Beruflich Dokumente
Kultur Dokumente
Comparison of Dexmedetomidine and Clonidine As Adjuvant To Ropivacaine in Supraclavicular Brachial Plexus Nerve Blocks
Hochgeladen von
IOSRjournalOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Comparison of Dexmedetomidine and Clonidine As Adjuvant To Ropivacaine in Supraclavicular Brachial Plexus Nerve Blocks
Hochgeladen von
IOSRjournalCopyright:
Verfügbare Formate
IOSR Journal of Dental and Medical Sciences (IOSR-JDMS)
e-ISSN: 2279-0853, p-ISSN: 2279-0861.Volume 14, Issue 3 Ver. V (Mar. 2015), PP 91-97
www.iosrjournals.org
Comparison of Dexmedetomidine and Clonidine as Adjuvant to
Ropivacaine in Supraclavicular Brachial Plexus Nerve Blocks
Don Sebastian1, Ravi M2 * , Dinesh K3 ,Somasekharam P 4
1
(Junior Resident, Department of Anaesthesiology & Critical Care, Sri Devaraj Urs Medical College / Sri
Devaraj Urs University , India)
2,3,4
(Professors, Department of Anaesthesiology & Critical Care, Sri Devaraj Urs Medical College / Sri
Devaraj Urs University , India)
Abstract: Adjuncts to local anaesthetics for brachial plexus block enhances the quality and duration of
analgesia. The purpose of this study was to compare two alpha-2 agonists clonidine and dexmedetomidine,
when added as adjuvant to ropivacaine, in respect to onset, duration of sensory and motor block along with
duration of analgesia. After informed consent, Sixty ASA I and II patients scheduled for elective upper limb
surgeries under supraclavicular brachial plexus block in R L Jalappa Hospital were divided into two equal
groups in a randomized, double-blinded fashion. To ropivacaine 29 ml (0.5%), Group C received clonidine 1
ml (50 g) and Group D received dexmedetomidine 1ml (50g). Onset and duration of sensory and motor block,
duration of analgesia were studied in both the groups. Both groups were comparable with regard to age, sex
distribution, pulse rate and mean arterial blood pressure. There was no statistically significant difference.
Onset of sensory and motor blockade was faster in Group D, which is statistically significant. The Duration of
sensory block and motor block, analgesia was also greatest in group D, which is statistically significant. There
was no statistically significant difference between two groups in number of rescue analgesia requirement during
first 24 hrs. There were no adverse events noted in either group. All patients were haemodynamically stable
without requiring anaesthetists intervention. Dexmedetomidine when added to ropivacaine in supraclavicular
brachial plexus block had faster onset, greater duration of sensory and motor block and also, the duration of
analgesia, than clonidine. Dexmedetomidine is better adjuvant than clonidine when added as adjuvant to
ropivacaine in supraclavicular brachial plexus block.
Keywords - Ropivacaine, Dexmedetomidine, Clonidine, Supraclavicular Brachial plexus block
I.
Introduction
Brachial plexus block is one of the peripheral nerve blockade which has been used for surgeries of
upper limb. It provides both intraoperative anaesthesia as well as postoperative analgesia. Being a regional
anaesthesia technique, it has many advantages over general anaesthesia like effective analgesia with good motor
blockade, awake patient, extended postoperative analgesia, early mobilization, no airway manipulation,
avoiding polypharmacy and decreased incidence of postoperative nausea and vomiting.1
Many local anaesthetics has been used to produce brachial plexus block. Most common among them
being bupivacaine, because of its higher potency and prolonged duration of action. One of the disadvantage is
that its cardiotoxicity, especially with inadvertent injection into subclavian artery. So ropivacaine was developed
with properties similar to bupivacaine, having lower lipid solubility and less cardiotoxicity. 2
Many drugs are used as adjuvants for faster onset, denser block and for prolonging the duration of
peripheral nerve blockade. Alpha-2-adrenergic agonists were chosen for their sedative, analgesic,
antihypertensive and antiemetic properties along with decreased requirement of drugs. Clonidine a partial alpha
2 agonist has been shown to prolong the duration of anaesthesia and analgesia in nerve blocks. 7
Dexmedetomidine, a selective alpha2 agonist, with affinity eight times that of clonidine, also has been shown to
prolong the sensory and motor duration when added as an adjuvant to local anaesthetic in nerve blocks3,4,5,6
As not much literature is available with regard to use of dexmedetomidine as adjuvant in
supraclavcicular brachial plexus block with ropivacaine, the study was done.
II.
Methodology
A randomized double blind clinical study was done in R L Jalappa Hospital during the period from
February 2013 to May 2014. The study was done to compare the effects of clonidine 1ml (50 microgram) and
dexmedetomidine 1ml (50 microgram) when added as adjuvant to 29 ml ropivacaine 0.5% in supraclavicular
brachial plexus block using nerve stimulator for elective upper limb surgeries.
The study was undertaken after obtaining ethical committee clearance as well as informed consent
from all patients. Sixty patients aged between 18 to 55 years with ASA class I and II posted for elective upper
limb surgeries were included in the study. The study population were randomly divided using computer
DOI: 10.9790/0853-14359197
www.iosrjournals.org
91 | Page
Comparison of dexmedetomidine and clonidine as adjuvant to ropivacaine in
generated numbers into 2 groups with 30 patients in each group. Group C (n = 30) received 29 ml 0.5%
ropivacaine + 1 ml (50 microgram) clonidine Group D (n = 30) received 29 ml 0.5% ropivacaine + 1ml (50
microgram) dexmedetomidine. Patients with any bleeding disorder or patient on anticoagulants, neurological
deficits involving brachial plexus, patients with allergy to local anaesthetics, patients with history of drug
allergy to dexmedetomidine, clonidine, local infection at the injection site, patients on any sedatives or
antipsychotics, patients suffering from cardiac and pulmonary disease were excluded from study.
On arrival of patients in the operating room, an 18 gauge intravenous cannula was inserted on the nonoperating hand and an infusion of Ringer Lactate was started. The patients heart rate (HR), noninvasive
measurements of systolic blood pressure (SBP), diastolic blood pressure (DBP), mean arterial blood pressure
(MAP), continuous electrocardiogram (ECG) monitoring and haemoglobin oxygen saturation (SPO2) were
monitored. The baseline blood pressure and heart rate were recorded. The heart rate and rhythm were also
monitored from a continuous visual display of electrocardiogram from lead II.
The supraclavicular brachial plexus block was performed by the classical approach using a singleinjection, nerve-stimulator technique. The electrical stimulation was started with an intensity of 2.0mA and a
pulse width of 100s. Once the desired response was obtained that is a muscle twitch of the fingers that is
clearly visible the current strength was reduced in increments of 0.2mA gradually to 0.4mA. If the desired
response persisted at 0.4mA the drug solution was injected. The study drug was injected in 3ml increments,
after a negative aspiration test, with repeat aspirations every 3ml. During the intraoperative period heart rate,
systolic, diastolic and mean arterial pressures were noted every 5 minutes (mins) during the first 15mins, then
every 15 mins throughout the surgery and hourly thereafter.
The following parameters were studied:
Onset and duration of Sensory block:
Sensory block was assessed by pinprick test using the blunt end of a 26-gauge needle at each minute
after completion of drug injection in the dermatomal areas corresponding to median nerve, ulnar nerve, radial
nerve and musculocutaneous nerve till complete blockade.
Sensory block was assessed by a 3-point scale:
0 - normal sensation,
1 - loss of sensation of pinprick (analgesia),
2 - loss of sensation of touch (anaesthesia).
Onset time was defined as the time interval between the end of total local anaesthetic administration
and complete sensory block (score 2).
Duration of sensory block was defined as the time interval between the end of local anaesthetic
administration and the complete resolution of anaesthesia (score 0).
Onset and duration of motor block:
Motor blockade was assessed by Modified Bromage Scale
0- Normal motor function,
1- Ability to move only fingers,
2- Complete motor block with inability to move elbow, wrist and finger
Motor block onset time was defined as the time interval between the end of total local anaesthetic
administration and complete motor block (MBS score 2).
Duration of motor block was defined as the time interval from the onset to the recovery of complete motor
function (MBS score 0).
Duration of analgesia or first request for analgesic/ requirements in first 24 hrs:
Pain was assessed using a standard 10 cm Visual Analogue Scale (VAS) by an independent
anaesthesiologist. Time for first request for postoperative analgesic (duration of analgesia) was noted.
Intravenous inj tramadol 100mg with inj ondansetron 4mg was given as rescue analgesic if VAS score was
greater than or equal to 4. Number of requirements of rescue analgesia in first 24 hrs was noted.
Management of unsuccessful block:
Inadequate sensory and motor blockade beyond 30mins following the infiltration was considered as
unsuccessful block. In that circumstance, the block was supplemented with general anaesthesia.
Incidence of nausea, vomiting, horners syndrome, phrenic nerve palsy, pneumothorax, respiratory
depression and signs and symptoms of local anaesthetic toxicity were looked for and noted along with any side
DOI: 10.9790/0853-14359197
www.iosrjournals.org
92 | Page
Comparison of dexmedetomidine and clonidine as adjuvant to ropivacaine in
effects, if any. The above assessments were made by the principal investigator who was blinded to the drugs
used in the study.
III.
Statistical Analysis
Descriptive statistical analysis has been carried out in the present study. Results on continuous
measurements are presented as Mean SD and results on categorical measurements are presented in Number
(%). The student t test was used to determine whether there was a statistical difference between study groups
in the parameters measured.
In the above tests the p value of less than 0.05 was accepted as indicating statistical significance.
Data analysis was carried out using Statistical Package for Social Science (SPSS version 17) and Microsoft
word and Excel have been used to generate graphs, tables etc.
IV.
Observations And Results
There was no significant difference in the patient characteristics including age and gender. The
haemodynamic parameters taken into consideration were the heart rate mean arterial blood pressure and oxygen
saturation. Pulse rate in both the groups were comparable without any statistical significance. The mean arterial
pressures were also comparable in both the groups without any statistical significance.(Figure 1,2 )
Onset of sensory and motor block :
The mean time for onset of sensory block in group C was 11.6 1.754 min and in group D was 9.27
1.68 min. The mean time for onset of motor block in group C was 15.77 1.612 min and in group D was 12.87
1.592 min. Both differences were statistically significant (P < 0.01).(Table 1 and Figure 3)
Duration of sensory and motor block :
The mean duration of sensory block in group C was 463.5 40.325 min and in group D was 647.67
49.857 min. This difference was statistically significant (P < 0.01). The mean duration of motor block in group
C was 424.33 44.658 min and in group D was 600.83 46.722 min. This difference was also statistically
significant (P < 0.01) (figure 4 )
Duration of Analgesia:
In group C duration of analgesia was 510.83 42.306 min while for group D it was 720.83 44.16
min which is statistically significant. The number of rescue analgesic requirement in first 24 hours is similar in
two groups (not statistically significant). (Table 2)
V.
Complications
No complications / adverse effects were noted in the study groups during the procedure.
VI.
Discussion
For upper limb surgeries brachial plexus block provide both intraoperative anaesthesia as well as
postoperative analgesia and, it has an advantage over general anaesthesia like avoiding airway instrumentation,
polypharmacy, decreased incidence of nausea and vomiting, early mobilisation and extended postoperative
analgesia1. Of various approaches to brachial plexus, supraclavicular route is preferred as the narrowest part of
plexus is located there and there will be rapid, dense and predictable anaesthesia of entire upper limb. 7 Using
nerve stimulator we can avoid problems associated with the conventional technique like patient discomfort to
paresthesia , injury to nerve and surrounding structures , higher failure rates.8
The advantage of ropivacaine over bupivacaine is that it has similar properties to bupivacaine but with
lower lipid solubility and less cardiotoxicity.6 Adjuvants added to local anaesthetics results in faster onset denser
block and prolonged duration of analgesia especially alpha-2 agonists.9 In one study they used Fentanyl and
Tramadol as additives with Ropivacaine for Supraclavicular Brachial plexus blocks and they observed that in
fentanyl group the duration of sensory, motor block and analgesia was more ; VAS scores were also better in
fentanyl group.10
Various studies were done with clonidine as adjuvant to local anaesthetics. El Saied et al conducted a
study in which axillary brachial plexus blockade was performed with addition of clonidine to ropivacaine. 9 The
study showed that addition resulted in prolongation of sensory and motor block and analgesia without increased
incidence of side effects. In another study Giovanni Cucchiaro et al, evaluated the effects of clonidine on the
duration of sensory and motor block and analgesia time in children who underwent a variety of peripheral nerve
block including brachial plexus block and concluded that the addition of clonidine to bupivacaine and
ropivacaine can extend sensory and motor blocks. 11 In another study Casati et al. added clonidine to ropivacaine
(0.75%) for axillary brachial plexus block which provided increased post operative analgesia , without
DOI: 10.9790/0853-14359197
www.iosrjournals.org
93 | Page
Comparison of dexmedetomidine and clonidine as adjuvant to ropivacaine in
clinically relevant effects on the degree of sedation and cardiovascular homeostasis. 12 The above studies show
that selective 2- adrenoceptor agonist like clonidine when added as adjuvant to ropivacaine in different
peripheral nerve blocks potentiates the sensory and motor blockade and also prolonged duration of analgesia.
Dexmedetomidine is an 2 selective agonist. It acts in a manner similar to clonidine which is also an 2
selective agonist. Dexmedetomidine, the pharmacologically active d-isomer of medetomidine is a highly
specific and selective 2 adrenoceptor agonist with 2:1 binding selectivity ratio of 1620:1 as compared to
220:1 for clonidine, thus decreasing the unwanted side effects of 1 receptors. One of the highest densities of
2 receptors has been located in the locus coeruleus. The hypnotic and sedative effects of 2-adrenoceptor
activation have been attributed to this site in the CNS. It is also the site of origin for the descending
medullospinal noradrenergic pathway, known to be an important modulator of nociceptive neurotransmission. In
this region of the brain, 2-adrenergic and opioidergic systems have common effector mechanisms, indicating
that dexmedetomidine has a supraspinal site of action.. Presynaptic activation of 2 adrenoceptor in central
nervous system (CNS) inhibits the release of norepinephrine, terminating the propagation of pain signals and
their postsynaptic activation inhibits sympathetic activity, thereby decreasing HR and BP. 13
Aggarwal S, Aggarwal R, Gupta P compared the effects of adding dexmedetomidine to bupivacaine in
supraclavicular brachial plexus block in fifty patients. 14 They concluded that dexmedetomidine added as an
adjuvant to bupivacaine for supraclavicular brachial plexus block significantly shortens the onset time and
prolongs the duration of sensory and motor blocks and duration of analgesia. Patients in dexmedetomidine
group were adequately sedated with no adverse effects except bradycardia in one.
Feroz Ahmad Dar, Mohd Rafiq Najar, Neelofar Jan evaluated the effect of adding dexmedetomidine to
ropivacaine for axillary brachial plexus blockade in eighty patients scheduled for elective forearm and hand
surgeries. Sensory and motor block onset times were shorter when dexmedetomidine was added, also sensory
and motor blockade durations were longer along with duration of analgesia.15
Saumya Biswas, Ratan Kumar Das, Gauri Mukherjee, Tapas Ghose evaluated the effect of combining
dexmedetomidine with levobupivacine with respect to duration of motor and sensory block and duration of
analgesia. They found sensory and motor block durations were longer when dexmedetomidine was added as
adjuvant. Duration of analgesia was also significantly longer with addition of dexmedetomidine. 16
These studies shows that dexmedetomidine has faster onset of sensory and motor blockade with
prolonged duration of sensory and motor blockade with increased duration of analgesia when added as adjuvant
to local anaesthetics. So the study was done to compare clonidine and dexmedetomidine, two alpha-2 agonists,
as adjuvant to ropivacaine in respect to onset, duration of sensory and motor block along with duration of
analgesia.
The result of our study shows that all patients in both groups were comparable with respect to
demographic profile. Onset of sensory and motor blockade was faster in Group D which was statistically
significant. Duration of sensory and motor blockade was more in Group D which was also statistically
significant. The duration of analgesia was more in Group D, also statistically significant. These results show that
dexmedetomidine has faster onset of sensory and motor blockade, prolonged duration of sensory and motor
blockade and also increased duration of analgesia.
These results are consistant with other studies. Harshavardhana H S did a study aiming to test the
hypothesis that dexmedetomidine produces a better analgesia, motor block and post operative analgesia when
added as an adjuvant to ropivacaine 0.5% in supraclavicular brachial plexus block compared with clonidine. He
found that dexmedetomidine prolonged the duration of sensory and motor block and enhances the quality of
block as compared with clonidine when used as an adjuvant to ropivacaine in peripheral nerve block and
concluded that dexmedetomidine when added to ropivacaine for brachial plexus block is a better adjuvant
compared to clonidine.17
Swami SS, Keniya VM, Ladi SD, Rao R. compared clonidine and dexmedetomidine as an adjuvant to
local anaesthetic agent in supraclavicular brachial plexus block with respect to onset and duration of sensory and
motor block and duration of analgesia. Their finding was that dexmedetomidine, when added to local
anaesthetic in supraclavicular brachial plexus block enhanced the duration of sensory and motor block and also
the duration of analgesia. The time for rescue analgesia was prolonged in patients receiving dexmedetomidine
and also enhanced the quality of block as compared with clonidine.3
Saurabh Singh , H. S. Nanda conducted a comparative study of clonidine and dexmedetomidine as
adjuvant to 0.25% bupivacaine in supraclavicular brachial plexus block for duration of action and
haemodynamic changes. Their findings was that dexmedetomidine significantly prolonged the duration of action
and significant decrease in haemodynamic parameters, but did not require any active intervention for the same. 18
Both groups were comparable with regard to pulse rate, mean arterial blood pressure and oxygen
saturation. There was no statistically significant difference (P > 0.05). No adverse effects like bradycardia,
hypotension etc were noted in the study. The number of rescue analgesic requirements in first 24 hours is similar
in two groups (not statistically significant).
DOI: 10.9790/0853-14359197
www.iosrjournals.org
94 | Page
Comparison of dexmedetomidine and clonidine as adjuvant to ropivacaine in
To conclude, dexmedetomidine has faster onset, prolonged duration of sensory and motor block and
increased duration of analgesia as compared with clonidine when used as an adjuvant to ropivacaine in
peripheral nerve block.
VII.
Conclusion
We conclude that dexmedetomidine, when added as adjuvant to ropivacaine in supraclavicular brachial
plexus block has faster onset of sensory and motor blockade and, prolonged duration of sensory and motor
blockade and duration of analgesia, when compared with clonidine. No significant side effects were noted. So
dexmedetomidine is better adjuvant than clonidine in supraclavicular brachial plexus block for upper limb
surgeries.
References
[1].
[2].
[3].
[4].
[5].
[6].
[7].
[8].
[9].
[10].
[11].
[12].
[13].
[14].
[15].
[16].
[17].
[18].
Cousins MJ Bridenbaugh. Neural blockade in clinical anaesthesia and pain medicine. 4th ed.: Lippincott Williams and Wilkins;
2009.
McClure JH. Ropivacaine. British Journal of Anaesthesia 1996; 76:300-7.
Swami SS, Keniya VM, Ladi SD, Rao R. Comparison of dexmedetomidine and clonidine (2 agonist drugs) as an adjuvant to local
anaesthesia in supraclavicular brachial plexus block: A randomised double-blind prospective study. Indian J Anaesth 2012; 56:2439.
Yoshitomi T, Kohjitani A, Maeda S, Higuchi H, Shimada M, Miyawaki T. Dexmedetomidine Enhances the Local Anaesthetic
Action of Lidocaine via an -2A Adrenoceptor. Anesth Analg 2008; 107:96 101.
Saadawy I, Boker A, Elshahawy MA, Almazrooa A, Melibar S, Abdellatif AA, et al. Effect of dexmedetomidine on the
characteristics of bupivacaine in a caudal block in paediatrics. Acta Anaesthesiol Scand 2009; 53: 251256.
Esmaoglu A, Yegenoglu F, Akin A, Yildirim C. Dexmedetomidine Added to Levobupivacaine Prolongs Axillary Brachial Plexus
Block. Anesth Analg 2010; 111:1548-51.
Edward G Morgan, Maged S Mikhail, Micheal J Murray. Peripheral nerve blocks,4th ed. Chapter 17. In: Clinical anaesthesiology,
New Delhi: Tata McGraw-Hill; 2009.
Yasuda I, Hirano T, Ojima T, Ohhira N, Kaneko T and Yamamuro M. Supraclavicular brachial plexus block using a nerve
stimulator and an insulated needle. Br J Anaesth 1980; 52: 409.
El Saied AH, Steyn MP, Ansermino JM; Clonidine prolongs the effect of ropivacaine for axillary brachial plexus blockade. Can J
Anaesth 2000; 47: 962967.
Ravi Madhusudhana*, Krishna Kumar , Ramesh Kumar , Somasekharam Potli, Dinesh Karthik, Manu Kapil. Supraclavicular
brachial plexus block with 0.75 % ropivaciane and with additivestramadol, fentanyl- a comparative pilot study. Int J Biol Med Res.
2011; 2(4): 1061 1063.
Cucchiaro G, Ganesh A; The effects of clonidine on postoperative analgesia after peripheral nerve blockade in children. Anest h
Analg 2007;104: 532-537.
Casati A, Magistris L, Beccaria P, Cappelleri G, Aldegheri G, Fanelli G; Improving postoperative analgesia after axillary brachial
plexus anesthesia with 0.75% ropivacaine: A double-blind evaluation of adding clonidine. Minerva Anestesiol 2001; 67: 407412.
12 Gertler R, Brown HC, Mitchell DH, Silvius EN. Dexmedetomidine: a novel sedative-analgesic agent. BUMC Proceedings 2001;
14:1321.
Agarwal S, Aggarwal R, Gupta P. Dexmedetomidine prolongs the effect of bupivacaine in supraclavicular brachial plexus block. J
Anaesthesiol Clin Pharmacol 2014;30;36-40.
Dar F A , Najar M R, Jan N .Dexmedetomidine Added to Ropivacaine Prolongs Axillary Brachial Plexus Block. International
Journal of Biomedical and Advance Research 2013; 4: 719-722.
Biswas S, Das RK, Mukherjee G, Ghose T. Dexmedetomidine an Adjuvant to Levobupivacaine in Supraclavicular Brachial Plexus
Block: A Randomized Double Blind Prospective Study. Ethiop J Health Sci 2014; 24: 203208.
Harshavardhana H S .Efficacy of Dexmedetomidine Compared to Clonidine added to Ropivacaine in Supraclavicular Nerve Blocks:
A Prospective, Randomized, Double Blind Study. Int J Med Health Sci 2014;3;127-133.
Singh S, Nanda H S et al. A comparative study of clonidine and dexmedetomidine as adjuvant o 0.25% bupivacaine in
supraclavicular brachial plexus block for post operative analgesia and sedation. International Journal of Current Research 2014 ; 9:
876-879.
Figure 1: comparison of the pulse rate between the groups at different time intervals
DOI: 10.9790/0853-14359197
www.iosrjournals.org
95 | Page
Comparison of dexmedetomidine and clonidine as adjuvant to ropivacaine in
Figure 2: comparison of the mean arterial blood pressure between the groups at different time intervals
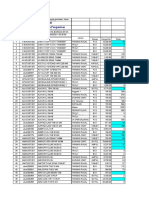
Table 1: Sensory and motor block onset time, duration of sensory and motor block and analgesia
durations in both groups
Figure 3: comparison of onset of sensory and motor blockade among dexmedetomidine and clonidine groups.
DOI: 10.9790/0853-14359197
www.iosrjournals.org
96 | Page
Comparison of dexmedetomidine and clonidine as adjuvant to ropivacaine in
Figure 4: comparison of duration of sensory blockade, motor blockade and duration of analgesia among
dexmedetomidine and clonidine groups. .
Table 2 : shows the number of times the patients in both dexmedetomidine and clonidine groups
required rescue analgesia in 24 hrs. There is no significant statistical difference between the groups
(P>0.05).
Number of rescue
analgesia in 24 hrs
Clonidine
Dexmedetomidine
P value
1.5 0.5085
1.4666 0.5074
0.7687
DOI: 10.9790/0853-14359197
www.iosrjournals.org
97 | Page
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (120)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- SOAP Notes: AuthorsDokument6 SeitenSOAP Notes: AuthorsRanita Kumalasari100% (4)
- Kinesics, Haptics and Proxemics: Aspects of Non - Verbal CommunicationDokument6 SeitenKinesics, Haptics and Proxemics: Aspects of Non - Verbal CommunicationInternational Organization of Scientific Research (IOSR)Noch keine Bewertungen
- Soil Transmitted Helminth Infections: The Nature, Causes and Burden of The ConditionDokument79 SeitenSoil Transmitted Helminth Infections: The Nature, Causes and Burden of The ConditionYokaiCO100% (1)
- A Proposed Framework On Working With Parents of Children With Special Needs in SingaporeDokument7 SeitenA Proposed Framework On Working With Parents of Children With Special Needs in SingaporeInternational Organization of Scientific Research (IOSR)Noch keine Bewertungen
- Socio-Ethical Impact of Turkish Dramas On Educated Females of Gujranwala-PakistanDokument7 SeitenSocio-Ethical Impact of Turkish Dramas On Educated Females of Gujranwala-PakistanInternational Organization of Scientific Research (IOSR)Noch keine Bewertungen
- The Role of Extrovert and Introvert Personality in Second Language AcquisitionDokument6 SeitenThe Role of Extrovert and Introvert Personality in Second Language AcquisitionInternational Organization of Scientific Research (IOSR)Noch keine Bewertungen
- Attitude and Perceptions of University Students in Zimbabwe Towards HomosexualityDokument5 SeitenAttitude and Perceptions of University Students in Zimbabwe Towards HomosexualityInternational Organization of Scientific Research (IOSR)Noch keine Bewertungen
- A Review of Rural Local Government System in Zimbabwe From 1980 To 2014Dokument15 SeitenA Review of Rural Local Government System in Zimbabwe From 1980 To 2014International Organization of Scientific Research (IOSR)Noch keine Bewertungen
- "I Am Not Gay Says A Gay Christian." A Qualitative Study On Beliefs and Prejudices of Christians Towards Homosexuality in ZimbabweDokument5 Seiten"I Am Not Gay Says A Gay Christian." A Qualitative Study On Beliefs and Prejudices of Christians Towards Homosexuality in ZimbabweInternational Organization of Scientific Research (IOSR)Noch keine Bewertungen
- Relationship Between Social Support and Self-Esteem of Adolescent GirlsDokument5 SeitenRelationship Between Social Support and Self-Esteem of Adolescent GirlsInternational Organization of Scientific Research (IOSR)Noch keine Bewertungen
- Investigation of Unbelief and Faith in The Islam According To The Statement, Mr. Ahmed MoftizadehDokument4 SeitenInvestigation of Unbelief and Faith in The Islam According To The Statement, Mr. Ahmed MoftizadehInternational Organization of Scientific Research (IOSR)Noch keine Bewertungen
- The Impact of Technologies On Society: A ReviewDokument5 SeitenThe Impact of Technologies On Society: A ReviewInternational Organization of Scientific Research (IOSR)100% (1)
- An Evaluation of Lowell's Poem "The Quaker Graveyard in Nantucket" As A Pastoral ElegyDokument14 SeitenAn Evaluation of Lowell's Poem "The Quaker Graveyard in Nantucket" As A Pastoral ElegyInternational Organization of Scientific Research (IOSR)Noch keine Bewertungen
- Comparative Visual Analysis of Symbolic and Illegible Indus Valley Script With Other LanguagesDokument7 SeitenComparative Visual Analysis of Symbolic and Illegible Indus Valley Script With Other LanguagesInternational Organization of Scientific Research (IOSR)Noch keine Bewertungen
- Motivational Factors Influencing Littering in Harare's Central Business District (CBD), ZimbabweDokument8 SeitenMotivational Factors Influencing Littering in Harare's Central Business District (CBD), ZimbabweInternational Organization of Scientific Research (IOSR)Noch keine Bewertungen
- Assessment of The Implementation of Federal Character in Nigeria.Dokument5 SeitenAssessment of The Implementation of Federal Character in Nigeria.International Organization of Scientific Research (IOSR)Noch keine Bewertungen
- Edward Albee and His Mother Characters: An Analysis of Selected PlaysDokument5 SeitenEdward Albee and His Mother Characters: An Analysis of Selected PlaysInternational Organization of Scientific Research (IOSR)Noch keine Bewertungen
- Transforming People's Livelihoods Through Land Reform in A1 Resettlement Areas in Goromonzi District in ZimbabweDokument9 SeitenTransforming People's Livelihoods Through Land Reform in A1 Resettlement Areas in Goromonzi District in ZimbabweInternational Organization of Scientific Research (IOSR)Noch keine Bewertungen
- Topic: Using Wiki To Improve Students' Academic Writing in English Collaboratively: A Case Study On Undergraduate Students in BangladeshDokument7 SeitenTopic: Using Wiki To Improve Students' Academic Writing in English Collaboratively: A Case Study On Undergraduate Students in BangladeshInternational Organization of Scientific Research (IOSR)Noch keine Bewertungen
- Importance of Mass Media in Communicating Health Messages: An AnalysisDokument6 SeitenImportance of Mass Media in Communicating Health Messages: An AnalysisInternational Organization of Scientific Research (IOSR)Noch keine Bewertungen
- Role of Madarsa Education in Empowerment of Muslims in IndiaDokument6 SeitenRole of Madarsa Education in Empowerment of Muslims in IndiaInternational Organization of Scientific Research (IOSR)Noch keine Bewertungen
- Beowulf: A Folktale and History of Anglo-Saxon Life and CivilizationDokument3 SeitenBeowulf: A Folktale and History of Anglo-Saxon Life and CivilizationInternational Organization of Scientific Research (IOSR)Noch keine Bewertungen
- Human Rights and Dalits: Different Strands in The DiscourseDokument5 SeitenHuman Rights and Dalits: Different Strands in The DiscourseInternational Organization of Scientific Research (IOSR)Noch keine Bewertungen
- Women Empowerment Through Open and Distance Learning in ZimbabweDokument8 SeitenWomen Empowerment Through Open and Distance Learning in ZimbabweInternational Organization of Scientific Research (IOSR)Noch keine Bewertungen
- Substance Use and Abuse Among Offenders Under Probation Supervision in Limuru Probation Station, KenyaDokument11 SeitenSubstance Use and Abuse Among Offenders Under Probation Supervision in Limuru Probation Station, KenyaInternational Organization of Scientific Research (IOSR)Noch keine Bewertungen
- An Exploration On The Relationship Among Learners' Autonomy, Language Learning Strategies and Big-Five Personality TraitsDokument6 SeitenAn Exploration On The Relationship Among Learners' Autonomy, Language Learning Strategies and Big-Five Personality TraitsInternational Organization of Scientific Research (IOSR)Noch keine Bewertungen
- The Lute Against Doping in SportDokument5 SeitenThe Lute Against Doping in SportInternational Organization of Scientific Research (IOSR)Noch keine Bewertungen
- Classical Malay's Anthropomorphemic Metaphors in Essay of Hikajat AbdullahDokument9 SeitenClassical Malay's Anthropomorphemic Metaphors in Essay of Hikajat AbdullahInternational Organization of Scientific Research (IOSR)Noch keine Bewertungen
- Designing of Indo-Western Garments Influenced From Different Indian Classical Dance CostumesDokument5 SeitenDesigning of Indo-Western Garments Influenced From Different Indian Classical Dance CostumesIOSRjournalNoch keine Bewertungen
- Design Management, A Business Tools' Package of Corporate Organizations: Bangladesh ContextDokument6 SeitenDesign Management, A Business Tools' Package of Corporate Organizations: Bangladesh ContextInternational Organization of Scientific Research (IOSR)Noch keine Bewertungen
- Micro Finance and Women - A Case Study of Villages Around Alibaug, District-Raigad, Maharashtra, IndiaDokument3 SeitenMicro Finance and Women - A Case Study of Villages Around Alibaug, District-Raigad, Maharashtra, IndiaInternational Organization of Scientific Research (IOSR)Noch keine Bewertungen
- A Study On The Television Programmes Popularity Among Chennai Urban WomenDokument7 SeitenA Study On The Television Programmes Popularity Among Chennai Urban WomenInternational Organization of Scientific Research (IOSR)Noch keine Bewertungen
- How Is Turner Syndrome DiagnosedDokument9 SeitenHow Is Turner Syndrome DiagnosedAnonymous lKO78aNoch keine Bewertungen
- Case Study 7 - Antepartum BleedingDokument2 SeitenCase Study 7 - Antepartum BleedingRahul Tharwani100% (1)
- Nervous SystemDokument92 SeitenNervous SystemmaricarNoch keine Bewertungen
- Intro To HematologyDokument9 SeitenIntro To HematologyDayledaniel SorvetoNoch keine Bewertungen
- Drug Name Dosage, Route, Frequency Mechanism of Action Indication Contraindication Adverse Effect Nursing ResponsibilitiesDokument1 SeiteDrug Name Dosage, Route, Frequency Mechanism of Action Indication Contraindication Adverse Effect Nursing ResponsibilitiesJonna Mae TurquezaNoch keine Bewertungen
- Adilah TranskripDokument1 SeiteAdilah Transkripadik_mira893219Noch keine Bewertungen
- Dental JOURNAL: Geographic Tongue in A 6 Year Old Child: A Case Report With Review of LiteratureDokument6 SeitenDental JOURNAL: Geographic Tongue in A 6 Year Old Child: A Case Report With Review of LiteraturewennyNoch keine Bewertungen
- Critical Illness Rider LICDokument1 SeiteCritical Illness Rider LICSwadeep Kumar ShuklaNoch keine Bewertungen
- CV - Updated April 2023Dokument6 SeitenCV - Updated April 2023api-641524095Noch keine Bewertungen
- Alhydrogel TDSDokument2 SeitenAlhydrogel TDSMirela IoanaNoch keine Bewertungen
- Spinal OrthosisDokument16 SeitenSpinal OrthosisChristya Ari NugrahaNoch keine Bewertungen
- INTRODUCTION of Tuberculosis Final NewDokument2 SeitenINTRODUCTION of Tuberculosis Final Newbatch1Noch keine Bewertungen
- Rs Pena 98 Jl. Pemuda Pengasinan N0.36 Kec Gn. Sindur Bogor Telp: (021) 7587 4401,-FaxDokument61 SeitenRs Pena 98 Jl. Pemuda Pengasinan N0.36 Kec Gn. Sindur Bogor Telp: (021) 7587 4401,-Faxrichard fernandoNoch keine Bewertungen
- 2Dokument78 Seiten2api-3744136Noch keine Bewertungen
- Brochure Biology & Medicine 03 2022 - CompressedDokument40 SeitenBrochure Biology & Medicine 03 2022 - CompressedMerida Bertrand Alex PodgaNoch keine Bewertungen
- Soal Bahasa Inggris - Evaluasi TestDokument9 SeitenSoal Bahasa Inggris - Evaluasi TestHamdani IlhamNoch keine Bewertungen
- Levels of Organization PowerpointDokument15 SeitenLevels of Organization PowerpointGloriefe QuitongNoch keine Bewertungen
- Euthanasia Methods For Dogs and CatsDokument3 SeitenEuthanasia Methods For Dogs and Catssharath_mbNoch keine Bewertungen
- Literature ReviewDokument7 SeitenLiterature ReviewResianaPutriNoch keine Bewertungen
- 2021 American College of Rheumatology Guideline For The Treatment of Rheumatoid ArthritisDokument30 Seiten2021 American College of Rheumatology Guideline For The Treatment of Rheumatoid Arthritisjose pablo quero reyesNoch keine Bewertungen
- Allied Mcv100 ManualDokument36 SeitenAllied Mcv100 ManualRigneshvaren ThangamoneyNoch keine Bewertungen
- Polymerase Chain ReactionDokument22 SeitenPolymerase Chain ReactionPoornaBasuri100% (1)
- Case OSCEsDokument74 SeitenCase OSCEsHassan R. G.75% (4)
- Black Seed PresentationDokument25 SeitenBlack Seed Presentationsakib khanNoch keine Bewertungen
- Antifungal AgentsDokument37 SeitenAntifungal AgentsChandrashekhar UnakalNoch keine Bewertungen
- 200 Bed Hospital Project ReportDokument59 Seiten200 Bed Hospital Project ReporttonyNoch keine Bewertungen
- Food Safety in Hospitality Industry: Hari PurnomoDokument6 SeitenFood Safety in Hospitality Industry: Hari PurnomoYANNA INGKOHNoch keine Bewertungen
- First AidDokument22 SeitenFirst Aidlinaj67% (3)