacksburg, VA, USA).
Patients with hepatic cirrhosis, HIV and those
being treated with chemotherapy for various malignancies were excluded. We also subdivided the
cases into those that were hospital acquired (HA)
and those that were community acquired (CA)
based on time from admission to time of presentation with CDI [13]. Cross-sectional data, on
admission, were obtained for BMI, and known risk
factors as well as demographics. Ultimately, 189
cases were enrolled. These cases were compared
with a group of 189 controls admitted during
the same period of time as the case cohort (1
January 201231 July 2013). The controls were
matched for age (3 years) and gender, and were
applied with the same exclusion criteria as the
cases (Hepatic cirrhosis, HIV positivity and those
being treated with chemotherapy for malignancies).
Statistical analysis
We powered the study to be able to detect a difference in BMI of 2 kg/m2 with a pooled SD of
5 kg/m2 and found that at a two-sided = 0.05,
we would achieve a power of >90% with case
and control groups of 189 subjects. Therefore, we
enrolled 189 adult (18 years) cases and the same
number of age (3 years) and gender-matched controls admitted during the period January 2012July
2013, inclusive. Univariate categorical associations
were analysed in contingency tables by Fishers
exact test for 2 2 tables and chi-square test for
2 n tables (race/ethnicity). Continuous data were
tested for normality by the DAgostino-Pearson
omnibus normality test. All were found to be
non-Gaussian and log transformations also did not
achieve distributions judged to be normal. Thus,
these data are presented as medians and interquartile ranges (IQR) and two group-wise comparisons
were evaluated by a nonparametric statistical
method, the MannWhitney test. For baseline
characteristics to be considered as potential confounders, p-values 5 (p 0.25) were required.
Potential confounders that met this criterion were
to be included in a multivariable logistic regression
model only if the univariate analyses were statistically signicant, i.e., odds ratios (OR) not including
a value of 1.00 in the 95% condence interval (CI)
and p < 0.05 (two-sided). Data were analysed using
Prism software (GraphPad Corp., San Diego, CA,
USA) and SPSS v. 18 (IBM Corp., Armonk, NY, USA).
52
E. Punni et al.
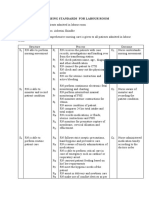
Table 1 Baseline characteristics of the subjects. All continuous data are given as medians and interquartile range
(25th75th percentile); categorical data given as counts. Abbreviations: HA, hospital-acquired; CA, community
acquired; NA, not applicable; DM, diabetes mellitus; HTN, hypertension; CHF, congestive heart failure; PPI, proton
pump inhibitors; H2RA, histamine type 2 receptor antagonists.
Parameter
Cases
Controls
p-Value
Age (years)
Gender (F/M)
Race/ethnicity
Black
Hispanic
White
Other
Albumin (g/dL)
HA/CA/indeterminate
DM
HTN
CHF
Fluoroquinolones
All antibiotics
PPI
H2RA
69 (5782)
103/86
70 (5681)
103/86
0.877
1.000
0.460
46
8
115
14
3.3 (2.83.8)
157/38/4
75/114
120/69
18/171
17/172
92/97
57/132
12/177
45
3
123
13
3.8 (3.34.2)
NA
61/128
115/74
16/173
13/176
58/131
34/155
6/183
Results
Baseline characteristics of the groups
Demographic characteristics (Table 1) reveal similarities in age, gender (patients were matched to
both these characteristics) and racial and ethnic
backgrounds. Hospital-acquired cases accounted
for 83% of all cases. Not unexpectedly, cases cohorts
were found to be hypoalbuminemic relative to controls and were found to be signicantly associated
with PPI (p = 0.008) and antibiotic usage (p = 0.001)
(excluding vancomycin and metronidazole, used to
treat CDI). Interestingly, our cases were not associated with uoroquinolone usage; however, this
study was not powered for that covariate and there
were relatively few patients in our groups (17 cases
and 13 controls who were treated with uoroquinolones).
Comparison of BMI in cases and controls
Of the cases, 36% were obese (BMI > 30 kg/m2 ) and
of the controls 30% were found to be obese. There
was no signicant difference between cases and
controls in this regard (p = 0.258). We were unable
to detect a difference in the BMI of cases and controls (Fig. 1A). Median BMI for cases was 26.5 kg/m2
(IQR: 22.132.5); for controls the median was
26.0 kg/m2 (IQR: 22.731.0); p = 0.696. We, similarly, could not detect a statistically signicant
difference between HA (n = 146) and CA cases
(n = 39) (Fig. 2B), with medians and IQR for HA
<0.0001
NA
0.163
0.672
0.858
0.569
0.001
0.008
0.226
cases being 26.6 kg/m2 (21.632.3) and CA being
26.5 kg/m2 (22.233.0); p = 0.638 (Fig. 2B).
Effect size, as evaluated by OR and 95% CI
was evaluated at three levels of BMI: 25, 30 and
35 kg/m2 . These data are given in Fig. 2. At all BMI
levels evaluated, the lower 95% condence value
included unity, precluding any statistically signicant difference. Per protocol, these data were not
subjected to multivariable analysis in light of their
not suggesting a signicant association between BMI
and CDI.
Discussion
Given the rapid increase in the incidence of CDI
infection over the past decade, risk factor surveillance is clearly warranted. Patients, potentially
at risk for developing diarrhoea secondary to CDI,
when identied, could be monitored during their
hospital stay and subjected to therapeutic alterations which may decrease the likelihood of their
developing CDI. As an example, in the case of
stress ulcer prophylaxis, substituting type-2 histamine receptor antagonists for PPIs (the use of
which represents a well-established risk factor for
CDI) decreased the risk for developing CDI [5,6].
Several exposures that are associated with CDI,
namely hypoalbuminemia, advanced age and diabetes [11,1417] suggest that nutritional factors
may play a role in its development. Obesity is frequently a product of poor nutrition; in fact, it may
Is obesity a risk factor for Clostridium difcile infection?
Figure 1 BMI measurements for individuals enrolled in
the study. (A) Compares all cases with controls (n = 189
per group; p = 0.696). (B) Compares HA (n = 146) and
CA cases (n = 39) for which comparison the p-value was
0.638. Box and whisker plots show median (centre of the
box) and IQR (ends of box) with maximum and minimum
values at ends of error bars.
reect a state of malnutrition [18]. Thus, awareness of patients who are overweight or obese may
represent an approach to identifying subjects who
are potentially at risk for CDI.
In routine clinical practice, BMI is the most frequently used surrogate for body composition. It
has limitations based on its comparison to actual
Figure 2 OR for CDI at BMI of 25, 30 and 35 kg/m2 ; error
bars are 95% CI.
53
adiposity. In a recent study, Bishara et al. [12] evaluated BMI in 148 cases of CDI and 148 age and
gender-matched controls. They proposed that CDI
is associated with obesity, and this association was
based on the differences in BMI between these
groups.
In this study, we also examined the relationship
between BMI and CDI in a casecontrol model. Our
ndings do not conrm the purported association
between obesity and CDI. In fact, the subjects with
CDI had BMI values that were, at the median, barely
overweight and quite similar to the controls. The
reason for these discrepant results bears investigation. There is the possibility that the diets of
the populations represented by the sample cases
in the two studies are likely quite different. In
2012, Antunes et al. [19] provided new insights into
understanding the links between nutrient acquisition and virulence in C. difcile. One example is
the ability of C. difcile to use an extended range of
carbohydrates, which may be important during the
pathogenesis process (by means of promoting survival and growth in the intestine). Another example
is reected in the composition and development
of infant gut microbiota, namely C. difcile, as
inuenced by BMI, weight, and weight gain of mothers during pregnancy [20]. Hence, although it has
been reported that deviations in gut microbiota
composition may predispose towards obesity, and
specic groups of commensal gut bacteria may
harvest energy from food more efciently than
others obesity may not be an independent risk
factor for CDI. Physiologic factors related to the
degree of diversity in the case and control samples
may also be reective of the observed discrepancy.
As further conrmation of the role of diet in CDI,
while in Northeast-Brazil, Maciel et al. [21] investigated the effect of high doses of oral vitamin A and
suggested the role of retinol is also a protective
one with regards to early childhood diarrhoea associated with CDI. Furthermore, the effect of various
diets on C. difcile in mice has been established
[22] in addition to the negative role of an atherogenic diet fed to hamsters [23].
In our opinion, the characterisation of obesity
as a risk factor for CDI remains an open issue,
one perhaps best adjudicated from an investigational standpoint through the use of a better
surrogate of body composition such as the use of
body impedance analysis instrumentation [24] in a
prospective cohort of hospitalised patients. In lieu
of the results of such a study, currently planned
in our institution, we can only comment on our
present ndings that suggest that obesity may not
be a risk factor for CDI in all populations.
54
E. Punni et al.
Conict of interest statement
The authors have no conicts of interest, nancial
or otherwise, to disclose.
References
[1] Gould CV, McDonald LC. Bench-to-bedside review: Clostridium difcile colitis. Crit Care 2008;12:203.
[2] Freeman J, Bauer MP, Baines SD, Corver J, Fawley WN,
Goorhuis B, et al. The changing epidemiology of Clostridium difcile infections. Clin Microbiol 2010;23:529
49.
[3] Surawicz CM. Reining in recurrent Clostridium difcile infection whos at risk? Gastroenterology
2009;139:1524.
[4] Pacheco SM, Johnson S. Important clinical advances in the
understanding of Clostridium difcile infection. Curr Opin
Gastroenterol 2013;29:428.
[5] Jayatilaka S, Shakov R, Eddi R, Bakaj G, Baddoura WJ,
DeBari VA. Clostridium difcile infection in an urban medical center: ve-year analysis of infection with the use of
proton pump inhibiors. Ann Clin Lab Sci 2007;37:2417.
[6] Barletta JF, El-Ibiary SY, Davis LE, Nguyen B, Raney
CR. Proton pump inhibitors and the risk for hospitalacquired Clostridium difcile infection. Mayo Clin Proc
2013;88:108590.
[7] Eddi R, Malik MN, Shakov R, Baddoura WJ, Chandran C,
DeBari VA. Chronic kidney disease as a risk factor for
Clostridium difcile infection. Nephrology 2010;15:4715.
[8] Moshkowitz M, Ben-Baruch E, Kline Z, Shimoni Z, Niven M,
Konikoff F. Risk factors for severity and relapse of pseudomembranous colitis in an elderly population. Colorectal
Dis 2007;9:1737.
[9] Trudel JL. Clostridium difcile colitis. Clin Colon Rectal
Surg 2010;20:137.
[10] Dubberke ER, Reske KA, Yan Y, Olsen MA, McDonald LC,
Fraser VJ. Clostridium difcile-associated disease in a setting of endemicity: identication of novel risk factors. Clin
Infect Dis 2007;45:15439.
[11] Shakov R, Salazar RS, Kagunye SK, Baddoura WJ, DeBari VA.
Diabetes mellitus as a risk factor for recurrence of Clostridium difcile infection in the acute care hospital setting. Am
J Infect Control 2011;39:1948.
[12] Bishara J, Farah R, Mograbi J, Khalaila W, Abu-Elheja O,
Mahamid M, et al. Obesity as a risk factor for Clostridium
difcile infection. Clin Infect Dis 2013;57:48993.
[13] Khanna S, Pardi DS, Aronson SL, Kammer P, Orenstein R,
Sauver JL, et al. The epidemiology of community-acquired
Clostridium difcile infection: a population-based study.
Am J Gastroenterol 2012;107:8995.
[14] Salazar-Kagunye R, Shah A, Loshkajian G, Baddoura WJ,
DeBari VA. Association of decreased serum protein fractions with Clostridium difcile infection in the acute care
setting: a casecontrol study. Biomark Med 2012;6:6639.
[15] Cleary RK.Clostridium difcile-associated diarrhea and colitis: clinical manisfestations, diagnosis and treatment. Dis
Colon Rectum 1998;41:143549.
[16] Wang F, Ma X, Hao Y, Yang R, Ni J, Xiao Y, et al. Serum
glycated albumin is inversely inuenced by fat mass and
visceral adipose tissue in Chinese with normal glucose tolerance. PLoS ONE 2010;7:e51098.
[17] Henrich TJ, Krakower D, Bitton A, Yokoe DS. Clinical risk
factors for severe Clostridium difcile-associated disease.
Emerg Infect Dis 2009;15:41522.
[18] Via M. The malnutrition of obesity: micronutrient deciencies that promote diabetes. ISRN Endocrinol 2012,
http://dx.doi.org/10.5402/2012/103472.
[19] Antunes A, Camiade E, Monot M, Courtois E, Barbut F, Sernova NV, et al. Global transcriptional control by glucose
and carbon regulator CcpA in Clostridium difcile. Nucleic
Acids Res 2012;40:1070118.
[20] Collado MC, Isolauri E, Laitinen K, Salminen S. Effect of
mothers weight on infants microbiota acquisition, composition, and activity during early infancy: a prospective
follow-up study initiated in early pregnancy. Am J Clin Nutr
2010;92:102330.
[21] Maciel AA, Ori RB, Braga-Neto MB, Braga AB, Carvalho EB,
Lucena HB, et al. Role of retinol in protecting epithelial cell
damage induces by Clostridium difcile toxin A. Toxicon
2007;50:102740.
[22] Mahe S, Corthier G, Dubos F. Effect of various diets on toxin
production by two strains of Clostridium difcile in gnotobiotic mice. Infect Immun 1987;55:18015.
[23] Blankenship-Paris TL, Walton BJ, Hayes YO, Chang J.
Clostridium difcile infection in hamsters fed an atherogenic diet. Vet Pathol 1995;32:26973.
[24] Beeson WL, Batech M, Schultz E, Salto L, Firek A, DeLeon
M, et al. Comparison of body composition by bioelectrical
impedance analysis and dual-energy X-ray absorptiometry
in Hispanic diabetics. Int J Body Compos Res 2010;8:4550.
Available online at www.sciencedirect.com
ScienceDirect
Das könnte Ihnen auch gefallen
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (894)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- Infusion Pumps, Large-Volume - 040719081048Dokument59 SeitenInfusion Pumps, Large-Volume - 040719081048Freddy Cruz BeltranNoch keine Bewertungen
- Hyperglycemia in Critically Ill Management (: From ICU To The Ward)Dokument20 SeitenHyperglycemia in Critically Ill Management (: From ICU To The Ward)destiana samputriNoch keine Bewertungen
- Amanita PhalloidesDokument15 SeitenAmanita PhalloidesJair Carrillo100% (1)
- Skin Infection Lab ReportDokument6 SeitenSkin Infection Lab Reportthe someone100% (2)
- Jurnal Obesitas 2Dokument9 SeitenJurnal Obesitas 2zernikevictoriaNoch keine Bewertungen
- HBM Explains Health BehaviorDokument3 SeitenHBM Explains Health BehaviorAKbarNoch keine Bewertungen
- MMHS 15 Proceeding in Jakarta Indonesia Conference PDFDokument37 SeitenMMHS 15 Proceeding in Jakarta Indonesia Conference PDFzernikevictoriaNoch keine Bewertungen
- MMHS 15 Proceeding in Jakarta Indonesia Conference PDFDokument37 SeitenMMHS 15 Proceeding in Jakarta Indonesia Conference PDFzernikevictoriaNoch keine Bewertungen
- Drug StudyDokument17 SeitenDrug StudyTherese ArellanoNoch keine Bewertungen
- Breast and Nipple Thrush - 280720Dokument6 SeitenBreast and Nipple Thrush - 280720Robbie WilliamsNoch keine Bewertungen
- Role of IV Meropenem in Current EraDokument38 SeitenRole of IV Meropenem in Current EraImtiyaz Alam SahilNoch keine Bewertungen
- Hong Kong Dental Journal - Volume 2 - Number 2 - YuLeungDokument1 SeiteHong Kong Dental Journal - Volume 2 - Number 2 - YuLeungFebySiampaNoch keine Bewertungen
- Drugs Induce Hematologic DisordersDokument3 SeitenDrugs Induce Hematologic DisorderspaymanmatinNoch keine Bewertungen
- Probiotics vs Prebiotics: Differences, Advantages, TrendsDokument5 SeitenProbiotics vs Prebiotics: Differences, Advantages, TrendsNaevisweloveuNoch keine Bewertungen
- 155 Anaesthesia For Transurethral Resection of The Prostate (TURP)Dokument8 Seiten155 Anaesthesia For Transurethral Resection of The Prostate (TURP)Verico PratamaNoch keine Bewertungen
- Emergency Contact ListDokument1 SeiteEmergency Contact ListthubanNoch keine Bewertungen
- Thesis On HPV VaccineDokument8 SeitenThesis On HPV Vaccinegjftqhnp100% (2)
- Gender-Dysphoric-Incongruene Persons, Guidelines JCEM 2017Dokument35 SeitenGender-Dysphoric-Incongruene Persons, Guidelines JCEM 2017Manel EMNoch keine Bewertungen
- Nursing Standards for Labour RoomDokument3 SeitenNursing Standards for Labour RoomRenita ChrisNoch keine Bewertungen
- Ob Assessment FinalDokument10 SeitenOb Assessment Finalapi-204875536Noch keine Bewertungen
- CSL 6 - HT PE Groin LumpDokument5 SeitenCSL 6 - HT PE Groin LumpSalsabilla Ameranti PutriNoch keine Bewertungen
- Complications After CXLDokument3 SeitenComplications After CXLDr. Jérôme C. VryghemNoch keine Bewertungen
- Qip ProjectDokument13 SeitenQip Projectapi-534216481Noch keine Bewertungen
- Dental BS Delta 1500 PPO Benefit Summary 2018Dokument4 SeitenDental BS Delta 1500 PPO Benefit Summary 2018deepchaitanyaNoch keine Bewertungen
- Community Pharmacy Management CH 3 Prescription and Prescription Handlind NotesDokument9 SeitenCommunity Pharmacy Management CH 3 Prescription and Prescription Handlind Notesi.bhoomi12Noch keine Bewertungen
- Dr. Ayesha Latif's Guide to Airway ManagementDokument32 SeitenDr. Ayesha Latif's Guide to Airway ManagementAyesha LatifNoch keine Bewertungen
- Understanding Plasma Cell Dyscrasias: MGUS, Myeloma, Waldenstrom's and AmyloidosisDokument41 SeitenUnderstanding Plasma Cell Dyscrasias: MGUS, Myeloma, Waldenstrom's and AmyloidosisDr MonikaNoch keine Bewertungen
- Endocrine System: Capillary Glucose MonitoringDokument34 SeitenEndocrine System: Capillary Glucose Monitoringjoel david knda mj100% (1)
- AIDS (Powerpoint Summary)Dokument14 SeitenAIDS (Powerpoint Summary)iris203550% (2)
- Nursing Management of Nephrotic SyndromeDokument2 SeitenNursing Management of Nephrotic SyndromeMARYAM AL-KADHIMNoch keine Bewertungen
- Cerebral Concussion - PresentationDokument19 SeitenCerebral Concussion - PresentationAira AlaroNoch keine Bewertungen
- What Is ScabiesDokument7 SeitenWhat Is ScabiesKenNoch keine Bewertungen
- ImgDokument1 SeiteImgLIDIYA MOL P V100% (1)
- Kuisioner Nutrisi Mini Nutritional AssessmentDokument1 SeiteKuisioner Nutrisi Mini Nutritional AssessmentNaufal AhmadNoch keine Bewertungen