Beruflich Dokumente
Kultur Dokumente
Resumption of Methimazole After I Therapy of Hyperthyroid Diseases: Effect On Thyroid Function and Volume Evaluated by A Randomized Clinical Trial
Hochgeladen von
MaharRkpOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Resumption of Methimazole After I Therapy of Hyperthyroid Diseases: Effect On Thyroid Function and Volume Evaluated by A Randomized Clinical Trial
Hochgeladen von
MaharRkpCopyright:
Verfügbare Formate
European Journal of Endocrinology (2003) 149 485492
ISSN 0804-4643
CLINICAL STUDY
Resumption of methimazole after 131I therapy of hyperthyroid
diseases: effect on thyroid function and volume evaluated by a
randomized clinical trial
Steen J Bonnema, Finn N Bennedbk, Jeppe Gram, Annegrete Veje1, Jens Marving1 and Laszlo Hegedus
Departments of Endocrinology and 1Nuclear Medicine, Odense University Hospital, DK-5000, Denmark
(Correspondence should be addressed to Steen J Bonnema; Email: steen.bonnema@dadlnet.dk)
Abstract
Objective: Retrospective studies have indicated that anti-thyroid drugs (ATD) might possess a radioprotective effect, leading to a higher rate of recurrence of hyperthyroidism after iodine-131 (131I) therapy.
Design: A randomized clinical trial was performed to clarify whether resumption of methimazole after
131
I influences the final outcome of this treatment.
Methods: We assigned 149 patients with Graves disease or a toxic nodular goitre to groups either to
resume (ATD) or not to resume (2ATD) methimazole 7 days after 131I. Before 131I therapy, all patients
were rendered euthyroid by methimazole, which was discontinued 4 days before the 131I therapy.
Results: During the follow-up period of 12 months, 13 patients developed hypothyroidism, 42 were
euthyroid, and 18 had recurrence of hyperthyroidism in the ATD group; the respective numbers in
the 2ATD group were 16, 42 and 18 (P 0.88). At 3 weeks after 131I therapy, the serum free-thyroxine
index was slightly decreased (by 5.7%; 95% confidence interval (CI) 215.5 to 5.4%) in the ATD
group, in contrast to an increase of 35.9% (95% CI 18.8 to 55.5%) in the 2ATD group (P , 0.001
between groups). In the subgroup that remained euthyroid during follow-up, thyroid volume reduction,
assessed by ultrasonography, was smaller in the ATD group [38.7% (95% CI 33.3to 44.1%)] than in
the 2ATD group [48.6% (95% CI: 41.5 55.6%)] (P , 0.05).
Conclusion: No radioprotective effect could be demonstrated, with regard to final thyroid function, for the
resumpton of methimazole 7 days after 131I therapy. Although resumption of methimazole slightly
reduced the magnitude of shrinkage of the goitre obtained by 131I, the prevention of a temporary thyrotoxicosis in the early period after radiation favours this regimen.
European Journal of Endocrinology 149 485492
Introduction
For the last half century, radioiodine (131I) therapy has
been widely used as the definitive treatment of patients
with hyperthyroidism. Approximately 30% of physicians prefer to render their patients euthyroid by prescribing anti-thyroid drugs (ATDs) before 131I therapy,
whereas 40% use ATDs after the therapy (1). However,
the use of ATDs in conjunction with 131I treatment
may not be without problems. ATDs at physiological
concentrations in cell cultures appear to have scavenger-like properties, inhibiting the production of hydrogen peroxide (2), which may hamper the intended
cytogenetic damage induced by the 131I radiation.
Whether this observation has any clinical relevance is
unknown. Other factors may also be of importance.
Administration of ATDs before 131I therapy does not
seem to influence the iodine kinetics (3), but it is a
matter of speculation whether ATDs diminish the susceptibility to ionizing radiation through a decrease in
thyroid metabolism. Regardless of the mechanism that
q 2003 Society of the European Journal of Endocrinology
might be responsible, several retrospective studies
have consistently suggested that ATDs possess radioprotective properties, thereby attenuating the effect of
131
I, with a subsequently greater rate of recurrence of
hyperthyroidism. This applies to the periods both
before (4 13) and after (14 18) 131I therapy. However, the possible radioprotective role of ATDs remains
controversial (19), and was brought strongly into question recently by the findings of two randomized trials,
in which methimazole pre-treatment was shown not
to affect the outcome of the 131I therapy (20, 21).
The aim of this randomized clinical trial was to elucidate the role of resumption of methimazole after
131
I treatment for hyperthyroidism.
Materials and methods
Patients and design
We enrolled patients with toxic nodular goitre or
recurrent Graves disease, who were referred for 131I
Online version via http://www.eje.org
486
S J Bonnema and others
treatment at our institution. No patient had previously
received 131I. Before 131I therapy, all patients were
treated with methimazole. The dose of methimazole
was adjusted to ensure a stable euthyroidism for at
least 3 months before the 131I treatment. All patients
were instructed to stop the medication 4 days before
undergoing radioiodine therapy. At the time of inclusion
in the study, the patients were allocated randomly (computer-generated numbers in closed envelopes) to groups
either to receive no methimazole (2 ATD) after 131I, or
to resume the pre-treatment dose of methimazole 7
days after the 131I therapy ( ATD). In the latter case,
the medication was subsequently discontinued, at the
earliest, 1 month after 131I, providing biochemical
euthyroidism. The two ATD regimens are summarized
in Fig. 1. Thyroid function was monitored after 3, 6
and 12 weeks, and thereafter every 3 months for a
follow-up period of 1 year. If biochemical evidence of
thyrotoxicosis was observed in the early period after
131
I, b-blockers were commenced, provided that the
patient had symptoms of thyrotoxicosis. If hyperthyroidism persisted beyond 6 weeks, methimazole was reinstituted (2 ATD group) or maintained ( ATD group), and
this medication was subsequently tapered during the
follow-up period. If this was not successful, a second
dose of 131I was eventually administered, at the earliest,
9 months after the initial therapy. Hypothyroidism was
treated with levothyroxine (L -T4). If a low dose of L -T4
was required, a trial of discontinuation was made
within the follow-up period, to ensure that the
hypothyroidism was not transient. At the end of
follow-up, the patients were classified as being hypothyroid, euthyroid or hyperthyroid according to their thyroid
function resulting from the initial 131I treatment (e.g. a
patient developing myxoedema after a second 131I
EUROPEAN JOURNAL OF ENDOCRINOLOGY (2003) 149
administration because of failure of the initial 131I
dose was classified as having recurrence of hyperthyroidism). Euthyroidism was defined as serum T4 and
tri-iodothyronine (T3) indices within the normal range;
hypothyroidism was defined as serum thyroid-stimulating hormone (TSH) above the normal range and serum
T4 index below the normal range; hyperthyroidism was
defined as serum TSH below the normal range and
serum T4 or T3 indices above the normal range.
The study was approved by the Ethics Committee of
the county of Funen, Denmark (journal no. 95/10).
All patients provided signed informed consent.
Assays, imaging and
131
I therapy
Total serum T4 (normal range 65 135 nmol/l) and T3
(normal range 1.00 2.10 nmol/l) were measured by
RIA (Diagnostic Products Corp., Los Angeles, CA,
USA and Johnson & Johnson, Amersham, UK, respectively). Serum TSH (normal range 0.30 4.0 mU/l) was
determined by DELFIA (Wallac OY, Turku, Finland).
Free T4 and free T3 indices were calculated by multiplying the total values by the percent T3 resin uptake.
Serum anti-thyroid peroxidase (anti-TPO) antibodies
were determined at baseline and at the end of followup by the RIA DYNO test (Brahms Diagnostics, Berlin,
Germany; normal range , 200 U/l). Thyroid 99mtechnetium scintigraphy was performed at baseline on a
high resolution gamma camera equipment. Ultrasound, including a morphological imaging and a planimetric volume estimation, was performed at baseline
and 1 year after 131I, by trained endocrinologists.
This method for determination of thyroid volume has
intra- and interobserver coefficients of variation of 5%
and 7% respectively (22). Classification as Graves or
Figure 1 Study design. Until 4 days before the 131I therapy, all patients were treated with methimazole. In the ATD group, methimazole treatment was resumed 7 days after the 131I therapy. Renewed withdrawal of methimazole in that group was performed when the
thyroid function test revealed euthyroidism, at the earliest, 1 month after treatment. In the 2ATD group, methimazole were resumed
only if hyperthyroidism persisted beyond 6 weeks after treatment. d, days; w, weeks; m, months.
www.eje.org
EUROPEAN JOURNAL OF ENDOCRINOLOGY (2003) 149
nodular thyroid disease was based on the clinical presentation, the results of the imaging methods and a
determination of serum TSH-receptor antibodies
(Medi-Lab, Copenhagen, Denmark).
131
I was given routinely as a single oral dose on an
outpatient basis. The amount of radioactivity was
based solely on the size of the gland estimated by ultrasound. The administered activities were 200 MBq for
glands , 30 ml, 400 MBq for glands . 30 ml and
, 60 ml, and 600 MBq if the size was in excess of
60 ml. However, to ensure that the iodine pool was
equal in both groups, a 24-h 131I-uptake measurement
was performed at random in a subset of patients
(n 85).
Statistical analysis
Anticipating a cure rate (euthyroidism or hypothyroidism) of 60% in one of the randomization arms, we calculated that a sample size of 72 per group would
provide 90% power to ensure detection of a difference
in cure rate of at least 25% between the two arms.
Baseline data are presented as mean^S.D. , or median
and range if the data were not normally distributed.
x2-test, one-way analysis of variance (ANOVA) and
Mann Whitney test (if appropriate) were used to compare baseline characteristics, and x2-test and one-way
ANOVA were used in analyses of differences in outcome. McNemars test was used to analyse whether a
shift had occurred in the status of thyroid autoantibodies (negative or positive titre). Measurement errors
are given as 95% confidence intervals (CI). A stepwise
multinomial logistic regression analysis was used for
testing correlations. Logarithmic data transformation
was performed in the case of skewed distribution of
data, or if calculations involved ratios. A P value
, 0.05 was considered statistically significant.
Results
During a period of 3.5 years, a total of 434 hyperthyroid patients were referred for 131I treatment (Fig. 2).
Two hundred and sixty-seven individuals were not eligible for inclusion for various reasons, e.g. current
treatment with propylthiouracil (PTU), large or partly
intrathoracic goitre, allergic reaction to methimazole,
physical or psychiatric disabilities, or anticipation of
practical difficulties in completion of follow-up. Fifteen
patients declined to participate in the trial. Another
three patients were secondarily excluded shortly after
random allocation to groups and before 131I therapy,
because they regretted their commitment. Of the
remaining 149 patients who were included, four individuals died of unrelated causes, and another two
patients were lost to complete follow-up. The thyroid
status of these patients at the time of dropout is
included in the analysis. The patients in the two
Resuming methimazole after
131
I therapy
487
randomization arms did not differ in most baseline
characteristics (Table 1). The median age of the study
population was 59 years (range 23 90 years), but in
the ATD group the patients were, on average, 4.8
years older. Patients with Graves disease were younger
than those with toxic nodular disease (49.8^12.1
years and 63.1^11.3 years, respectively, P , 0.001).
Serum TSH before 131I therapy was below the reference
interval in 58.1% of the patients and did not differ
between the 2 ATD and ATD groups. The median
dose of methimazole was 5.0 mg (range 2.5 20 mg),
and the median 131I activity administered was
400 MBq (range 200 600 MBq; mean 395^154 MBq),
with insignificant between-group differences of both
variables. According to the routine recommended in
our department, glucocorticoids were used prophylactically in 18 patients in order to prevent a worsening of
pre-existing Graves ophthalmopathy. Forty-six patients
suffered from Graves disease, 22 had a solitary toxic
nodule, and 81 were classified as having a multinodular toxic goitre. The median time for discontinuation of
the medication after 131I in the ATD group was 6
weeks (range 4 44 weeks).
At the end of the 1-year follow-up period, 84 patients
were classified as euthyroid, 29 developed permanent
hypothyroidism, and the remaining 36 experienced
recurrence of hyperthyroidism (Table 2). The figures
in each of the two randomization arms were nearly
similar, with no indication of any influence of methimazole on the efficacy of 131I therapy (P 0.88). This also
held true when the outcome was evaluated separately
for type of disease (Table 2). Patients with a multinodular gland were usually (74% of the cases) rendered
euthyroid, whereas this was achieved in only 33% of
patients with Graves disease. Patients with Graves disease significantly more often experienced permanent
hypothyroidism or recurrence, respectively, than did
the patients with non-autoimmune hyperthyroid diseases. This relationship became less obvious according
to a multiple regression model taking into account a
number of factors (including ATD) with a potential
impact on the final effect of 131I therapy (Table 3). In
the case of permanent hypothyroidism, a small thyroid
volume (P 0.014) and young age (P 0.013) were
independent variables, whereas presence of Graves
disease was the only risk factor with regard to recurrence (P 0.015) (Table 3). Sex, presence of pretreatment anti-TPO antibodies and the TSH concentration
were not found to have any independent roles, as was
the case with ATD. In none of the groups was the
status of anti-TPO antibodies significantly altered by
the 131I therapy (conversion of the serum titre from
negative to positive or vice versa).
Marked differences in the serum concentrations of T4
and T3 were seen in the period early after treatment
(Fig. 3). In the ATD group, the serum free-T4 index
decreased by 2 5.7% (95% CI 2 15.5 to 5.4%) and
2 10.6% (CI 95% 2 21.3 to 1.5%) respectively, at
www.eje.org
488
S J Bonnema and others
EUROPEAN JOURNAL OF ENDOCRINOLOGY (2003) 149
Figure 2 Trial profile. *Status of thyroid function at dropout is included in the analysis.
3 and 6 weeks after 131I therapy. In contrast, in the
2 ATD group the same variable increased by 35.9%
(95% CI 18.8 to 55.5%) and 30.1% (95% CI
14.1 to 49.7%) respectively at these times
(P , 0.001; Fig. 3). A similar pattern, although
slightly blunted, was found for the serum free-T3
index (Fig. 3). In the 2 ATD group, 26.4% of the
patients attained thyroid hormone concentrations
above the normal range, compared with 11.1% in the
ATD group, which resulted in a more frequent use
of b-blockade in the former group (eight patients and
one patient, P , 0.02). As persisting hyperthyroidism
triggered an intervention in terms of reinstitution of
www.eje.org
methimazole and, eventually, a second dose of 131I,
no further analysis of this aspect of the 131I therapy
was made beyond these first 6 weeks.
For the euthyroid subgroup, being without influence
from either L -T4 or a second dose of 131I, the reduction
in thyroid volume was 43.4% (95% CI 39.0 to 47.9%).
There was, however, a significantly lower reduction
(38.7%; 95% CI 33.3 to 44.1%) in the ATD group,
compared with that in the 2 ATD group (48.6%; 95%
CI 41.5 to 55.6%) (P , 0.05; Table 2). Stratifying for
type of disease, this difference also held for the patients
with multinodular toxic goitre, but the numbers of
patients with Graves disease and a solitary toxic
Resuming methimazole after
EUROPEAN JOURNAL OF ENDOCRINOLOGY (2003) 149
131
I therapy
489
Table 1 Group characteristics.
Variable
Age (years)
Sex (female/male)
Classification
Graves disease
AFTN
MNTG
Previous thyroidectomy
Thyroid volume (ml)
24-h 131I uptake (%)*
131
I activity administered (MBq)
Presence of anti-TPO antibodies
Serum TSH (mU/l)
Serum free T3 index (nmol/l)
Serum free T4 index (nmol/l)
Prophylactic steroids
ATD resumed (n 73)
ATD not resumed (n 76)
61.6^12.1
58/15
56.8^13.8
66/10
,0.05
ns
17
10
46
4
45 (7140)
65.2^15.7
400 (200600)
20
0.05 (,0.019.12)
1.79^0.72
96.7^46.2
5
29
12
35
4
41 (14125)
65.3^12.1
400 (200600)
25
0.09 (,0.01 4.96)
1.82^0.75
90.6^33.0
13
ns
ns
ns
ns
ns
ns
ns
ns
ns
ns
Values are number of patients, mean^S.D. or median (range).
AFTN, autonomously functioning toxic nodule; MNTG, multinodular toxic goitre.
* Measurement of uptake was performed at random in 85 patients to ensure congruence of this variable between the groups.
Table 2 Thyroid function 1 year after 131I therapy, according to randomization in 149 patients, and reduction in thyroid volume at followup for 77 euthyroid patients.
Thyroid function (H/E/R)
All glands (n 149)
Graves disease (n 46)
AFTN (n 22)
MNTG (n 81)
Thyroid volume reduction (%)
All glands (n 77)
Graves disease (n 13)
AFTN (n 8)
MNTG (n 56)
ATD resumed
ATD not resumed
13/42/18
6/4/7
1/4/5
6/34/6
16/42/18
9/11/9
3/5/4
4/26/5
ns
ns
ns
ns
38.7 (33.3 to 44.1)
55.4 (41.7 to 69.1)
47.8 (20.1 to 75.5)
36.1 (30.3 to 41.9)
48.6 (41.5 to 55.6)
61.2 (51.4 to 71.0)
27.9 (0.0 to 83.7)
46.7 (38.7 to 54.6)
,0.05
ns
ns
,0.05
Values are numbers of patients or mean (95% confidence interval).
H, hypothyroidism; E, euthyroidism; R, recurrence; AFTN, autonomously functioning toxic nodule; MNTG, multinodular toxic goitre.
Table 3 Relevant variables included in the regression analysis
for prediction of either recurrence or hypothyroidism 1 year after
131
I therapy.
Variable
ATD resumption
Sex
Graves disease
Presence of anti-TPO Ab
Small thyroid volume
Young age
TSH concentration before 131I
Recurrence
(n 36)
Hypothyroidism
(n 29)
ns
ns
P 0.015
ns
ns
ns
ns
ns
ns
ns
ns
P 0.014
P 0.013
ns
AB, antibody.
nodule were too small to allow any valid conclusion to
be drawn (Table 2). Possible confounding factors, such
as the pretreatment concentrations of serum TSH and
anti-TPO antibodies, and age, did not affect this
relationship between resumption of methimazole and
reduction in thyroid volume.
Discussion
This study enrolling 149 patients with hyperthyroid
diseases is the first randomized trial to evaluate the
impact of the resumption of methimazole 7 days after
131
I therapy, and it is one of very few randomized
studies addressing the issue of radioprotective properties of ATD. Recent randomized trials (20, 21) have
documented in sharp contrast to what was indicated
by previous retrospective studies (4 13) that pretreating hyperthyroid patients with methimazole
before 131I therapy does not interfere with the final
cure rate. In 1988, Velkeniers et al. (14) reported that
treatment failure occurred almost five times more
often if ATDs were resumed after 131I therapy of
hyperthyroidism. Subsequently, the findings of other
studies (15 17) supported the view that the use of
ATDs in the period after 131I treatment reduced the
cure rate from the therapy, in some cases associated
with a blunted 131I-induced increase in the titres of
thyroid autoantibodies (17). However, all those studies
www.eje.org
490
S J Bonnema and others
Figure 3 Percent changes in (a) serum free thyroxine (FT4) index
and (b) serum free tri-iodothyronine (FT3) index in the early period
after 131I treatment. Pretreatment values are given as 100%. Bars
represent 95% confidence intervals. *P , 0.001, **P 0.004
comparing the 2ATD (n 76) and ATD groups (n 73).
(14 17) suffered from the drawbacks unavoidable in
retrospective designs. In the randomized study by
Kung et al. (18), also dealing with the impact of methimazole in the period after 131I therapy, a lower incidence of early permanent hypothyroidism, but not of
recurrence, was demonstrated after 131I therapy of
patients with Graves disease. In that study (18),
patients were not pre-treated with ATDs, and methimazole was instituted 4 days after 131I therapy, followed by
a block-replacement regimen, which included a larger
dose of methimazole than was used in the present
study, in addition to L -T4.
The two regimens applied in our study are widely used
routinely at institutions treating patients with
hyperthyroidism, and we could not demonstrate any
effect on the final thyroid function caused by the
resumption of methimazole 7 days after 131I treatment.
It remains an open question whether the outcome would
have been different if the delay between the administration of 131I and the resumption of methimazole
www.eje.org
EUROPEAN JOURNAL OF ENDOCRINOLOGY (2003) 149
had been shorter. Our findings are further underscored
by the outcome of the multivariate analysis taking into
account the type of disease, thyroid volume, anti-TPO
antibodies, TSH concentration at treatment, age and
sex. In such an analysis, correction is made for any
bias that might have occurred despite randomization.
Only the presence of Graves disease was related to recurrence of hyperthyroidism. Young age per se did not prove
to be an independent factor, as has been shown in other
studies (12, 13), but this finding probably reflects the
fact that patients with Graves disease were younger
than those with thyroid nodular diseases.
Although a 24-h uptake measurement was performed to ensure congruence between the two randomization groups, dosage of the 131I therapy was
calculated according to a simplified algorithm taking
into account only the thyroid volume (estimated by
ultrasound). At several institutions, including ours,
elaborate algorithms for dose calculation have been disregarded in favour of a more simple approach. This is
justified by studies showing that calculated doses do
not carry any advantages over fixed doses (23 25).
Detrimental to any algorithm that includes a 24-h
uptake is the great variation in 131I uptake and turnover over short periods of time (26). In addition, the
correlation between the intended and the actual dose
delivered to the thyroid is highly variable, with a
mean coefficient of variation of 45% (27). It is therefore
not surprising that susceptibility of the thyroid to a
wide range of 131I radiation shows huge individual
variations (28).
Similarly to other recent studies (12, 29, 30) performed in order to evaluate the efficacy of 131I therapy,
we included patients with both autoimmune (Graves
disease) and non-autoimmune hyperthyroid diseases.
Our finding of no radioprotection of methimazole,
among patients with either Graves disease or toxic
nodular goitre, is in contrast to the findings by Korber
et al. (30). In their study, continuation of ATD therapy
until at least 14 days after 131I therapy resulted in a
lower success rate, but only among patients with
toxic nodular disease. However, patients were not allocated randomly to groups, and those receiving ATDs
had greater serum concentrations of TSH, which was
not the case in our study. In non-randomized studies,
patients who continue to take ATDs during and after
131
I therapy are prone to suffer from a more aggressive
disease, with a greater degree of hyperthyroidism. This
is obviously a source of bias that cannot easily be corrected for in a multivariate analysis. Thus, on the
basis of our own results, we find no reason to believe
that any radioprotective effect from methimazole
should act preferentially against certain subtypes of
hyperthyroid disease, provided the TSH concentration
is taken into account. One study (7) also non-randomized has indicated that PTU could have a greater
radioprotective effect, if any such effect were present at
all, than methimazole. For this reason we excluded
EUROPEAN JOURNAL OF ENDOCRINOLOGY (2003) 149
patients pre-treated with PTU. Whether this drug has
any radioprotective potential when tested in a randomized design remains an open question.
Although the resumption of methimazole did not
affect long-term thyroid function, some impact was
found as regards thyroid volume. The ultrasound planimetric method used in this study is a very precise
method for estimation of thyroid volume (22). The
overall 43% reduction in thyroid volume, a little less
for nodular glands and more for diffuse glands, corresponds well to the results from earlier studies (31 33).
However, in patients who resumed methimazole, 131I
treatment resulted in a significantly smaller reduction
in thyroid volume. An independency of the effects of
131
I on thyroid size and function has been described
previously (31). The difference was detectable only in
multinodular glands showing a reduction in thyroid
volume of 36% if methimazole was resumed, compared
with 47% if methimazole was not resumed. Our finding seems to be of only minor clinical relevance in
most patients; however, should the hyperthyroidism
be caused by a large symptomatic compressive thyroid
gland, methimazole should probably not be resumed
after 131I therapy, in order to optimize the reduction
in goitre size.
The most pronounced difference between the two
regimens used in this study was seen in the thyroid hormone concentrations early after the 131I therapy. In
patients randomly assigned to resumption of methimazole, thyroid function was very stable after the 131I
therapy and fluctuations in the thyroid hormone concentrations were generally avoided. In contrast, the
serum T4 concentration increased by a mean of 36%
at 3 weeks if methimazole was not resumed, which
resulted in more patients having symptoms of
thyrotoxicosis. Radiation thyroiditis defined as thyroid tenderness, increased sedimentation rate and
thyrotoxicosis is seen in a small percentage of
patients after 131I therapy (34). To avoid dumping
of thyroid hormones into the circulation and the rare
precipitation of thyroid storm, guidelines (35) recommend pretreatment with ATDs before 131I therapy,
to deplete the thyroid hormone stores. The importance
of thyroid peroxidase suppression during 131I therapy
has been elucidated by Andrade et al. (36) and Burch
et al. (37). From these important studies, both randomized, it is clear that 131I therapy in untreated and
thyrotoxic patients with Graves disease does not lead
to any further secretion of the thyroid hormones. In
contrast, in patients rendered euthyroid by ATDs, the
serum hormone concentrations increase by 50 100%
(but from a euthyroid level) if the medication is discontinued a few days before 131I therapy (36, 37).
Although 131I therapy per se apparently does not
cause exacerbation of the thyrotoxicosis, the present
results clearly show that, once methimazole has been
instituted in hyperthyroid patients, this restraint upon
the thyroid hormone production is important to carry
Resuming methimazole after
131
I therapy
491
through until the destructive effect of the 131I therapy
ensues. By resumption of methimazole after 131I
therapy, the early and transient thyrotoxic phase can
be avoided, and although such strategy seems to
attenuate the goitre shrinkage to a minor degree in
patients with multinodular glands, it does not interfere
with the final outcome as regards thyroid function.
Acknowledgements
This study was supported by research grants from The
Agnes and Knut Mrks Foundation and The A.P. Mller
Support Foundation.
References
1 Solomon B, Glinoer D, Lagasse R & Wartofsky L. Current trends in
the management of Graves disease. Journal of Clinical Endocrinology and Metabolism 1990 70 1518 1524.
2 Imamura M, Aoki N, Saito T, Ohno Y, Maruyama Y, Yamaguchi J
et al. Inhibitory effects of antithyroid drugs on oxygen radical formation in human neutrophils. Acta Endocrinologica 1986 112
210216.
3 Connell JM, Hilditch TE, Robertson J, Coghill G & Alexander WD.
Radioprotective action of carbimazole in radioiodine therapy for
thyrotoxicosis influence of the drug on iodine kinetics. European
Journal of Nuclear Medicine 1987 13 358 361.
4 Crooks J, Buchanan WW, Wayne EJ & MacDonald E. Effect of
pretreatment with methylthiouracil on results of 131I therapy.
British Medical Journal 1960 16 151154.
5 Clerc J, Izembart M, Dagousset F, Jais JP, Heshmati HM, Chevalier
A et al. Influence of dose selection on absorbed dose profiles in
radioiodine treatment of diffuse toxic goiters in patients receiving
or not receiving carbimazole. Journal of Nuclear Medicine 1993 34
387393.
6 Hancock LD, Tuttle RM, LeMar H, Bauman J & Patience T. The
effect of propylthiouracil on subsequent radioactive iodine
therapy in Graves disease. Clinical Endocrinology 1997 47
425430.
7 Imseis RE, Vanmiddlesworth L, Massie JD, Bush AJ & Vanmiddlesworth NR. Pretreatment with propylthiouracil but not methimazole reduces the therapeutic efficacy of iodine-131 in
hyperthyroidism. Journal of Clinical Endocrinology and Metabolism
1998 83 685687.
8 Reynolds LR & Kotchen TA. Antithyroid drugs and radioactive
iodine. Fifteen years experience with Graves disease. Archives of
Internal Medicine 1979 139 651653.
9 Sabri O, Zimny M, Schulz G, Schreckenberger M, Reinartz P, Willmes K et al. Success rate of radioiodine therapy in Graves disease:
the influence of thyrostatic medication. Journal of Clinical Endocrinology and Metabolism 1999 84 12291233.
10 Turton DB, Silverman ED & Shakir KM. Time interval between the
last dose of propylthiouracil and I-131 therapy influences cure
rates in hyperthyroidism caused by Graves disease. Clinical
Nuclear Medicine 1998 23 810 814.
11 Tuttle RM, Patience T & Budd S. Treatment with propylthiouracil
before radioactive iodine therapy is associated with a higher treatment failure rate than therapy with radioactive iodine alone in
Graves disease. Thyroid 1995 5 243247.
12 Allahabadia A, Daykin J, Sheppard MC, Gough SC & Franklyn JA.
Radioiodine treatment of hyperthyroidism prognostic factors for
outcome. Journal of Clinical Endocrinology and Metabolism 2001 86
36113617.
13 Alexander EK & Larsen PR. High dose of (131)I therapy for the
treatment of hyperthyroidism caused by Graves disease. Journal
of Clinical Endocrinology and Metabolism 2002 87 10731077.
www.eje.org
492
S J Bonnema and others
14 Velkeniers B, Cytryn R, Vanhaelst L & Jonckheer MH. Treatment
of hyperthyroidism with radioiodine: adjunctive therapy with
antithyroid drugs reconsidered. Lancet 1988 1 11271129.
15 Jarlv AE, Christensen E, Hegedus L, Kristensen L., Nygaard B &
Hansen JM. Factors associated with recurrence of hyperthyroidism after 131I treatment: the inadvertent influence of antithyroid
drug administration after 131I treatment of hyperthyroidism.
Thyroidology 1997 9 55 59.
16 Marcocci C, Gianchecchi D, Masini I, Golia F, Ceccarelli C, Bracci E
et al. A reappraisal of the role of methimazole and other factors on
the efficacy and outcome of radioiodine therapy of Graves
hyperthyroidism. Journal of Endocrinological Investigation 1990
13 513520.
17 Nakazato N, Yoshida K, Mori K, Kiso Y, Sayama N, Tani JI et al.
Antithyroid drugs inhibit radioiodine-induced increases in thyroid
autoantibodies in hyperthyroid Graves disease. Thyroid 1999 9
775 779.
18 Kung AW, Yau CC & Cheng AC. The action of methimazole and
L-thyroxine in radioiodine therapy: a prospective study on the
incidence of hypothyroidism. Thyroid 1995 5 712.
19 Perros P. Anti-thyroid drug treatment before radioiodine in
patients with Graves disease: soother or menace? Clinical Endocrinology 2000 53 12.
20 Braga M, Walpert N, Burch HB, Solomon BL & Cooper DS. The
effect of methimazole on cure rates after radioiodine treatment
for Graves hyperthyroidism: a randomized clinical trial. Thyroid
2002 12 135 139.
21 Andrade VA, Gross JL & Maia AL. The effect of methimazole pretreatment on the efficacy of radioactive iodine therapy in Graves
hyperthyroidism: one-year follow-up of a prospective, randomized
study. Journal of Clinical Endocrinology and Metabolism 2001 86
34883493.
22 Hegedus L. Thyroid size determined by ultrasound. Influence of
physiological factors and non-thyroidal disease (Thesis). Danish
Medical Bulletin 1990 37 249263.
23 Kok SW, Smit JW, de Craen AJ, Goslings BM, Eck-Smit BL &
Romijn JA. Clinical outcome after standardized versus dosimetric
radioiodine treatment of hyperthyroidism: an equivalence study.
Nuclear Medicine Communications 2000 21 10711078.
24 Jarlv AE, Hegedus L, Kristensen L, Nygaard B & Hansen JM. Is
calculation of the dose in radioiodine therapy of hyperthyroidism
worth while? Clinical Endocrinology 1995 43 325 329.
25 Leslie WD, Ward L, Salamon EA, Ludwig S, Rowe RC & Cowden
EA. A randomized comparison of radioiodine doses in Graves
hyperthyroidism. Journal of Clinical Endocrinology and Metabolism
2003 88 978 983.
26 Van Isselt JW, de Klerk JM, Koppeschaar HP & Van Rijk PP. Iodine131 uptake and turnover rate vary over short intervals in Graves
disease. Nuclear Medicine Communications 2000 21 609616.
www.eje.org
EUROPEAN JOURNAL OF ENDOCRINOLOGY (2003) 149
27 Catargi B, Leprat F, Guyot M, Valli N, Ducassou D & Tabarin A.
Optimized radioiodine therapy of Graves disease: analysis of the
delivered dose and of other possible factors affecting outcome.
European Journal of Endocrinology 1999 141 117121.
28 Howarth D, Epstein M, Lan L, Tan P & Booker J. Determination of
the optimal minimum radioiodine dose in patients with Graves
disease: a clinical outcome study. European Journal of Nuclear Medicine 2001 28 14891495.
29 Ahmad AM, Ahmad M & Young ET. Objective estimates of the
probability of developing hypothyroidism following radioactive
iodine treatment of thyrotoxicosis. European Journal of Endocrinology 2002 146 767775.
30 Korber C, Schneider P, Korber-Hafner N, Hanscheid H & Reiners C.
Antithyroid drugs as a factor influencing the outcome of radioiodine therapy in Graves disease and toxic nodular goitre? European
Journal of Nuclear Medicine 2001 28 1360 1364.
31 Nygaard B, Hegedus L, Gervil M, Hjalgrim H, Hansen BM, SeJensen P et al. Influence of compensated radioiodine therapy on
thyroid volume and incidence of hypothyroidism in Graves disease. Journal of Internal Medicine 1995 238 491497.
32 Nygaard B, Hegedus L, Nielsen KG, Ulriksen P & Hansen JM.
Long-term effect of radioactive iodine on thyroid function and
size in patients with solitary autonomously functioning toxic
thyroid nodules. Clinical Endocrinology 1999 50 197 202.
33 Nygaard B, Hegedus L, Ulriksen P, Nielsen KG & Hansen JM.
Radioiodine therapy for multinodular toxic goiter. Archives of
Internal Medicine 1999 159 13641368.
34 Nygaard B, Knudsen JH, Hegedus L, Veje A & Hansen JE. Thyrotropin receptor antibodies and Graves disease, a side-effect of
131I treatment in patients with nontoxic goiter. Journal of Clinical
Endocrinology and Metabolism 1997 82 29262930.
35 Meier DA, Brill DR, Becker DV, Clarke SE, Silberstein EB, Royal HD
et al. Procedure guideline for therapy of thyroid disease with
(131)iodine. Journal of Nuclear Medicine 2002 43 856 861.
36 Andrade VA, Gross JL & Maia AL. Effect of methimazole pretreatment on serum thyroid hormone levels after radioactive treatment in Graves hyperthyroidism. Journal of Clinical
Endocrinology and Metabolism 1999 84 40124016.
37 Burch HB, Solomon BL, Cooper DS, Ferguson P, Walpert N &
Howard R. The effect of antithyroid drug pretreatment on acute
changes in thyroid hormone levels after (131)I ablation for
Graves disease. Journal of Clinical Endocrinology and Metabolism
2001 86 30163021.
Received 6 June 2003
Accepted 22 August 2003
Das könnte Ihnen auch gefallen
- Thyroid Suppression Test With L-Thyroxine and TC) PertechnetateDokument7 SeitenThyroid Suppression Test With L-Thyroxine and TC) PertechnetatejeffsunilNoch keine Bewertungen
- ClonidineDokument4 SeitenClonidineDR RAVI ANANDNoch keine Bewertungen
- Bja 2013Dokument9 SeitenBja 2013Gihan NakhlehNoch keine Bewertungen
- Chassot 2012Dokument9 SeitenChassot 2012docadax848Noch keine Bewertungen
- 33 FullDokument5 Seiten33 FullIndahK.WardhaniPutriNoch keine Bewertungen
- Henke 2003Dokument6 SeitenHenke 2003handrionoNoch keine Bewertungen
- 3781 FullDokument6 Seiten3781 FullSukhvinder Singh RanaNoch keine Bewertungen
- Wa0010.Dokument9 SeitenWa0010.deinoterraNoch keine Bewertungen
- Early Postoperative ComplicationsDokument6 SeitenEarly Postoperative Complications49hr84j7spNoch keine Bewertungen
- Comparison of Ketamine-Midazolam-Propofol Combination and Fentanyl-Midazolam-Propofol Combination For Sedation in ColonosDokument8 SeitenComparison of Ketamine-Midazolam-Propofol Combination and Fentanyl-Midazolam-Propofol Combination For Sedation in ColonosDendy AgusNoch keine Bewertungen
- Thyroid-Hormone Concentrations After Radiolodine Therapy For HyperthyroidismDokument5 SeitenThyroid-Hormone Concentrations After Radiolodine Therapy For HyperthyroidismShane AllenNoch keine Bewertungen
- Haloperidol Combined With DexamethasoneDokument6 SeitenHaloperidol Combined With Dexamethasoneapi-741687858Noch keine Bewertungen
- Seo2016 PDFDokument8 SeitenSeo2016 PDFNovia AyuNoch keine Bewertungen
- dst50234 PDFDokument7 Seitendst50234 PDFtaniaNoch keine Bewertungen
- HyperthyroidDokument7 SeitenHyperthyroidHaerun Nisa SiregarNoch keine Bewertungen
- Remifentanil Compared With Midazolam and Pethidine Sedation During Colonoscopy: A Prospective, Randomized StudyDokument7 SeitenRemifentanil Compared With Midazolam and Pethidine Sedation During Colonoscopy: A Prospective, Randomized Studyade_liaNoch keine Bewertungen
- The Analgesic Efficacy of Tramadol As A Pre-Emptive Analgesic in Pediatric Appendectomy Patients PDFDokument6 SeitenThe Analgesic Efficacy of Tramadol As A Pre-Emptive Analgesic in Pediatric Appendectomy Patients PDFUmmu Qonitah AfnidawatiNoch keine Bewertungen
- The Effects of Age On Neural Blockade and Hemodynamic Changes After Epidural Anesthesia With RopivacaineDokument6 SeitenThe Effects of Age On Neural Blockade and Hemodynamic Changes After Epidural Anesthesia With RopivacaineAnonymous K9tmd7T0PzNoch keine Bewertungen
- Annals of International Medical and Dental ResearchDokument4 SeitenAnnals of International Medical and Dental ResearchDr Rohit varshneyNoch keine Bewertungen
- Retroperitoneal MassDokument22 SeitenRetroperitoneal Massapi-434838777Noch keine Bewertungen
- Hellp 2Dokument7 SeitenHellp 2Nur Rahmat WibowoNoch keine Bewertungen
- Adrenal Insufficiency in Thyroid Cancer Patients Treated With Tyrosine Kinase Inhibitors and Detected by ACTH Stimulation TestDokument9 SeitenAdrenal Insufficiency in Thyroid Cancer Patients Treated With Tyrosine Kinase Inhibitors and Detected by ACTH Stimulation TestEmanuel CalderonNoch keine Bewertungen
- Artikel Mathemathical Model Graves DiseaseDokument12 SeitenArtikel Mathemathical Model Graves DiseaseFreija GeldofNoch keine Bewertungen
- Prevention of Shivering During Regional Anaesthesia - Comparison of Midazolam, Midazolam Plus Ketamine, Tramadol, and Tramadol Plus KetamineDokument17 SeitenPrevention of Shivering During Regional Anaesthesia - Comparison of Midazolam, Midazolam Plus Ketamine, Tramadol, and Tramadol Plus Ketamineandi ananNoch keine Bewertungen
- Ajrccm 163 1 16310aDokument3 SeitenAjrccm 163 1 16310amisulica2010Noch keine Bewertungen
- Jurnal AnastesiDokument5 SeitenJurnal AnastesiNadya Tenriany NajibNoch keine Bewertungen
- Randomised Trial of Corticosteroids in The of Tuberculous PleurisyDokument4 SeitenRandomised Trial of Corticosteroids in The of Tuberculous PleurisyDrVinod Kumar Goud VemulaNoch keine Bewertungen
- Taprogge Et Al 2021 A Systematic Review and Meta Analysis of The Relationship Between The Radiation Absorbed Dose ToDokument10 SeitenTaprogge Et Al 2021 A Systematic Review and Meta Analysis of The Relationship Between The Radiation Absorbed Dose ToLesly LoachamínNoch keine Bewertungen
- Personalized Dosimetry in Diagnostic and Therapeutic Nuclear MedicineDokument34 SeitenPersonalized Dosimetry in Diagnostic and Therapeutic Nuclear MedicineRafa PopocaNoch keine Bewertungen
- Adherence To Oral Hypoglycemic MedicatioDokument20 SeitenAdherence To Oral Hypoglycemic Medicatioashenafi woldesenbetNoch keine Bewertungen
- 2014-Effects and Mechanisms of Transcutaneous Electroacupuncture On Chemotherapy Induced Nausea and VomitingDokument6 Seiten2014-Effects and Mechanisms of Transcutaneous Electroacupuncture On Chemotherapy Induced Nausea and VomitingvictoregvNoch keine Bewertungen
- The Hemodynamic Effects of Propofol in Children With Congenital Heart DiseaseDokument6 SeitenThe Hemodynamic Effects of Propofol in Children With Congenital Heart DiseaseAngelica Lucero OrtizNoch keine Bewertungen
- 2010 Stuard Pycnogenol Improves Kidney Function in Metabolic SyndromeDokument6 Seiten2010 Stuard Pycnogenol Improves Kidney Function in Metabolic Syndromeindoglo1Noch keine Bewertungen
- Journal 2Dokument6 SeitenJournal 2chaNoch keine Bewertungen
- 701 2011 Article 959Dokument9 Seiten701 2011 Article 959Kumaran Bagavathi RagavanNoch keine Bewertungen
- 20Dokument9 Seiten20Amina GoharyNoch keine Bewertungen
- Dome-And-Dart T Waves and Hyperthyroidism - A Case ReportDokument3 SeitenDome-And-Dart T Waves and Hyperthyroidism - A Case ReportMiftah MiftahNoch keine Bewertungen
- Dysphagia: Impact On Quality of Life After Radio (Chemo) Therapy of Head and Neck CancerDokument7 SeitenDysphagia: Impact On Quality of Life After Radio (Chemo) Therapy of Head and Neck CancerNurul Afika LubisNoch keine Bewertungen
- Sedation For Fibreoptic Gastroscopy: A Comparative Study of Midazolam and DiazepamDokument8 SeitenSedation For Fibreoptic Gastroscopy: A Comparative Study of Midazolam and DiazepamRomaNoch keine Bewertungen
- JCO 2005 Pink 6809 11Dokument3 SeitenJCO 2005 Pink 6809 11claudiaNoch keine Bewertungen
- NIH Public Access: Author ManuscriptDokument10 SeitenNIH Public Access: Author ManuscriptNurci Efrilia SafitriNoch keine Bewertungen
- AMPT-induced Monoamine Depletion in Humans: Evaluation of Two Alternative (123I) IBZM SPECT ProceduresDokument7 SeitenAMPT-induced Monoamine Depletion in Humans: Evaluation of Two Alternative (123I) IBZM SPECT ProceduresMihaela ToaderNoch keine Bewertungen
- Radio Active Iodine Ablation in Well Differentiated Thyroid Cancers 2155 9619.1000e103Dokument1 SeiteRadio Active Iodine Ablation in Well Differentiated Thyroid Cancers 2155 9619.1000e103Yola Ivonny HariantoNoch keine Bewertungen
- Jcem2157 PDFDokument6 SeitenJcem2157 PDFRidwan Putra Beng-BengNoch keine Bewertungen
- Jurnal AnastesiaDokument8 SeitenJurnal AnastesiaFikri SatriaNoch keine Bewertungen
- 00003Dokument8 Seiten00003Anonymous zPwXqwNoch keine Bewertungen
- Nice SugarDokument15 SeitenNice SugarRafaela LealNoch keine Bewertungen
- A Double Blind, Randomised, Controlled Trial To Study The Effect of Dexmeditomidine On Hemodynamic and Recovery Responses During Tracheal ExtubationDokument8 SeitenA Double Blind, Randomised, Controlled Trial To Study The Effect of Dexmeditomidine On Hemodynamic and Recovery Responses During Tracheal ExtubationramukolakiNoch keine Bewertungen
- Rogers 1993Dokument4 SeitenRogers 1993Nadia SaiNoch keine Bewertungen
- Consevative RX of AnDokument6 SeitenConsevative RX of AnMusthafa Afif WardhanaNoch keine Bewertungen
- AJCC6 TH Ed Cancer Staging Manual Part 1Dokument8 SeitenAJCC6 TH Ed Cancer Staging Manual Part 1handrionoNoch keine Bewertungen
- 689 FullDokument5 Seiten689 FullBlu TuxNoch keine Bewertungen
- Reports of Practical Oncology and Radiotherapy 1 8 (2 0 1 3) S186-S197Dokument2 SeitenReports of Practical Oncology and Radiotherapy 1 8 (2 0 1 3) S186-S197Elisa SalakayNoch keine Bewertungen
- Hemodynamic Effects of Chest-Knee Position: Comparison of Perioperative Propofol and Sevoflurane AnesthesiaDokument6 SeitenHemodynamic Effects of Chest-Knee Position: Comparison of Perioperative Propofol and Sevoflurane AnesthesiaAprilico Fadhil PangestuNoch keine Bewertungen
- Comparison of The Efficacy of Propofol TCI and Midazolam For Patients Undergoing ESWL - RCTDokument5 SeitenComparison of The Efficacy of Propofol TCI and Midazolam For Patients Undergoing ESWL - RCTharvardboyNoch keine Bewertungen
- Consensus and Controversy of Radioiodine and PET (Or Pet/Ct) in The Management of Well-Differentiated Thyroid CancerDokument31 SeitenConsensus and Controversy of Radioiodine and PET (Or Pet/Ct) in The Management of Well-Differentiated Thyroid CancerBosan KhalidNoch keine Bewertungen
- New Evidence in Home Mechanical Ventilation: Thematic Poster Session Hall 2-4 - 12:50-14:40Dokument5 SeitenNew Evidence in Home Mechanical Ventilation: Thematic Poster Session Hall 2-4 - 12:50-14:40Shirley CoelhoNoch keine Bewertungen
- 131I Therapy For Elevated Thyroglobulin LevelsDokument8 Seiten131I Therapy For Elevated Thyroglobulin LevelsMeutia sariNoch keine Bewertungen
- TraztuzumabDokument8 SeitenTraztuzumabArlina Wiyata GamaNoch keine Bewertungen
- Introduction To Parasitology & Lab Diagnosis of ParasiticDokument33 SeitenIntroduction To Parasitology & Lab Diagnosis of ParasiticMaharRkpNoch keine Bewertungen
- Cell Structures Part One: Roxanne Ferguson Biology Graves County High SchoolDokument13 SeitenCell Structures Part One: Roxanne Ferguson Biology Graves County High SchoolMaharRkpNoch keine Bewertungen
- Functional Expressions Starting The CommunicationDokument7 SeitenFunctional Expressions Starting The CommunicationMaharRkpNoch keine Bewertungen
- 6 Adjective ClauseDokument16 Seiten6 Adjective ClauseMaharRkpNoch keine Bewertungen
- 8 Functional ExpressionsDokument35 Seiten8 Functional ExpressionsMaharRkpNoch keine Bewertungen
- 10 AbbreviationDokument5 Seiten10 AbbreviationMaharRkpNoch keine Bewertungen
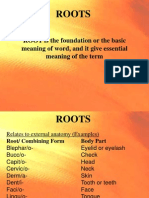
- Roots: ROOT Is The Foundation or The Basic Meaning of Word, and It Give Essential Meaning of The TermDokument4 SeitenRoots: ROOT Is The Foundation or The Basic Meaning of Word, and It Give Essential Meaning of The TermMaharRkpNoch keine Bewertungen
- Cell VocabularyDokument18 SeitenCell VocabularyMaharRkpNoch keine Bewertungen
- Mitosis and The Cell CycleDokument27 SeitenMitosis and The Cell CycleMaharRkpNoch keine Bewertungen
- Mutasi Gonosom ManusiaDokument20 SeitenMutasi Gonosom ManusiaMaharRkpNoch keine Bewertungen
- Cell Structures Lesson2Dokument12 SeitenCell Structures Lesson2MaharRkpNoch keine Bewertungen
- Cell Division: MeiosisDokument16 SeitenCell Division: MeiosisMaharRkpNoch keine Bewertungen
- Roots: ROOT Is The Foundation or The Basic Meaning of Word, and It Give Essential Meaning of The TermDokument4 SeitenRoots: ROOT Is The Foundation or The Basic Meaning of Word, and It Give Essential Meaning of The TermMaharRkpNoch keine Bewertungen
- 6 Adjective ClauseDokument16 Seiten6 Adjective ClauseMaharRkp100% (1)
- A Comparison of The Revised Delirium Rating ScaleDokument8 SeitenA Comparison of The Revised Delirium Rating ScaleMaharRkpNoch keine Bewertungen
- English of NursingDokument6 SeitenEnglish of NursingMaharRkpNoch keine Bewertungen
- Pengaruh Deep Back Massage Terhadap Penurunan NyeriDokument14 SeitenPengaruh Deep Back Massage Terhadap Penurunan NyeriMaharRkpNoch keine Bewertungen
- Uv DoseDokument6 SeitenUv DoseRajesh DeshmukhNoch keine Bewertungen
- Aceclofenac Vs Diclofenac On Hexosamine LevelsDokument11 SeitenAceclofenac Vs Diclofenac On Hexosamine LevelsMartin MoranNoch keine Bewertungen
- PlacentaDokument21 SeitenPlacentaAttiqaQureshiNoch keine Bewertungen
- Klinefelters SyndromeDokument2 SeitenKlinefelters SyndromeAlexandra Gabriella ZawisnyNoch keine Bewertungen
- Grade 4 Chondromalacia Patella TreatmentDokument3 SeitenGrade 4 Chondromalacia Patella TreatmentTroy0% (1)
- 2 Articles From Oui Magazine (Feat. Robert Anton Wilson)Dokument16 Seiten2 Articles From Oui Magazine (Feat. Robert Anton Wilson)Jakob AndradeNoch keine Bewertungen
- Form 4 Medical Certificate For Non-Gazetted Officer Recommended For Leave or Extension or Commutation of LeaveDokument2 SeitenForm 4 Medical Certificate For Non-Gazetted Officer Recommended For Leave or Extension or Commutation of LeaveDr RajaNoch keine Bewertungen
- Refeeding SyndromeDokument10 SeitenRefeeding SyndromePhysiology by Dr RaghuveerNoch keine Bewertungen
- Order of Payment: Food and Drug AdministrationDokument2 SeitenOrder of Payment: Food and Drug AdministrationTheGood GuyNoch keine Bewertungen
- CeftriaxoneDokument2 SeitenCeftriaxoneFlora Angeli PastoresNoch keine Bewertungen
- A Systematic Review of Trunk Restraint TrainingDokument1 SeiteA Systematic Review of Trunk Restraint Traininggans_therapist3321Noch keine Bewertungen
- AJODO-90 Petrovic Et Al Role of The Lateral Pterigoid Muscle and Menisco Temporomandibular...Dokument12 SeitenAJODO-90 Petrovic Et Al Role of The Lateral Pterigoid Muscle and Menisco Temporomandibular...ortodoncia 2018Noch keine Bewertungen
- Medical Laboratory Technology Journal: Potensi Antifungi Tangkai Daun Jarak Pagar Terhadap PERTUMBUHAN Candida AlbicansDokument5 SeitenMedical Laboratory Technology Journal: Potensi Antifungi Tangkai Daun Jarak Pagar Terhadap PERTUMBUHAN Candida Albicanskhoko holicNoch keine Bewertungen
- WC500059147 PDFDokument140 SeitenWC500059147 PDFAnaStankovićNoch keine Bewertungen
- Case Study - DR EldaDokument3 SeitenCase Study - DR EldaShashi KumarNoch keine Bewertungen
- Neuroshield ReportDokument2 SeitenNeuroshield Reportrahim pathanNoch keine Bewertungen
- Case Study 103Dokument8 SeitenCase Study 103Jonah MaasinNoch keine Bewertungen
- Pediatric Meningitis Case StudyDokument5 SeitenPediatric Meningitis Case StudyCheska PalomaNoch keine Bewertungen
- Una Coales-Get Through Medical School - 1000 Sbas Bofs and Emqs (Get Through Series) (2003) PDFDokument151 SeitenUna Coales-Get Through Medical School - 1000 Sbas Bofs and Emqs (Get Through Series) (2003) PDFCathy QianNoch keine Bewertungen
- Metatron Resonance Brochure WebsiteDokument3 SeitenMetatron Resonance Brochure WebsiteShaun DennisNoch keine Bewertungen
- Pre-Diabetes:: Don't Let It Lead To Type-2Dokument1 SeitePre-Diabetes:: Don't Let It Lead To Type-2ARIA MINDNoch keine Bewertungen
- Service Manual 2008-10-09 SP1Dokument116 SeitenService Manual 2008-10-09 SP1brunorafoNoch keine Bewertungen
- Physiotherapy in DementiaDokument4 SeitenPhysiotherapy in DementiaNabilla Yuharlina100% (1)
- PMLS 2 LEC Module 3Dokument8 SeitenPMLS 2 LEC Module 3Peach DaquiriNoch keine Bewertungen
- Romsons All ProductDokument53 SeitenRomsons All ProductBoyke WinterbergNoch keine Bewertungen
- Writing Letters of RecommendationDokument4 SeitenWriting Letters of Recommendationwenskyrose1100% (1)
- Case Study AnalysisDokument13 SeitenCase Study Analysisapi-317809407Noch keine Bewertungen
- Orthodontics!!Dokument9 SeitenOrthodontics!!Ayesha AwanNoch keine Bewertungen
- Saccharothrixsp Abh26 PDFDokument7 SeitenSaccharothrixsp Abh26 PDFAlia RahmaNoch keine Bewertungen