Beruflich Dokumente
Kultur Dokumente
tmp40DA TMP
Hochgeladen von
FrontiersOriginalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
tmp40DA TMP
Hochgeladen von
FrontiersCopyright:
Verfügbare Formate
Case Report
Modified Desensitization Protocols for a Pediatric
Patient with Anaphylactic Reaction to Deferoxamine
Pacharapan Surapolchai MD*, Orapan Poachanukoon MD*,
Wallee Satayasai MD*, Pakatip Silapamongkonkul MD*
* Department of Pediatrics, Faculty of Medicine, Thammasat University, Pathumthani, Thailand
Thalassemia major is an inherited form of chronic hemolytic anemia that results in iron overload due to regular
blood transfusions. Deferoxamine is used as chelating agent for treatment of patients with chronic iron overload worldwide.
Anaphylactic reaction to deferoxamine is rare, and the mechanism of deferoxamine-induced anaphylaxis is not well understood.
Only a few pediatric cases of successful desensitization for deferoxamine hypersensitivity have been described, and a different
protocol has been used in each report. We report a case of anaphylaxis to deferoxamine in a thirteen-years-old Thai boy with
Hemoglobin E/-thalassemia disease who underwent successful desensitization. He had been receiving blood transfusions
since the age of ten months. At age eleven, the patient began treatment with deferoxamine. Treatment was interrupted after the
occurrence of anaphylaxis, with urticaria, wheezing and gastrointestinal symptoms. A skin prick test was positive, indicating
a type 1 hypersensitivity reaction. Deferoxamine desensitization was attempted with various different protocols. Finally, the
patient could tolerate deferoxamine therapy at the dose previously administered. We proposed this modified subcutaneous
desensitization protocol for pediatric cases that develop allergic reactions to deferoxamine.
Keywords: Deferoxamine, Anaphylaxis, Desensitization, Subcutaneous
J Med Assoc Thai 2014; 97 (Suppl. 8): S217-S222
Full text. e-Journal: http://www.jmatonline.com
Thalassemia is the most common human
single gene disorder worldwide. Hemoglobin E/betathalassemia (Hb E/-thalassemia) is a very common
form of beta-thalassemia that exhibits a heterogeneous
clinical presentation and variable clinical course. The
highest frequencies are observed in India and
throughout Southeast Asia, particularly in Thailand,
Laos and Cambodia(1,2). Hb E/-thalassemia results from
co-inheritance of a beta-thalassemia allele from one
parent and the structural variant Hemoglobin E from
the other. Severe forms are characterized by very low
Hemoglobin (Hb) levels, and affected patients are
treated as thalassemia major patients with regular blood
transfusion and iron chelation. Iron overload may lead
to organ toxicity and even fatal complications if iron
chelating therapy cannot be achieved.
For clinical use, iron chelators are designed
to either promote clearance of excess iron by excretion
or maintain safe iron levels in situations that pose a
risk for developing toxic levels of iron. Three chelators
are approved for therapeutic use: deferoxamine,
Correspondence to:
Surapolchai P, Department of Pediatrics, Faculty of Medicine,
Thammasat University, Pathumthani 12120, Thailand.
Phone: 0-2926-9514, Fax: 0-2926-9513
E-mail: doctorning@hotmail.com
J Med Assoc Thai Vol. 97 Suppl. 8 2014
deferasirox, and deferiprone, and these agents are
sometimes are used in combination(3,4). Deferoxamine
(DFO), also known as desferrioxamine or desferal, is
the most important drug and commonly used in the
treatment of thalassemia major and other hematological
diseases following multiple blood transfusions. It is
administered by intravenous injection or
subcutaneously with iron complexes being cleared
mainly by biliary and urinary routes. Allergic reactions
to DFO are rare and difficult to manage. The mechanism
of hypersensitivity is various and need to be explored.
The purpose of this article is to report a pediatric case
of anaphylaxis to DFO in which the patient underwent
successful desensitization.
Case Report
A 13-years-old Thai boy with Hb E/thalassemia had been receiving frequent blood
transfusions from the age of 10 months. He had a
splenectomy at the age of 5 because of hypersplenism
and began to receive a transfusion every 1-2 months
after that. The iron chelation therapy was started at the
age of 11. He was receiving intravenous DFO infusion
at a standard dose of 30 mg/kg/day (750 mg of DFO in
50 mL of saline solution) for 3 consecutive days per
week at the Thammasat University Hospital. Because
S217
of a further increase in serum ferritin level (>2,000 ng/
mL), he also received oral daily deferiprone as a
combined therapy. Fourteen months after DFO
administration, he had an anaphylactic reaction
described as generalized urticaria, itching, wheezing,
dyspnea, tachycardia and vomiting 10 minutes
after beginning DFO infusion. The infusion was
stopped immediately, and the patient was treated
with intramuscular epinephrine, antihistamines,
corticosteroids and salbutamol nebulization.
Two weeks after the first anaphylactic
reaction, the patient was admitted for investigation and
desensitization. The total serum immunoglobulin E
(IgE) was within a normal range. The skin prick test
(SPT) with diluted DFO solution (15 mg/mL) was
positive (size 25x6 mm) in this patient while the tests
were negative in all 5 thalassemia patients of the control
group. For further testing with the patient, SPT with
common food allergens was negative. The FIRST
desensitization protocol was modified by the method
of Miller et al(5). The desensitization was started with a
solution of 1/100,000 of the anticipated final intravenous
infusion concentrations (0.0075 mg in 50 mL of saline
solution) and continued with the following schedule:
0.075, 0.75, 7.5, 75, 750 mg in 50 mL at 30-minute intervals
(Table 1). At a dose of 0.75 mg (solution of 1/1,000), he
had a similar anaphylaxis episode, and the trial was
discontinued. The complete blood count during this
episode showed eosinophilia (absolute eosinophil
count of 3,066/cu.mm.). One week later, the SECOND
desensitization was attempted by increasing the
concentrations of DFO as in the first but increasing the
interval between doses from 30-minute to 24-hour
interval and changing the route from intravenous to
continuous subcutaneous infusion (Table 2). This trial
was successful without any reactions. The patient was
discharged and then admitted one week later for 3 days
of daily 24-hour subcutaneous infusion of 750 mg of
DFO. However, a similar anaphylactic reaction occurred
again on the first day of desensitization. The infusion
Table 1. The FIRST desensitization protocol via intravenous infusion at 30-minute intervals for each bottle without
premedication
Bottles
Time (hours)
Dose (mg) of DFO in 50 mL
of saline solution
Ratio of DFO in solution to the
anticipated final infusion dose (750 mg)
1
2
3
4
5
6
0
0.5
1.0
1.5
2.0
2.5
0.0075
0.075
0.75
7.5
75
750
1:100,000
1:10,000
1:1,000 Anaphylaxis
1:100
1:10
1:1
DFO = deferoxamine
Modified by the method of Miller et al(5)
Table 2. The SECOND desensitization protocol via continuous subcutaneous infusion* at 24-hour intervals for each bottle
without premedication
Bottles
Time (hours)
Dose (mg) of DFO in 50 mL
of saline solution
Ratio of DFO in solution to the anticipated
final infusion dose (750 mg)
1
2
3
4
5
6
0
24
48
72
96
120
0.0075
0.075
0.75
7.5
75
750
1:100,000
1:10,000
1:1,000
1:100
1:10
1:1
DFO = deferoxamine
* The continuous subcutaneous infusion of DFO was administered via slow subcutaneous infusion uniformly over 24 hours
using a portable infusion pump.
S218
J Med Assoc Thai Vol. 97 Suppl. 8 2014
was suspended, and the patient received treatment for
anaphylaxis.
Two months later, he was admitted for the
THIRD desensitization (Table 3). Because of the high
risk of anaphylaxis, pretreatment was started with
intravenous antihistamines and corticosteroids
(chlorpheniramine 0.1 mg/kg and hydrocortisone 5 mg/
kg), single dose prior to desensitization. The patient
was hospitalized for desensitization with eight
continuous cycles of DFO. Finally, they were completed
with no untoward reactions. However, anaphylaxis
recurred one week later when the patient received 750
mg DFO infusion over 24 hours. Three weeks later, 10
weekends of the FOURTH desensitization were
attempted continuously by increasing the concentrations of subcutaneous DFO infusion with
premedication. The infusion interval periods were
tapered weekly from 6-hour to 10-minute interval (6, 5,
4, 3, 2, 1 hours and 45, 30, 20, 10 minutes, respectively)
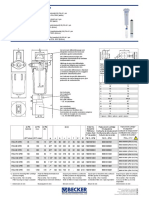
(Table 4). The THIRD and FORTH desensitization are
summarized in Fig. 1.
This trial was completed without further
allergic reaction, even after discontinuing the
premedication. During 2 years after the fourth
desensitization, the patient regularly received
subcutaneous infusion of 750 mg DFO in 10 mL of
Table 3. The THIRD desensitization protocol via continuous subcutaneous infusion* at 24-hour intervals for each bottle
with premedication (antihistamines and corticosteroids) for total eight continuous cycles**
Bottles
Time (hours)
Dose (mg) of DFO in 50 mL
of saline solution
Ratio of DFO in solution to the anticipated
final infusion dose (750 mg)
1
2
3
4
5
6
0
24
48
72
96
120
0.0075
0.075
0.75
7.5
75
750
1:100,000
1:10,000
1:1,000
1:100
1:10
1:1
DFO = deferoxamine
* The continuous subcutaneous infusion of DFO was administered via slow subcutaneous infusion uniformly over 24 hours
using a portable infusion pump.
** For the eight continuous cycles, the first three cycles (Cycle 1-3) were started with a 24-hour interval at DFO infusion
dose of 1/100,000 (0.0075 mg, Bottle No. 1) and continued with an increasing concentration until the final dose (750 mg).
Then the last five cycles (Cycle 4-8) were attempted by beginning at Bottle No. 2, 3, 4, 5, 6 respectively and continued with
an increasing concentration over 24 hours each bottle until the final dose. The Cycle 1 to Cycle 8 is continuing administration
without cessation.
Table 4. The FORTH desensitization protocol via subcutaneous infusion at different intervals tapering for each cycle with
premedication (antihistamines and corticosteroids) for total ten weekend cycles
Bottles
Dilution (mg) of DFO in 10 ml of saline solution
Ratio of DFO in solution to the anticipated final
infusion concentrations (750 mg)
1
2
3
4
5
6
0.075 mg subcutaneous infusion in 6 hours*
0.75 mg subcutaneous infusion in 6 hours*
7.5 mg subcutaneous infusion in 6 hours*
75 mg subcutaneous infusion in 6 hours*
750 mg subcutaneous infusion in 6 hours*
750 mg subcutaneous infusion in 8 hours
1:10,000
1:1,000
1:100
1:10
1:1
1:1
DFO = deferoxamine
* For the ten weekend cycles, the desensitization started with decreased the subcutaneous infusion interval periods for each
bottle of DFO from 6-hour to 5-, 4-, 3-, 2-, 1-hour and 45-, 30-, 20-, 10-minute interval, respectively. At the end of each
desensitization phase, an 8-hour subcutaneous infusion of 750 mg solution was given.
J Med Assoc Thai Vol. 97 Suppl. 8 2014
S219
Fig. 1A
The timeline of THIRD and FORTH Desensitization of deferoxamine. A) The THIRD Desensitization timeline (Please see the Table 3 for additional
information of protocol).
Fig. 1B The FORTH desensitization timeline (Please see
the Table 4 for additional information of protocol).
saline solution (30 mg/kg/day, over 8 hours/day for
three consecutive days per week) at the hospital without
any allergic reaction. Thereafter, the subcutaneous
infusion was given to the patient for self-therapy at
home. He has continued home DFO subcutaneous
infusions for the last 1.5 years. Finally, his chelation
therapy was switched to oral deferiprone as
monotherapy, when the serum ferritin was less than
1,000 ng/mL. A repeat SPT with DFO (using a 1/10
dilution of DFO 15 mg/mL solution) 6 months after
cessation of DFO was still positive (size 15x15 mm).
S220
Discussion
There have been rare case reports of
desensitization for DFO anaphylactic reactions
from the United States of America, France, Italy,
Turkey(5,7-10). This is the first case report of a successful
subcutaneous desensitization in a pediatric patient who
had experienced an anaphylactic reaction to DFO. For
immediate-type drug reactions, allergy skin testing may
be useful, although there is a lack of standardized testing
reagents. Skin testing by prick or intradermal methods
is practicable, but it is important to establish a nonirritating drug dose for skin testing. In our case, the
SPT with diluted DFO was positive, whereas the same
test dose was negative in 5 other thalassemia patients.
This suggests that the patient had an IgE-dependent
hypersensitivity reaction to DFO. However, due to the
lack of standardized reagents, the positive and negative
predictive values of skin testing for DFO remain
unknown. Furthermore, our results do not rule out the
possibility that DFO allergy is related to direct mast
cell activation as previously described(6). Such a nonIgE mediated allergic reaction has been proposed to
explain DFO-induced anaphylaxis in adult and pediatric
patients who have negative skin prick tests and absent
specific serum IgE to DFO(8-10). Finally, it is possible
that both IgE-mediated and non-IgE mediated direct
mast cell activation coexist in some patients. A limitation
of the present study is that the authors did not test the
patient with validated in vitro immunological testing
for serum IgE to DFO; however, this test is not widely
available.
Desensitization using gradual titration of
drug administered parenterally is the gold standard for
management of many types of drug allergies. However,
this procedure should only be performed by
experienced and trained physicians in an appropriate
setting. The time required for successful desensitization
varies with the type of medication and is patientspecific. Intravenous DFO as previously described(5,8,9)
can provide an avenue for early challenging during
desensitization. Why intravenous therapy as opposed
to subcutaneous therapy is generally well tolerated is
not fully understood. Suggested mechanisms range
from the simple mechanics of putting small volumes of
DFO intravenously with subsequent rapid distribution
(particularly relevant for localized reactions) to
differences in the immune system response depending
on the route of DFO administration, e.g. dermal mast
cell activation(11). Eventually, complications can still
occur, with anaphylaxis documented in our patient
during intravenous desensitization. The successful use
J Med Assoc Thai Vol. 97 Suppl. 8 2014
of a subcutaneous desensitization protocol in this
patient with DFO hypersensitivity represents a novel
finding. For premedication, systemic treatment with
antihistamines and/or corticosteroids were used as
described in previous reports(5,8,9). Antihistamines and
corticosteroids may have provided some benefit during
our desensitization therapy, but they were insufficient
alone to account for the success of the protocol.
Conclusion
This report illustrates the utility of using a
subcutaneous desensitization approach with
premedication for treatment of immediate-type
hypersensitivity to DFO. The modified desensitization
protocol proposed in the present study was effective
in preventing allergic reactions and in reducing iron
overload. The authoes propose this as an alternative
desensitization protocol for pediatric cases that are
anaphylaxis to DFO and require long-term iron chelation
therapy.
What is already known on this topic?
1. Anaphylactic reaction to deferoxamine is a
relatively rare condition in childhood.
2. The standard desensitization protocol for
deferoxamine hypersensitivity is not well established.
What this study adds?
1. Desensitization to deferoxamine in pediatric
patients is safe using our protocol. We have had a
successful delivery of subcutaneous deferoxamine in
our patients with thalassemia major.
2. Skin testing data is not routinely available
due to the lack of commercially available testing
reagents. Without standardized reagents, the positive
and negative predictive values of skin testing for
deferoxamine remain unknown.
3. Further establishment of the treatment
protocols by a multicenter study for desensitization of
life-sustaining drugs and effectiveness of this treatment
are required.
Acknowledgement
The authors are indebted to all pediatric
residents and clinical staff members at Thammasat
University Hospital who cared for this patient. The
patient and family members who took part in the present
J Med Assoc Thai Vol. 97 Suppl. 8 2014
study are highly appreciated for their contribution.
Potential conflicts of interest
None.
References
1. Modell B, Darlison M. Global epidemiology of
haemoglobin disorders and derived service
indicators. Bull World Health Organ 2008; 86: 4807.
2. Weatherall DJ, Clegg JB. Inherited haemoglobin
disorders: an increasing global health problem. Bull
World Health Organ 2001; 79: 704-12.
3. Porter JB. Optimizing iron chelation strategies in
beta-thalassaemia major. Blood Rev 2009; 23 (Suppl
1): S3-7.
4. Brittenham GM. Iron-chelating therapy for
transfusional iron overload. N Engl J Med 2011;
364: 146-56.
5. Miller KB, Rosenwasser LJ, Bessette JA, Beer DJ,
Rocklin RE. Rapid desensitisation for
desferrioxamine anaphylactic reaction. Lancet
1981; 1: 1059.
6. Shalit M, Tedeschi A, Miadonna A, Levi-Schaffer
F. Desferal (desferrioxamine)a novel activator
of connective tissue-type mast cells. J Allergy Clin
Immunol 1991; 88: 854-60.
7. Athanasion A, Shepp MA, Necheles TF.
Anaphylactic reaction to desferrioxamine. Lancet
1977; 2: 616.
8. Bousquet J, Navarro M, Robert G, Aye P, Michel
FB. Rapid desensitisation for desferrioxamine
anaphylactoid reaction. Lancet 1983; 2: 859-60.
9. La Rosa M, Romeo MA, Di Gregorio F, Russo G.
Desensitization treatment for anaphylactoid
reactions to desferrioxamine in a pediatric patient
with thalassemia. J Allergy Clin Immunol 1996; 97:
127-8.
10. Gulen F, Demir E, Tanac R, Aydinok Y, Gulen H,
Yenigun A, et al. Successful desensitization of a
case with desferrioxamine hypersensitivity.
Minerva Pediatr 2006; 58: 571-4.
11. Lombardo T, Ferro G, Frontini V, Percolla S. Highdose intravenous desferrioxamine (DFO) delivery
in four thalassemic patients allergic to subcutaneous DFO administration. Am J Hematol 1996;
51: 90-2.
S221
S222
J Med Assoc Thai Vol. 97 Suppl. 8 2014
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- tmp3CAB TMPDokument16 Seitentmp3CAB TMPFrontiersNoch keine Bewertungen
- tmpCE8C TMPDokument19 SeitentmpCE8C TMPFrontiersNoch keine Bewertungen
- tmpFFE0 TMPDokument6 SeitentmpFFE0 TMPFrontiersNoch keine Bewertungen
- tmpE7E9 TMPDokument14 SeitentmpE7E9 TMPFrontiersNoch keine Bewertungen
- tmp6F0E TMPDokument12 Seitentmp6F0E TMPFrontiersNoch keine Bewertungen
- tmpE3C0 TMPDokument17 SeitentmpE3C0 TMPFrontiersNoch keine Bewertungen
- tmpF178 TMPDokument15 SeitentmpF178 TMPFrontiersNoch keine Bewertungen
- tmp80F6 TMPDokument24 Seitentmp80F6 TMPFrontiersNoch keine Bewertungen
- tmpEFCC TMPDokument6 SeitentmpEFCC TMPFrontiersNoch keine Bewertungen
- Tmp1a96 TMPDokument80 SeitenTmp1a96 TMPFrontiersNoch keine Bewertungen
- tmpF3B5 TMPDokument15 SeitentmpF3B5 TMPFrontiersNoch keine Bewertungen
- Tmpa077 TMPDokument15 SeitenTmpa077 TMPFrontiersNoch keine Bewertungen
- tmp72FE TMPDokument8 Seitentmp72FE TMPFrontiersNoch keine Bewertungen
- tmpF407 TMPDokument17 SeitentmpF407 TMPFrontiersNoch keine Bewertungen
- tmpC0A TMPDokument9 SeitentmpC0A TMPFrontiersNoch keine Bewertungen
- tmp60EF TMPDokument20 Seitentmp60EF TMPFrontiersNoch keine Bewertungen
- tmp8B94 TMPDokument9 Seitentmp8B94 TMPFrontiersNoch keine Bewertungen
- tmp6382 TMPDokument8 Seitentmp6382 TMPFrontiersNoch keine Bewertungen
- tmp998 TMPDokument9 Seitentmp998 TMPFrontiersNoch keine Bewertungen
- tmp4B57 TMPDokument9 Seitentmp4B57 TMPFrontiersNoch keine Bewertungen
- tmp9D75 TMPDokument9 Seitentmp9D75 TMPFrontiersNoch keine Bewertungen
- tmp37B8 TMPDokument9 Seitentmp37B8 TMPFrontiersNoch keine Bewertungen
- tmpC30A TMPDokument10 SeitentmpC30A TMPFrontiersNoch keine Bewertungen
- tmpD1FE TMPDokument6 SeitentmpD1FE TMPFrontiersNoch keine Bewertungen
- tmpB1BE TMPDokument9 SeitentmpB1BE TMPFrontiersNoch keine Bewertungen
- tmp3656 TMPDokument14 Seitentmp3656 TMPFrontiersNoch keine Bewertungen
- tmpA0D TMPDokument9 SeitentmpA0D TMPFrontiersNoch keine Bewertungen
- Tmp75a7 TMPDokument8 SeitenTmp75a7 TMPFrontiersNoch keine Bewertungen
- tmp27C1 TMPDokument5 Seitentmp27C1 TMPFrontiersNoch keine Bewertungen
- tmp2F3F TMPDokument10 Seitentmp2F3F TMPFrontiersNoch keine Bewertungen
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- VNC Function Operation InstructionDokument11 SeitenVNC Function Operation InstructionArnaldo OliveiraNoch keine Bewertungen
- VARCDokument52 SeitenVARCCharlie GoyalNoch keine Bewertungen
- AIATS 2021 (OYMCF) Test 01 Offline - Code A - SolutionsDokument34 SeitenAIATS 2021 (OYMCF) Test 01 Offline - Code A - Solutionsbhavyakavya mehta100% (1)
- ThesisDokument250 SeitenThesislax mediaNoch keine Bewertungen
- Research Paper On Organ DonationDokument8 SeitenResearch Paper On Organ Donationsheeliya whiteNoch keine Bewertungen
- Denodo Job RoleDokument2 SeitenDenodo Job Role059 Monisha BaskarNoch keine Bewertungen
- 3 Steel Grating Catalogue 2010 - SERIES 1 PDFDokument6 Seiten3 Steel Grating Catalogue 2010 - SERIES 1 PDFPablo MatrakaNoch keine Bewertungen
- Hotel and Restaurant at Blue Nile FallsDokument26 SeitenHotel and Restaurant at Blue Nile Fallsbig johnNoch keine Bewertungen
- Indian Institute OF Management, BangaloreDokument20 SeitenIndian Institute OF Management, BangaloreGagandeep SinghNoch keine Bewertungen
- BSC6900 UMTS V900R011C00SPC700 Parameter ReferenceDokument1.010 SeitenBSC6900 UMTS V900R011C00SPC700 Parameter Referenceronnie_smgNoch keine Bewertungen
- Practical LPM-122Dokument31 SeitenPractical LPM-122anon_251667476Noch keine Bewertungen
- Crash Cart - General Checklist For Medical Supplies On Crash CartsDokument3 SeitenCrash Cart - General Checklist For Medical Supplies On Crash CartsYassen ManiriNoch keine Bewertungen
- Mesopotamia CivilizationDokument56 SeitenMesopotamia CivilizationYashika TharwaniNoch keine Bewertungen
- Rubric - Argumentative EssayDokument2 SeitenRubric - Argumentative EssayBobNoch keine Bewertungen
- Medical filter performance specificationsDokument1 SeiteMedical filter performance specificationsPT.Intidaya Dinamika SejatiNoch keine Bewertungen
- 9 - NCP Computer Science PGDokument19 Seiten9 - NCP Computer Science PGM AmbreenNoch keine Bewertungen
- Health Information System Developmen T (Medical Records)Dokument21 SeitenHealth Information System Developmen T (Medical Records)skidz137217100% (10)
- LLoyd's Register Marine - Global Marine Safety TrendsDokument23 SeitenLLoyd's Register Marine - Global Marine Safety Trendssuvabrata_das01100% (1)
- EG-45-105 Material Information Sheet (Textura) V2Dokument4 SeitenEG-45-105 Material Information Sheet (Textura) V2GPRNoch keine Bewertungen
- Arduino Nano based K1EL Winkeyer compatible CW contest keyerDokument35 SeitenArduino Nano based K1EL Winkeyer compatible CW contest keyerSreejith SreedharanNoch keine Bewertungen
- COT EnglishDokument4 SeitenCOT EnglishTypie ZapNoch keine Bewertungen
- STERNOL Specification ToolDokument15 SeitenSTERNOL Specification ToolMahdyZargarNoch keine Bewertungen
- OLA CAB MARKET ANALYSIS AND TRENDSDokument55 SeitenOLA CAB MARKET ANALYSIS AND TRENDSnitin gadkariNoch keine Bewertungen
- CIGB B164 Erosion InterneDokument163 SeitenCIGB B164 Erosion InterneJonathan ColeNoch keine Bewertungen
- Maximizing modular learning opportunities through innovation and collaborationDokument2 SeitenMaximizing modular learning opportunities through innovation and collaborationNIMFA SEPARANoch keine Bewertungen
- HU675FE ManualDokument44 SeitenHU675FE ManualMar VeroNoch keine Bewertungen
- Future Design of Accessibility in Games - A Design Vocabulary - ScienceDirectDokument16 SeitenFuture Design of Accessibility in Games - A Design Vocabulary - ScienceDirectsulaNoch keine Bewertungen
- Tugas B InggrisDokument6 SeitenTugas B Inggrisiqbal baleNoch keine Bewertungen
- Research Paper Theory of Mind 2Dokument15 SeitenResearch Paper Theory of Mind 2api-529331295Noch keine Bewertungen
- HP 5973 Quick ReferenceDokument28 SeitenHP 5973 Quick ReferenceDavid ruizNoch keine Bewertungen