Beruflich Dokumente
Kultur Dokumente
Management of Arrhythmias
Hochgeladen von
Aray Al-AfiqahOriginalbeschreibung:
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Management of Arrhythmias
Hochgeladen von
Aray Al-AfiqahCopyright:
Verfügbare Formate
Intensive Care Unit, Prince of Wales Hospital, Chinese University of Hong Kong
MANAGEMENT OF ARRHYTHMIAS
The types of arrhythmias you are likely to encounter in the ICU can be broadly
divided into bradyarrhythmias and tachyarrhythmias
Tachyarrhythmia
Heart rate > 100 bpm
Supraventricular
Paroxysmal supraventricular tachycardias
Atrial fibrillation
Atrial flutter
Multifocal atrial tachycardia
Junctional tachycardia
Sinus tachycardia
Ventricular
Ventricular tachycardia (>/= 5 beats at >/=120 bpm; non-sustained
<30s, sustained >30s; monomorphic, polymorphic; with pulse, pulseless)
Ventricular fibrillation
Diagnosis
Rhythm strip is easily accessible in ICU. However, must obtain a 12-lead
ECG as much as is possible
How to differentiate between SVT vs VT will not be mentioned in this
manual
Echo may be necessary to exclude structural heart disease
? invasive electrophysiological study
Acute treatment
If in doubt and patient, treat as VT. If patient haemodynamically unstable,
immediate DC cardioversion/defibrillation
Active seek out and treat causes (acute coronary syndrome, acute
respiratory insufficiency of various aetiologies, sepsis, electrolytes)
In this ICU, our first line anti-arrhythmic is amiodarone unless
contraindicated
Correct electrolytes : keep serum K > 4 mmol/L and Mg > 2 mmol/L
Narrow complex tacharrhythmias
Haemodynamic unstable
Immediate DC cardioversion (50J for PSVT/A flutter; 200J for AF)
Haemodynamic stable
Vagal maneouvres
IV adenosine 6 mg (ATP=10mg)---2 min---6 mg(10)---2 min--12 mg(20)
IV Amiodarone (loading dose of 150mg over 10 mins, may
repeat if failed to rate control; followed by infusion 30 mg/hour)
caution long term side effects
Page 1 of 4
Intensive Care Unit, Prince of Wales Hospital, Chinese University of Hong Kong
Check with senior if failed to rate-control with amiodarone
may consider other anti-arrhythmics eg
Diltiazem (0.25 to 0.35 mg/kg loading followed by infusion 5-15
mg/hour) caution hypotension
IV Beta- blockers (metoprolol titrate 0.5-1mg, esmolol
0.5mg/kg/min for one min followed by 0.05-0.2mg/kg/min)
caution hypotension
IV Digoxin (1 mg over 24 hours in increments of 0.25 to 0.5
mg, followed by 0.125 mg to 0.25 mg daily)
Wide complex tachyarrhythmias
Haemodynamic unstable
Immediate DC cardioversion start at 100J, increase if unsuccessful
Defibrillation according to ACLS protocol for VF and pulseless VT
Haemodynamic stable
SVT (see above)
VT or uncertain
IV Amiodarone (loading dose of 150mg over 10 mins, may
repeat if failed to rate control; followed by infusion 30 mg/hour)
Note: for tachyarrhythmias postoperative cardiac surgery the surgeons prefer
their protocol which is 300 mg amiodarone IV over the first hour and 900 mg
infusion over the next 23 hours (600 mg if small patient)
Atrial Fibrillation
Deserves a separate mention as it is very commonly encountered in the ICU
Can be classified into
Recurrent: when AF occurs on 2 or more occasions
Paroxysmal: episodes that generally last </= 7 days (most last <24h)
Persistent: AF that last >/=7 days
Permanent: paroxysmal or persistent AF with failure to cardiovert or not
attempted
Causes (refers to those seen in ICU, list not exhaustive)
Acute and temporary (alcohol, post-operative esp cardiac or thoracic
surgery, electrocution, myocarditis, pulmonary embolism, other pulmonary
diseases, hyperthyroidism, post-operative AMI)
Underlying CVS diseases (valvular heart esp mitral, coronary artery
disease, hypertension esp if LV hypertrophy present)
Neurogenic heightened vagal or adrenergic tone
Note: In our ICU PAF can be a non-specific sign of failed weaning, acute
respiratory pathology, sepsis, acute coronary syndrome
Assessment
What nature and symptoms associated with AF, clinical type, previous
treatment received, underlying heart or pulmonary diseases or other
reversible causes
Page 2 of 4
Intensive Care Unit, Prince of Wales Hospital, Chinese University of Hong Kong
Investigations 12 lead ECG looking for LV hypertrophy, BBB, AMI
CXR acute pneumonia, heart failure
Echo
Thyroid function test
Management
Unstable DC cardioversion start at 200J
Stable rate control (antiarrhythmics, cardioversion), anticoagulation
Anticoagulate if AF present >/= 48 hours and if persistent (LMWH bd dose
or UH to APTT 1.5 -2 times)
Long term antiarrhythmic agent not necessary unless AF>3 months
duration
Antiarhythmics commonly used in ICU for AF
Amiodarone (loading dose of 150mg over 10 mins, may repeat if
failed to rate control; followed by infusion 30 mg/hour) caution
long term side effects
Check with senior if failed to rate-control with amiodarone may
consider other anti-arrhythmics eg
Diltiazem (0.25 to 0.35 mg/kg loading followed by infusion 5-15
mg/hour) caution hypotension
Beta- blockers (metoprolol IV, esmolol)
Bradyarrhythmia
Heart rate < 60 bpm
Sinus node dysfunction (sinus bradycardia, sinus pause)
AV node dysfunction (1st, 2nd, 3rd degree AV block)
Actively seek and eliminate causes (ICU mediated, extrinsic)
ICU vagally mediated causes
Intubation, suctioning, increased intracranial pressure,
urination, defaecation, vomiting , retching
Extrinsic causes
Drugs (antiarrhythmic agents)
Electrolytes (K, Mg, Ca)
Hypothyroidism
Hypothermia
Sepsis
Specific infection (eg. endocarditis)
AMI (inferior AMI related AV blocks often transient; Anterior
AMI related AV blocks often irreversible)
Acute treatment
May not need immediate treatment if haemodynamically stable
Correct electrolytes
Treat if
Symptomatic sinus bradycardia (hypotension, ischaemia, escape
ventricular arrhythmia)
Page 3 of 4
Intensive Care Unit, Prince of Wales Hospital, Chinese University of Hong Kong
Give
Ventricular asystole
Symptomatic AV block (2nd degree Type I or 3rd degree with
narrow-complex escape rhythm)
Atropine: IV 0.6 mg (max 3 mg)
Isoprenaline: Infusion at 0.5 10 mcg/min (caution in ischaemic
heart disease)
Pacing: for symptomatic bradycardia. Types including
transcutaneous/epicardial/transvenous/permanent. Inform ICU senior if
pacing required
Pacing
Indications for urgent transcutaneous pacing
1. Sinus bradycardia with symptoms (SBP <80mmHg) unresponsive to drug
therapy
2. Mobitz type II 2nd degree AV block
3. 3rd degree heart block
4. Bilateral BBB (alternating BBB or RBBB with alternating LAFB/LPFB)
5. Newly acquired or age indeterminate bifascicular block (LBBB, RBBB with
LAFB or LPFB) with 1st degree AV block
Because transcutaneous pacing may be uncomfortable, especially when
prolonged, it is intended to be prophylactic and temporary. Refer to cardiologist
for transvenous pacing in patients who require ongoing pacing and in those with
a very high probability of requiring pacing
Indications for temporary transvenous pacing
1. Asystole
2. Symptomatic bradycardia (includes sinus bradycardia with hypotension
and Type I 2nd degree AV block with hypotension not responsive to
atropine)
3. Mobitz type II 2nd degree AV block
4. 3rd degree heart block
5. Bilateral BBB (alternating BBB or RBBB with alternating LAFB/LPFB)
6. Newly acquired or age indeterminate bifascicular block (LBBB, RBBB with
LAFB or LPFB) with 1st degree AV block
Monitor to ensure appropriate pacing and sensing functions and absence of
dislodgment (CXR)
Frequent (at least once per 24 hours) testing of pacing thresholds (pacing
energy is usually set at more than 3 times the threshold)
Page 4 of 4
Das könnte Ihnen auch gefallen
- Arterial Lines Mark Hammerschmidt, RN FromDokument9 SeitenArterial Lines Mark Hammerschmidt, RN FromMark Hammerschmidt100% (3)
- Fall Risk Assessment FormDokument3 SeitenFall Risk Assessment FormMichael Silva100% (1)
- Basic Care & Comfort Nclex RN UwDokument10 SeitenBasic Care & Comfort Nclex RN Uwgwen scribd100% (1)
- PB 20Dokument10 SeitenPB 20Cheng CapunoNoch keine Bewertungen
- BackgroundsDokument13 SeitenBackgroundsRaMinah100% (8)
- Cardiovascular Disorders Proper 1232011849539043 1Dokument111 SeitenCardiovascular Disorders Proper 1232011849539043 1api-19824701Noch keine Bewertungen
- Sinus Bradycardia: I. Sinus Dysrhythmias Description ManagementDokument4 SeitenSinus Bradycardia: I. Sinus Dysrhythmias Description ManagementMargueretti Delos ReyesNoch keine Bewertungen
- Chest TubesDokument12 SeitenChest TubesMark Hammerschmidt100% (4)
- IV Dosage CalculationsDokument4 SeitenIV Dosage Calculationsjessie monroeNoch keine Bewertungen
- Nursing Test Bank QuestionDokument97 SeitenNursing Test Bank QuestionADEDIRAN ABIONANoch keine Bewertungen
- Cardiovascular System: By: Marc Anthony Liao RNDokument59 SeitenCardiovascular System: By: Marc Anthony Liao RNloveseeker06Noch keine Bewertungen
- Nursing Management in Abdominal SurgeryDokument19 SeitenNursing Management in Abdominal Surgeryejguy7777100% (2)
- CH 29 - Management of Patients With Structural, Infectious, and Inflmmatory Cardiac DisordersDokument15 SeitenCH 29 - Management of Patients With Structural, Infectious, and Inflmmatory Cardiac DisordersPye Antwan Delva100% (1)
- Arrhythmias Teacher GuideDokument12 SeitenArrhythmias Teacher GuideMayer Rosenberg100% (3)
- Fluids and Electrolytes ConceptDokument31 SeitenFluids and Electrolytes ConceptDarwin AndalNoch keine Bewertungen
- Chronic Kidney Disease: Prepared by Zakia RogerDokument27 SeitenChronic Kidney Disease: Prepared by Zakia Rogerbene dugaNoch keine Bewertungen
- Adult Health III Final Study GuideDokument12 SeitenAdult Health III Final Study GuideRyanne JNoch keine Bewertungen
- 4 Urinary and Bowel EliminationDokument59 Seiten4 Urinary and Bowel Eliminationsechzhen100% (1)
- IV TherapyDokument15 SeitenIV Therapyprincessmonique_208609100% (2)
- NCM 118 Midterms ReviewerDokument7 SeitenNCM 118 Midterms ReviewerKai SamaNoch keine Bewertungen
- The 30 Most Important Must Know Drugs For NclexDokument2 SeitenThe 30 Most Important Must Know Drugs For NclexmsgailNoch keine Bewertungen
- College of Nursing Procedures Checklist: Giving Subcutaneous InjectionsDokument2 SeitenCollege of Nursing Procedures Checklist: Giving Subcutaneous InjectionsCamillus Carillo AngelesNoch keine Bewertungen
- Periop Power PointDokument97 SeitenPeriop Power PointAldrine Albor Anyayahan INoch keine Bewertungen
- Dosage Calculations 2012oct19 - CalcreviewDokument25 SeitenDosage Calculations 2012oct19 - CalcreviewBingle PedrozoNoch keine Bewertungen
- Revise ELECTROCARDIOGRAM MONITORINGDokument2 SeitenRevise ELECTROCARDIOGRAM MONITORINGsenyorakath100% (1)
- Periop 8Dokument18 SeitenPeriop 8Bern GervacioNoch keine Bewertungen
- FNP Final TestDokument10 SeitenFNP Final TestNelson MandelaNoch keine Bewertungen
- Post OpDokument4 SeitenPost OpLeo Paolo LuceroNoch keine Bewertungen
- Chest Pain: Jean J. Chatham, MDDokument40 SeitenChest Pain: Jean J. Chatham, MDYermia RashaquatNoch keine Bewertungen
- Catheterization DemoDokument48 SeitenCatheterization Demojonna casumpangNoch keine Bewertungen
- Scope and Practice of Emergency With LectureDokument34 SeitenScope and Practice of Emergency With LectureArvie ReyesNoch keine Bewertungen
- Dosage & CalculationsDokument20 SeitenDosage & CalculationsKnight-Zussette VillarNoch keine Bewertungen
- Tracheostomy Care SkillsDokument8 SeitenTracheostomy Care Skillshoangt2002Noch keine Bewertungen
- Necrotizing Otitis 2022Dokument20 SeitenNecrotizing Otitis 2022asmashNoch keine Bewertungen
- Basic Drug Computations Part 1Dokument8 SeitenBasic Drug Computations Part 1Carl Elexer Cuyugan Ano100% (4)
- Emergency Nursing: By: Keverne Jhay P. ColasDokument61 SeitenEmergency Nursing: By: Keverne Jhay P. ColasGaras AnnaBerniceNoch keine Bewertungen
- Central Venous Pressure (CVP)Dokument38 SeitenCentral Venous Pressure (CVP)Kimberly Abella CabreraNoch keine Bewertungen
- Hepatobiliary Disorders: Katrina Saludar Jimenez, R. NDokument42 SeitenHepatobiliary Disorders: Katrina Saludar Jimenez, R. NKatrinaJimenezNoch keine Bewertungen
- 1538 Exam 4 Cell Reg & GriefDokument35 Seiten1538 Exam 4 Cell Reg & GriefJade EdanoNoch keine Bewertungen
- Shock Types 141009102815 Conversion Gate01Dokument41 SeitenShock Types 141009102815 Conversion Gate01Samjaisheel SamsonNoch keine Bewertungen
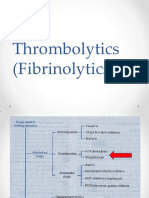
- Thrombolytics (Fibrinolytics)Dokument14 SeitenThrombolytics (Fibrinolytics)J lodhiNoch keine Bewertungen
- Thorax Breast and Lymphatic System AssesmentDokument106 SeitenThorax Breast and Lymphatic System AssesmentJanelle LasalaNoch keine Bewertungen
- Basics of ECGDokument32 SeitenBasics of ECGNachiket Vijay PotdarNoch keine Bewertungen
- Blood Transfusion PDFDokument10 SeitenBlood Transfusion PDFjamesNoch keine Bewertungen
- Care of Clients With Problems in OxygenationDokument5 SeitenCare of Clients With Problems in OxygenationSkyla FiestaNoch keine Bewertungen
- HW InotropesDokument3 SeitenHW InotropesNatalie YeohNoch keine Bewertungen
- Clinical Case Study - Online Discussion Form Fall 2020-1Dokument14 SeitenClinical Case Study - Online Discussion Form Fall 2020-1Sabrina Odies100% (1)
- Janeth Cardiovascular ExamDokument10 SeitenJaneth Cardiovascular ExammatthewandmaverickjeNoch keine Bewertungen
- GI Disorders NursingDokument93 SeitenGI Disorders NursingAmy100% (4)
- Intravenous InfusionDokument35 SeitenIntravenous InfusionDael GerongNoch keine Bewertungen
- Chest Tube DrainageDokument4 SeitenChest Tube DrainageJeah Lei CuencaNoch keine Bewertungen
- ABG Analysis NCLEX ExamDokument5 SeitenABG Analysis NCLEX ExamAngie MandeoyaNoch keine Bewertungen
- Vital SignsDokument51 SeitenVital SignsEstelita M. Dela CruzNoch keine Bewertungen
- Advanced Cardiac Life SupportDokument42 SeitenAdvanced Cardiac Life SupportDennis MiritiNoch keine Bewertungen
- Nursing Review Bullet For Funda (-Credits To OWNER-)Dokument4 SeitenNursing Review Bullet For Funda (-Credits To OWNER-)Camille Honeyleith Lanuza FernandoNoch keine Bewertungen
- Burn 2Dokument4 SeitenBurn 2lyn_aiNoch keine Bewertungen
- Perioperative NursingDokument18 SeitenPerioperative NursingJhosita Flora LarocoNoch keine Bewertungen
- COMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideVon EverandCOMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideNoch keine Bewertungen
- NURSING CARE OF ADULTS II: Passbooks Study GuideVon EverandNURSING CARE OF ADULTS II: Passbooks Study GuideNoch keine Bewertungen
- A Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsVon EverandA Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsNoch keine Bewertungen
- EP TCR 21 1 F10 InfanticideDokument26 SeitenEP TCR 21 1 F10 InfanticideAray Al-AfiqahNoch keine Bewertungen
- (Belle) Diabetes in PregnancyDokument3 Seiten(Belle) Diabetes in PregnancyAray Al-AfiqahNoch keine Bewertungen
- Sexual AbuseDokument4 SeitenSexual AbuseAray Al-AfiqahNoch keine Bewertungen
- Perkembangan Fetus Dr. Richardi., SP - OGDokument43 SeitenPerkembangan Fetus Dr. Richardi., SP - OGAray Al-AfiqahNoch keine Bewertungen
- 12 9 10 - PeltzDokument66 Seiten12 9 10 - Peltzagha_sajjad90Noch keine Bewertungen
- Head Injuries: Head Injuries Scalp Lacerations Skull Fractures Brain Injuries Complications of Head InjuriesDokument11 SeitenHead Injuries: Head Injuries Scalp Lacerations Skull Fractures Brain Injuries Complications of Head InjuriesAray Al-AfiqahNoch keine Bewertungen
- Trauma KepalaDokument43 SeitenTrauma KepalaAray Al-AfiqahNoch keine Bewertungen
- E BookDokument1 SeiteE BookAray Al-AfiqahNoch keine Bewertungen
- Stentofon Pulse: IP Based Intercom SystemDokument22 SeitenStentofon Pulse: IP Based Intercom SystemCraigNoch keine Bewertungen
- Network Fundamentas ITEC90Dokument5 SeitenNetwork Fundamentas ITEC90Psychopomp PomppompNoch keine Bewertungen
- Cyclic MeditationDokument8 SeitenCyclic MeditationSatadal GuptaNoch keine Bewertungen
- Mechanical Engineering - Workshop Practice - Laboratory ManualDokument77 SeitenMechanical Engineering - Workshop Practice - Laboratory Manualrajeevranjan_br100% (4)
- Maritta Koch-Weser, Scott Guggenheim - Social Development in The World Bank - Essays in Honor of Michael M. Cernea-Springer (2021)Dokument374 SeitenMaritta Koch-Weser, Scott Guggenheim - Social Development in The World Bank - Essays in Honor of Michael M. Cernea-Springer (2021)IacobNoch keine Bewertungen
- Alkosign Product CatalogeDokument20 SeitenAlkosign Product CatalogeShree AgrawalNoch keine Bewertungen
- Biological Assets Sample ProblemsDokument4 SeitenBiological Assets Sample ProblemsKathleenNoch keine Bewertungen
- Hydro Electric Fire HistoryDokument3 SeitenHydro Electric Fire HistorygdmurfNoch keine Bewertungen
- Internship Report Format For Associate Degree ProgramDokument5 SeitenInternship Report Format For Associate Degree ProgramBisma AmjaidNoch keine Bewertungen
- Mathematics Mock Exam 2015Dokument4 SeitenMathematics Mock Exam 2015Ian BautistaNoch keine Bewertungen
- 82686b - LOAD SHARING MODULEDokument2 Seiten82686b - LOAD SHARING MODULENguyễn Đình ĐứcNoch keine Bewertungen
- Chapter 08 - Change in Accounting Policy: Problem 8-1 (AICPA Adapted)Dokument5 SeitenChapter 08 - Change in Accounting Policy: Problem 8-1 (AICPA Adapted)Kimberly Claire AtienzaNoch keine Bewertungen
- 19c Upgrade Oracle Database Manually From 12C To 19CDokument26 Seiten19c Upgrade Oracle Database Manually From 12C To 19Cjanmarkowski23Noch keine Bewertungen
- MME 52106 - Optimization in Matlab - NN ToolboxDokument14 SeitenMME 52106 - Optimization in Matlab - NN ToolboxAdarshNoch keine Bewertungen
- Virtual Assets Act, 2022Dokument18 SeitenVirtual Assets Act, 2022Rapulu UdohNoch keine Bewertungen
- Union Test Prep Nclex Study GuideDokument115 SeitenUnion Test Prep Nclex Study GuideBradburn Nursing100% (2)
- 1B20 40Dokument4 Seiten1B20 40Electrival TcatallerNoch keine Bewertungen
- General Chemistry 2 Q1 Lesson 5 Endothermic and Exotheric Reaction and Heating and Cooling CurveDokument19 SeitenGeneral Chemistry 2 Q1 Lesson 5 Endothermic and Exotheric Reaction and Heating and Cooling CurveJolo Allexice R. PinedaNoch keine Bewertungen
- Elpodereso Case AnalysisDokument3 SeitenElpodereso Case AnalysisUsama17100% (2)
- Form Expense ClaimDokument2 SeitenForm Expense Claimviedelamonde_3868443Noch keine Bewertungen
- Epreuve Anglais EG@2022Dokument12 SeitenEpreuve Anglais EG@2022Tresor SokoudjouNoch keine Bewertungen
- Computers in Industry: Hugh Boyes, Bil Hallaq, Joe Cunningham, Tim Watson TDokument12 SeitenComputers in Industry: Hugh Boyes, Bil Hallaq, Joe Cunningham, Tim Watson TNawabMasidNoch keine Bewertungen
- Eurocode 3: Design of Steel Structures "ReadyDokument26 SeitenEurocode 3: Design of Steel Structures "Readywazydotnet80% (10)
- Formula:: High Low Method (High - Low) Break-Even PointDokument24 SeitenFormula:: High Low Method (High - Low) Break-Even PointRedgie Mark UrsalNoch keine Bewertungen
- Project Formulation and Appraisalpdf PDFDokument12 SeitenProject Formulation and Appraisalpdf PDFabhijeet varadeNoch keine Bewertungen
- Facebook: Daisy BuchananDokument5 SeitenFacebook: Daisy BuchananbelenrichardiNoch keine Bewertungen
- Speed, Velocity & Acceleration (Physics Report)Dokument66 SeitenSpeed, Velocity & Acceleration (Physics Report)Kristian Dave DivaNoch keine Bewertungen
- National Football League FRC 2000 Sol SRGBDokument33 SeitenNational Football League FRC 2000 Sol SRGBMick StukesNoch keine Bewertungen
- Sankranthi PDFDokument39 SeitenSankranthi PDFMaruthiNoch keine Bewertungen