Beruflich Dokumente
Kultur Dokumente
PD0909 03 PDF
Hochgeladen von
Desi RatnaningtyasOriginalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
PD0909 03 PDF
Hochgeladen von
Desi RatnaningtyasCopyright:
Verfügbare Formate
Update on Diagnosis
and Topical
Management of
Erythrasma
This under-diagnosed cutaneous infection is caused by a bacterium
but may respond to anti-fungal therapies.
By Joseph Bikowski, MD
September 2009 | Practical Dermatology | 47
Photos courtesy of Joseph Bikowski, MD
rythrasma is a frequently
under-diagnosed cutaneous
infection caused by
Corynebacterium minutissimum. It commonly affects body
folds, particularly the groin, and
has been identified as one of the
leading causes of interdigital foot
infections.1 Traditionally, erythrasma has been considered to
more frequently affect individuals
living in warmer climates, though
it can occur at any lattitude.
Along with candidiasis, intertrigo,
candida folliculitis, furunculosis,
tinea cruris, and folliculitis, eryErythrasma. The image above shows involvement of the right axilla at baseline (left) and
thrasma has been reported to
improvement following four weeks of once-daily application of ketoconazole foam (right).
occur with increased incidence
2
among obese individuals and
those with diabetes.1 However, the infection may
tial diagnosis of erythrasma includes cutaneous
also be common among athletes, particularly
fungal infections, including pityriasis rotunda,
when affecting the toe webs.3
tinea corporis/cruris,4 tinea pedis, and pityriasis
Among other cutaneous diseases, the differenversicolor.5 Importantly, erythrasma may coexist
Erythrasma
with cutaneous dermatophyte infections.6 Proper
diagnosis of erythrasma and any concomitant skin
infection(s) is essential to allow initiation of
appropriate therapy targeted at all causative
organisms. Topical anti-infective therapy, including broad-spectrum ketoconazole, is typically sufficient to manage the condition, although systemic
antibiotics have traditionally been advocated for
erythrasma and may be indicated for severe or
refractive cases.
Presentation and Prevalence
Erythrasma is a bacterially mediated scaly skin
eruption typically localized to warm, moist skin
folds. The rash tends to be deep red to brown in
color and is not typically associated with significant pruritus. Erythrasma was once improperly
considered a fungal infection, though research
over the past 50 years has confirmed the role of
C. minutissimum in its pathogenesis. 7,8 These
gram-positive bacteria are typically part of the
normal resident flora of human skin. In 1965,
Montes, et al. evaluated biopsied skin from
patients with erythrasma absent any concomitant
fungal etiology.8 They found C. minutissimum dispersed over the skin surface, between and penetrating superficial cornified cells, and within keratinized cells. Their investigation showed that the
stratum corneum of affected patients was hyperkeratotic and identified likely keratolytic processes
associated with the presence of intracellular bacteria.
Erythrasma generally is diagnosed through
visualization, but it may be mistaken for candidiasis, intertrigo, psoriasis, seborrheic dermatitis,
contact dermatitis, or dermatophytosis.1
Luminecescence with a Woods Lamp reveals a
coral pink fluorescence that confirms the presence
of C. minutissimum and supports the diagnosis.
The diagnosis may be missed if the patient has
bathed within the preceeding 24 hours; bathing
may wash away coproporphyrin III, the pigment
produced by C. minutissimum that causes fluorescence. Fungal culture may be used to rule out
concomitant fungal infection.
48 | Practical Dermatology | September 2009
Erythrasma has been found to have a higher
prevalence in diabetics and the obese.1,2
Treatment Options
Systemic antibiotics offer proven efficacy and
have been used for the management of erythrasma; Erythromycin 250mg four times daily for 14
days has been recommended as the systemic
antibiotic treatment of choice.1 Yet systemic
antibiotics are currently described as a third-line
treatment option for erythrasma, and they are
known to confer limited efficacy for affected toewebs.9,10 As dermatologists and other physicians
have become increasingly aware of antibiotic
resistance and its potential long-term impact on
patient care, there have been efforts to reduce the
use of systemic antibiotics. Furthermore, systemic
medications in general tend to present a greater
risk of side effects and/or drug interactions compared to topical agents. Given that erythrasma is a
generally benign condition, the use of systemic
antibiotics as first-line therapy becomes questionable.
Topical antimicrobial therapies are second-line
choices for erythrasma management.9 Topical
preparations containing antibiotics have not been
shown in the published literatureto be very effective for treating erythrasma. However, antimicrobial fusidic acid ointment 2% has demonstrated
efficacy, as has Whitfields ointment (salicylic acid
and benzoic acid).1,9 Whitfields ointment reportedly has similar efficacy to systemic erythromycin
for erythrasma affecting the axillae and groin and
is superior to the oral agent in the interdigital
areas.1
Despite the potential efficacy of the topical
antimicrobial ointment preparations, they are not
ideal in the clinical setting. They may lack cosmetic elegance and thus be associated with low
compliance. Most patients are unwilling to apply
thick, greasy preparations to intertriginous areas
or toe webs.
Although a role for dermatophytes, yeasts, and
molds in the pathogenesis of pure erythrasma has
been disproven, topical antifungal formulations
have been used with success to
manage the condition and are
described as first-line treatment
options.9 Topical miconazole,11,12
clotrimazole,12 and econazole9
have all been shown effective
for erythrasma. In one trial
involving 61 patients with fungal
infection or erythrasma, subjects
were randomized to use topical
tioconazole base 1% w/w or
econazole nitrate 1% creams for
a mean treatment period of 40
and 38 days respectively.13 All
but two patients in each arm
achieved clinical and mycologic
cure and described treatment as The patient above is shown at baseline (left) and following 10 days of once-daily application
generally acceptable, though
of ketoconazole foam.
mild intermittent pruritus was
with hydrocortisone acetate 1%, no therapy, ointreported with econazole. Again, creams may not
ment vehicle alone, or hydrocortisone acetate
be ideal for use in skin folds and interdigital
alone. For the killed bacteria (i.e., no infection)
spaces.
groups, topical ketoconazole had anti-inflammatoIn my clinical experience, a new ketoconazole
ry activity comparable to that of hydrocortisone
foam 2% formulation (Extina, Stiefel), has been a
acetate. For infected animals, ketoconazole was
welcome new treatment option for erythrasma.
superior to hydrocortisone. Combination therapy
The foam vehicle (VersaFoam HF) is a
was beneficial in both groups.
hydroethanolic formulation that is neither hydratAn added benefit of topical ketoconazole for the
ing nor drying. It is designed to rapidly dissolve at
management of erythrasma is that the broad-specskin temperature leaving little to no residue. As
trum antifungal will address any concomitant funsuch, it is ideal for application to skin folds. The
gal component of the presentation, eliminating the
foam can be easily applied to various body sites
large and small and is readily applied to hair-bear- need for culture and optimizing the likelihood of
complete cutaneous clearance.
ing skin, making it suitable for use in the axilla
and hair-bearing chest and abdomen. It is also
Prevention
easily and comfortably applied to the toe webs.
To reduce the likelihood of recurrence of erythrasKetoconazole has long been recognized as havma, patients must make efforts to reduce bacterial
ing a broad spectrum of activity.14 It confers docucolonization and minimize moisture in the skin
mented anti-inflammatory and antibacterial
folds. The use of antibacterial washes has been
effects.15 Researchers demonstrated the agents
anti-inflammatory and antibacterial properties in a recommended, though no published data are
guinea pig model.12 First, either living or killed
available. Advise patients to thoroughly dry the
Staphylococcus aureus was applied to the backs of
skin after bathing.
the animals, which then received either ketoconaAlthough standard laundering practices are
zole 0.5% ointment alone or with hydrocortisone
expected to prevent bacterial colonization of clothacetate 1%, ketoconazole 2% ointment alone or
ing, bacteria may, like dermatophytes, colonize
September 2009 | Practical Dermatology | 49
Photos courtesy of Joseph Bikowski, MD
Erythrasma
Erythrasma
Cutaneous Infections Associated with Obesity
Common cutaneous
infections:
Candidiasis
Intertigo
Candida folliculitis
Furunculosis
Erythrasma
Tinea cruris
Folliculitis
Less common infections:
Cellulitis
Necrotizing fasciitis
Gas gangrene
Scheinfeld NS
Clin Dermatol. 22(4):303-9
out greasy residue, supporting patient compliance
with therapy.
Dr. Bikowski has served on the advisory board,
served as a consultant, received honoraria, and/or
served on the speakers bureau for Allergan, Barrier,
CollaGenex, Coria, Galderma, Intendis, Medicis,
OrthoNeutrogena, PharmaDerm, Quinnova, Ranbaxy,
Sanofi-Aventis, SkinMedica, Stiefel, UCB, and
Warner Chilcott.
1. Holdiness MR. Management of cutaneous erythrasma. Drugs.
2002;62(8):1131-41.
2. Scheinfeld NS. Obesity and dermatology. Clin Dermatol. 2004 JulAug;22(4):303-9.
moist footwear. Patients with erythrasma involving the toe webs may need to disinfect or replace
shoes to eliminate exposure to bacteria. Once
clear, patients should be advised to allow their
shoes to thoroughly dry between wearing, perhaps
alternating footwear every-other-day, if needed, to
allow drying.
Patients with a history of recalcitrant or recurrent erythrasma may be directed to prophylactically apply topical ketaconozole foam to previously affected areas once daily.
3
Multi-Targeted Intervention
The ability to manage a generally benign, bacterially-mediated cutaneous eruption with a topical
formulation that poses minimal risk of side effects
and no risk of bacterial resistance is ideal. As
with all dermatologic presentations, therapeutic
outcomes are optimized when patients are compliant with therapy. In light of these considerations,
ketoconazole foam 2% represents a new treatment
option for the management of erythrasma that
may increase compliance.
Topical ketoconazole provides both anti-inflammatory and antibacterial properties that directly
target the underlying bacterial cause of erythrasma. It also provides broad-spectrum antifungal
effects that eradicate the fungal component that
frequently co-exists with erythrasma. The foam
vehicle is particularly suited for application to
skin folds, toe webs, and hair-bearing skin with-
50 | Practical Dermatology | September 2009
3. Conklin RJ. Common cutaneous disorders in athletes. Sports Med. 1990
Feb;9(2):100-19.
4. Gupta S. Pityriasis rotunda mimicking tinea cruris/corporis and erythrasma in
an Indian patient. J Dermatol. 2001 Jan;28(1):50-3.
5. Aste N, Pau M, Aste N. Pityriasis versicolor on the groin mimicking erythrasma. Mycoses. 2004 Jun;47(5-6):249-51.
6. Karakatsanis G, Vakirlis E, Kastoridou C, Devliotou-Panagiotidou D.
Coexistence of pityriasis versicolor and erythrasma. Mycoses. 2004
Aug;47(7):343-5.
7. Marks R, Ramnarain ND, Bhogal B, Moore NT. The erythrasma microorganism in
situ: studies using the skin surface biopsy technique. J Clin Pathol. 1972
Sep;25(9):799-803.
8. Montes LF, McBride ME, Johnson WP, Owens DW, Knox JM. Ultrastructural study
of the host-bacterium relationship in erythrasma. J Bacteriol. 1965
Nov;90(5):1489-91.
9. Barkham MC, Smith AC. Erythrasma in Treatment of Skin Disease:
Comprehensive Therapeutic Strategies, Lebwohl MG, et al., eds. 2005 Mosby,
Incorporated
10. Seville RH, Somerville DA. The treatment of erythrasma in a hospital for the
mentally subnormal.Br J Dermatol. 1970 May;82(5):502-6
11. Pitcher DG, Noble WC, Seville RH. Treatment of erythrasma with miconazole.
Clin Exp Dermatol. 1979 Dec;4(4):453-6.
12. Clayton YM, Knight AG. A clinical double-blind trial of topical miconazole and
clotrimazole against superficial fungal infections and erythrasma. Clin Exp
Dermatol. 1976 Sep;1(3):225-32.
13. Grigoriu D, Grigoriu A. Double-blind comparison of the efficacy, toleration
and safety of tioconazole base 1% and econazole nitrate 1% creams in the treatment of patients with fungal infections of the skin or erythrasma. Dermatologica.
1983;166 Suppl 1:8-13.
14. Van Tyle JH. Ketoconazole. Mechanism of action, spectrum of activity, pharmacokinetics, drug interactions, adverse reactions and therapeutic use.
Pharmacotherapy. 1984 Nov-Dec;4(6):343-73.
15. Van Cutsem J, Van Gerven F, Cauwenbergh G, Odds F, Janssen PA. The antiinflammatory effects of ketoconazole. A comparative study with hydrocortisone
acetate in a model using living and killed Staphylococcus aureus on the skin of
guinea-pigs. J Am Acad Dermatol. 1991 Aug;25(2 Pt 1):257-61.
Das könnte Ihnen auch gefallen
- Adolescent Acne Vulgaris Consultant For Pediatricians Feb. 2015 PDFDokument3 SeitenAdolescent Acne Vulgaris Consultant For Pediatricians Feb. 2015 PDFDesi RatnaningtyasNoch keine Bewertungen
- Jurnal Stress OksidatifDokument8 SeitenJurnal Stress OksidatifDesi RatnaningtyasNoch keine Bewertungen
- Patch Test DrugDokument9 SeitenPatch Test DrugDesi RatnaningtyasNoch keine Bewertungen
- Antioxidants 06 00095Dokument11 SeitenAntioxidants 06 00095Desi RatnaningtyasNoch keine Bewertungen
- UV Radiation and Skin PDFDokument27 SeitenUV Radiation and Skin PDFDesi RatnaningtyasNoch keine Bewertungen
- Management of Cutaneous ErythrasmaDokument11 SeitenManagement of Cutaneous ErythrasmaDesi RatnaningtyasNoch keine Bewertungen
- Diagnosis of Common, Benign Neonatal Dermatoses: Daniel Wallach, MDDokument5 SeitenDiagnosis of Common, Benign Neonatal Dermatoses: Daniel Wallach, MDDesi RatnaningtyasNoch keine Bewertungen
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5795)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Surigao Del Sur State University: Review of Related LiteratureDokument9 SeitenSurigao Del Sur State University: Review of Related LiteraturePrincess Marcelhyn VillegasNoch keine Bewertungen
- Awareness On HepatitisDokument52 SeitenAwareness On HepatitisMizanur RahmanNoch keine Bewertungen
- ENG 114 Medical Terminology Module 23-24Dokument47 SeitenENG 114 Medical Terminology Module 23-24zainablovebhNoch keine Bewertungen
- Pharmacologic ClassDokument4 SeitenPharmacologic ClassBianca Nicole Gacad FernandezNoch keine Bewertungen
- MOH DHA HAAD Dental Study Material Part 2Dokument33 SeitenMOH DHA HAAD Dental Study Material Part 2Junaid Ramzan89% (37)
- Gujarat Technological University: W.E.F. AY 2017-18Dokument3 SeitenGujarat Technological University: W.E.F. AY 2017-18raj royelNoch keine Bewertungen
- IMNCI Management of Childhood Illness Chart Booklet WHO 2018Dokument54 SeitenIMNCI Management of Childhood Illness Chart Booklet WHO 2018IgweNoch keine Bewertungen
- Jurnal HPLC KromatografiDokument8 SeitenJurnal HPLC KromatografiDevi AtikahNoch keine Bewertungen
- ACTD Rev.1 Part IV Clinical DocumentDokument50 SeitenACTD Rev.1 Part IV Clinical DocumentRaeanne SabadoNoch keine Bewertungen
- Role of DOAC in The Management of COVID-19 Patients: Desak Nyoman Desy LestariDokument32 SeitenRole of DOAC in The Management of COVID-19 Patients: Desak Nyoman Desy Lestaridesy lestariNoch keine Bewertungen
- Screening For Osteoporosis - UpToDateDokument22 SeitenScreening For Osteoporosis - UpToDatesindy suarezNoch keine Bewertungen
- Grand Coaching: Medical Surgical NursingDokument22 SeitenGrand Coaching: Medical Surgical NursingEsarpy (Nana)Noch keine Bewertungen
- Urinary Tract Infection, Complicated (UTI) - Johns Hopkins ABX GuideDokument5 SeitenUrinary Tract Infection, Complicated (UTI) - Johns Hopkins ABX GuideLaoMed plusNoch keine Bewertungen
- Sympathomimetics 2023 MCQDokument12 SeitenSympathomimetics 2023 MCQHossam MohamedNoch keine Bewertungen
- 12 Letter WordsDokument494 Seiten12 Letter Wordstrakds0% (1)
- 121220190CNS StimulantsDokument23 Seiten121220190CNS StimulantsHemantNoch keine Bewertungen
- Skelton Et Al-2015-Cochrane Database of Systematic ReviewsDokument30 SeitenSkelton Et Al-2015-Cochrane Database of Systematic ReviewsDamian MarreroNoch keine Bewertungen
- Bhanga 3Dokument35 SeitenBhanga 3Shanmugam PiramanayagamNoch keine Bewertungen
- Brochure TSMU - GeorgiaDokument9 SeitenBrochure TSMU - GeorgiashahulNoch keine Bewertungen
- BLUEPRINT - Basic Principles of Toxicology Elective TYDokument2 SeitenBLUEPRINT - Basic Principles of Toxicology Elective TYDAMBALENoch keine Bewertungen
- HAADDokument52 SeitenHAADElsayed AbdallahNoch keine Bewertungen
- CefuroximeDokument2 SeitenCefuroximeAngel CatalanNoch keine Bewertungen
- Drug Abuse Among The Students: June 2015Dokument8 SeitenDrug Abuse Among The Students: June 2015MohdAlifAbdullahNoch keine Bewertungen
- CHAPTER8Dokument21 SeitenCHAPTER8SankaraSatyadevNoch keine Bewertungen
- Digoxin (Lanoxin) : Routes of Administration Methods For Iv Administration and DosageDokument2 SeitenDigoxin (Lanoxin) : Routes of Administration Methods For Iv Administration and Dosageiamlx2Noch keine Bewertungen
- Review Article: Thymoma in Myasthenia Gravis: From Diagnosis To TreatmentDokument6 SeitenReview Article: Thymoma in Myasthenia Gravis: From Diagnosis To TreatmentHeru SigitNoch keine Bewertungen
- Azole Antifungals HandoutDokument8 SeitenAzole Antifungals Handoutapi-648714317Noch keine Bewertungen
- M6 Pharmaceutical LabelsDokument23 SeitenM6 Pharmaceutical Labelscbun22222Noch keine Bewertungen
- Coverage Midterm Examination 2021 Drug and Vice ControlDokument4 SeitenCoverage Midterm Examination 2021 Drug and Vice ControlTaga Phase 7Noch keine Bewertungen
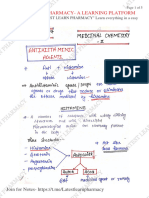
- L 1 Unit 1 Medicinal Chemistry LL LATEST LEARN PHARMACYDokument5 SeitenL 1 Unit 1 Medicinal Chemistry LL LATEST LEARN PHARMACYYASH DESHMUKH 66Noch keine Bewertungen