Beruflich Dokumente
Kultur Dokumente
Preoperative Assessment
Hochgeladen von
1234chocoCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Preoperative Assessment
Hochgeladen von
1234chocoCopyright:
Verfügbare Formate
ANAESTHESIA II
Anaesthesia II
Preoperative assessment
F J Garca-Miguel, P G Serrano-Aguilar, J Lpez-Bastida
Although anaesthetic and surgical procedures should be individualised for every patient, in practice many preoperative
protocols and routines are used generally. In this article, we aim to emphasise: why preoperative assessment is
important; how it should be done, and by whom; what can be expected; and the importance of test selection based on
patients needs and on scientific evidence of effectiveness. We outline the roles of preoperative medical assessment
in otherwise healthy patients. Clinical history, preoperative questionnaires, physical examination, routine tests,
individual risk-assessment, and fasting policies are investigated by review of published work. Cost of routine
preoperative assessment, the anaesthetists legal responsibility, and patients views in the preoperative process are
also considered. A thorough clinical preoperative assessment of the patient is more important than routine
preoperative tests, which should be requested only when justified by clinical indications. Moreover, this practice
eliminates unnecessary cost without compromising the safety and quality of care. Education and training of medical
doctors should be more scientifically guided, emphasising the relevance of effectiveness, and cost-effectiveness in
clinical decision-making and complemented by audit.
Preoperative assessment is the clinical investigation that
precedes anaesthesia for surgical or non-surgical
procedures, and is the responsibility of the anaesthetist.
The aims of preoperative assessment are to reduce the
risks associated with surgery and anaesthesia, to increase
the quality (thus decreasing the cost) of peroperative care,
to restore the patient to the desired level of function, and
to obtain the patients informed consent for the
anaesthetic procedure.1 This assessment should rely on
the rational use of information from the patients medical
records, clinical interview, physical examination, and
some additional tests.2 Traditionally, a preoperative
consultation with the anaesthetist has facilitated these
goals. Nevertheless, the process of preoperative
assessment has undergone major changes. The increasing
number of day-case surgery procedures has affected the
way in which the anaesthetist assesses patients
preoperatively. Overuse and unexplained variations of
tests for preoperative assessment have been extensively
documented.312 Although most institutions have
established recommendations for the use of laboratory
tests, information is scarce about the ability of such
guidelines to modify and improve the selection of
preoperative tests. It is important to investigate costeffectiveness and efficiency while providing the best
care.35 This article is an update on recent management
issues in preoperative assessment. Our aims are: (1) To
review and assess the evidence related to the health-care
benefits of preoperative assessment; (2) to offer a
reference framework for the practice of preanaesthetic
assessment; and (3) to stimulate research.
Lancet 2003; 362: 174957
Department of Anaesthesiology and Reanimation, Hospital General
de Segovia, Segovia, Spain (F J Garca-Miguel PhD); and Department
of Planning and Evaluation, Servicio Canario de Salud, Canary
Islands, Spain (P G Serrano-Aguilar PhD, J Lpez-Bastida PhD)
Correspondence to: Dr F J Garca-Miguel, Department of
Anaesthesiology and Reanimation, Hospital General de Segovia,
Crta Avila s/n 40002, Segovia, Spain
(e-mail: fgarcia@hgse.sacyl.es)
Preoperative medical assessment
A preoperative assessment is believed to be a basic
element of anaesthetic care. However, we were unable to
find any controlled trials on the clinical effect of provision
of a preanaesthetic review of medical records, or an
adequate physical examination.2 The aim of assessment of
patients before anaesthesia and surgery is to improve the
outcome, by identifying potential anaesthetic difficulties,
identifying existing medical conditions, improving safety
by assessing and quantifying risk, allowing planning of
peroperative care, providing the opportunity for
explanation and discussion, and allaying fear and anxiety.
Good preoperative assessment will help to reduce costs
and increase efficiency of operative theatre time.13
Search strategy
We searched for trials in MEDLINE, EMBASE, and HealthSTAR
databases. The databases of the UK Centre for Reviews and
Dissemination (DARE and NHS economic evaluation
database) and the Cochrane Collaboration (The Cochrane
Library) were also used. The search included all published
articles regardless of the language. Terms used in the search
were preoperative evaluation, pre-anaesthetic assessment,
preoperative test, surgical risk, and informed consent. All
relevant studies concerning chest radiograph,
electrocardiogram (ECG), laboratory tests, and legal aspects
were retrieved. Information on preoperative test
recommendations for elective surgery in asymptomatic
patients was mainly obtained from systematic reviews
published for International Health Technology Assessment
Agencies.612 To complete the review on the specific topic of
preoperative testing we accepted the work done by Munro
and colleagues6 and by the National Institute for Clinical
Excellence (NICE)12 as the most comprehensive, and we
extended the search strategy used by Munro and colleagues
from 1997 to 2003. The definition used in this paper for
routine preoperative testing is that of tests ordered for
asymptomatic, apparently healthy individuals, in the absence
of any specific clinical indication, to identify conditions
undetected by clinical history and examination.6
THE LANCET Vol 362 November 22, 2003 www.thelancet.com
For personal use. Only reproduce with permission from The Lancet publishing Group.
1749
ANAESTHESIA II
Panel 1: Preoperative questionnaire for adults13
Panel 2: Preoperative questionnaire for children13,23
Have you ever suffered from any of the following? (if yes,
please give details)
Heart disease or any sort
Chest pain, palpitations, or blackouts
High blood pressure
Rheumatic fever
Asthma, bronchitis, or other chest disease
Breathless on exertion at night
Diabetes or sugar in the urine
Kidney or urinary trouble
Convulsions or fits
Anaemia or other blood disorders
Bruising or bleeding problems
Blood clots in the legs or lungs
Jaundice (yellowness)
Indigestion or heartburn
Any other serious illness
1. Has your child had good growth, development, and
exercise tolerance?
2. Has your child been admitted to or frequently attended
hospital?
3. Has your child attended a doctor in the past 4 weeks?
4. Has your child had any of these symptoms in the past
4 weeks: high temperature, rash, cough, cold, sore
throat?
5. Has your child been in contact with an infectious disease
in the past 4 weeks?
6. Does your child have any heart problems?
7. Has your child ever been short of breath while exercising
or been blue around the lips?
8. Does your childs chest ever sound wheezy and whistling?
9. Does your child have any kidney problems?
10. Has your child ever been jaundiced?
11. Does your child bruise easily?
12. Has your child ever had any convulsions or seizures?
13. Does your child, or does anyone in the family, have nerve
or muscle problems?
14. Have your child or family members ever had problems
with anaesthesia?
15. Does your child have any other medical conditions?
16. For female children: has your child started her periods?
If yes, what was the date of her last menstrual period?
17. Is there any chance that your child might be pregnant?
Do you smoke, or you have stopped recently?
(if yes, how many a day?)
Do you drink alcohol (if yes, how much a week?)
Do you have false, capped or crowned teeth?
Do you wear contact lenses or a hearing aid?
Do you have a pacemaker or any implants?
Women
Could you be pregnant?
Are you on the pill or HRT?
What is your approximate weight?
What is your approximate height?
Are you taking any medicines or drugs?
Are you allergic to any drugs or materials?
Please list any previous operations or anaesthetics
Have you, or any member of your family, had any problems
with anaesthetics?
Is there anything else that your anaesthetist or surgeon
should know?
In several studies, specific preoperative outcomes (eg,
cardiac, respiratory) have been reported in patients with
specific pre-existing conditions (eg, hypertension, previous
myocardial infarction, smoking, airway abnormalities).1420
However, since these studies were not controlled trials, they
were not judged to be rigorous enough to provide
unequivocal evidence.
Interview
The preoperative interview is the anaesthetists first
introduction to a patient. This is the most efficient and
productive of the three basic techniques used in
preoperative assessment. The objectives of the interview in
patients who are presumed to be basically healthy is to
detect unrecognised disease that could increase the risk of
surgery above the baseline.21 The preoperative medical
history should focus on the indication for surgical
procedures, allergies, and undesirable side-effects to
medications or other agents, known medical problems,
surgical history, major trauma, and current medications. A
focused review of issues pertinent to the planned anaesthetic
procedures (cardiopulmonary function, homoeostatic
status, possibility of pregnancy, personal or family history of
1750
anaesthetic problems, smoking and drinking habits, and
functional status) has also been shown to be useful.22,23
Questionnaires are an effective way of gleaning basic
background information. Many institutions have developed
questionnaires to improve efficiency in preoperative clinics.
They can be given to the patient at the surgical outpatient
clinic to be completed immediately or taken home and
returned by post. However, questionnaires should not be
seen as a substitute for preoperative interview but as an
additional source of information. The questionnaire is not
supposed to shorten the consultation but to reduce the time
spent asking basic questions, allowing more time to discuss
the actual problem and the operation (panels 1 and 2).13, 2325
Physical examination
A complete physical examination in presumed healthy
individuals includes:2,23 weight and height; main vital signs
blood pressure, pulse (rate and regularity), and respiratory
rate; cardiac and pulmonary examination; anatomical
conditions required for specific anaesthetic procedures,
such as intubation (airway examination), regional
anaesthesia, venous access, etc; and other particular
examinations thought to be of use.
Routine tests
Most patients admitted for elective surgery undergo a range
of routine preoperative tests. These tests, whether or not
guided by the patients clinical needs, have been part of
preoperative clinical practice for many years.7,8,26 The
purposes of routine preoperative testing are: the assessment
of a pre-existing health problem, the identification of
unsuspected medical conditions, the prediction of
preoperative or postoperative complications, the
establishment of a baseline reference for later comparisons,
and the screening of patients opportunistically. This
inappropriate use of resources has been widely
documented,7,2651 especially for the routine chest radiograph,
but besides the small probability of finding a relevant
THE LANCET Vol 362 November 22, 2003 www.thelancet.com
For personal use. Only reproduce with permission from The Lancet publishing Group.
ANAESTHESIA II
SBU7
ANDEM9
OSTEBA8
GR10
NCCHTA6
GPAC11
NICE12
Chest radiography
Electrocardiogram
Immigrants from developing
countries without a chest
radiograph during the
previous 12 months
Immigrants from developing
countries who have not
had a chest radiograph
during the previous
12 months
Men older than 5060 years, When the need for
women older than
transfusions is
6070 years
envisioned
Blood count
Haemostasis
Other analyses
Not recommended
Not indicated
If history suggests risk
of haemorrhage; if not
possible to know the
past history; for special
treatments
The cost-effectiveness
of examination
increases with age,
although the age from
which it must be done
is not clear
If anamnesis suggests
coagulation problems,
difficult surgical
homoeostasis, and for
drinkers of more than
500 mL of wine per
day or equivalent
Immigrants from developing Men and women older
Not recommended routinely
If past history suggests
countries who have not had than 60 years
except in children of younger than haemorrhagic disorders;
a chest radiograph during
1 year of age and patients of non- for treatment with oral
the previous 12 months;
white origin, but recommended for anticoagulants
long-term smokers
surgery in which need for
transfusions is expected
Not indicated
Not indicated
Not indicated
If the anamnesis
suggests homoeostasis
disorders
Not indicated
Not indicated
Not indicated
If the anamnesis
suggests homoeostasis
disorders
Not recommended
Men and women younger
Men and women older than
No recommended
than 60 years if asthmatic or 60 years of age undergoing
smoker. Indicated for those
major surgery.
older than 80 years
Blood urea nitrogen or
creatinine and
glycaemia tests for
people older than
40 years
Men older than 4045 years, Minor surgerydo not do
women older than 55 years
routinely except in patients
younger than 1 year, the elderly,
pregnant women, and immigrants
from developing countries, but
recommended for potentially
haemorrhagic surgery
People older than 60 years; Men and women older than
Not recommended routinely
obese individuals with
60 years; those older than
except in newborns, people older
body-mass index greater
40 years without a previous than 60 years, and fertile women,
than 30; smokers of more
ECG
but recommended for potentially
than 20 cigarettes per day
haemorrhagic surgery (more than
500 mL bloodloss)
Creatinine for persons
over 60 years of age
Not indicated
Not indicated
Renal function in
patients older than
40 years undergoing
a major surgery.
Dipstick urine test in
those older than
16 years
SBU=Swedish Council on Technology Assessment in Health Care. ANDEM=Agence Nationale pour le Developpment de lEvaluation Medicale (France). OSTEBA=Office
for Health Technology assessment (Spain). GR=Health Council of the Netherlands. NCCHTA=National Coordinating Centre for Health Technology assessment (UK).
GPAC=Guidelines and Protocols Advisory Committee (USA). NICE=National Institute for Clinical Excellence (UK).
Indications for preoperative tests for elective surgery in otherwise healthy patients, extracted from systematic reviews
abnormality in the absence of any clinical indication,33,5257
abnormal findings have a surprisingly small effect on
subsequent anaesthetic and surgical management.54,58,59
Drawbacks to the extensive use of routine preoperative
testing are: patients discomfort; unnecessary waiting times
for some procedures; unnecessary direct costs and emerging
opportunity costs; potential for unnecessary subsequent
tests related to false-positive abnormal findings.1,28,60
The evidence suggests that 6070% of preoperative
testing52,61,62 is unnecessary, if a proper history and physical
examination are done.63 Most studies in which the number
of preoperative tests was reduced without adversely
affecting the patients health results have been retrospective.
However, data from some prospective studies48,64 have
confirmed this finding.
Which tests should be ordered preoperatively for elective
surgery? This question, focused on patients with no
symptoms other than those relevant to the planned
operation, has been repeatedly tackled by health technology
assessment agencies since 1989,612 by means of systematic
reviews of published work and, in some cases, by expert
panels or consensus conferences. The UK National
Institute of Clinical Excellence has published a comprehensive review of the evidence on routine preoperative
testing.12 The table shows information about the indications
for preoperative tests in asymptomatic patients.
Because selective ordering of tests, according to the
patients needs, is safer and more efficient for the patient
and the health-care system, some researchers have
investigated the reasons for the internationally widespread
custom of ordering preoperative tests.7,8,26,65,66 A common
reason is protection from legal liability. However, additional
testing does not seem to provide legal protection; in most
retrospective studies a change in management has been
reported in fewer than 5% of patients with abnormal test
findings.54,58,59
Research has been done to obtain information about
attitudes and opinions of anaesthetists about the use of
preoperative assessment tests.7,26,6567 The pioneer study of
the Swedish Council on Technology Assessment in Health
Care from 19897 quantified the high degree of inappropriate
use of preoperative tests for elective surgery. It also obtained
information on the reasons or motives behind the observed
deviations from evidence-based practice through a national
survey of anaesthetists. 60% of participants agreed with the
statement there is no scientific evidence to support
widespread use of chest radiography or ECG in
asymptomatic patients. Studies in Spain26,65,66 and Italy67
had similar findings; about 70% of anaesthetists agreed that
legal liability purposes are among the reasons for most
preoperative tests requested in asymptomatic patients, and
80% of participants rejected, or judged to be doubtful, the
statement that published work supports routine
preoperative testing.
Preoperative risk assessment
Nowadays anaesthesia is safer than it used to be. In a review
of over 100 000 procedures under general and spinal
anaesthesia, patient and surgical risk factors were much
more important than anaesthetic factors in prediction of
7-day mortality.68 The anaesthetist must be aware of any
medical problem of his or her patient, in order to provide
THE LANCET Vol 362 November 22, 2003 www.thelancet.com
For personal use. Only reproduce with permission from The Lancet publishing Group.
1751
ANAESTHESIA II
anaesthesia in the best possible conditions to maximise
safety and comfort.69 The American Society of
Anaesthesiologists classification was the first systematic
attempt to stratify the risk for patients undergoing
anaesthesia. This classification refers to mortality, based
on the general clinical impression of the severity of
systemic illnesses. The anaesthetist is principally
responsible for choosing a particular anaesthetic
technique or agent, and the selection should be based on
the type of procedure to be undertaken and on the specific
needs and risks of the patient. 69
General versus regional anaesthesia
The decision whether to apply general or regional
anaesthesia is a matter of great debate. Early data
suggested that mortality did not differ between the two
approaches.69,70 However, these studies often did not
include the postoperative period, and did not take into
account other outcomes such as time to discharge, patient
satisfaction, and time taken by the anaesthetist. Regional
anaesthetic techniques have now been improved, so older
studies may no longer be valid.69 Most studies comparing
epidural and general anaesthesia have not been adequately
designed to detect clinical differences, since the incidence
of events was low and small numbers of patients were
investigated. Nevertheless, these studies can make us
aware of any potential differences and how they affect our
decisions about the type of anaesthesia to apply.7174
Results of a meta-analysis including 141 trials and
9559 patients showed that epidural or spinal anaesthesia
reduced mortality, risk of myocardial infarction,
transfusion requirements, incidence of pneumonia, and
respiratory
depression,
compared
with
general
anaesthesia.75 Epidural anaesthesia also reduces the risk of
venous thromboembolism and the likelihood of a
thrombophilic
state,
compared
with
general
anaesthesia.7680 The precise mechanism for this reduction
of risk is not clear. Epidural anaesthesia decreases
intraoperative loss of blood, presumably because of a
reduction in arterial blood pressure and a redistribution of
bloodflow. Additionally, elimination of the need for
positive pressure ventilation reduces venous backpressure
into the surgical field. Finally, sympathetic blockade
results in increased bloodflow to the legs and feet.
Cardiac risk
The overall risk of postoperative cardiac death or major
cardiac complications is less than 6% in patients older
than 40 years undergoing major non-cardiac
operations.8182 However, the risk is not uniform, but is
increased by old age and pre-existing heart disease. The
best approach is to identify patients at high risk so that
appropriate testing and therapeutic measures can be
undertaken to reduce or eliminate the risk.83 Several
multivariate indices of risk have been developed for
patients with known or suspected cardiac disease. All
seem to be similar in their ability to predict cardiac
problems during the operation.8487
In 2002, the American College of Cardiology and the
American Heart Association jointly updated the practice
guidelines on perioperative cardiovascular assessment for
non-cardiac surgery.88 These guidelines incorporate
clinical predictors and functional status into the
preoperative risk assessment algorithm, and show how this
assessment can best be undertaken without submitting the
patient to unnecessary interventions. They emphasise that
preoperative testing should be restricted to circumstances
in which the results will affect management and outcome.
The estimation of preoperative risk should integrate
1752
Panel 3: Similarities and differences between
guidelines of the American College of
Cardiology/American Heart Association
(ACC/AHA) and the American College of
Physicians (ACP)
Similarities
Emergency surgery cases proceed directly to the operating
room without further risk stratification
Both algorithms incorporate Detsky predictors86*
Patients eventually placed into low, intermediate, or high risk
categories
Differences
ACC/AHA preoperative guideline
Presence or absence of coronary artery disease is the
first risk assessment
Clinical predictors derived from Goldman82 and Detsky86
criteria
Patients with poor functional status require stress testing
ACP preoperative guideline
Destky criteria are the first determinants of risk
stratification
Minor clinical predictors derived from Eagle87 and
Vanzetto20 criteria
ACP felt functional status not proved to be useful risk
predictor
Patients undergoing vascular surgery require stress
testing
Adapted with permission from Karnath.90 *Detsky and colleagues
reported ten variables associated with an increased risk for
perioperative cardiac complications in patients undergoing noncardiac
surgery (age older than 70 years, myocardial infarction after 6 months,
etc). Each risk factor was assigned a point score, and patients are
stratified into three risk categories based on their total score.
clinical determinants of risk: those who have had coronary
revascularisation in the previous 5 years, or a favourable
result of either coronary angiography or cardiac stress test
in the preceding 2 years, may be submitted to surgery
without further cardiac assessment. The American
College of Physicians has also published guidelines for
assessment and management of perioperative risk.89 Both
sets of preoperative guidelines are evidence-based.
Similarities and differences between the guidelines are
outlined in panel 3.
Pulmonary risk
Postoperative lung complications contribute substantially
to overall peroperative morbidity and mortality.
Pulmonary complications occur significantly more often
than cardiac complications and are associated with
significantly longer hospital stays.91,92 One broad definition
of postoperative lung complication includes an
identifiable disease or dysfunction that is clinically
relevant and adversely affects the clinical course.9396 This
classification would include several major problems such
as atelectasis, infection (bronchitis and pneumonia),
prolonged mechanical ventilation, respiratory failure,
exacerbation of underlying chronic lung disease, and
bronchospasm.
Risk factors for pulmonary complications can be
grouped as patient-related or procedure-related.
Patient-related factors
Chronic lung disease is the most important patient-related
risk factor for postoperative pulmonary complicationsit
increases the risk of postoperative complications 26 to
THE LANCET Vol 362 November 22, 2003 www.thelancet.com
For personal use. Only reproduce with permission from The Lancet publishing Group.
ANAESTHESIA II
6 fold.17,88 Patients with asthma that is well controlled and
with a peak flow measurement of greater than 80% of that
predicted can proceed to surgery with an average risk.97
Current cigarette smokers have an increased risk for
postoperative pulmonary complications, even in the
absence of chronic lung disease. Smokers of more than
20 packs per year have a higher incidence of postoperative
pulmonary complications than those smoking fewer
cigarettes (rate of complications varied from 155% to
55%).98 The relative risk of pulmonary complications in
smokers is four times higher than in people who have not
smoked within the past 2 months.91
Changes related to morbid obesity can accentuate and
increase the risk of postoperative pulmonary
complications. However, there is a clear discrepancy
between different reports. Differences may arise, in part,
because many studies do not adequately distinguish
between obesity itself and comorbid conditions. Despite
controversy, a balanced interpretation of the evidence
suggests that obesity is not a risk factor for postoperative
pulmonary complications and should not affect patient
selection for otherwise high-risk procedures.91,99
The risk due to age alone, once corrected for
comorbidities, seems small, although data are
conflicting.100102
Surgery-related factors
The site of surgery is the most important factor in
predicting the overall risk of postoperative pulmonary
complications. The rate of complications is inversely
related to the distance of the surgical incision from the
diaphragm. Thus, the rate is substantially higher for
thoracic and upper abdominal surgery (1959% and
1617%, respectively) than for lower abdominal surgery
(05%).92,95,101,103
Surgical procedures lasting longer than 34 h are
associated with an increased risk of pulmonary
complications.100,101,104,105 General anaesthesia seems to be
associated with a higher risk of clinically important
pulmonary complications than epidural or spinal
anaesthesia. Regional nerve block is associated with
reduced risk, and should be considered, if possible, for
patients at high risk.75,95,105,106
Preoperative fasting policies
Restricted intake of food and oral fluid before general
anaesthesia has for a long time been judged vital, to
reduce the risk of regurgitation of the gastric contents.
However, preoperative fasting can impair nutrition and
hydration. Anaesthetists concerned with the well-being,
hydration, comfort, and safety of their patient try to
establish safe periods of preoperative fasting without
unnecessary starvation.107,108 Several unsystematic reviews
of the literature109114 have suggested that an overly long
fasting period (such as the traditional nothing by mouth
from midnight) might be unnecessary or even
detrimental to the patient. Any re-assessment of our
fasting policy should be welcome. A number of
associations have published new or revised guidelines
dealing with preoperative fasting inpatients undergoing
elective surgery.108111,113,114 The most comprehensive report
was published in 1999 by the American Society of
Anaesthesiologists,115 which recommended that adults
should have no clear fluids for at least 2 h, and should
take their last light meal at least 6 h before having surgery
with general anaesthesia, regional anaesthesia, or sedation
or analgesia. The routine use of gastrointestinal stimulants
to decrease the risk of pulmonary aspiration in otherwise
healthy patients was discouraged.
Children have specific preoperative needs.116,117 Infants
need regular feeding in the form of breastmilk, non-human
milk, or infant formula to prevent hunger, thirst,
hypoglycaemia, dehydration, and discomfort. As a group,
the nutritional needs of children are heterogeneous. For
instance, neonates (<1 month) are different from infants
(1 month to 1 year) and, similarly, the needs of the older
child (>1 year) are different from those of younger
children. Guidelines published by the American Society of
Anaesthesiologists recommend a 6 h fast for non-human
milk or infant formulae for neonates and infants, and a less
strict 4 h policy for breastmilk feeding, before procedures
requiring general anaesthesia, regional anaesthesia, or
monitored anaesthetic care.
Patients perspective
The anaesthetists preoperative consultation with the
patient is important to enhance trust and confidence. The
patient should know the anaesthetists name and status. If
the anaesthetist is still in training, the patient will want to
know that his or her levels of competence and experience
are appropriate, and that a senior specialist will be at
hand.13 The preoperative anaesthetic clinic is the place and
time to assess the patients fitness for surgery as well as to
discuss the most appropriate anaesthetic technique in the
light of the patients preferences, clinical state, the
operation itself, and the anaesthetists preferences and
special skills.13,118 This is also the time to help the patient
raise any doubts and questions about aspects of anaesthetic
care, and to obtain the patients explicit consent to what is
agreed. Discussion between anaesthetist and patient
should include how the patient will get to the theatre, if
there is a choice; what will be experienced in the recovery
room, or in ICU, if that is planned; what time the
operation is scheduled, with a prompt explanation if the
time slips; whether a blood transfusion is likely to be given;
how postoperative and postdischarge pain will be managed
and what choices there might be. If the patient is to wake
up with an epidural catheter or a patient-controlled
analgesia machine, intravenous line, oxygen mask, etc,
those too must be explained.3,23
Patients prefer to be seen preoperatively by the same
anaesthetist who will later anaesthetise them.118 Most
anaesthetists agree, and this practice is deemed to be a
marker of high-quality anaesthesia by the UK Association
of Anaesthetists.119,120 Finally, a postoperative visit, however
brief, by the anaesthetist, completes the patients
perception of good quality of care.
Legal issues
As far as medical responsibility is concerned, no specific
rules can be formulated, neither for anaesthetists or any
other medical specialists, nor for the different medical
acts. In October, 1987, the US Congress approved the
duties of preanaesthetic care (last modified in October,
1993), stating that the anaesthetist has a responsibility to
determine the medical condition of the patient, to develop
a plan of anaesthetic care, and to inform the patient or
guardian of this plan. These principles apply to all patients
who are going to undergo anaesthesia or a monitored
anaesthetic procedure121 and can only be modified in
special circumstances, such as an extreme emergency. The
specifications state that preoperative screening tests are
usually useful, but no systematic tests are required for
the pre-anaesthetic assessment.121 Anaesthetists, the
anaesthetic department, and medical institutions should
develop scientifically based guidelines to define the tests to
be used preoperatively. The probable contribution of each
test to the final result of surgery should be assessed
THE LANCET Vol 362 November 22, 2003 www.thelancet.com
For personal use. Only reproduce with permission from The Lancet publishing Group.
1753
ANAESTHESIA II
individually. Every anaesthetist should, additionally, ask
for any specific tests, the results of which could affect, in
his or her opinion, the decisions to take, the risks involved,
and the ways to control the anaesthesia and surgery in
every individual case.
In France, a 1974 government circular established the
preoperative anaesthetic consultation as compulsory; the
assessment must be summarised in a preoperative report,
and done far enough in advance to allow time for all the
necessary complementary tests.122
In other countries, there are no similarly defined
regulations. In Spain, failure to do adequate preoperative
tests is judged, in view of recent court cases, to be serious
negligence, unless surgery is urgent and vital. Biochemical
and haematological tests, radiography, and an electrocardiogram have been judged, in legal cases, to be
necessary to show the true condition of the patient and to
eliminate, or at least diminish, the likelihood of treatment
failure or death.123 However, as previously mentioned,
there is much evidence that routine preoperative testing is
done, not for clinical reasons, but to prevent possible legal
claims by the patients.5
Cost of routine preoperative assessment
The broad use of routine preoperative tests generates costs
in several ways: the cost of the tests, the cost of follow-up
tests to ascertain the importance of any abnormal findings,
the need for additional consultations, and delays in
surgery.1 The costs are not negligible, and can be
substantially reduced through appropriate selective
ordering of preoperative diagnostic tests. Economic
analyses on preoperative assessment have been undertaken
in Sweden, Spain, the UK, and the USA,7,8,49,124,125 reaching
estimates of savings that could be achieved if evidencebased protocols were implemented. In Sweden the annual
costs generated by preoperative investigations were
estimated to be 726 million Swedish crowns (SEK),
including one inpatient day in 75% of all patients
undergoing surgery. With restricted criteria for
preoperative investigations, the potential savings in the
long term were calculated as SEK 100200 million per
year in 1989 (or roughly $167 000$334 000).7 In Spain
(Basque Country, 1992), the potential estimated reduction
in yearly costs of preoperative testing, according to
different uses of a scientific based protocol8 for healthy
patients needing elective surgery, was US$286 million in
1998.126 The same procedure, applied to healthy patients
undergoing elective surgery in the regional public health
system of the Canary Islands, Spain, estimated a potential
cost reduction of 213324 million in 2000 (equivalent
to $226344 million).124 Investigators from a local study
in the UK estimated conservatively that 50 000 ($83 000)
could be saved per year;49 extrapolation to all hospitals in
the National Health Service could result in savings of
several million pounds. In the USA, it has been estimated
that by ordering no laboratory tests except those indicated
by the history or physical examination, almost $100 could
be saved per patient. Since 29 million patients undergo
some form of surgical procedure annually in USA, about
$29 billion dollars could be saved in total.125 Evidence
suggests that the number of preoperative tests in hospitals
could be reduced without affecting patients outcomes,
and with substantial concomitant reduction in costs.
involvement in making decisions. Information technologies
are powerful instruments for bringing information to
patients and citizens. However, these issues also raise
questions: who is going to lead the processclinicians,
public or patients, health-care administrators, or other
institutions? Who will facilitate the cost-effective selection
of preoperative tests?
Second, there is a strong need for improvement and
increase in research and audit about preoperative
assessment. As NICE pointed out in their recent
publication,12 there is no empirical evidence for the benefits
of preoperative testing in the healthy or asymptomatic
population, since there are few comparative studies on
alternative strategies for testing. Meanwhile, the costs and
results of alternative strategies for preoperative testing
could be monitored in different groups of patients. If
safety, effectiveness, and cost-effectiveness are going to be
the leading principles in decision-making in preoperative
testing, research is needed to identify the best test strategy
and the best methods in every surgical condition. The poor
quality of study design, execution, and reporting also limit
the validity and usefulness of the available noncomparative studies. We propose that future research
projects should include a prospective case-series
investigating the effect on clinical management of routine
testing in patients older than 60 years, and a randomised
trial of outcomes and costs, etc, in patients who do or do
not have the full set of routine preoperative tests. Further
analysis of the existing evidence could include: estimates of
the predictive values or likelihood ratios for different tests
in respect of postoperative events, from studies that
contain adequate data; meta-analysis of pooled results
from existing studies and economic modelling of the
probable resource costs and patients outcomes in current
practice, by use of best estimates of test performance.
Professional societies should take the initiative to
implement and assess a continuing education system that
would effectively bring updated scientific information to
clinicians, allowing them to improve their knowledge and
use the results of research. However, the complexity of
medical decision-making on this topic means that we need
more than better research, education, training, and
scientific based guidelines. How do we address the issues
of fear and the practice of defensive medicine, and the
need for a comprehensive strategy to bring together
scientific societies, health-care administrators, public
representatives, and judicial organisations?
We thank Diego Reverte and Eduardo Tello for their valuable assistance
in the preparation of this manuscript
Conflict of interest statement
None declared.
References
1
2
3
4
5
The future
First, the public and patients are willing to play a more
active role in the decision-making process on their own
health.127129 Some health-care systems are working to
empower citizens and patients to improve the value of their
1754
Roizen MF. More preoperative assessment by physicians and less
by laboratory tests. N Engl J Med 2000; 342: 20405.
American Society of Anesthesiologists Task Force on Preanesthesia
Evaluation. Practice advisory for preanesthesia evaluation: a report
by the American Society of Anesthesiologists Task Force on
Preanesthesia Evaluation. Anesthesiology 2002; 96: 48596.
Myers LM. Preoperative evaluation. Florida: Jacksonville Medicine,
1998.
Lundberg D, Hgerdal M. Pre-anaesthetic assessment.
Acta Anaesthesiol Scand 1996; 40: 961.
Roizen MF. What is necessary for preoperative patient assessment?
In: Barash PG, Deutsch S, Tinker J, eds. The American Society
of Anesthesiologists. Philadelphia: Lippincott-Raven, 1995:
189202.
Munro J, Booth A, Nicholl J. Routine preoperative testing: a
systematic review of the evidence. Southampton: National
Coordinating Centre for Health Technology Assessment, 1997.
THE LANCET Vol 362 November 22, 2003 www.thelancet.com
For personal use. Only reproduce with permission from The Lancet publishing Group.
ANAESTHESIA II
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
The Swedish Council on Technology Assessment in Health Care
(SBU). Preoperative routines. Stockholm: SBU, 1989.
Office for Health Technology Assessment (OSTEBA).
Healthy/asymptomatic patient preoperative evaluation. VictoriaGasteiz: Health Department, 1994.
Agence Nationale pour le Development de lEvaluation Medicale
(ANDEM). Indication of Preoperative Tests. Paris: ANDEM, 1992.
Health Council of the Netherlands, Gezondheidsraad (GR).
Preoperative Evaluation. Den Haag: Gezondheidsraad, 1997.
Guidelines and Protocols Advisory Committee (GPAC), Medical
Services Commission, and British Columbia Medical Association.
Guideline for Routine Pre-Operative Testing. Victoria BC: Ministry
of Health, 2000.
National Institute for Clinical Excellence (2003) Guidance on the use
of preoperative tests for elective surgery. NICE Clinical Guideline
No 3. London: National Institute for Clinical Excellence, 2003.
The association of Anaesthetists of Great Britain and Ireland.
Pre-operative assessment. The role of the anaesthetist.
http://www.aagbi.org/pdf/pre-operative_ass.pdf (accessed Nov 10,
2003)
Duncan PG, Cohen MM. Postoperative complications: factors of
significance to anaesthetic practice. Can J Anaesth 1987; 34: 28.
Eagle KA, Brundage BH, Chaitman BR, et al. Guidelines for
perioperative cardiovascular evaluation for noncardiac surgery: report
of the American College of Cardiology/ American Heart Association
Task Force on Practice Guidelines (Committee on Perioperative
Cardiovascular Evaluation for Noncardiac Surgery). J Am Coll Cardiol
1996; 27: 91048.
Forrest JB, Rehder K, Cahalan MK, Goldsmith CH. Multicenter
study of general anesthesia. III. Predictors of severe perioperative
adverse outcomes. Anesthesiology 1992; 76: 315.
Kroenke K, Lawrence VA, Theroux JF, Tuley MR, Hilsenbeck S.
Postoperative complications after thoracic and major abdominal
surgery in patients with and without obstructive lung disease. Chest
1993; 104: 144551.
American Academy of Pediatrics. Evaluation and preparation of
pediatric patients undergoing anesthesia (RE9633). Pediatrics 1996;
98: 50208.
Lawrence VA, Dhanda R, Hilsenbeck SG, Page CP. Risk of
pulmonary complications after elective abdominal surgery. Chest
1996; 110: 74450.
Vanzetto G, Machecourt J, Blendea D, et al. Additive value of
thallium single-photon emission computed tomography myocardial
imaging for prediction of perioperative events in clinically selected
high cardiac risk patients having abdominal aortic surgery.
Am J Cardiol 1996; 77: 14348.
Smetana GW. Preoperative medical evaluation of the healthy patient
(Up To Date Review). Up To Date 2002; 10: N3.
http://www.uptodate.com (accessed Jan 30, 2003).
Arvidsson S, Ouchterlony J, Nilsson S, Sjstedt L, Svrdsudd K. The
Gothenburg study of preoperatory risk. I. Preoperative findings,
postoperative complications. Acta Anaesthesiol Scand 1994; 38:
67990.
Institute for Clinical Systems Improvement. Health Care Guideline:
Preoperative evaluation. Bloomington: Institute for Clinical Systems
Improvement, 2002.
Alcalde J, Ruiz P, Acosta F, Landa JI, Jaurrieta E. Proyecto para la
elaboracin de un protocolo de evaluacin preoperatoria en ciruga
programada. Cir Esp 2001; 69: 58490.
Ladfors MB, Lofgren MEO, Gabriel B, Olsson JHA. Patient accept
questionnaires integrated in clinical routinea study by the Swedish
National Register of Gynecological Surgery. December 2001.
Acta Obstet Gynecol Scand 2002; 81: 43742.
Serrano Aguilar P, Lpez Bastida J, Duque Gonzlez B, et al.
Preoperative testing routines for healthy, asymptomatic patients in the
Canary Islands (Spain). Rev Esp Anestesiol Reanim 2001; 48: 30713.
Kerr IH. Preoperative chest x ray. Br J Anaesth 1974; 46: 55863.
Sagel SS, Evens RG, Forrest JV. Efficacy of routine screening and
lateral chest radiographs in a hospital based population. N Engl J Med
1974: 291; 100104.
Seymour DC, Pringle R, Shaw JW. The role of the routine preoperative chest x-ray in the elderly general surgical patient.
Postgrad Med J 1982; 58: 74145.
Rees AM, Roberts CJ, Bligh AS, Evans KT. Routine preoperative
chest radiography in non-cardiopulmonary surgery. BMJ 1976; 1:
133335.
Sane SM, Worsing RA Jr, Wiens CW, Sharma RK. Value of
preoperative chest X-ray examinations in children. Pediatrics 1977; 60:
66972.
Umbach GE, Zubek S, Deck HJ, Buhl R, Bender HG, Jungblut RM.
The value of preoperative chest X-rays in gynecological patients.
Arch Gynecol Obstet 1988; 243: 17985.
33 Adams JG Jr, Weigelt JA, Poulos E. Usefulness of preoperative
laboratory assessment of patients undergoing elective herniorrhaphy.
Arch Surg 1992; 127: 80104.
34 MacDonald JB, Dutton MJ, Stott DJ, Hamblen DL. Evaluation of
pre-admission screening of elderly patients accepted for major joint
replacement. Health Bull Edinb 1992; 50: 5460.
35 Ramsey G, Arvan DA, Stewart S, Blumberg N. Do preoperative
laboratory tests predict blood transfusion needs in cardiac operations?
J Thorac Cardiovasc Surg 1983; 85: 56469.
36 Jones MW, Harvey IA, Owen R. Do children need routine
preoperative blood-tests and blood cross matching in orthopedic
practice. Ann R C Surg Engl 1989; 71: 13.
37 Kozak EA, Brath LK. Do screening coagulation tests predict bleeding
in patients undergoing fiberoptic bronchoscopy with biopsy? Chest
1994; 106: 70305.
38 Manning SC, Beste D, McBride T, Goldberg A. An assessment of
preoperative coagulation screening for tonsillectomy and
adenoidectomy. Int J Pediatr Otorhinolaryngol 1987; 13: 23744.
39 Aghajanian A, Grimes DA. Routine prothrombin time determination
before elective gynecologic operations. Obstet Gynecol 1991; 78:
83739.
40 Bouillot JL, Fingerhut A, Paquet JC, Hay JM, Coggia M. Are routine
preoperative chest radiographs useful in general surgery? A
prospective, multicentre study in 3959 patients. Association des
Chirurgiens de lAssistance Publique pour les Evaluations medicales.
Eur J Surg 1996; 162: 597604.
41 Lavernia CJ, Hernandez RA, Rodriguez JA. Perioperative X-rays in
arthroplasty surgery: outcome and cost. J Arthroplasty 1999; 14:
66971.
42 Garca-Miguel FJ, Garca Caballero J, Gmez de Caso-Canto JA.
Indications for thoracic radiography in the preoperative evaluation for
elective surgery. Rev Esp Anestesiol Reanim 2002; 49: 8088.
43 Garca-Miguel FJ, Garca Caballero J, Gmez de Caso-Canto JA.
Indications for electrocardiogram in the preoperative assessment for
programmed surgery. Rev Esp Anestesiol Reanim 2002; 49: 512.
44 Escolano F, Gomar C, Alonso J, Sierra P, Cabrera JC, Castao J.
Usefulness of the preoperative electrocardiogram in elective surgery.
Rev Esp Anestesiol Reanim 1996; 43: 30509.
45 Silvestri L, Maffessanti M, Gregori D, Berlot G, Gullo A. Usefulness
of routine pre-operative chest radiography for anaesthetic
management: a prospective multicentre pilot study. Eur J Anaesthesiol
1999; 16: 74960.
46 Murdoch CJ, Murdoch DR, McIntyre P, Hosie H, Clark C. The preoperative ECG in day surgery: a habit? Anaesthesia 1999; 54: 90708.
47 Liu LL, Dzankic S, Leung JM. Preoperative electrocardiogram
abnormalities do not predict postoperative cardiac complications in
geriatric surgical patients. J Am Geriatr Soc 2002; 50: 118691.
48 Schein OD, Katz J, Bass EB, et al. The value of routine preoperative
medical testing before cataract surgery. N Engl J Med 2000; 342:
16875.
49 Johnson RK, Mortimer AJ. Routine pre-operative blood testing: is it
necessary? Anaesthesia 2002; 57: 91417.
50 Alsumait BM, Alhumood SA, Ivanova T, Mores M, Edeia M. A
prospective evaluation of preoperative screening laboratory tests in
general surgery patients. Med Princ Pract 2002; 11: 4245.
51 Ansermino JM, Than M, Swallow PD. Pre-operative blood tests in
children undergoing plastic surgery. Ann R Coll Surg Engl 1999; 81:
17578.
52 Kaplan EB, Sheiner LB, Boeckmann AJ. The usefulness of
preoperative laboratory screening. JAMA 1985; 253: 357681.
53 Narr BJ, Hansen TR, Warner MA. Preoperative laboratory screening
in healthy Mayo patients: cost effective elimination of tests and
unchanged outcomes. Mayo Clin Proc 1991; 66: 15559.
54 Tape TG, Mushlin AI. How useful are routine chest x-rays of 55
preoperative patients at risk for postoperative chest disease?
J Gen Intern Med 1988; 3: 1520.
55 Rucker L, Frye EB, Staten MA. Usefulness of screening chest
roentgenograms in preoperative patients. JAMA 1983; 250: 320911.
56 Mendelson DS, Khilnani N, Wagner LD, Rabinowitz JG.
Preoperative chest radiography: value as a baseline examination for
comparison. Radiology 1987; 165: 34143.
57 Gagner M, Chiasson A. Preoperative chest X-ray films in elective
surgery: a valid screening tool. Can J Surg 1990; 33: 27174.
58 Turnbull JM, Buck C. The value of preoperative screening
investigations in otherwise healthy individuals. Arch Intern Med 1987;
147: 110105.
59 Johnson H Jr, Knee-Ioli S, Butler TA, Muoz E, Wise L. Are routine
preoperative laboratory screening tests necessary to evaluate
ambulatory surgical patients? Surgery 1988; 104: 63945.
60 Loder RE. Routine preoperative chest radiography. 1977 compared
with 1955 at Peterborough District General Hospital. Anaesthesia
1978; 33: 97274.
THE LANCET Vol 362 November 22, 2003 www.thelancet.com
For personal use. Only reproduce with permission from The Lancet publishing Group.
1755
ANAESTHESIA II
61 Macario A, Roizen MF, Thisted RA, Kim S, Orkin FK, Phelps C.
Reassessment of preoperative laboratory testing has changed the
test ordering pattern of physicians. Surg Gynecol Obstet 1992; 75:
53947.
62 Velanovich V. The value of routine preoperative laboratory testing in
predicting postoperative complications: a multivariate analysis.
Surgery 1991; 109: 23643.
63 Roizen MF, Foss JF, Fischer SP. Preoperative evaluation. In:
Miller RD, ed. Anesthesia. 5th edn. Philadelphia: Churchill
Livingstone, 2000: 82483.
64 Narr BJ, Warner ME, Schroeder DR, Warner MA. Outcomes of
patients with no laboratory assessment before anaesthesia and a
surgical procedure. Mayo Clin Proc 1997; 72: 50509.
65 Vilarasau J, Farr M, Martn-Baranera, Oliva G. Survey of
preoperative assessment practices in Catalonia (I). What protocols are
being followed? Rev Esp Anestesiol Reanim 2001; 48: 410.
66 Oliva G, Vilarasau Farr J, Martn-Baranera M. Survey of
preoperative assessment practices in Catalonia (II). How do the
anesthesiologists and surgeons involved view current practice?
Rev Esp Anestesiol Reanim 2001; 48: 1116.
67 Ricciardi G, Angelillo IF, Del Prete U, et al. Routine preoperative
investigation. Results of a multicenter survey in Italy.
Int J Technol Assess Health Care 1998; 14: 52634.
68 Cohen MM, Duncan PG, Tate RB. Does anesthesia contribute to
perioperative mortality? JAMA 1988; 260: 285963.
69 Kaboli PJ, Wilson S, Steven Hata J. Anesthesia techniques and their
impact on perioperative management (Up To Date Review). Up
To Date 2002; 10: N3. http://www.uptodate.com (accessed Jan 30,
2003).
70 Davis FM, Woolner DF, Frampton C, et al. Prospective multicentre trial of mortality following general or spinal anaesthesia
for hip fracture surgery in the elderly. Br J Anaesth 1987; 59:
108088.
71 Tuman KJ, McCarthy RJ, March RJ, De Laria GA, Patel RV,
Ivanovich AD. Effects of epidural anesthesia and analgesia on
coagulation and outcome after major vascular surgery. Anesth Analg
1991; 73: 696704.
72 Christopherson R, Beatti C, Frank SM, Norris EJ, Meinert CL,
Gottlieb SO. Perioperative morbidity in patients randomized to
epidural or general anesthesia for lower extremity vascular surgery.
The Perioperative Ischemia Randomized Anesthesia Trial Study
Group. Anesthesiology 1993; 79: 42234.
73 Bode RH Jr, Lewis KP, Zarich SW, et al. Cardiac outcome after
peripheral vascular surgery. Comparison of general and regional
anesthesia. Anesthesiology 1996; 84: 313.
74 Baron JB, Bertrand M, Barr E, et al. Combined epidural and general
anesthesia versus general anesthesia for abdominal aortic surgery.
Anesthesiology 1991; 75: 61118.
75 Rodgers A, Walker N, Schug S, et al. Reduction of postoperative
mortality and morbidity with epidural or spinal anaesthesia:
results from overview of randomised trials. BMJ 2000; 321:
149396.
76 Modig J, Borg T, Karlstrom G, Maripuu E, Sahlstedt B.
Thromboembolism after total hip replacement: role of epidural and
general anesthesia. Anesth Analg 1983; 62: 17480.
77 Mitchell D, Friedman RJ, Baker JD 3rd, Cooke JE, Darcy MD,
Miller MC 3rd. Prevention of thromboembolic disease following total
knee arthroplasty. Epidural versus general anesthesia. Clin Orthop
1991; 269: 10912.
78 Nielsen PT, Jorgensen LN, Albrecht-Beste E, Leffers AM,
Rasmussen LS. Lower thrombosis risk with epidural blockade in knee
arthoplasty. Acta Orthop Scand 1990; 61: 2931.
79 Sorenson RM, Pace NL. Anesthetic techniques during surgical repair
of femoral neck fractures. A metaanalysis. Anesthesiology 1992; 77:
1095104.
80 Prins MH, Hirsh J. A comparison of general anesthesia and regional
anesthesia as a risk factor for deep vein thrombosis following hip
surgery: a critical review. Thromb Haemost 1990; 64: 497500.
81 Joffe II, Morgan JP. Estimation of coronary risk before noncardiac
surgery (Up To Date Review). Up To Date 2002; 10: N3.
http://www.uptodate.com (accessed Jan 30, 2003).
82 Goldman L, Caldera DL, Nussbaum SR, et al. Multifactorial index of
cardiac risk in noncardiac surgical procedures. N Engl J Med 1977;
297: 84550.
83 Shammash JB, Mohler ER, Kimmel SE. Management of high-risk
patients with vascular disease prior to major noncardiac surgery (Up
To Date Review). Up To Date 2002; 10: N3.
http://www.uptodate.com (accessed Jan 30, 2003).
84 Gilbert K, Larocque BJ, Patrick LT. Prospective evaluation of cardiac
risk indices for patients undergoing noncardiac surgery.
Ann Intern Med 2000; 133: 35659.
85 Lee TH, Marcantonio ER, Mangione CM, et al. Derivation and
1756
prospective validation of a simple index for prediction of cardiac risk
of major noncardiac surgery. Circulation 1999; 100: 104349.
86 Younis LT, Miller DD, Chaitman BR. Preoperative strategies to
assess cardiac risk before noncardiac surgery. Clin Cardiol 1995; 18:
44754.
87 Eagle KA, Coley CM, Newell JB, et al. Combining clinical and
thallium data optimizes preoperative assessment of cardiac risk before
major vascular surgery. Ann Intern Med 1989; 110: 85966.
88 Eagle KA, Berger PB, Calkins H, et al. ACC/AHA guideline update
for perioperative cardiovascular evaluation for noncardiac surgery:
executive summary: a report of the American College of
Cardiology/American Heart Association Task Force on Practice
Guidelines (Committee to Update the 1996 Guidelines on
Perioperative Cardiovascular Evaluation for Noncardiac Surgery).
J Am Coll Cardiol 2002; 39: 54253.
89 Guidelines for assessing and managing the perioperative risk from
coronary artery disease associated with major noncardiac surgery.
American College of Physicians. Ann Intern Med 1997; 127:
30912.
90 Karnath BM. Preoperative cardiac risk assessment. Am Fam Physician
2002; 66: 188996.
91 Smetana GW. Evaluation of preoperative pulmonary risk. (Up To
Date Review). Up To Date 2002; 10: N3. http://www.uptodate.com
(accessed Jan 30, 2003).
92 Mohr DN, Jett JR. Preoperative evaluation of pulmonary risk factors.
J Gen Intern Med 1988; 3: 27787.
93 ODonohue WJ. Postoperative pulmonary complications: When are
preventive and therapeutic measures necessary? Postgrad Med 1992;
91: 16770.
94 Hall JC, Tarala MD, Hall JL, Mander J. A multivariate analysis of the
risk of pulmonary complications after laparotomy. Chest 1991; 99:
92327.
95 Gracey DR, Divertie MB, Didier EP. Preoperative pulmonary
preparation of patients with chronic obstructive pulmonary disease; a
prospective study. Chest 1979; 76: 12329.
96 Smetana GW. Preoperative pulmonary evaluation. N Engl J Med
1999; 340: 93744.
97 Warner DO, Warner MA, Barnes RD, et al. Perioperative respiratory
complications in patients with asthma. Anesthesiology 1996; 85:
46067.
98 Warner MA, Offord KP, Warner ME, Lennon RL, Conover MA,
Jansson-Schumacher V. Role of preoperative cessation of smoking
and other factors in postoperative pulmonary complications: a blinded
prospective study of coronary artery bypass patients. Mayo Clin Proc
1989; 64: 60916.
99 Pasulka PS, Bistian BR, Benotti PN, Blackburn GL. The risks of
surgery in obese patients. Ann Intern Med 1986; 104: 54046.
100 Kroenke K, Lawrence VA, Theroux JF, Tuley MR. Operative risk in
patients with severe obstructive pulmonary disease. Arch Intern Med
1992; 152: 96771.
101 Moller AM, Maaloe R, Pedersen T. Postoperative intensive care
admittance: the role of tobacco smoking. Acta Anesthesiol Scand 2001;
45: 34548.
102 Thomas DR, Ritchie CS. Preoperative assessment of older adults.
J Am Geriatr Soc 1995; 43: 81121.
103 Arozullah AM, Daley J, Henderson WG, Khuri SF. Multifactorial risk
index for predicting postoperative respiratory failure in men after
major noncardiac surgery. The National Veterans Administration
Surgical Quality Improvement Program. Ann Surg 2000; 232:
24253.
104 Brooks-Brunn JA. Predictors of postoperative pulmonary
complications following abdominal surgery. Chest 1997; 111:
56471.
105 Celli BR, Rodrguez KS, Snider GL. A controlled trial of intermittent
positive pressure breathing, incentive spirometry, and deep breathing
exercises in preventing pulmonary complications after abdominal
surgery. Am Rev Respir Dis 1984; 130: 1215.
106 Yeager MP, Glass DD, Neff RK, Brinck-Johnsen T. Epidural
anesthesia and analgesia in high-risk surgical patients. Anesthesiology
1987; 66: 72936.
107 Brady M, Kinn S, Stuart P. Preoperative fasting for adults (protocol
for a Cochrane review). In: The Cochrane Library, Issue 3, 2001.
Oxford: Update Software.
108 Lpez-Muoz AC, Toms Braulio J, Montero R. Guidelines for
preoperative fasting and premedication to reduce the risk of
pulmonary aspiration. Rev Esp Anestesiol Reanim 2002; 49:
31423.
109 Kallar SK, Everett LL. Potential risks and preventive measures for
pulmonary aspiration: new concepts in preoperative fasting guidelines.
Anesth Analg 1993; 77: 17182.
110 Petring OU, Blade DW. Gastric emptying in adults: an overview
related to anaesthesia. Anaesth Intensive Care 1993; 21: 77481.
THE LANCET Vol 362 November 22, 2003 www.thelancet.com
For personal use. Only reproduce with permission from The Lancet publishing Group.
ANAESTHESIA II
111 Dowling JL Jr. Nulla per os after midnight reassessed.
Rhode Island Medicine 1995; 78: 33941.
112 Corbett AR, Mortimer AJ. Pre-operative fasting: how long is
necessary? Eur J Anaesth 1997; 14: 55557.
113Pandit UA, Pandit SK. Fasting before and after ambulatory surgery.
J Perianesth Nursing 1997; 12: 18187.
114 Eriksson LI, Sandin R. Fasting guidelines in different countries.
Acta Anaesthesiol Scand 1996; 40: 97174.
115American Society of Anesthesiologists Task Force on Preoperative
Fasting. Practice guidelines for preoperative fasting and the use of
pharmacologic agents to reduce the risk of pulmonary aspiration:
application to healthy patients undergoing elective procedures.
Anesthesiology 1999; 90: 896905.
116 Brady M, Kinn S, Stuart P. Preoperative fasting for children (protocol
for a Cochrane review). In: The Cochrane Library, Issue 3, 2001.
Oxford: Update Software.
117 Splinter WM, Schreiner MS. Preoperating fasting in children.
Anesth Analg 1999; 89: 8089.
118 Simini B, Bertolini G. Should same anaesthetist do preoperative
anaesthetic visit and give subsequent anaesthetic? Questionnaire survey
of anaesthetists. BMJ 2003; 327: 7980.
119 Simini B. Pre-operative visits by anaesthetists. Anaesthesia 2001; 56:
591.
120 Royal College of Anaesthetists and Association of Anaesthetists of
Great Britain and Ireland. Good practice: a guide for departments of
anaesthesia. 1998.
121 American Society of Anesthesiologists: The ASA Directory of
Members 1994. American Society of Anesthesiologists, Park Ridge,
IL, 1994.
122 Acapem J, Bouillot JL, Paquet JC, Hay JM, Coggia M. La
radiographie thoracique propratoire systmatique en chirurgie
gnrale est-elle utile? Ann Fr Anesth Ranim 1992; 11: 8895.
123 Garca-Miguel FJ. Efectividad del electrocardiograma y la radiografa
de trax preoperatorios en el Hospital General de Segovia. Propuestas
de mejora. PhD thesis, Universidad autnoma de Madrid, 2000:
26971.
124 Lpez-Bastida J, Serrano-Aguilar P, Duque-Gonzlez B,
Talavera-Dniz A. Cost analysis and potential cost savings related to
the use of preoperative tests in hospitals of the Canary Islands (Spain).
Gac Sanit 2003; 17: 13136.
125 Roizen MF. A prospective evalution of the value of preoperative
laboratory testing for office anesthesia and sedation.
J Oral Maxilofac Surg 1999; 57: 2122.
126 Asua J, Lpez-Argumedo M. Preoperative evaluation in elective
surgery. INAHTA Synthesis Report. Int J Technol Assess Health Care
2000; 16: 67383.
127 Deber RB, Kraetschmer N, Irvine J. What role do patients wish to play
in treatment decision making? Arch Intern Med 1996; 156: 141420.
128 Jadad A, Rizo C, Enkin M. I am a good patient, believe it or not. BMJ
2003; 326: 129395.
129 Moumjid N, Bremond A, Carrere MO. From information to shared
decision making in medicine. Health Expect 2003; 6: 18788.
THE LANCET Vol 362 November 22, 2003 www.thelancet.com
For personal use. Only reproduce with permission from The Lancet publishing Group.
1757
Das könnte Ihnen auch gefallen
- Clinical ReasoningDokument4 SeitenClinical Reasoningapi-351971578Noch keine Bewertungen
- Three-Stage Assessment. 2021Dokument14 SeitenThree-Stage Assessment. 2021Mwanja Moses100% (1)
- What Is A PICO QuestionDokument3 SeitenWhat Is A PICO QuestionBoid Gerodias100% (2)
- Football Emergency Medicine Manual 2 EditionDokument152 SeitenFootball Emergency Medicine Manual 2 EditionNicolás Alvarez VidelaNoch keine Bewertungen
- Clinical DX in PMR Case by CaseDokument143 SeitenClinical DX in PMR Case by CaseNayem comNoch keine Bewertungen
- DR - Muhammad Aasam Maan: Consultant Pain SpecialistDokument23 SeitenDR - Muhammad Aasam Maan: Consultant Pain SpecialistMuhammad Aasim MaanNoch keine Bewertungen
- Abdominal Examination: Male - Palpate Prostate Gland Female - Feel For CervixDokument5 SeitenAbdominal Examination: Male - Palpate Prostate Gland Female - Feel For CervixRemelou Garchitorena AlfelorNoch keine Bewertungen
- OBGYN HistoryDokument1 SeiteOBGYN Historysgod34Noch keine Bewertungen
- Case 5 - Pancreatitis-1Dokument4 SeitenCase 5 - Pancreatitis-1ngNoch keine Bewertungen
- What Causes Urinary Retention?Dokument4 SeitenWhat Causes Urinary Retention?darkz_andreaslimNoch keine Bewertungen
- Fellowship in Critical Care MedicineDokument12 SeitenFellowship in Critical Care MedicinerajiNoch keine Bewertungen
- MS Obst & GynaeDokument77 SeitenMS Obst & GynaeAmna MunawarNoch keine Bewertungen
- Hospital Discharge Education For CHFDokument18 SeitenHospital Discharge Education For CHFarafathusein29Noch keine Bewertungen
- Polyhydramnios and Oligohydramnios Clinical ExamDokument2 SeitenPolyhydramnios and Oligohydramnios Clinical ExamAhmad FahroziNoch keine Bewertungen
- OSCE Station 1 Diabetic LL ExamDokument5 SeitenOSCE Station 1 Diabetic LL ExamJeremy YangNoch keine Bewertungen
- psc006 PDFDokument2 Seitenpsc006 PDFPHitphitt Jeleck SangaattNoch keine Bewertungen
- National Guidelines On Management of Dengue Fever & Dengue Haemorrhagic Fever in Children and Adolescents - Sri LankaDokument53 SeitenNational Guidelines On Management of Dengue Fever & Dengue Haemorrhagic Fever in Children and Adolescents - Sri LankaNational Dengue Control Unit,Sri Lanka100% (1)
- Health AssessmentDokument25 SeitenHealth AssessmentGovindaraju Subramani100% (1)
- Critical Thinking and Nursing ProcessDokument49 SeitenCritical Thinking and Nursing ProcessjeorjNoch keine Bewertungen
- Preceptor Evaluation of StudentDokument2 SeitenPreceptor Evaluation of Studentapi-382409594100% (2)
- Geriatrics Study GuideDokument44 SeitenGeriatrics Study GuideahkrabNoch keine Bewertungen
- Antenatal Care Services: by DR - Chinedu Ibeh Thursday, 16 APRIL 2015Dokument81 SeitenAntenatal Care Services: by DR - Chinedu Ibeh Thursday, 16 APRIL 2015SehaRizaNoch keine Bewertungen
- Practice Marketing Plan FinalDokument14 SeitenPractice Marketing Plan Finalapi-317365152Noch keine Bewertungen
- Testicular CancerDokument48 SeitenTesticular Cancerluckyswiss7776848Noch keine Bewertungen
- Osteoid OsteomaDokument24 SeitenOsteoid Osteomadrqazi777Noch keine Bewertungen
- Knee ExaminationDokument14 SeitenKnee ExaminationAsimNoch keine Bewertungen
- A KhamDokument324 SeitenA KhamQuang NhânNoch keine Bewertungen
- Final 2010 GYN Module Clinical ObjectivesDokument36 SeitenFinal 2010 GYN Module Clinical Objectiveslolapell100% (1)
- Nursing Handover of Vital Signs at The Transition of Care Fromthe Emergency Department To The Inpatient Ward Anintegrative ReviewDokument12 SeitenNursing Handover of Vital Signs at The Transition of Care Fromthe Emergency Department To The Inpatient Ward Anintegrative ReviewLilac SpaceNoch keine Bewertungen
- Spinal Cord Injury: Andi IhwanDokument31 SeitenSpinal Cord Injury: Andi IhwanAndi Muliana SultaniNoch keine Bewertungen
- Comprehensive Geriatric Assessment Proforma Apr-15Dokument11 SeitenComprehensive Geriatric Assessment Proforma Apr-15Udin Nicotinic100% (2)
- Orthopediatric LWWDokument398 SeitenOrthopediatric LWWかちえ ちょうNoch keine Bewertungen
- History TakingDokument55 SeitenHistory TakingDeepika MahajanNoch keine Bewertungen
- COPD Follow UpDokument1 SeiteCOPD Follow Upe-MedTools100% (4)
- Olivia Engle NP ResumeDokument1 SeiteOlivia Engle NP Resumeapi-654403621Noch keine Bewertungen
- Clinical Practice Guidelines We Can Trust PDFDokument291 SeitenClinical Practice Guidelines We Can Trust PDFpierdevaloisNoch keine Bewertungen
- Pain PhysiologyDokument40 SeitenPain PhysiologyAnmol Jain100% (1)
- Nursing Reflection - 1st Year PostingDokument5 SeitenNursing Reflection - 1st Year PostingNurul NatrahNoch keine Bewertungen
- Please Read The Entire Form Carefully Before SigningDokument2 SeitenPlease Read The Entire Form Carefully Before SigningKoh LudzNoch keine Bewertungen
- Health Screening ChecklistDokument1 SeiteHealth Screening ChecklistRominaPulvermüllerSalvatierraNoch keine Bewertungen
- Care of The Patient in The Perioperative PeriodDokument20 SeitenCare of The Patient in The Perioperative PeriodMohammed FaragNoch keine Bewertungen
- Template Soap NeuroDokument2 SeitenTemplate Soap NeuroJohan SitepuanNoch keine Bewertungen
- Management of Vacuum Assisted Closure TherapyDokument14 SeitenManagement of Vacuum Assisted Closure TherapyVoiculescu MihaelaNoch keine Bewertungen
- ThrombophlebitisDokument3 SeitenThrombophlebitismirrejNoch keine Bewertungen
- Case ReportDokument6 SeitenCase ReportJellie MendozaNoch keine Bewertungen
- Pediatric Orthopedic Conditions ManagementDokument142 SeitenPediatric Orthopedic Conditions Managementluh martaniNoch keine Bewertungen
- Fetal assessment overview under 40 charsDokument3 SeitenFetal assessment overview under 40 charsAde Yonata100% (1)
- Report On Family Planning (4400)Dokument27 SeitenReport On Family Planning (4400)Bikram KushaalNoch keine Bewertungen
- StrokeDokument6 SeitenStrokeRaulLopezJaimeNoch keine Bewertungen
- DDH Treatment - PFDokument30 SeitenDDH Treatment - PFHendra SantosoNoch keine Bewertungen
- Critical Incident AnalysisStacy CentenoDokument2 SeitenCritical Incident AnalysisStacy Centenocentenochicago100% (1)
- Cancer Pain ManagementDokument22 SeitenCancer Pain ManagementWanie KafleeNoch keine Bewertungen
- MMP Handy Chart October 2011 V2Dokument69 SeitenMMP Handy Chart October 2011 V2Icha IchaNoch keine Bewertungen
- Physical Examination Form: Medications AllergiesDokument4 SeitenPhysical Examination Form: Medications AllergiesIris Ann PhillipsNoch keine Bewertungen
- Pa Tool MihpDokument23 SeitenPa Tool MihpNassif M. BangcolaNoch keine Bewertungen
- Complete Physical Examination ChecklistDokument5 SeitenComplete Physical Examination Checklistapi-641836481Noch keine Bewertungen
- Tuberculosis of SpineDokument11 SeitenTuberculosis of SpineSepti RahadianNoch keine Bewertungen
- OSCE Assessment Workshop GuideDokument55 SeitenOSCE Assessment Workshop GuideShouja ChauduryNoch keine Bewertungen
- ICU Scoring Systems A Complete Guide - 2020 EditionVon EverandICU Scoring Systems A Complete Guide - 2020 EditionNoch keine Bewertungen
- Code Geass - StoriesDokument5 SeitenCode Geass - Stories1234chocoNoch keine Bewertungen
- QLD Rail Traim PDFDokument1 SeiteQLD Rail Traim PDF1234chocoNoch keine Bewertungen
- Blue Veins Sub Theme TVBDokument4 SeitenBlue Veins Sub Theme TVB1234chocoNoch keine Bewertungen
- Blue BirdDokument7 SeitenBlue Bird1234chocoNoch keine Bewertungen
- Mbs Quick Guide: JULY 2020Dokument2 SeitenMbs Quick Guide: JULY 20201234chocoNoch keine Bewertungen
- Pokemon Theme Song 22Dokument4 SeitenPokemon Theme Song 221234chocoNoch keine Bewertungen
- Fairy Tail - Main ThemeDokument3 SeitenFairy Tail - Main Theme1234chocoNoch keine Bewertungen
- Topical Steroids (Sep 19) PDFDokument7 SeitenTopical Steroids (Sep 19) PDF1234chocoNoch keine Bewertungen
- USMLE Flashcards: Anatomy - Side by SideDokument190 SeitenUSMLE Flashcards: Anatomy - Side by SideMedSchoolStuff100% (3)
- Osteo Infographic FinalDokument1 SeiteOsteo Infographic Final1234chocoNoch keine Bewertungen
- Doctor Talk: Communication Practice Role PlaysDokument6 SeitenDoctor Talk: Communication Practice Role Plays1234chocoNoch keine Bewertungen
- # 3 - Prospective Study of The Diagnostic Accuracy of The Simplify D-Dimer Assay For Pulmonary Embolism in EDDokument7 Seiten# 3 - Prospective Study of The Diagnostic Accuracy of The Simplify D-Dimer Assay For Pulmonary Embolism in ED1234chocoNoch keine Bewertungen
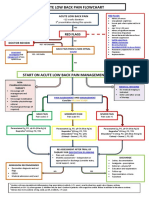
- Acute Low Back Pain Flowchart January 2017Dokument1 SeiteAcute Low Back Pain Flowchart January 20171234chocoNoch keine Bewertungen
- Topical Steroids (Sep 19) PDFDokument7 SeitenTopical Steroids (Sep 19) PDF1234chocoNoch keine Bewertungen
- Getting the Hospital Job: A Step-by-Step Guide to Applying for Your First PositionDokument41 SeitenGetting the Hospital Job: A Step-by-Step Guide to Applying for Your First Position1234chocoNoch keine Bewertungen
- PBM Module1 MTP Template 0Dokument2 SeitenPBM Module1 MTP Template 01234chocoNoch keine Bewertungen
- VTE GuidelinesDokument11 SeitenVTE Guidelines1234chocoNoch keine Bewertungen
- Fluids ElectrolytesDokument2 SeitenFluids Electrolytes1234chocoNoch keine Bewertungen
- The Effects of Social Networks On Disability in Older AustraliansDokument22 SeitenThe Effects of Social Networks On Disability in Older Australians1234chocoNoch keine Bewertungen
- Metro South Intern Training Form (Logan)Dokument3 SeitenMetro South Intern Training Form (Logan)1234chocoNoch keine Bewertungen
- 2016 Applicant Guide Web V2Dokument83 Seiten2016 Applicant Guide Web V21234chocoNoch keine Bewertungen
- Defining and Assessing Risks To Health PDFDokument20 SeitenDefining and Assessing Risks To Health PDF1234chocoNoch keine Bewertungen
- Language of PreventionDokument9 SeitenLanguage of Prevention1234chocoNoch keine Bewertungen
- FLOWCHART - ARC Adult Cardiorespiratory ArrestDokument1 SeiteFLOWCHART - ARC Adult Cardiorespiratory Arrest1234chocoNoch keine Bewertungen
- Taking a Social and Cultural History: A Biopsychosocial ApproachDokument3 SeitenTaking a Social and Cultural History: A Biopsychosocial Approach1234chocoNoch keine Bewertungen
- Managing Mental Illness in Patients From CALD Backgrounds: PsychiatryDokument5 SeitenManaging Mental Illness in Patients From CALD Backgrounds: Psychiatry1234chocoNoch keine Bewertungen
- Herd Immunity'' A Rough Guide PDFDokument6 SeitenHerd Immunity'' A Rough Guide PDF1234chocoNoch keine Bewertungen
- Clinical Contributions To Addressing The Social Determinants of HealthDokument5 SeitenClinical Contributions To Addressing The Social Determinants of Health1234chocoNoch keine Bewertungen
- ImprovingMedAdherenceOlderAdultslyer Final 508CDokument2 SeitenImprovingMedAdherenceOlderAdultslyer Final 508CKumar PatilNoch keine Bewertungen
- A Conceptual Framework For HealthDokument1 SeiteA Conceptual Framework For Health1234chocoNoch keine Bewertungen
- Bell's Palsy: N. Julian Holland and Jonathan M. BernsteinDokument21 SeitenBell's Palsy: N. Julian Holland and Jonathan M. BernsteinEeqNoch keine Bewertungen
- Original Article: Bipolar Disorders. 2021 00:1-22Dokument22 SeitenOriginal Article: Bipolar Disorders. 2021 00:1-22Carolina MuñozNoch keine Bewertungen
- Part A-7-Snake BiteDokument7 SeitenPart A-7-Snake Bitefernanda1rondelli0% (1)
- The Effectiveness of Complementary ManualDokument10 SeitenThe Effectiveness of Complementary ManualAli DptNoch keine Bewertungen
- Environmental Impact Identification ReviewDokument1 SeiteEnvironmental Impact Identification ReviewChun Jie Goh100% (1)
- End-Stage Renal DiseaseDokument3 SeitenEnd-Stage Renal DiseaseAkira Pongchad B100% (1)
- PCL S PDFDokument1 SeitePCL S PDFspectre68Noch keine Bewertungen
- Dental Management of The Patient Undergoing Radiotherapy or ChemoterapyDokument43 SeitenDental Management of The Patient Undergoing Radiotherapy or ChemoterapyJenadi Binarto100% (1)
- Pros and cons of experimental medical treatmentsDokument3 SeitenPros and cons of experimental medical treatmentskingfish1021Noch keine Bewertungen
- The Fight or Flight ResponseDokument22 SeitenThe Fight or Flight ResponseKaushalNoch keine Bewertungen
- Factors influencing health status and contact with health servicesDokument6 SeitenFactors influencing health status and contact with health servicesPuskesmas Sungai IliranNoch keine Bewertungen
- Nursing Diagnosis For SeizureDokument6 SeitenNursing Diagnosis For SeizureKenneth Cole100% (1)
- Admission and Basic Nursing CareDokument26 SeitenAdmission and Basic Nursing CareKardana PutraNoch keine Bewertungen
- Home RemedyDokument187 SeitenHome RemedyAnh Vu100% (5)
- How To Make Kombucha Tea - Complete HandbookDokument0 SeitenHow To Make Kombucha Tea - Complete Handbookcherrera73100% (1)
- Trabeculectomy-Related Corneal ComplicationsDokument7 SeitenTrabeculectomy-Related Corneal ComplicationsDian Putri NingsihNoch keine Bewertungen
- General Definition of The Nursing MetaparadigmDokument3 SeitenGeneral Definition of The Nursing MetaparadigmDennise Kate CabiedesNoch keine Bewertungen
- NCP: Prenatal InfectionDokument10 SeitenNCP: Prenatal InfectionJavieNoch keine Bewertungen
- Jac Brown Specific Techniques vs. Common Factors 2015Dokument17 SeitenJac Brown Specific Techniques vs. Common Factors 2015Mayra HernandezNoch keine Bewertungen
- Comm 210 Informative Speech OutlineDokument5 SeitenComm 210 Informative Speech Outlineapi-269568046Noch keine Bewertungen
- 3.8.25 Physical TherapyDokument25 Seiten3.8.25 Physical TherapyNeil OsborneNoch keine Bewertungen
- Effects of Mobile LegendsDokument3 SeitenEffects of Mobile LegendsRiziel SolaresNoch keine Bewertungen
- Dosage and SolutionsDokument3 SeitenDosage and SolutionsNicole PageNoch keine Bewertungen
- PanthenolDokument14 SeitenPanthenolSherif Adel EmamNoch keine Bewertungen
- Tarpan Therapy A Potential Ocular Therapeutics in AyurvedaDokument3 SeitenTarpan Therapy A Potential Ocular Therapeutics in AyurvedaBozidar MicicNoch keine Bewertungen
- Materia Medica For StudentsDokument5 SeitenMateria Medica For StudentsAnmol Vashistha0% (1)
- Control of Odors in The Sugar Beet Processing Industry: Technical PaperDokument7 SeitenControl of Odors in The Sugar Beet Processing Industry: Technical PaperIrvan DwikiNoch keine Bewertungen
- STI Power Point PresentationDokument33 SeitenSTI Power Point PresentationHervis Fantini100% (1)
- Anz Complaint ProcessDokument2 SeitenAnz Complaint ProcessBung HerryNoch keine Bewertungen
- Interview Reflection PaperDokument3 SeitenInterview Reflection Paperapi-250740396Noch keine Bewertungen