Beruflich Dokumente
Kultur Dokumente
CS in Peritoneal TB
Hochgeladen von
apaelonganCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
CS in Peritoneal TB
Hochgeladen von
apaelonganCopyright:
Verfügbare Formate
52
CLINICAL ARTICLES
Corticosteroid Treatment of Peritoneal Tuberculosis
Abdulrahman A. Alrajhi, Magid A. Halim,
Abdullah Al-Hokail, Fahad Alrabiah, and
Kawther Al-Omran
From the Section of Infectious Diseases, Department of Medicine, King
Faisal Specialist Hospital and Research Centre, Riyadh, Saudi Arabia
The recent resurgence of tuberculosis (TB) is global. This
increase has been mainly attributed to HIV infection, but TB
also affects the HIV-negative population to a lesser extent [1].
The increase in the incidence of extrapulmonary TB over a 5year period was 20%, compared with an incidence of pulmonary tuberculosis of 3% in the United States [2]. Peritoneal TB
accounts for 3.3% of cases of extrapulmonary TB [3]. Most
patients with TB do well with antimycobacterial therapy alone.
The beneficial role of steroid administration in conjunction with
antituberculous chemotherapy was noted for few conditions,
notably pericarditis and meningitis [4 12]. Other conditions
for which steroid administration may be beneficial are severe
debilitation, hypoxia in association with miliary TB, and pleurisy [13 15].
See editorial response by Haas on pages 57 8.
Few reports regarding the effect of steroid use in conjunction
with antituberculous therapy for peritoneal TB have been pub-
Received 7 October 1997; revised 5 January 1998.
This work was presented in part at the 18th Annual Congress of the European
Society of Mycobacteriology and the 2nd International Symposium on Mycobacteria of Clinical Interest held in June 1997 in Cordoba, Spain.
Reprints or correspondence: Dr. Abdulrahman A. Alrajhi, Department of
Medicine (MBC 46), King Faisal Specialist Hospital and Research Centre,
P.O. Box 3354, Riyadh 11211, Saudi Arabia.
Clinical Infectious Diseases 1998;27:526
q 1998 by the Infectious Diseases Society of America. All rights reserved.
10584838/98/27010010$03.00
/ 9c51$$jy37
06-15-98 21:34:36
lished. Some studies showed beneficial effects, but others did
not [16, 17]. Considering the limited data [16] and extrapolating
from the benefit of steroid treatment for other TB conditions
[4 12], some of the physicians at our institution routinely
administer steroids along with antituberculous therapy to patients with peritoneal TB. We reviewed our experience with
corticosteroid administration combined with antituberculous
therapy for peritoneal TB; the outcome for these patients was
also reviewed.
Methods
We reviewed all cases of TB at King Faisal Specialist Hospital and Research Centre (Riyadh, Saudi Arabia) over a 10-year
period (1987 1996). Peritoneal TB was defined by at least
one of the following two criteria: isolation of Mycobacterium
tuberculosis from ascitic fluid or a peritoneal tissue biopsy
specimen, or observation of small tubercles in the peritoneum
during laparoscopy or laparotomy with biopsy-proven granulomata and a favorable clinical response to antituberculous chemotherapy. Basic demographic and diagnostic data were collected for all the patients meeting the inclusion criteria. Data
on follow-up, symptoms and signs, duration of follow-up,
emergency department visits and admissions because of abdominal pain, and laparotomy for treatment of intestinal obstruction after therapy were collected before data about treatment and steroid use. Data on treatment (including types and
duration of antituberculous therapy and dose and duration of
steroids) were collected by a different investigator to reduce
cidas
UC: CID
Downloaded from http://cid.oxfordjournals.org/ by guest on March 29, 2015
Corticosteroids are beneficial as treatment of certain tuberculosis syndromes. We reviewed
all cases of peritoneal tuberculosis diagnosed at our institution over 10 years to evaluate the
role of corticosteroid administration combined with antituberculous therapy. Nine patients were
treated with steroids plus antituberculosis agents (cases), and 26 received antituberculosis treatment only (controls). The two groups were not significantly different in terms of their basic
demographics or disease. Nineteen controls compared with one case had recurrent abdominal
pain. Seven controls had 17 emergency department visits because of abdominal pain. Intestinal
obstruction was diagnosed for five of these patients, four of whom underwent laparotomy revealing extensive adhesions. Three controls died, and no case died. No case required laparotomy,
had a diagnosis of intestinal obstruction, or visited the emergency department because of abdominal pain. These findings suggest that corticosteroid administration combined with antituberculosis treatment reduces the frequency of morbidity and complications in patients with peritoneal
tuberculosis.
CID 1998;27 (July)
Corticosteroid Treatment of Peritoneal Tuberculosis
Results
Forty-one cases met one or both of the inclusion criteria.
Six cases could not be included in the analysis: two had a
postmortem diagnosis (M. tuberculosis was isolated from ascitic fluid that was drawn during evaluation; these cases never
received anti-TB treatment), and four were referred to our institution for laparoscopy and were sent back to their referring
hospitals after the procedure (peritoneal TB was confirmed by
culture weeks later; no treatment was initiated at our institution,
and no follow-up was performed).
Detailed data were available for 35 patients. Nine were
treated with steroids and anti-TB therapy (cases), and 26 were
treated with anti-TB therapy without steroids (controls). The
cases of peritoneal TB in both groups were spread evenly over
the 10-year period. There were 17 males and 18 females. All
35 patients were followed up for a mean of 24 months (range,
2 118 months). The cases had a mean follow-up of 23 months
(range, 13 32 months; median, 22 months) compared with a
mean follow-up of 24 months (range, 2 118 months; median,
16 months) for the controls. The shorter minimal follow-up for
the controls resulted from the early death of a patient in this
group.
Ascitic fluid specimens from 27 patients were sent for culture
for acid-fast bacilli (AFB); M. tuberculosis was isolated from
14 (52%) of these patients. Peritoneal biopsy specimens from
26 patients were sent for AFB culture; M. tuberculosis was
isolated from 24 (92%) of these patients. AFB staining of
the two culture-negative biopsy specimens was negative, and
histopathologic examination of these specimens revealed caseating granulomata. M. tuberculosis was not isolated from ascitic
fluid or peritoneal biopsy specimens from one case and three
/ 9c51$$jy37
06-15-98 21:34:36
controls. These four patients were included in the analysis on
the basis of their laparoscopic and histopathologic findings and
their good clinical response to anti-TB medications. There was
no significant difference between the patients for whom cultures yielded M. tuberculosis and those for whom cultures
did not, in terms of their basic demographic data, duration of
symptoms, and results of ascitic fluid analysis. M. tuberculosis
was isolated from a mesenteric lymph node specimen from one
case, and two cases had chest roentgenograms suggestive of
TB. M. tuberculosis was isolated from cecum, adrenal gland,
and liver specimens from three controls, and seven controls
had chest roentgenograms suggestive of TB.
All patients received isoniazid and rifampin at the initiation
of therapy except for one control who received rifampin without isoniazid because of concerns that this patients chronic
viral hepatitis would worsen. Use of other first-line antituberculous drugs was similar in both groups. Cases were given steroids with antituberculous therapy according to the caring physicians practice. Cases received a dose of prednisone, 0.5
1.0 mg/(kgrd) for a mean of 6.6 weeks (range, 4 9 weeks).
Corticosteroids were given as oral prednisone once daily, and
the dose was tapered by 5 10 mg every 10 14 days. Steroids
were given at the initiation of anti-TB therapy to six cases and
after 3, 4, and 6 days to three cases.
The side effects attributed to steroids in the cases records
were limited to epigastric discomfort in two cases; the discomfort was treated by antacids in one and ranitidine in the other.
A third cases oral hypoglycemic requirements were increased
because of either steroid or rifampin administration. All noted
that side effects abated after the completion of the steroid
course.
There was no significant difference between the cases and
controls in terms of their mean age, gender distribution, mean
duration of symptoms before treatment, duration of treatment,
mean highest recorded temperature, results of ascitic fluid analysis, differential blood cell count, types and duration of anti-TB
therapy, duration of follow-up, and susceptibility pattern of the
isolated organism. These findings are summarized in table 1.
During follow-up, 19 controls (73%) complained repeatedly
of abdominal pain compared with one case (11%) (Fishers
exact test, P .0019). Seven controls (27%) had recurrent
vomiting compared with none of the cases. These seven controls presented to the emergency department 17 times because
of abdominal pain and vomiting. Five of these controls were
admitted, and intestinal obstruction with radiological evidence
of air-fluid levels was diagnosed; four required laparotomy.
Extensive adhesions were noted and thought to be the cause of
the intestinal obstruction. On the other hand, no case underwent
laparotomy or had a diagnosis of intestinal obstruction. None
of the cases visited the emergency department because of abdominal pain. These data are summarized in table 2.
One control had secondary infertility requiring in vitro fertilization on two occasions. A subgroup analysis of patients with
cidas
UC: CID
Downloaded from http://cid.oxfordjournals.org/ by guest on March 29, 2015
bias. If the patient complained of unexplained abdominal pain
during at least three different follow-up visits, recurrent abdominal pain was noted as a late complication of peritoneal TB.
Any emergency department visit because of abdominal pain
during or after treatment was recorded, as was intestinal obstruction (which was indicated in the patients record if supported by radiological evidence of air-fluid levels).
The patients were grouped into two groups: those treated
with steroids plus anti-TB therapy (cases) and those treated
with anti-TB therapy without steroids (controls). The two
groups were compared in terms of their basic demographics,
symptoms and signs, duration of symptoms before treatment,
diagnostic findings, susceptibility of M. tuberculosis isolates,
types and duration of treatment, and follow-up findings.
Data entry and analysis were performed by Epi-Info Version
6.04 (USD, Stone Mountain, GA) and Statistica Version 5.0
(StatSoft, Tulsa, OK). The Students t test was used to calculate
continuous variables, and the x2 or Fishers exact test was
used to calculate categorical variables. A P value of .05 was
considered significant.
53
54
Alrajhi et al.
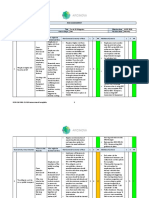
Table 1. Comparison between patients with peritoneal tuberculosis
who were treated with antituberculous therapy with (cases) or without
(controls) steroids.
Variable
Controls
P value
9
40 (1.85)
5 (56)
26
47 (2.8)
13 (50)
.20
.69
14.2 (2.63)
15.8 (2.70)
.76
38.2 (0.22)
37.8 (0.16)
.18
1,385 (553)
1,036 (272)
.53
68 (5.68)
78 (4.75)
.21
57 (3.38)
46 (4.82)
.32
13 (2.4)
10 (1.0)
.12
23 (2.0)
24 (5.5)
.85
peritoneal complications compared with patients without complications showed no significant difference in terms of their
initial demographics or disease criteria. The duration of symptoms before therapy for patients with complications was 8
weeks longer than that for patients without (mean, 18 weeks
vs. 10 weeks) but was not statistically significant (P .17),
probably because of the small numbers.
Three controls died. One of them died after 9 months of
treatment, of complications of hepatic cirrhosis and gastrointestinal bleeding related to hepatitis C virus infection. The other
two controls died after 8 and 10 weeks of treatment, respectively, of complications related to intestinal obstruction, perforation, and multiorgan failure in one and debilitation, massive
ascites, and sepsis in the other. No case died.
ated with no progression of TB if anti-TB chemotherapy was
used [22].
It took more than a decade before a comprehensive review of
steroid administration in TB cases was reported [23]. Adjuvant
steroid therapy has certain benefits in some cases of TB syndromes. Improved survival was noted when corticosteroids
were used by some investigators for treatment of tuberculous
meningitis [7 11]. There is also good evidence to support the
use of concurrent steroids with anti-TB therapy in cases of
tuberculous pericarditis as indicated by the Working Group on
Steroid Use of the Infectious Diseases Society of America
[12]. The antiinflammatory effect of steroids reduces restrictive
pericarditis and decreases the morbidity and mortality due to
tuberculous pericarditis [6].
On the other hand, for peritoneal TB, no conclusive evidence
for or against the combination of steroids plus anti-TB therapy
was found [12]. In 1969, Singh et al. [16] reported a nonblinded
study where they prospectively gave steroids to alternate patients with peritoneal TB. Of 47 patients, 23 were given 30
mg of prednisone daily for 3 months along with isoniazid and
streptomycin. The prednisone dose was tapered over the fourth
month to zero. There was no difference between the two groups
in terms of the initial symptomatic response. During followup, the patients treated with the steroid plus anti-TB therapy
had no intestinal obstruction compared with three of the 24
patients treated with anti-TB therapy only who had intestinal
obstruction requiring surgical intervention to free adhesive
bands. There were no deaths in either groups. To our knowledge, no other study in the English-language literature reported
the effect of steroids on the outcome of peritoneal TB.
In three recent reviews of steroid use in TB cases [13, 24,
25], peritoneal TB was not even discussed as a TB condition
Table 2. Outcome variables for patients with peritoneal tuberculosis
who were treated with antituberculous therapy with (cases) or without
(controls) steroids.
Variable
Discussion
Corticosteroids have significant antiinflammatory and immunosuppressive effects. They inhibit the production of some
cytokines by lymphocytes and mononuclear phagocytes [18].
Steroids also block the effect of cytokines on some target cells
[19], reduce the polymorphonuclear inflammatory response,
and decrease peripheral blood lymphocytes, monocytes, basophils, and eosinophils. Historically, the immunosuppressive effect of steroids on the progression of TB was noted before
the availability of anti-TB chemotherapy [20]. Corticosteroid
administration in cases of TB was thought to be contraindicated
[21], but subsequently corticosteroids were noted to be associ-
/ 9c51$$jy37
06-15-98 21:34:36
No. (%) of patients complaining
of repeated abdominal pain
No. (%) of patients visiting the
emergency department
because of abdominal pain
No. (%) of patients for whom
intestinal obstruction was
diagnosed
No. (%) of patients who
underwent laparotomy for
treatment of intestinal
obstruction
Controls
(n 26)
Cases
(n 9)
P value*
19 (73)
1 (11)
.0019
7 (27)
.15
5 (19)
.29
4 (15)
.55
* Fishers exact test; values are two-tailed.
cidas
UC: CID
Downloaded from http://cid.oxfordjournals.org/ by guest on March 29, 2015
No. of patients
Mean age in y (SE)
No. (%) of females
Mean duration of symptoms
before treatment in w
(SE)
Mean highest temperature
in 7C (SE)
Mean WBC count in ascitic
fluid in /mm3 (SE)
Mean lymphocyte
percentage in ascitic fluid
(SE)
Mean total protein level in
ascitic fluid in g/dL (SE)
Mean treatment duration in
mo (SE)
Mean follow-up duration in
mo (SE)
Cases
CID 1998;27 (July)
CID 1998;27 (July)
Corticosteroid Treatment of Peritoneal Tuberculosis
/ 9c51$$jy37
06-15-98 21:34:36
In our series, the three deaths of controls cannot be attributed
to the lack of steroid use. One patients death was related to
hepatic cirrhosis and gastrointestinal bleeding complicating viral hepatitis after several months of anti-TB treatment. The two
other patients died of complications of peritoneal TB that may
not have been prevented by steroid treatment.
Although our study was not prospective, we tried to reduce
reviewer bias by first collecting follow-up data and then collecting treatment data (including steroid use) by another investigator. A prospective, randomized, double-blind study would be
the investigation to convincingly prove that steroid use reduces
morbidity in cases of peritoneal TB. To our knowledge, similar
studies have never been performed for other conditions (e.g.,
tuberculous meningitis); nevertheless, the role of steroids as
adjuvant therapy for tuberculous meningitis is not disputed
now. Until results of a prospective, randomized, double-blind
trial are available, we advocate the use of steroids with antiTB drugs to reduce the frequency of complications and morbidity in patients with peritoneal TB.
Acknowledgments
The authors thank Dr. Abderrezak Bouchama for his assistance
with the French literature, Dr. Gary Miller for his thoughtful review
of the manuscript, Mary Louise Guy for record keeping, and Bernadette Martinez for secretarial assistance.
References
1. Sundre P, ten Dam G, Kochi A. Tuberculosis: a global overview of the
situation today. Bull World Health Organ 1992; 70:149 59.
2. Haas DW, Des Prez RM. Tuberculosis and acquired immunodeficiency
syndrome: a historical perspective on recent developments. Am J Med
1994; 96:439 50.
3. Reider HL, Snider DE, Cauthen GM. Extrapulmonary tuberculosis in the
United States. Am Rev Respir Dis 1990; 141:347 51.
4. Fowler NO. Tuberculous pericarditis. JAMA 1991; 266:99 103.
5. Rooney JJ, Crocco JA, Lyons HA. Tuberculous pericarditis. Ann Intern
Med 1970; 72:73 8.
6. Strang JIG, Gibson DG, Nunn AJ, Kakaza HHS, Girling DJ, Fox W.
Controlled trial of prednisolone as adjuvant in treatment of tuberculous
constrictive pericarditis in Transkei. Lancet 1987; 2:1418 22.
7. Kendig EL Jr. Steroids for meningitis: tuberculous and bacterial. Pediatr
Infect Dis J 1989; 8:541 2.
8. Molavi A, Lefrock JL. Tuberculous meningitis. Med Clin North Am 1985;
69:315 31.
9. Girgis NI, Farid Z, Kilpatrick ME, Sultan Y, Mikhail IA. Dexamethasone
adjunctive treatment for tuberculous meningitis. Pediatr Infect Dis J
1991; 10:179 83.
10. Shane SJ, Riley C. Tuberculosis meningitis. N Engl J Med 1953; 249:829
34.
11. Escobar JA, Belsey MA, Duenas A, Medina P. Mortality from tuberculosis
meningitis reduced by steroid therapy. Pediatrics 1975; 56:1050 5.
12. McGowan JE, Chesney PJ, Crossley KB, LaForce FM. Guidelines for the
use of systemic glucocorticosteroids in the management of selected
infections. J Infect Dis 1992; 165:1 13.
13. Alzeer AH, Fitzgerald JM. Corticosteroids and tuberculosis: risks and use
as adjunct therapy. Tuber Lung Dis 1993; 74:6 11.
cidas
UC: CID
Downloaded from http://cid.oxfordjournals.org/ by guest on March 29, 2015
that may benefit from steroid treatment. Bastani et al. [26]
reported using steroids as therapy for more than one-half of
their patients with tuberculous peritonitis but did not mention
the effect of this treatment on the patients outcomes. Other
studies of peritoneal TB retrospectively analyzed the role of
adding corticosteroid therapy to anti-TB treatment [27]; of 22
patients, six were given varying doses of prednisone at different
times in their disease course. No additional benefit was noted
from steroid treatment. The outcome parameters that Pieron et
al. [20] evaluated were different from those in our series. In
another French report [28] of 20 patients, six received steroid
therapy and had more rapid resolution of symptoms than did
other patients, but long-term follow-up was not reported. The
case definition in these and other series [17] was not clear, and
cases of abdominal or intestinal TB were also included.
Bennani et al. [17] prospectively randomized 50 of 100 patients to receive 30 mg of prednisone for the first 8 weeks.
Response to treatment was similar in the two groups. Followup laparoscopy after 12 or 24 months of therapy showed that
25 of 30 patients in the control group compared with 24 of
28 patients in the steroid group had persistent adhesions. The
methodology was not clear, and intervals for evaluation of
granulomata were not consistent in both groups. Clinical follow-up data were not reported.
In our series, all patients had confirmed tuberculosis of the
peritoneum. The cases and controls were quite comparable
in terms of criteria, disease severity, duration, antimicrobial
therapy, and microbial susceptibility. Although fewer patients
were treated with steroids than with anti-TB therapy alone,
only one of the nine cases complained of abdominal pain during
follow-up visits. Looking at a more objective outcome, the
number of emergency department visits by the controls was
17 (0.7 visit per patient) during the follow-up period. No case
visited the emergency department because of abdominal pain
or had a diagnosis of intestinal obstruction. Abdominal pain
was described in 83% of patients with peritoneal TB in other
series [26, 29].
Similar to the findings of Singh et al. [16], intestinal obstruction was diagnosed for five of our controls by clinical and
radiological parameters. Four of these patients required laparotomy for treatment of intestinal obstruction. Extensive adhesive
bands were noted in the abdomen and thought to be the cause
of the obstruction. These adhesions were attributed to previous
peritoneal TB and the associated inflammatory fibrotic process.
This process was probably modified by concurrent use of steroids, as shown in a randomized, prospective study of TB
pericarditis [6]. Khoury et al. [29] described 30 patients with
peritoneal TB; 14 presented to the emergency department, of
whom five had emergency abdominal surgery and two had
bowel resection for treatment of the obstruction. Of the 29
patients who had abdominal surgery, 12 had adhesions, and
one underwent another operation 1 month later for division of
the adhesions.
55
56
Alrajhi et al.
/ 9c51$$jy37
06-15-98 21:34:36
21. American Trudeau Society. The effect of cortisone and/or corticotrophin
on tuberculosis infection in man. American Review of Tuberculosis
1952; 66:245 56.
22. Houghton LE. Combined corticotropin therapy and chemotherapy in pulmonary tuberculosis. Lancet 1954; 1:595.
23. Horne NW. A critical evaluation of corticosteroids in tuberculosis. Advances in Tuberculosis Research 1966; 15:1 54.
24. Cisneros JR, Murray KM. Corticosteroids in tuberculosis. Ann Pharmacother 1996; 30:1298 303.
25. Senderovitz T, Viskum K. Corticosteroids and tuberculosis. Respir Med
1994; 88:561 5.
26. Bastani B, Shariatzadeh MR, Dehdashti F. Tuberculous peritonitis report
of 30 cases and review of the literature. Q J Med 1985; 56:549 57.
27. Pieron R, Lesobre B, Mafart Y, Boccara H. Aspects actuels de la tuberculose peritoneale. A propos de vingt-deux cas chez ladulte. Semaine des
Hopitaux 1980; 56:107 13.
28. Nenna AD, Quevauvillier J, Remmy JM, Raynaud de Lage C, Touboul J.
Tuberculosis peritoneale de ladult. Etude de 20 ans. Ann Med Interne
(Paris) 1977; 128:179 82.
29. Khoury GA, Payne CR, Harvey DR. Tuberculosis of the peritoneal cavity.
Br J Surg 1978; 65:808 11.
cidas
UC: CID
Downloaded from http://cid.oxfordjournals.org/ by guest on March 29, 2015
14. Horne NW. Prednisolone in treatment of pulmonary tuberculosis: a controlled trial. BMJ 1960; 5215:1751 6.
15. Lee CH, Wang WJ, Lan RS, Tsai YH, Chiang YC. Corticosteroids in the
treatment of tuberculous pleurisy: a double-blind, placebo-controlled,
randomized study. Chest 1988; 94:1256 9.
16. Singh MM, Bhargava AN, Jain KP. Tuberculous peritonitis. An evaluation
of pathogenetic mechanisms, diagnostic procedures and therapeutic
measures. N Engl J Med 1969; 281:1091 4.
17. Bennani A, Ouazzani H, Fadli F, Dafiri N, Ouazzani L. Aspects diagnos` propos
tiques et thrapeutiques au Maroc des tuberculoses pritonales. A
de 300 cas. Ann Gastroenterol Hepatol (Paris) 1988; 24:347 54.
18. Lew W, Oppenheim JJ, Matsushima K. Analysis of the suppression of IL-1
alpha and IL-1 beta production in human peripheral blood mononuclear
adherent cells by glucocorticoid hormones. J Immunol 1988; 140:1895
902.
19. Locksley RM, Wilson CB. Cell mediated immunity and its role in host
defense. In: Mandell GL, Bennett JE, Dolin R, eds. Mandell, Douglas,
and Bennetts principles and practice of infectious diseases. 4th ed. New
York: Churchill Livingstone, 1995:102 49.
20. Fred L, Levine MH, Rivo SB, Barbett TF. Development of active
tuberculosis during ACTH and cortisone therapy. JAMA 1951; 145:
242 6.
CID 1998;27 (July)
Das könnte Ihnen auch gefallen
- Template Status Pasien Igd Per BulanDokument2 SeitenTemplate Status Pasien Igd Per BulanapaelonganNoch keine Bewertungen
- Weekly Ruangan Bedah SarafDokument5 SeitenWeekly Ruangan Bedah SarafapaelonganNoch keine Bewertungen
- Weekly Report: Central Operating TheaterDokument75 SeitenWeekly Report: Central Operating TheaterapaelonganNoch keine Bewertungen
- JADWAL Ko-Ass PROBOLINGGO JUNI2014Dokument3 SeitenJADWAL Ko-Ass PROBOLINGGO JUNI2014apaelonganNoch keine Bewertungen
- Referat Cover Ot CtsDokument1 SeiteReferat Cover Ot CtsapaelonganNoch keine Bewertungen
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Physician's Health Evaluation For Prospective MissionaryDokument8 SeitenPhysician's Health Evaluation For Prospective MissionaryDarryl FranciscoNoch keine Bewertungen
- Care ProspectusDokument50 SeitenCare ProspectusJeya LakshmiNoch keine Bewertungen
- Abdul Sami Presentation On Panamin G UpdateDokument22 SeitenAbdul Sami Presentation On Panamin G UpdateNOMAN ALAMNoch keine Bewertungen
- Blueoptimum Plus Ppo Plan: Benefit SummaryDokument4 SeitenBlueoptimum Plus Ppo Plan: Benefit Summarylooksmart111Noch keine Bewertungen
- Ectopic Pregnancy Student LectureDokument19 SeitenEctopic Pregnancy Student Lectureapi-370504650% (4)
- RetinopathyDokument64 SeitenRetinopathySiti NcitNoch keine Bewertungen
- Basics of Medical Billing & CodingDokument86 SeitenBasics of Medical Billing & CodingRic Sánchez100% (3)
- Department of Health - Knock Out Tigdas 2007 - 2011-10-19Dokument3 SeitenDepartment of Health - Knock Out Tigdas 2007 - 2011-10-19daryl ann dep-asNoch keine Bewertungen
- Aceclofenac Efficacy and Safety Vs DiclofenacDokument6 SeitenAceclofenac Efficacy and Safety Vs DiclofenacpdelaxNoch keine Bewertungen
- 1 Pre Principles in MLS 1Dokument12 Seiten1 Pre Principles in MLS 1Maria Faith Jeneen BisnarNoch keine Bewertungen
- 9 - Chronic Tonsillitis & PharyngitisDokument31 Seiten9 - Chronic Tonsillitis & PharyngitisFajar Agung Prayogo100% (1)
- Salter, J. (2014) - Behind The Screen. Demos, London.Dokument122 SeitenSalter, J. (2014) - Behind The Screen. Demos, London.brenderdanNoch keine Bewertungen
- Perioperative Nursing 1Dokument2 SeitenPerioperative Nursing 1Rosie Cuasito100% (2)
- Answer All Questions: Model Question PaperDokument24 SeitenAnswer All Questions: Model Question PaperPrashant DhakadNoch keine Bewertungen
- SALIXIUM COVID-19 Rapid Antigen Test Flyer - ENG - 2021.07.16 - V6 (2 Pages)Dokument2 SeitenSALIXIUM COVID-19 Rapid Antigen Test Flyer - ENG - 2021.07.16 - V6 (2 Pages)driftailNoch keine Bewertungen
- Obg QuestionsDokument3 SeitenObg QuestionsRenuka JamwalNoch keine Bewertungen
- Executive SummaryDokument5 SeitenExecutive SummaryPachamuthu SchoolNoch keine Bewertungen
- Medical Helminthology Introduction PDFDokument13 SeitenMedical Helminthology Introduction PDFfaiz0% (1)
- Who BG PDFDokument21 SeitenWho BG PDFAastha AroraNoch keine Bewertungen
- Bezold AbscessDokument2 SeitenBezold AbscessSamuel anNoch keine Bewertungen
- LaryngitisDokument40 SeitenLaryngitisMikhail Guidicelli100% (1)
- Ref - Medscape - Cervical Cancer Treatment Protocols - Treatment ProtocolsDokument4 SeitenRef - Medscape - Cervical Cancer Treatment Protocols - Treatment Protocolsapoteker intanNoch keine Bewertungen
- Ways Radiation Is Used in Medicine - Cobalt 60 Radiotherapy MachineDokument22 SeitenWays Radiation Is Used in Medicine - Cobalt 60 Radiotherapy MachineKavidu KeshanNoch keine Bewertungen
- 76962CT0010006-01 en USDokument98 Seiten76962CT0010006-01 en USKathy ApergisNoch keine Bewertungen
- Lesson Exemplar in Mapeh Grade Level Learning Area QuarterDokument8 SeitenLesson Exemplar in Mapeh Grade Level Learning Area QuarterErwin Balid GasconNoch keine Bewertungen
- Iio Ow Waa B Bo Oaarrd D O Off N Nu Urrssiin NG GDokument34 SeitenIio Ow Waa B Bo Oaarrd D O Off N Nu Urrssiin NG GWichipirichiNoch keine Bewertungen
- RA-EHS-047-E2 - Covid-19 Site Risk Assessment 002Dokument16 SeitenRA-EHS-047-E2 - Covid-19 Site Risk Assessment 002Samsu RizalNoch keine Bewertungen
- Pain Mangement Flyer Word Document.-1Dokument2 SeitenPain Mangement Flyer Word Document.-1atifNoch keine Bewertungen
- Health Assessment MCQs QuizDokument6 SeitenHealth Assessment MCQs QuizAddisu Sertsu100% (1)
- Neral Information Title: Venue: Date: Participants:: Project ProposalDokument2 SeitenNeral Information Title: Venue: Date: Participants:: Project ProposalAida Potacag Buasen100% (1)