Beruflich Dokumente
Kultur Dokumente
2nd Sem - ImmunoSero - Introduction and Natural Immunity
Hochgeladen von
Aisle Malibiran PalerOriginalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
2nd Sem - ImmunoSero - Introduction and Natural Immunity
Hochgeladen von
Aisle Malibiran PalerCopyright:
Verfügbare Formate
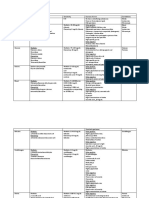
Chapter 1: Introduction and Natural Immunity
1960
Cells responsible for immune response were identified and
characterized
Immunology and Serology
Immunity and Immunization
Immunology
The study of hosts reactions when foreign substances are
introduced into the body
Antigen
Foreign substances that induces immune response
Variolation (1500)
Developed by Chinese
Exposing individuals to material from smallpox lesions
Theory: If a healthy individual was exposed as a child or
young adult, effects of the disease are minimized
Edward Jenner (1700)
Relationship between exposure to cowpox and immunity to
smallpox
Vaccination
From the Latin word vacca meaning cow
Injecting cellular material that provide protection
Cross-immunity
Phenomenon in which, exposure to one agent produces
protection against other agent
Louis Pasteur
First attenuated vaccine
Attenuation
Change; remains as basis for immunizations
May occur through:
o
Chemical
o
Heat
o
Aging
Cellular versus Humoral Immunity
Ellie Metchnikoff
Phagocytosis (cells eat cells)
o
Foreign objects introduced to transparent starfish
larvae become surrounded by motile cells
Immunity to disease was based on action of scavenger cells
Theory of Humoral Immunity
Noncellular elements in the blood were responsible for
protection from microorganisms
Almoth Wright
Linked 2 theories by showing that immune response
involved both cellular & humoral elements
o
Opsonins
Circulating factors
Coat bacteria so that they become more
susceptible to phagocytosis
o
Antibodies
Serum factors
Specific proteins
o
Acute phase reactants
Nonspecific factors
Increase nonspecifically in any infection
Natural or Innate Immunity
Ability of individual to resist infection by means of normally
present body function
Non-adaptive/ nonspecific
SAME for all pathogens
NO PRIOR EXPOSURE REQUIRED
Factors that influence Mechanism of Natural Immunity
1. Fatigue
2. Age
3. Nutrition
4. Genetic Determinants
5. Stress
Acquired Immunity
Specific for individual pathogen
REMEMBER PRIOR EXPOSURE
response upon repeated exposure
**Both systems (Natural and Acquired Immunity) are essential to
maintain good health and are dependent on one another for maximal
effectiveness
Two (2) parts of Natural Defense System
1. Internal
a. Cellular Mechanisms
b. Humoral Factors
2. External
External Defense System
Keep microorganisms from entering the body
Internal Defense System
Promote phagocytosis which results in foreign cell
destruction
o
Inflammation
Brings cells and humoral factors to are in need of
healing
External Defense System
External Defense System
Composed of structural barriers that prevent most infections
from entering the body
a. Unbroken skin
b. Mucosal Membrane surfaces
Skin
Major structural barrier
Secretions
Discourages the growth of microorganisms
o
Lactic acid
Sweat
Skin (pH 5.6) and Vagina (pH 5)
o
Fatty acid
Sebaceous glands
Maintain pH 5.6
o
Mucous secretions + cilia
Nasopharynx
Clears 90% of deposited materials
o
Urine
Flushing action
Slight acidity
Genitourinary tract
o
Hydrochloric acid
Stomach
pH 1, halts microbial growth
o
Tears and Saliva
Contains lysozyme that attacks cell wall of gram +
bacteria
o
Normal flora
Competitive exclusion
Keeps
pathogens
from
establishing
themselves
Internal Defense System
Internal Defense System
Second part of natural immunity
Cells and soluble factors plays essential parts
Recognize molecules that are unique to infectious organisms
e.g. recognizing mannose which is not evident in human
cells
Phagocytosis
Engulfment of cells or particulate matter
Chapter 1: Introduction and Natural Immunity
-
Immunology and Serology
Most important function of the internal defense system
Enhanced by soluble factors/ Acute phase reactants
a.
b.
c.
Acute-Phase Reactants
Acute-Phase Reactants
Normal serum constituents
Increases rapidly by at least 25% due to:
a. Infection
b. Injury
c. Trauma
Produce primarily by HEPATOCYTES within 12-24 hours
Cytokines
Intercellular signaling polypeptides
Cell messengers
a. IL-1
b. IL-6
c. TNF-
Mainly produced by MONOCYTES and MACROPHAGES at
the site of inflammation
C-Reactive Protein (CRP)
Trace constituent of serum
Increases rapidly within 2-6 hours following infection
Increase 100x-1000x
Peak Value: 48 hours
Member of Pentraxins
o
Protein with 5 subunits
Main substrate is phosphocholine
Capable of:
a. Opsonization
b. Agglutination
c. Precipitation
d. Complement activation
Binding is calcium-dependent and nonspecific
Able to act as defense until specific antibodies can be
produced (Acts before antibodies are produced)
Most widely used indicator of inflammation
noninvasive means of following the course of malignancy
and organ transplantation
Normal levels:
a. Men 1.5 mg/L
b. Women 2.5 mg/L
CRP Levels
a. Malignancy
b. Organ rejection
c. Bacterial and viral infection
d. Tuberculosis
e. Myocardial infarction
f.
Ischemic stroke
Mannose-Binding Protein
Aka Mannose-Binding Lectin
A trimer that acts as a opsonin
Calcium-dependent
Widely distributed on mucosal suface
Similar to C1q
Binding activates complement cascade
Normal concentrations: 10 g/ mL
MBP recurrent yeast infection
Alpha1-Antitrypsin
Major component of - band when serum is electrophoresed
General plasma inhibitor of Elastase (Protease)
o
Elastase
Endogenous enzyme that can degrade elastin and
collagen
Damages lung tissue in chronic pulmonary
inflammation
Mop up, counteracts the effects of neutrophil invasion
Regulates expression of proinflammatory cytokines
AAT
a. Premature emphysema
b. Idiopathic pulmonary fibrosis
Homozygous inheritance leads to:
a. Cirrhosis
b. Hepatitis
c. Hepatoma
Can also react with any serine protease
Haptoglobin
2- globulin
bind irreversibly to free hemoglobin released by intravascular
hemolysis
Haptoglobin + Free hemoglobin cleared by Kupffer cells
and parenchymal cells
plasma haptoglobin due to de novo synthesis in the liver
Increases 2x-10x following:
a. Inflammation
b. Stress
c. Tissue necrosis
Normal plasma concentration: 40-290 mg/dL
Function
a. Protects from kidney damage
b. Prevent loss of iron
c. Protection against oxidative damage by free
hemoglobin
o
Free hemoglobin
Powerful oxidizing agent
Generate peroxides and hydroxyl radicals
Fibrinogen
Most abundant coagulation factors
Forms the fibrin clot
Dimer
Normal levels: 100-400 mg/dL
Cleaved by thrombin to form fibrils that make up the fibrin
clot
Clot formation:
a. Increase the strength of the wound
b. Stimulates endothelial cell adhesion and
proliferation
c. Creates a barrier that helps prevent the spread of
microorganisms further into the body
Promote aggregation of RBC
Fibrinogen Levels
o
risk for coronary artery disease in women
Ceruloplasmin
** CRP Levels is a risk factor in Myocardial infarction and Ischemic
stroke
Serum Amyloid A
Increase 1000x
Apolipoprotein synthesized in the liver
Normal levels: 30 g/L
Associated with HDL; cholesterol metabolism
Contributes to site if tissue injury clean up
Recycles cholesterol and phospholipids for reuse un building
new membranes in acute inflammation
Bacterial Infection (SAA Levels) > Viral Infection (SAA
Levels)
Complement
Series of serum proteins
Mediates inflammation
o
Classical Cascade
Nine (9) proteins activated by bound antibodies in
a sequence
Major functions:
Opsonization
Chemotaxis
Lysis of cells
Chapter 1: Introduction and Natural Immunity
-
Immunology and Serology
Principal copper-transporting protein
Acts as ferroxidase
o
Feroxidase
Oxidizes iron from Fe2+ to Fe3+
Means of releasing iron from ferritin for binding to
transferrin
o
Wilsons disease
Autosomal recessive genetic disorder
Depletion of ceruloplasmin
Massive increase of copper in tissues
Copper accumulates in the liver and brain, cornea,
kidneys, and bones
2.
3.
4.
5.
Eosinophils
12-15 m in diameter
1-3% of circulating WBC
in parasitic infections, allergic reactions
Less efficient than neutrophils in phagocytosis because of
the lack of digestive enzymes
Main function:
o
Neutralize basophil and mast cell products
o
Kill parasites
Nucleus: Bilobed, ellipsoidal, eccentric
Cytoplasm: Filled with large orange to red-orange granules
a. Primary Granules
Contains:
Acid phosphatase
Arylsulfatase
b. Eosinophil-Specific Granules
Contains:
Major basic protein
Eosinophil cationic protein
Eosinophil peroxidase
Eosinophil-derived neurotoxin
Basophils
Less than 1% of circulating WBC
Smallest granulocyte (10-15 m)
IgE binds to Basophil cell membranes and granules release
constituents when in contact with antigen
Lacks hydrolytic enzymes but contains peroxidase
Contains coarse, densely staining deep-bluish-purple
granules which obscure the nucleus for hypersensitivity
reactions
a. Histamine
Vasoactive amine that contracts smooth muscle
b. Heparin
anticoagulant
c. Eosinophil-chemotactic factor
Mast Cells
Resemble basophils but larger
CT cells of mesenchymal origin
Small round nucleus and more granules
Life span: 9-18 months
For hypersensitivity reactions
Granules contain:
o
Acid phosphatase
o
Alkaline phosphatase
o
Protease
Monocytes
Mononuclear cells
Largest cells in peripheral blood
12-20 m diameter: average diameter 18 m
Irregularly folded or horseshoe-shaped nucleus that
occupies one half of the cell
Cytoplasm stains dull grayish blue and has a ground glass
appearance containing digestive vacuoles
4-10% of total circulating WBC
Stay in peripheral blood for up to 70 hours
Becomes macrophages (macrophages precursors)
Granules:
a. 1st type
Similar to lysosomes of neutrophils
Contains:
Cellular Defense Mechanisms
Five (5) Principal Types of WBC (Leukocytes)
1. Neutrophil
2. Eosinophil
3. Basophil
4. Monocyte
5. Lymphocyte
** Neutrophil, eosinophil, and basophil are granulocytes
Myeloid line
WBC that participate in phagocytosis
Arise from common precursor in the marrow
Neutrophil
Aka Polymorphonuclear neutrophilic leukocyte (PMN)
50-70% of total peripheral WBC
10-15 m in diameter
Nucleus: 2 & 5 lobes
Life span: 5 days
immediately in acute infection
Large number of neutral staining granules
a. Primary/ Azurophilic Granules
Contains:
Myeloperoxidase
Elastase
Proteinase 3
Lysozyme
Cathepsin G
defensins
b. Secondary Granules
Contains:
Collagenase
Lactoferrin
Lysozyme
Reduced NADPH oxidase
c. Tertiary granules
Newly discovered
Contains:
Gelatinase
Plasminogen activator
Lysosomes
Separate compartments that contain acid hydrolase
Marginating
Allow neutrophils to move from circulating blood to the
tissue by diapedesis
Diapedesis
Movement through the blood vessel walls
Selectins
Receptors that make neutrophils sticky and enhance
adherence to endothelial cells
Chemotaxins
Chemical messengers that cause cells to migrate in a
particular direction
Factors that are Chemotactic to Neutrophils
1. Complement
Proteins from coagulation cascade
Products from bacteria and virus
Platelet activating factor
Secretion from mast cells, lymphocyte, macrophages and
other neutrophils
Chapter 1: Introduction and Natural Immunity
b.
Peroxidase
Acid phosphatase
Arylsulfatase
2nd type
Contains:
- glucuronidase
Lysozyme
Lipase
No alkaline phosphatase
Tissue Macrophages
Arise from monocytes
Monocyte to macrophage
Enlarges between 25-80 m
Contains no peroxidase
Motility is slow; not as efficient as neutrophil
Life span: months
Macrophage + cytokines/ microorganism = macrophage
becomes activated
Cytokines
Chemical messengers released by T lymphocytes
Monocyte-Macrophage system
Initiate and regulate the immune respons
Immunology and Serology
Specific names of Macrophage according to location
1. Alveolar macrophage lungs
2. Kupffer cells liver
3. Microglial cells brain
4. Histiocytes connective tissue
Function of Macrophage
1. Microbial killing
2. Tumoricidal activity
3. Intracellular parasite eradication
4. Phagocytosis
5. Secretion of cell mediators
6. Antigen presentation
Dendritic cells
Covered with long membranous extensions
Main function:
o
Phagocytose antigen and present it to helper T
lymphocyte
Descendent of myeloid lines
Most potent phagocytic cell
1.
2.
3.
4.
Physical contact between WBC and foreign particle
Formation of phagosome
Fusion with cytoplasmic granules to form phagolysosome
Digestion and release of debris to the outside
Opsonins
To
prepare
for
eating
Serum proteins that attach to a foreign substance and help
prepare it for phagocytosis
Neutralizes surface charge on foreign particle
o
CRP
o
Complement components
o
Antibodies
Respiratory or Oxidative Burst
Occurs within the cell as the pseudopodia enclose the
particle within a vacuole
Inflammation
Inflammation
Overall reaction of the body to injury or invasion by infectious
agent
Classification based on location
1. Langerhans cells - skin
2. Interstital dendritic cells heart, lungs, liver, kidney, GIT
3. Interdigitating dendritic cells T lymphocyte areas of
secondary lymphoid tissue and thymus
4 Cardinal Signs or Clinical Symptoms
1. Redness
2. Swelling
3. Heat
4. Pain
Toll-like Receptors
Very similar molecules with toll found on human leukocytes
and some nonleukocyte cell types
Highest concentration of these receptors occurs on
monocytes, macrophages, and neutrophils
Enhances natural immunity
There are 11 slightly 11 different TLRs in humans
a. TLR2
Recognizes teichoic acid and peptidoglycan (gram
positive bacteria)
b. TLR4
Recognizes LPS (gram negative bacteria)
c. TLR1
Recognizes Mycobacteria
Major Events Associated with Inflammation
1. Inc. blood supply to infected areas
2. Inc. permeability caused by retraction of endothelial cells
3. Migration of WBC (Neutrophils) to surrounding tissue
4. Migration of macrophages to injured area
Histamine
Chemical mediator
Release from injured mast cell
Cause dilation of blood vessels and adds blood flow to
affected area
Acute-Phase Reactants
Soluble mediators
Amplification
Occurs through formation of clots by the coagulation system
and triggering of fibrinolytic system
Phagocytosis
4 Main Steps in Phagocytosis
Chapter 1: Introduction and Natural Immunity
Neutrophils
Mobilized within 30-60 minutes
Major cell type in acute inflammation
Emigration: 24-48 hours
Proportional to level of chemotactic factors
Macrophages
Immunology and Serology
Peaks at 16-48 hours
Clear areas by phagocytosis
Chronic Inflammation
Prolonged inflammation
Das könnte Ihnen auch gefallen
- Blood and Immunity Study GuideDokument4 SeitenBlood and Immunity Study GuideKimberly PollyNoch keine Bewertungen
- Gram Negative Rods of Enteric TractDokument2 SeitenGram Negative Rods of Enteric TractJohn TerryNoch keine Bewertungen
- The Pyridine Nucleotide CoenzymesVon EverandThe Pyridine Nucleotide CoenzymesJohannes EverseNoch keine Bewertungen
- Frontiers in Clinical Drug Research - Hematology: Volume 3Von EverandFrontiers in Clinical Drug Research - Hematology: Volume 3Noch keine Bewertungen
- Mockboards Reviewer FinalDokument161 SeitenMockboards Reviewer FinalRoselle Joyce Arce CalubanNoch keine Bewertungen
- Selected Topics in the History of Biochemistry. Personal Recollections. Part IIIVon EverandSelected Topics in the History of Biochemistry. Personal Recollections. Part IIIBewertung: 1 von 5 Sternen1/5 (1)
- Man Meets Microbes: An Introduction to Medical MicrobiologyVon EverandMan Meets Microbes: An Introduction to Medical MicrobiologyNoch keine Bewertungen
- ImmunoSeroLab M1 M4 MergedDokument14 SeitenImmunoSeroLab M1 M4 Mergedela kikayNoch keine Bewertungen
- Test Bank Exam 3Dokument81 SeitenTest Bank Exam 3Sajjad AhmadNoch keine Bewertungen
- Hematologic DisordersDokument32 SeitenHematologic DisordersQuolette ConstanteNoch keine Bewertungen
- EndocrinologyDokument12 SeitenEndocrinologyNathaniel Derige AndesNoch keine Bewertungen
- Red Blood Cell and Platelet PreservationDokument27 SeitenRed Blood Cell and Platelet PreservationiamdlawNoch keine Bewertungen
- BacillusDokument5 SeitenBacillusNeha SinhaNoch keine Bewertungen
- Lab Clin Test BankDokument87 SeitenLab Clin Test Bankemms meNoch keine Bewertungen
- Introduction To ImmunologyDokument9 SeitenIntroduction To ImmunologyDr-Rmz RabadiNoch keine Bewertungen
- Microbiology 15 Campylobacter, Vibrio Etc 431-449Dokument18 SeitenMicrobiology 15 Campylobacter, Vibrio Etc 431-449JenNoch keine Bewertungen
- Lymphoid SystemDokument11 SeitenLymphoid SystemSheena PasionNoch keine Bewertungen
- Poxviruses: Smallpox and Cowpox: Suzan Matar PHD in Medical Microbiology and ImmunologyDokument21 SeitenPoxviruses: Smallpox and Cowpox: Suzan Matar PHD in Medical Microbiology and ImmunologyDaniel AtiehNoch keine Bewertungen
- Vitamin B12 and FolateDokument12 SeitenVitamin B12 and FolateAllessandria DimaggioNoch keine Bewertungen
- Intro To ImmunohematoDokument48 SeitenIntro To Immunohematojong188Noch keine Bewertungen
- Liver Function (Clinical Chemistry)Dokument11 SeitenLiver Function (Clinical Chemistry)Patricia PerfectoNoch keine Bewertungen
- Hyponatremia: ElectrolytesDokument5 SeitenHyponatremia: ElectrolytesCyreen Jill Aliling100% (1)
- Bio 2 Quiz ReviewerDokument2 SeitenBio 2 Quiz ReviewerAlexandra RoderoNoch keine Bewertungen
- Clinical Chemistry Review 1 110Dokument6 SeitenClinical Chemistry Review 1 110DELLNoch keine Bewertungen
- 1 CCHM Trans LecDokument5 Seiten1 CCHM Trans LecCRUZ, ANNA MARIELLENoch keine Bewertungen
- CC Bishop QuestionsDokument3 SeitenCC Bishop QuestionsJohanna Kate DiestroNoch keine Bewertungen
- 2.13.08 Cold Agglutinin RogersDokument27 Seiten2.13.08 Cold Agglutinin RogersJessica StewartNoch keine Bewertungen
- Summary of Reagent Strip TestsDokument8 SeitenSummary of Reagent Strip TestsDarla YsavelNoch keine Bewertungen
- Types of ImmunityDokument2 SeitenTypes of ImmunityChiqui Lao DumanhugNoch keine Bewertungen
- History of PhlebotomyDokument46 SeitenHistory of PhlebotomyDorothy AtilanoNoch keine Bewertungen
- Microbiology Notes Chapers 1-2Dokument3 SeitenMicrobiology Notes Chapers 1-2dinkinpdNoch keine Bewertungen
- Bacteriostatic Agents: Drugs Which Bind To The 50s Ribosomal UnitDokument3 SeitenBacteriostatic Agents: Drugs Which Bind To The 50s Ribosomal UnitJoshua TrinidadNoch keine Bewertungen
- A. Two Forms of Carbohydrates: 1. Draw The FollowingDokument7 SeitenA. Two Forms of Carbohydrates: 1. Draw The FollowingJoshua TrinidadNoch keine Bewertungen
- Is PPT CompleteDokument456 SeitenIs PPT CompleteCelso Rodil IIINoch keine Bewertungen
- Immunology & Serology Week 1Dokument2 SeitenImmunology & Serology Week 1Romie SolacitoNoch keine Bewertungen
- Innate Immunity: Dr. Prasanna Honnavar, PHDDokument44 SeitenInnate Immunity: Dr. Prasanna Honnavar, PHDmus zaharaNoch keine Bewertungen
- Study Guide Hematologic AssessmentDokument5 SeitenStudy Guide Hematologic AssessmentNancy LemusNoch keine Bewertungen
- Gram Staining 01Dokument11 SeitenGram Staining 01MARICAR RAFAELNoch keine Bewertungen
- Microbiology 2Dokument53 SeitenMicrobiology 2pikachuNoch keine Bewertungen
- Assessment Exam in Cc1Dokument6 SeitenAssessment Exam in Cc1mika de guzmanNoch keine Bewertungen
- (MID) IMMUNOSERO - Chapter 13 - Hypersensitivity (Reviewer)Dokument6 Seiten(MID) IMMUNOSERO - Chapter 13 - Hypersensitivity (Reviewer)Aisle Malibiran PalerNoch keine Bewertungen
- 2 Blood and Immunology Module Study GuideDokument37 Seiten2 Blood and Immunology Module Study GuideMaryam FidaNoch keine Bewertungen
- Micropara Final LabNotesDokument75 SeitenMicropara Final LabNotescream oNoch keine Bewertungen
- Parasitology For Nursing LectureDokument13 SeitenParasitology For Nursing LectureebenezermanzanormtNoch keine Bewertungen
- Chapter 10 (Hemoglobin Metabolism)Dokument3 SeitenChapter 10 (Hemoglobin Metabolism)Joannah Marie100% (1)
- Aubf Case Study AbcdefDokument9 SeitenAubf Case Study AbcdefChiara Kate CodillaNoch keine Bewertungen
- Body FluidsDokument81 SeitenBody FluidsAris ResurreccionNoch keine Bewertungen
- 02 HemoglobinDokument78 Seiten02 HemoglobinpixiedustNoch keine Bewertungen
- Lecture 10 Vibrio, Aeromonas, Campylobacter and HelicobacterDokument4 SeitenLecture 10 Vibrio, Aeromonas, Campylobacter and HelicobacterRazmine RicardoNoch keine Bewertungen
- Fatty Acid OxidationDokument28 SeitenFatty Acid OxidationEmm NomanNoch keine Bewertungen
- T Cells and B CellsDokument3 SeitenT Cells and B CellsMarta DaNoch keine Bewertungen
- Pox VirusDokument13 SeitenPox VirusmukundvatsNoch keine Bewertungen
- Blood ComponentDokument17 SeitenBlood ComponentJes CmtNoch keine Bewertungen
- Amniotic Fluid: Group 5Dokument29 SeitenAmniotic Fluid: Group 5Francis ValdezNoch keine Bewertungen
- Reflection Paper My Sisters KeeperDokument1 SeiteReflection Paper My Sisters KeeperAllyson VillarealNoch keine Bewertungen
- Molbio HandoutDokument29 SeitenMolbio HandoutHazel FlorentinoNoch keine Bewertungen
- Physical Methods of Microbial ControlDokument65 SeitenPhysical Methods of Microbial ControlJuno MuniNoch keine Bewertungen
- Bacteseminar DSSMDokument4 SeitenBacteseminar DSSMPrincess AguirreNoch keine Bewertungen
- Biochemical Functions of LiverDokument94 SeitenBiochemical Functions of LiverMi PatelNoch keine Bewertungen
- (MID) IMMUNOSERO - Chapter 10 - Labeled ImmunoassaysDokument4 Seiten(MID) IMMUNOSERO - Chapter 10 - Labeled ImmunoassaysAisle Malibiran PalerNoch keine Bewertungen
- Genpath Midterms1Dokument3 SeitenGenpath Midterms1Aisle Malibiran PalerNoch keine Bewertungen
- (MT-RES) Manuscript Evaluation ToolDokument5 Seiten(MT-RES) Manuscript Evaluation ToolAisle Malibiran PalerNoch keine Bewertungen
- (MT-RES) Peer Evaluation (New)Dokument1 Seite(MT-RES) Peer Evaluation (New)Aisle Malibiran PalerNoch keine Bewertungen
- (MID) IMMUNOSERO - Chapter 13 - Hypersensitivity (Reviewer)Dokument6 Seiten(MID) IMMUNOSERO - Chapter 13 - Hypersensitivity (Reviewer)Aisle Malibiran PalerNoch keine Bewertungen
- 2nd Sem - Hema1 - An Overview of Clinical Laboratory HematologyDokument3 Seiten2nd Sem - Hema1 - An Overview of Clinical Laboratory HematologyAisle Malibiran PalerNoch keine Bewertungen
- Urinary System - LabDokument1 SeiteUrinary System - LabAisle Malibiran PalerNoch keine Bewertungen
- Research ProtocolDokument1 SeiteResearch ProtocolAisle Malibiran PalerNoch keine Bewertungen
- Bacte Chapt. 16Dokument4 SeitenBacte Chapt. 16Aisle Malibiran PalerNoch keine Bewertungen
- Bacteriology LectureDokument38 SeitenBacteriology LectureAisle Malibiran Paler100% (1)
- Bacte Chapt. 16Dokument4 SeitenBacte Chapt. 16Aisle Malibiran PalerNoch keine Bewertungen
- Paler, Aisle M. MT12221: Sonnet 144Dokument1 SeitePaler, Aisle M. MT12221: Sonnet 144Aisle Malibiran PalerNoch keine Bewertungen
- Pharma NotesDokument4 SeitenPharma NotesAisle Malibiran PalerNoch keine Bewertungen
- (F) Chapter 16 - Digestive System I, Oral Cavity and Associated StructuresDokument5 Seiten(F) Chapter 16 - Digestive System I, Oral Cavity and Associated StructuresAisle Malibiran PalerNoch keine Bewertungen
- Secrets of The New ManilaDokument1 SeiteSecrets of The New ManilaAisle Malibiran PalerNoch keine Bewertungen
- Microbiology, Bailey - S and Scotts Chapter 28, Moraxella and Related Orgs. by MT1232Dokument3 SeitenMicrobiology, Bailey - S and Scotts Chapter 28, Moraxella and Related Orgs. by MT1232Aisle Malibiran PalerNoch keine Bewertungen
- Chapter21 (Acinetobacter, Stenotrophomonas and Similar OrganismsDokument3 SeitenChapter21 (Acinetobacter, Stenotrophomonas and Similar OrganismsAisle Malibiran PalerNoch keine Bewertungen
- 1987 Philippine ConstitutionDokument1 Seite1987 Philippine ConstitutionAisle Malibiran PalerNoch keine Bewertungen
- I Am Filipino by Carlos RomuloDokument1 SeiteI Am Filipino by Carlos RomuloAisle Malibiran PalerNoch keine Bewertungen
- 1 - Overview of ComputersDokument99 Seiten1 - Overview of ComputersAisle Malibiran PalerNoch keine Bewertungen
- HistoryDokument1 SeiteHistoryAisle Malibiran PalerNoch keine Bewertungen
- Public Health Bylaws Under The Community CharterDokument9 SeitenPublic Health Bylaws Under The Community CharterAisle Malibiran PalerNoch keine Bewertungen
- I Am Filipino by Carlos RomuloDokument1 SeiteI Am Filipino by Carlos RomuloAisle Malibiran PalerNoch keine Bewertungen
- Ra8504 - Aids LawDokument8 SeitenRa8504 - Aids LawEnna TrivilegioNoch keine Bewertungen
- Description of The BarangayDokument1 SeiteDescription of The BarangayAisle Malibiran PalerNoch keine Bewertungen
- Igh 1Dokument4 SeitenIgh 1Aisle Malibiran PalerNoch keine Bewertungen
- Why Cysteine Is SpecialDokument3 SeitenWhy Cysteine Is SpecialAisle Malibiran PalerNoch keine Bewertungen
- FootnotesDokument6 SeitenFootnotesAisle Malibiran PalerNoch keine Bewertungen
- InsulinDokument10 SeitenInsulinAisle Malibiran PalerNoch keine Bewertungen
- 1and5.microscopes, Specializedstem Cells, Homeostasis - Answer KeyDokument1 Seite1and5.microscopes, Specializedstem Cells, Homeostasis - Answer KeyMCarmen López CastroNoch keine Bewertungen
- E&i QC Inspector Resum and DocumentsDokument24 SeitenE&i QC Inspector Resum and DocumentsIrfan 786pakNoch keine Bewertungen
- RAMSCRAM-A Flexible RAMJET/SCRAMJET Engine Simulation ProgramDokument4 SeitenRAMSCRAM-A Flexible RAMJET/SCRAMJET Engine Simulation ProgramSamrat JanjanamNoch keine Bewertungen
- Poster@IcepeDokument1 SeitePoster@IcepeAakash NawabNoch keine Bewertungen
- E-Cat35xt014 Xtro PhantomsDokument32 SeitenE-Cat35xt014 Xtro PhantomsKari Wilfong100% (5)
- Filtomat M300Dokument4 SeitenFiltomat M300Sasa Jadrovski100% (1)
- MPH EocDokument8 SeitenMPH EocGalaleldin AliNoch keine Bewertungen
- Eat Something DifferentDokument3 SeitenEat Something Differentsrajendr200100% (1)
- 20131022-Additive Manufacturing & Allied Technologies, PuneDokument56 Seiten20131022-Additive Manufacturing & Allied Technologies, Puneprakush_prakushNoch keine Bewertungen
- Lesson Plan Cot1Dokument9 SeitenLesson Plan Cot1Paglinawan Al KimNoch keine Bewertungen
- Balkhu Squatter SettlementDokument10 SeitenBalkhu Squatter SettlementShramina ShresthaNoch keine Bewertungen
- PTEG Spoken OfficialSampleTest L5 17mar11Dokument8 SeitenPTEG Spoken OfficialSampleTest L5 17mar11Katia LeliakhNoch keine Bewertungen
- MBF100 Subject OutlineDokument2 SeitenMBF100 Subject OutlineMARUTI JEWELSNoch keine Bewertungen
- VHP Series Five P9394Gsi S5: With Esm2 and Empact Emission Control SystemDokument2 SeitenVHP Series Five P9394Gsi S5: With Esm2 and Empact Emission Control SystemGabrielito PachacamaNoch keine Bewertungen
- CP R80.10 Installation and Upgrade GuideDokument246 SeitenCP R80.10 Installation and Upgrade GuideAlejandro OrtìzNoch keine Bewertungen
- Nationalisation of Insurance BusinessDokument12 SeitenNationalisation of Insurance BusinessSanjay Ram Diwakar50% (2)
- Comparativa Microplex F40 Printronix P8220 enDokument1 SeiteComparativa Microplex F40 Printronix P8220 enangel ricaNoch keine Bewertungen
- Industrial Training ReportDokument19 SeitenIndustrial Training ReportKapil Prajapati33% (3)
- Kharrat Et Al., 2007 (Energy - Fuels)Dokument4 SeitenKharrat Et Al., 2007 (Energy - Fuels)Leticia SakaiNoch keine Bewertungen
- (Walter Podolny, JR., John B. Scalzi) Construction PDFDokument354 Seiten(Walter Podolny, JR., John B. Scalzi) Construction PDFJuan Carlos CastroNoch keine Bewertungen
- Ram BookDokument52 SeitenRam BookRobson FletcherNoch keine Bewertungen
- Statistics 2Dokument121 SeitenStatistics 2Ravi KNoch keine Bewertungen
- Genstat Release 10.3de (Pc/Windows 7) 28 May 2012 06:35:59Dokument6 SeitenGenstat Release 10.3de (Pc/Windows 7) 28 May 2012 06:35:59Anna Nur HidayatiNoch keine Bewertungen
- First Certificate Star SB PDFDokument239 SeitenFirst Certificate Star SB PDFPatricia Gallego GálvezNoch keine Bewertungen
- CP AssignmentDokument5 SeitenCP AssignmentMSSM EngineeringNoch keine Bewertungen
- Takeover Strategies and DefencesDokument20 SeitenTakeover Strategies and DefencesJithu JoseNoch keine Bewertungen
- Merchant Accounts Are Bank Accounts That Allow Your Business To Accept Card Payments From CustomersDokument43 SeitenMerchant Accounts Are Bank Accounts That Allow Your Business To Accept Card Payments From CustomersRohit Kumar Baghel100% (1)
- SoC Showdown: Snapdragon 810 Vs Exynos 7420 Vs MediaTek Helio X10 Vs Kirin 935 - AndroidAuthority - PDDokument19 SeitenSoC Showdown: Snapdragon 810 Vs Exynos 7420 Vs MediaTek Helio X10 Vs Kirin 935 - AndroidAuthority - PDArpit SharmaNoch keine Bewertungen
- What Is The Effective Method For Dissolution of HDPE and LDPE - PDFDokument12 SeitenWhat Is The Effective Method For Dissolution of HDPE and LDPE - PDFAliNoch keine Bewertungen
- Teacher Resource Disc: Betty Schrampfer Azar Stacy A. HagenDokument10 SeitenTeacher Resource Disc: Betty Schrampfer Azar Stacy A. HagenRaveli pieceNoch keine Bewertungen