Beruflich Dokumente
Kultur Dokumente
GIT System: Bader Al-Mukhtar - RCSI - SC
Hochgeladen von
kinanOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
GIT System: Bader Al-Mukhtar - RCSI - SC
Hochgeladen von
kinanCopyright:
Verfügbare Formate
Bader Al- Mukhtar RCSI SC (2)
GIT System
History taking:
1. Presenting complaint + History of Presenting Complaint:
What brought you to the hospital?
Common CVS Symptoms:
1. Dysphagia
2. Odynophagia
3. Abdominal pain
4. Nausea and vomiting
5. Hematemesis
6. Bowel habit constipation and diarrhea
7. Rectal bleeding
8. Jaundice
9. Appetite and weight
10. Fever
Dysphagia - Difficulty swallowing
o
o
o
o
o
o
o
o
Onset (suddenly or gradually)
Duration
Frequency
Location
Progression
Severity (solid, fluid or both)
Aggravation factors
Relieving factors
Odynophagia
o
o
o
o
o
o
o
Onset
Duration
Frequency
Progression
Severity
Aggravation factors
Relieving factors
Abdominal pain
o
o
o
o
o
Onset (suddenly or gradually)
Duration
Frequency
Location
Radiation
Bader Al- Mukhtar RCSI SC (2)
Character
Progression
Severity
Aggravation factors (effect of movement, food, fasting, defecation and
micturition)
o Relieving factors (resting, certain position (leaning forward), specific
food, fasting, anatacid)
o
o
o
o
Abdominal swelling
o
o
o
o
o
o
o
Onset (sudden or gradual)
Duration
Frequency (is it intermittent)
Progression
Severity (how much weight gain recently)
Aggravated or relieving factors
Associated symptoms
Abdominal pain, SOB, fever to rule out Spontaneous bacterial
peritonitis
Cardiac, renal and GI symptoms to look for the cause
Nausea and vomiting
o
o
o
o
Duration
Frequency
Timing (specific time in the day OR in relation to meal)
Nature of vomitus
Food
Bile
Blood if yes ask about (amount, frequency, nature fresh or
coffee ground)
Constipation
o Constipation is the passage of stool <3 times/week, or stools that are hard
or difficult to pass.
o
o
o
o
o
Duration
Frequency
Progression
Aggravating factors
Relieving factors
Diarrhea
o Defined as an increase in stool volume (>200ml daily) and frequency
(3/day). Also a change in consistency to semi-formed or liquid stool.
Bader Al- Mukhtar RCSI SC (2)
Duration
Frequency especially night defecations
Color
Consistency
Contents:
Mucus
Blood if yes (amount, nature fresh blood, clots, timing start,
mixed, end, painful or painless)
Easy to flush away
o Progression
o Aggravating factors (recent antibiotic, strange food, recent travel)
o Relieving factors (fasting yes, then osmotic diarrhea)
o
o
o
o
o
Rectal bleeding
o
o
o
o
o
o
o
Duration
Frequency
Amount
Nature (brown, fresh blood, black), try to rule out melena as well
Timing in relation to stool
Aggravating and relieving factors
Associated symptoms:
Mucus, change in bowel habit, abdominal pain, weight loss
Jaundice
Duration
Extent
Dark urine and pale stool
Pruritis
Abdominal pain
Associated symptoms
fever, malaise, nausea and vomiting, diarrhea
o Risk factors
Contacts with jaundiced patient
Alcohol
Blood transfusion
IV drug users
Travel history
Sexual relationships sexually active
o
o
o
o
o
o
Change in appetite and weight
o Duration
Bader Al- Mukhtar RCSI SC (2)
o Severity
2. Past Medical History:
Have you ever had similar problem before?
o If yes what type? For how long you have it? Is it controlled with
your medications?
Have you ever been admitted to hospital for any reason?
Do you have any medical conditions or health problems of any kind?
If female obstetrics history
3. Past Surgical History:
Have you ever had any operations no matter how minor before?
o If yes When and what type? Any complications arised?
Have you had any trauma before? When? What happened?
4. Medications/Allergy:
Are you on any medications?
How about over the counter medications
Any herbal remedies?
Do you have any allergy against certain drugs/Food/dressings?
5. Family History:
Common question: Are there any medical conditions that run in the family?
Parents: Are your parents still alive? How is their health? or What was
the cause of their passing?
Siblings: Do you have brothers and sisters? How is their health?
6. Social History:
Wife and children: Are you married? Do you have kids? How is their health?
Smoking (how much and how long?).
Alcohol intake (how much and how long?)
o Important to ask about the CAGE questions to confirm alcoholism
if suspected:
A. Have you ever felt you should cut down on your drinking?
B. Have people annoyed you by criticising your drinking?
C. Have you ever felt bad or guilty about your drinking?
D. Have you ever had a drink first thing in the morning to steady
your nerves or get rid of a hangover (eye-opener)?
Bader Al- Mukhtar RCSI SC (2)
Occupation (his job).
Home circumstances: Including
o Who is with the patient at home and the general health of that person
o Home layout and where he is living
o Home modifications.
Physical examination:
General Inspection
1. First impression:
Does the patient appear well/unwell
Alert/Conscious and oriented (to person, space, time).
One of the diagnostic facies:
o Cushingoid face: plethoric and fat.
o Thyrotoxic face: thyroid stare, exopthalmus, lid retraction.
2. Weight, body habitus (physical build), posture and obvious scars:
Overweight/ Cachexia (weakness and wasting of the body due to severe
chronic illness)
Limb deformity, postural abnormality, obvious scars.
3. Hydration:
o Sunken eyes
o Dry mucous membranes (e.g. tongue).
o Reduced skin turgor (elasticity an area of skin when pulled away from
the body hangs in a wrinkled state for some seconds before falling back).
o Hypotension
o Coma (advanced).
4. Respiration
Rapid/laboured respiration
Chest symmetry during breathing
5. Abnormal discoloration:
Jaundice (Yellow discoloration of the skin and sclera)
Cyanosis (blue discoloration of the skin)
Pallor (suggesting anemia)
6. Comment on:
Equipment
Bedside table
Mobility
Bader Al- Mukhtar RCSI SC (2)
7. Vital signs
Radial pulse (look for CVS Ex).
Blood pressure
Temperature
Respiratory rate (normally about 14 breaths/min)
The hands:
1. Nails:
A. Leuconychia:
o Whitening of the nail bed due to hypoalbuminaemia
o Indicates: Hypoalbuminemia (e.g. malnutrition, malabsorption, hepatic
disease, nephritic syndrome).
B. Clubbing:
o Causes include: cirrhosis, celiac disease, IBD
C. Koilonychia
o Thin, brittle, concave finger nails
o May result from (chronic) iron deficiency anaemia
2. The Palms:
A. Palmar erythema:
o Reddening of the thenar and hypothenar eminences
o Attributed to raised oestrogen
o Can also occur with pregnancy/thyrotoxicosis/polycythaemia/rheumatoid
arthritis
B. Anemia:
o Inspect palmar creases for pallor [blood loss/malabsorption B12 and
folate], hemolysis (hypersplenism) or chronic disease.
C. Dupuytrens contracture
o Thickening and contraction of the palmar fascia causing permanent
flexion most often of the ring finger [associated with alcoholism, manual
work also familial]
D. Systemic sclerosis
Bader Al- Mukhtar RCSI SC (2)
o Tense tethering of the skin is associated with gastro-oesophageal
reflux/motility disorders
E. Hepatic Flap/Asterixis
3. The arms
A. Bruising
o Hepatocellular damage and the resulting coagulation disorder.
o Thrombocytopenia due to hypersplenism.
o Marrow suppression with alcohol.
B. Petechiae [pinhead sized bruises]
o Excessive alcohol consumption bone marrow depression
thrombocytopenia
o Splenomegaly [portal hypertension] hypersplenism
thrombocytopenia.
C. Scratch marks
o Obstructive or cholestatic jaundice may cause pruritis
o Commonly the presenting feature of primary biliary cirrhosis
4. The axillae
A. Lymphadenopathy
B. Acanthosis nigricans
o (a thickened, blackening of the skin. Velvety in appearance. May be
associated with intra-abdominal malignancy).
o Usually found in the axillae and the nape (back) of the neck
o Rarely associated with GIT carcinoma, lymphoma, acromegaly, DM
The face
1. Eyes
A. Jaundice:
Bader Al- Mukhtar RCSI SC (2)
o
A yellow discolouration of the sclera. This is usually the first place that
jaundice can be seen. Particularly useful in patient with dark skin tones in
whom jaundice would not be otherwise obvious.
B. Anaemia:
o
Pallor of the conjunctivae. You'll need experience to spot this easily.
C. Kayser-Fleisher rings:
o
Best seen with a slit-lamp in an ophthalmology clinic. A greenish-yellow
pigmented ring just inside the cornea-scleral margin. Due to copper
deposition. Seen in Wilson's disease.
D. Xanthelasma:
o
o
o
Raised yellow lesions caused by a build up of lipids beneath the skin often
seen encircling the eyes, especially at the nasal side of the orbit.
Cholestasis is associated with cholesterol
Xanthelasma are common in patients with primary biliary cirrhosis
2. Parotids/Parotidomegaly
o
o
o
Clench the teeth and palpate the masseter muscle
Parotid is best felt behind the masseter muscle and in front of the ear
Associated with alcoholism rather than liver disease
3. The Mouth
Ask the patient to show you their teeth then (open wide) and look carefully at the state of
the teeth, the tongue and the inner surface of the cheeks. You should also subtly attempt
to smell the patient's breath.
o
Angular stomatitis: a reddening and inflammation at the corners of the
mouth. A sign of thiamine, vitamin B12, and iron deficiencies.
o Circumoral pigmentation: Hyperpigmented areas surrounding the
mouth. Seen in Peutz-Jegher's syndrome (Freckle-like spots on the buccal
mucosa, fingers and toes are associated with hamartomas of the bowel,
Incidence of GIT adenocarcinoma is increased, Autosomal dominant
condition)
o
Dentition: note false teeth or if there is evidence of tooth decay.
Telangiectasia: dilatation of the small vessels on the gums and buccal
mucosa. Seen in Osler-Weber-Rendu syndrome.
o Gums: look especially for ulcers (causes include coeliac disease,
inflammatory bowel disease, Behet's disease and Reiter's syndrome) and
hypertrophy (caused by pregnancy, phenytoin use, leukaemia, scurvy
Bader Al- Mukhtar RCSI SC (2)
[vitamin C deficiency] or inflammation [gingivitis]). Aphthous
ulceration: Cause unknown
o
Breath: smell especially for:
o (Fetor hepaticus) a sweet-smelling breath.
o Ketosis: sickly sweet (pear-drop) smelling breath �
o Uraemia: a fishy smell
Tongue: look especially for:
o Glossitis: smooth, erythematous swelling of the tongue. Causes
include deficiencies of iron, vitamin B12, and folate deficiencies
o Macroglossia: enlarged tongue. Causes include amyloidosis,
hypothroidism, acromegaly, Down's syndrome, and neoplasia.
o Leukoplakia: a white-coloured thickening of the tongue and oral
mucus membranes. A premalignant condition caused by smoking,
poor dental hygiene, alcohol, sepsis and syphilis.
o Geographical tongue: painless red rings and lines on the surface
of the tongue looking rather like a map. Can be caused by vitamin
B2 (riboflavin) deficiency or may be a normal variant.
Candidiasis: (thrush). A fungal infection of the oral membranes seen as
creamy white curd-like patches which can be scraped off revealing
erythematous mucosa below. Causes include immunosuppression,
antibiotic use, poor oral hygiene, iron deficiency and diabetes.
The Neck
1. Palpate the cervical lymph nodes
o Examine the cervical and supraclavicular lymph nodes.
o Look especially for a supraclavicular node on the left-hand side which,
when enlarged, is called Virchow's node (Troisier's sign-suggestive of gastric
malignancy). These may be involved with gastric and other GIT malignancy
The Chest
1. Spider naevi
o Spider naevi: telangiectatic capillary lesions.
o A central red area with engorged capillaries spreading out from it in a
(spidery) manner.
o If the lesion is truly a spider naevus, it will be completely eliminated by
pressure at the centre using a pen-point or similar and will fill outwards when
the pressure is released.
o Found in the distribution of the superior vena cava arms, neck and chest
wall (usually above the nipple area).
1
Bader Al- Mukhtar RCSI SC (2)
o Causes include chronic liver disease, viral hepatitis, oestrogen excess and
pregnancy
2. Gynaecomastia
o Occurrence in the male of breasts resembling those of the sexually mature
female
o Sign of chronic liver disease
o Changes in the oestradiol to testosterone ratio may be responsible
o Spironolactone used to treat ascites is also a common cause
The abdomen inspection:
1. Scars:
o Indicating previous surgery or trauma:
2. Generalized abdominal distension:
o Causes include the Fs series:
i. Fat (gross obesity)
ii. Fluid (ascites)
iii. Foetus
iv. Flatus (gaseous distension due to bowel obstruction)
v. Faeces
vi. Big tumour or Phantom pregnancy
3. The shape of the umbilicus:
o Give a clue to the underlying cause of the distension.
o Inverted or everted
4. Local swelling:
o May indicate:
o Enlargement of one of the abdominal or pelvic organs
o Hernia: Protrusion of an intra-abdominal structure through an
abnormal opening. This may occur because of previous surgery
[incisional hernia], from a congenital abdominal wall defect or from
chronically increased intra-abdominal pressure.
5. Prominent veins:
Bader Al- Mukhtar RCSI SC (2)
o If these are present, the direction of venous flow should be elicited at this
stage, in order to differentiate between:
o Therefore, to distinguish caput Medusae from inferior vena caval
obstruction, determine the direction of flow below the umbilicus; it will be
towards the legs in the former and towards the head in the latter. Prominent
superficial veins can occasionally be congenital.
o Caput medusae: occur in patients with severe portal hypertension,
portal to systemic flow occurs through the umbilicus veins. The
direction of flow is away from the umbilicus.
o Inferior vena caval obstruction, usually due to a tumour or
thrombus, the abdominal veins enlarge to provide collateral blood
flow. The direction of flow is then upward towards the heart.
How to determine the flow of a vein?
(a) Place two fingers firmly on the vein. (b) The second finger is moved along the
vein to empty it of blood and keep it occluded. (c) The second finger is removed
but the vein does not refill. (d) At repeat testing and removing the first finger,
filling occurs, indicating the direction of flow.
6. Pulsations:
o An expanding central pulsation in the epigastrium suggests an abdominal
aortic aneurysm. In normal thin people the abdominal aorta may be seen to
pulsate.
7. Skin lesions
o These include the vesicles of herpes zoster, which occur in a radicular pattern
(they are localised to only one side of the abdomen in the distribution of a
single nerve root).
8. Striae
1
Bader Al- Mukhtar RCSI SC (2)
o Stretching of the abdominal wall severe enough to cause rupture of the elastic
fibres in the skin produces pink linear marks with a wrinkled appearance.
o When these are wide and purple-coloured, Cushing's syndrome may be the
cause.
o Ascites, pregnancy or recent weight gain are much more common causes of
striae.
9. Discoloration:
o Cullens sign: (Peri-umbilical bruising) Discoloration of the umbilicus with a
faintly bluish hue is rarely found in cases of extensive haemoperitoneum and
acute pancreatitis [the umbilical 'black eye']
o Grey Turners sign: (flank bruising) Skin discoloration may also rarely occur in
the flanks in severe cases of acute pancreatitis
The abdomen Palpation:
o Before you begin, ask the patient to let you know if you cause any discomfort.
You should be able to examine the abdomen without looking at it closely. Instead,
you should watch the patient's face for signs of pain.
1. General palpation:
o Light palpation:
o Look for tenderness or superficial masses
o If there is pain on light palpation, attempt to determine whether the
pain is worse when you press down or when you release the pressure
(rebound tenderness).
o If the abdominal muscles seem tense, determine whether it is localized
or generalized. Ensure the patient is relaxed-it may be helpful for the
patient to bend their knees slightly, relaxing the abdominal muscles.
An involuntary tension in the abdominal muscles apparently
protecting the underlying organs is called (guarding).
o Deep palpation
o This is used to detect deeper masses and to define those already
discovered.
o Any intra-abdominal mass must be carefully described.
Guarding:
o
o
o
o
resistance to palpation occurs due to contraction of the abdominal muscles
May result from tenderness or anxiety
Can be voluntary or involuntary
suggests peritonitis
Bader Al- Mukhtar RCSI SC (2)
Rigidity:
o Constant involuntary contraction of the abdominal muscles
o Associated with tenderness and indicates peritoneal irritation/peritonitis
Rebound tenderness:
o Strongly suggests the presence of peritonitis
o Compress abdominal wall slowly and release rapidly
o A sudden stab of pain results which may make patient wince
The liver:
1. Palpating the liver:
o On expiration the hand is advanced by 1-2cms closer to the right costal
margin.
o If the liver edge is identified the surface of the liver should be felt. It may be
hard or soft, tender or non-tender, regular or irregular and pulsatile or nonpulsatile.
2. The liver span:
o If the liver is palpable the total liver span is measured. Percuss down along the
right midclavicular line (starting from the sterna angle) until liver dullness is
detected. The normal upper border is the 6th rib.
o And then the lower edge starting from the RIF up to the costal margin
o The normal span is less than 13 cm.
The Gallbladder
o It is occasionally palpable below the right costal margin where this crosses the
lateral border of the rectus muscles
o Murphys sign: On taking a deep breath the patient catches his or her breath when
an inflammed gallbladder [cholecystitis] presses on the examiners hand which is
lying at the costal margin.
o Courvoisiers law: If the gallbladder is enlarged and the patient is jaundiced the
cause is unlikely to be gallstones. Carcinoma of the pancreas or lower biliary tree
resulting in obstructive jaundice is likely to be present
The spleen:
o The spleen enlarges inferiorly and medially. Begin with the examining hand in the
right iliac fossa and with the same technique used to examine for the liver slowly
move the hand towards the left costal margin.
o If the spleen is not palpable a two-handed technique is recommended. The left
hand is placed posterolaterally over the left lower ribs and the right hand is
placed on the abdomen below the umbilicus, parallel to the left costal margin.
Bader Al- Mukhtar RCSI SC (2)
This enables a slightly enlarged soft spleen to be felt as it moves down towards
the right iliac fossa.
o If the spleen is not palpable the patient is rolled onto the right side towards the
examiner and palpation is repeated. Begin palpation close to the left costal
margin.
o Splenomegaly becomes just detectable if the spleen is one-and-a-half to two
times enlarged.
The Kidneys
o The bimanual method is used.
o To palpate the right kidney the examiners left hand slides underneath the back to
rest with the heel of the hand under the right loin. The fingers remain free to flex
at the metacarpophalangeal joints in the area of the renal angle. The examiners
right hand is placed over the right upper quadrant.
o Ballotting: Press over the renal angle by flexing the fingers of the posterior hand.
The kidney can be felt to float upward and strike the anterior hand.
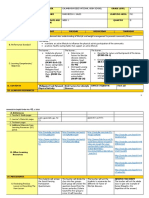
Table 9.1 Differentiating an enlarged spleen and an enlarged left kidney
Enlarged spleen
Enlarged kidney
Impossible to feel above
Can feel above the organ
Has a central notch on the leading No notch but you may feel the central hilar notch
edge
medially
Moves early on inspiration
Moves late on inspiration
Moves inferio-medially on
Moves inferiorly on inspiration
inspiration
Not ballottable
Ballottable
Dullness to percussion
Resonant percussion note due to overlying bowel
gas
May enlarge toward the umbilicus Enlarges inferiorly lateral to the midline
The abdomen Percussion:
Ascites:
o When 2-3 litres of ascites are present the abdomen will be dull to percussion in
the flanks. As fluid accumulates abdominal distension and umbilical eversion
occur. The dullness is then detectable closer to the midline.
o Shifting dullness
o Percuss out to the left flank until dullness is reached. Keeping your finger over
this area ask the patient to roll towards you. Ideally 30 seconds to 1 minute
should then pass so that gravity will cause the fluid to move to the right side of
the abdomen.
1
Bader Al- Mukhtar RCSI SC (2)
o Percussion is repeated and shifting dullness is present if the area of dullness has
changed to become resonant.
o Then go back to the umbilicus to confirm moving from resonant to dullness again.
o To sum up: from the umbilicus move to left, stay there, and then move back to
umbilicus.
o Fluid thrill
o This may be present when very large amounts of ascites are present.
o The patient can be asked to help by placing a hand in the midline of the
abdomen to prevent any ripple from passing through the fat of the anterior
abdominal wall. In a thin patient this is not necessary.
o One of the examiner's hands is placed flat on the patients flank.
o The other hand then flicks the other flank.
o A shock wave is transmitted to the palpating hand.
The abdomen Auscultation:
1. Bowel sounds:
o Place the diaphragm of the stethoscope just below the umbilicus. Bowel
sounds can be heard intermittently. They should be described as either present
or absent. Complete absence of bowel sounds over a 3 minute period indicates
paralytic ileus [complete absence of peristalsis in a paralysed bowel].
o Obstructed bowel produces a louder and higher pitched sound with a tinkling
quality.
2. Bruits:
o Just above the umbilicus over the aorta (abdominal aortic aneurysm).
o Either side of the midline just above the umbilicus (renal artery stenosis).
Das könnte Ihnen auch gefallen
- Test Bank For Medical Terminology 2nd Edition by BostwickDokument7 SeitenTest Bank For Medical Terminology 2nd Edition by Bostwicka596727542Noch keine Bewertungen
- Dysphagia, A Simple Guide To The Condition, Treatment And Related ConditionsVon EverandDysphagia, A Simple Guide To The Condition, Treatment And Related ConditionsBewertung: 5 von 5 Sternen5/5 (1)
- Crohn's Disease: Natural Healing Forever, Without MedicationVon EverandCrohn's Disease: Natural Healing Forever, Without MedicationNoch keine Bewertungen
- A Simple Guide to Blood in Stools, Related Diseases and Use in Disease DiagnosisVon EverandA Simple Guide to Blood in Stools, Related Diseases and Use in Disease DiagnosisBewertung: 3 von 5 Sternen3/5 (1)
- Case 5 - Pancreatitis-1Dokument4 SeitenCase 5 - Pancreatitis-1ngNoch keine Bewertungen
- History Taking and Physical ExaminationDokument53 SeitenHistory Taking and Physical ExaminationBoruuf If GammachuuNoch keine Bewertungen
- q2 Grade 9 Pe DLL Week 1Dokument11 Seitenq2 Grade 9 Pe DLL Week 1Airaa A. Baylan88% (8)
- Cholelithiasis & CholecystitisDokument16 SeitenCholelithiasis & CholecystitisMelissa Belair100% (9)
- Intestinal ObstructionDokument9 SeitenIntestinal ObstructionMuhammad Fuad Jaafar100% (1)
- Set 3 COMP-2Dokument71 SeitenSet 3 COMP-2Appu ayyalaNoch keine Bewertungen
- Crohns DiseaseDokument32 SeitenCrohns DiseaseMin Chi PakNoch keine Bewertungen
- MiscellaneousDokument487 SeitenMiscellaneoussalah subbahNoch keine Bewertungen
- Dentistry MCQ With AnswersDokument34 SeitenDentistry MCQ With AnswersAyesha Awan57% (7)
- Case Presentation OsteomylitisDokument64 SeitenCase Presentation OsteomylitisDemi Rose Bolivar100% (1)
- Surgical Audit and Peer Review Guide 2014Dokument54 SeitenSurgical Audit and Peer Review Guide 2014juweriyNoch keine Bewertungen
- SEMINAR ON MULTIPLE PREGNANCY ContentDokument21 SeitenSEMINAR ON MULTIPLE PREGNANCY ContentMonika shankar0% (1)
- C105a Pre-Sea and Periodic Medical Fitness Examinations For SeafarersDokument4 SeitenC105a Pre-Sea and Periodic Medical Fitness Examinations For SeafarersAbu ShabeelNoch keine Bewertungen
- Teen's Abdominal Pain Likely Due to Excessive Sorbitol IntakeDokument119 SeitenTeen's Abdominal Pain Likely Due to Excessive Sorbitol IntakeAnonymous Sgiok7100% (2)
- Cholelithiasis Case StudyDokument6 SeitenCholelithiasis Case StudySarah DentyNoch keine Bewertungen
- Gi Long CaseDokument8 SeitenGi Long CaseNadia SalwaniNoch keine Bewertungen
- Liver CirrhosisDokument75 SeitenLiver CirrhosisJohn Henry ValenciaNoch keine Bewertungen
- Crohn's DiseaseDokument38 SeitenCrohn's Diseasetintukmathew100% (1)
- Upper Gastrointestinal BleedingDokument69 SeitenUpper Gastrointestinal Bleedingeliza luisNoch keine Bewertungen
- General Medicine Practical NotesDokument33 SeitenGeneral Medicine Practical Notessaakshi parshionikarNoch keine Bewertungen
- NephrolithiasisDokument87 SeitenNephrolithiasissuwash100% (1)
- CholelitiasisDokument42 SeitenCholelitiasisEdwin YosuaNoch keine Bewertungen
- Colitis UlcerativeDokument4 SeitenColitis UlcerativeChatrina TandiloloNoch keine Bewertungen
- Case Study CholecystitisDokument28 SeitenCase Study CholecystitisK EV INNoch keine Bewertungen
- 1 IbdDokument11 Seiten1 Ibdmarinamaher14Noch keine Bewertungen
- Surgical History Taking and ExaminationDokument4 SeitenSurgical History Taking and ExaminationAnisah AliNoch keine Bewertungen
- Examen IM-gastroenterologieDokument15 SeitenExamen IM-gastroenterologieNicola BereholschiNoch keine Bewertungen
- Pedia 3B Manual Prelims - SGD casesDokument7 SeitenPedia 3B Manual Prelims - SGD casesMa Katherina ArellanoNoch keine Bewertungen
- Nurse caring for patient with abdominal mass and bowel obstructionDokument12 SeitenNurse caring for patient with abdominal mass and bowel obstructionabezareljvenNoch keine Bewertungen
- General Surgery ExamDokument48 SeitenGeneral Surgery ExamVarunavi SivakanesanNoch keine Bewertungen
- Abdominallecture 2015Dokument103 SeitenAbdominallecture 2015Abdelrahman MokhtarNoch keine Bewertungen
- Diabetes (HxPE)Dokument4 SeitenDiabetes (HxPE)ZH. omg sarNoch keine Bewertungen
- Diabetes (HxPE)Dokument4 SeitenDiabetes (HxPE)ZH. omg sarNoch keine Bewertungen
- Upper GI Guided NotesDokument9 SeitenUpper GI Guided NotesVanessaNoch keine Bewertungen
- Abdominal Exam For PA OSCEDokument11 SeitenAbdominal Exam For PA OSCEbumblebee9323Noch keine Bewertungen
- Adult Health Exam Hematology and LeukemiaDokument11 SeitenAdult Health Exam Hematology and Leukemiabrandie webbNoch keine Bewertungen
- Biliary System and PancreasDokument10 SeitenBiliary System and Pancreasjinkym123Noch keine Bewertungen
- Gastroenteritis in ChildrenDokument48 SeitenGastroenteritis in ChildrenKelsingra FitzChivalry FarseerNoch keine Bewertungen
- PBL Crohns DiseaseDokument4 SeitenPBL Crohns Diseasejack LermanNoch keine Bewertungen
- Diarrhea: Dr. Ali A. Ramadhan M.B.CH.B., Fibms, Fkbms (G & H)Dokument27 SeitenDiarrhea: Dr. Ali A. Ramadhan M.B.CH.B., Fibms, Fkbms (G & H)Ahmed NazarNoch keine Bewertungen
- Case Press WordDokument14 SeitenCase Press WordAlyssa BunquinNoch keine Bewertungen
- Presentation 1Dokument71 SeitenPresentation 1http_uglyNoch keine Bewertungen
- Surgery: Crohn's DiseaseDokument9 SeitenSurgery: Crohn's Diseaseapi-3829364Noch keine Bewertungen
- Liver Cirrhosis Patient with HematemesisDokument12 SeitenLiver Cirrhosis Patient with HematemesisMarianne R. LorenzoNoch keine Bewertungen
- Liver Nursing NotesDokument7 SeitenLiver Nursing NotesHeather ShantaeNoch keine Bewertungen
- Gastroenteritis in Children: Prepared by R. J. C. Manalo, BSN, RN, MNDokument45 SeitenGastroenteritis in Children: Prepared by R. J. C. Manalo, BSN, RN, MNHui ChenNoch keine Bewertungen
- Abdomen Exam Guide: Signs of GI PathologyDokument16 SeitenAbdomen Exam Guide: Signs of GI PathologyJerry GohNoch keine Bewertungen
- Cholecystitis Case Study: Pathophysiology, Clinical Assessments, Nursing CareDokument61 SeitenCholecystitis Case Study: Pathophysiology, Clinical Assessments, Nursing CarePlain GerlNoch keine Bewertungen
- Obstructive Jaundice DiagnosisDokument9 SeitenObstructive Jaundice DiagnosiswhosenahNoch keine Bewertungen
- Lapja KolelitiasisDokument46 SeitenLapja KolelitiasisDeyaSeisoraNoch keine Bewertungen
- Gerd Gerd Gerd: Dr. Rocky Danilo Willis, M.D., AMTDokument31 SeitenGerd Gerd Gerd: Dr. Rocky Danilo Willis, M.D., AMTRocky Willis100% (1)
- Medical Causes of Dysphagia - Evaluation and Diagnosis of GERD and Esophageal CancerDokument72 SeitenMedical Causes of Dysphagia - Evaluation and Diagnosis of GERD and Esophageal CancerMaisarah IsmailNoch keine Bewertungen
- PP03L038 Gallbladder DisordersDokument80 SeitenPP03L038 Gallbladder Disordersapi-3805855100% (2)
- Inflammatory Bowel DiseaseDokument12 SeitenInflammatory Bowel DiseasemoonsoundNoch keine Bewertungen
- GIT Conditions - StudentsDokument57 SeitenGIT Conditions - StudentsShamal KoyeNoch keine Bewertungen
- B6 - Surgery GS II Case 1Dokument9 SeitenB6 - Surgery GS II Case 1GregNoch keine Bewertungen
- Intestinal obstruction: causes, symptoms, diagnosis and treatmentDokument10 SeitenIntestinal obstruction: causes, symptoms, diagnosis and treatmentمنيب سالمNoch keine Bewertungen
- Intestinal Obstruction:: Classification: 1. Dynamic (Peristalsis Increased)Dokument6 SeitenIntestinal Obstruction:: Classification: 1. Dynamic (Peristalsis Increased)Qusai Al JarrahNoch keine Bewertungen
- General Survey by DR ADBDokument34 SeitenGeneral Survey by DR ADBRahul KumarNoch keine Bewertungen
- Gastroduodenal Disorders: Suazo, Trisha Mae S. 3BSN-ADokument12 SeitenGastroduodenal Disorders: Suazo, Trisha Mae S. 3BSN-AKenneth OpinaNoch keine Bewertungen
- Askep IbdDokument43 SeitenAskep IbdYou100% (1)
- Understanding Abdominal TraumaDokument10 SeitenUnderstanding Abdominal TraumaArmin NiebresNoch keine Bewertungen
- Alimentary and Biliary Conditions 3-1Dokument249 SeitenAlimentary and Biliary Conditions 3-1Mercy KeruboNoch keine Bewertungen
- Protocol ServandoDokument4 SeitenProtocol ServandoAllison Eunice ServandoNoch keine Bewertungen
- Clinical Approach To A Case of Obstructive JaundiceDokument22 SeitenClinical Approach To A Case of Obstructive JaundiceEsraa SalemNoch keine Bewertungen
- Primary Progressive Aphasia: Neurological ProgressDokument8 SeitenPrimary Progressive Aphasia: Neurological ProgressDranmar AhmedNoch keine Bewertungen
- Brain Tumor Segmentation and Detection Using Nueral NetworksDokument9 SeitenBrain Tumor Segmentation and Detection Using Nueral Networksjoshi manoharNoch keine Bewertungen
- Ulnar Nerve Entrapment - WikipediaDokument6 SeitenUlnar Nerve Entrapment - WikipediaSylvia GraceNoch keine Bewertungen
- Case StudyDokument18 SeitenCase StudyNovaWulandariPalufiNoch keine Bewertungen
- New PRC Form SampleDokument8 SeitenNew PRC Form SampleLanie Esteban EspejoNoch keine Bewertungen
- Cervical Cancer Literature ReviewDokument6 SeitenCervical Cancer Literature Reviewaflskeqjr100% (1)
- Immunization Case-Based Register: DHIS2 Tracker Data Model in PracticeDokument11 SeitenImmunization Case-Based Register: DHIS2 Tracker Data Model in PracticeGerald ThomasNoch keine Bewertungen
- HNP3Dokument9 SeitenHNP3dev darma karinggaNoch keine Bewertungen
- Running Head: Quality Improvement Project: Nurse To Patient Rati 1Dokument5 SeitenRunning Head: Quality Improvement Project: Nurse To Patient Rati 1api-300602911Noch keine Bewertungen
- Patient understood the effects of consuming sweets and soda to her blood sugar level. She will avoid soda and limit sweets intake to manage her blood glucoseDokument3 SeitenPatient understood the effects of consuming sweets and soda to her blood sugar level. She will avoid soda and limit sweets intake to manage her blood glucoseXerxes DejitoNoch keine Bewertungen
- RCOG - Management of Suspected Ovarian Masses in Premenopausal WomenDokument14 SeitenRCOG - Management of Suspected Ovarian Masses in Premenopausal WomenGabriela Andrade AriasNoch keine Bewertungen
- Accepted Manuscript: Journal of The Neurological SciencesDokument31 SeitenAccepted Manuscript: Journal of The Neurological SciencesZelNoch keine Bewertungen
- Infectious Bronchitis in Broiler - Veterinaria DigitalDokument3 SeitenInfectious Bronchitis in Broiler - Veterinaria DigitalMahesh KajagarNoch keine Bewertungen
- Non-Alcoholic Fatty Liver Disease - Causes, Diagnosis, Cardiometabolic Consequences, and Treatment StrategiesDokument12 SeitenNon-Alcoholic Fatty Liver Disease - Causes, Diagnosis, Cardiometabolic Consequences, and Treatment StrategiesntnquynhproNoch keine Bewertungen
- 02-09 2022 Pharm Pediatrics 2022 R4Dokument44 Seiten02-09 2022 Pharm Pediatrics 2022 R4Amira HelayelNoch keine Bewertungen
- Eli Lilly Insulin & DiabetesDokument4 SeitenEli Lilly Insulin & Diabetesm_dattaiasNoch keine Bewertungen
- Low-Level Laser Therapy (780 NM) On VEGF Modulation at Partially Injured Achilles TendonDokument5 SeitenLow-Level Laser Therapy (780 NM) On VEGF Modulation at Partially Injured Achilles TendonMichele GonçalvesNoch keine Bewertungen
- Indian Kino Tree Bark - VijaysarDokument3 SeitenIndian Kino Tree Bark - VijaysarNeutron ZionNoch keine Bewertungen
- Low Frequency Tens "Transcutaneos Electrical Nervestimulation"Dokument72 SeitenLow Frequency Tens "Transcutaneos Electrical Nervestimulation"Florian BeldimanNoch keine Bewertungen
- Posterior Circulation Stroke: By: DR - Pardeep MandhanDokument68 SeitenPosterior Circulation Stroke: By: DR - Pardeep MandhanSana ShafeeqNoch keine Bewertungen
- BONE SCAN - Chest Imaging (2010)Dokument38 SeitenBONE SCAN - Chest Imaging (2010)Luna WhiteNoch keine Bewertungen