Beruflich Dokumente
Kultur Dokumente
Mata
Hochgeladen von
vikrizkaOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Mata
Hochgeladen von
vikrizkaCopyright:
Verfügbare Formate
Ophthalmology and Eye Diseases
O r i g i nal Resea r c h
Open Access
Full open access to this and
thousands of other papers at
http://www.la-press.com.
Effect of Bevacizumab Injection before Vitrectomy
on Intravitreal Hemorrhage in Pseudophakic Patients
with Proliferative Diabetic Retinopathy
Mehmet Demir, Ersin Oba, Efe Can, Orhan Kara and Sonmez Cinar
Sisli Etfal Training and Research Hospital, Department of Ophthalmology, Istanbul, Turkey.
Corresponding author email: drmehmetfe@hotmail.com
Abstract: We evaluated the effect of intravitreal bevacizumab (IVB) injection before pars plana vitrectomy (PPV) on intravitreal
hemorrhage (VH) during and after vitrectomy for postoperative the first day and the first month in pseudophakic patients with proliferative diabetic retinopathy (PDR). This retrospective study was performed on 44 eyes of 44patients who underwent vitrectomy for
PDR. Patients were divided into PPV (n=22 eyes) and PPV+IVB (n=22 eyes) groups. Injection of bevacizumab (1.25mg/0.05mL)
was performed 3 days before vitrectomy. Outcomes of visual acuity as well as intraoperative and postoperative VH were compared
between the two groups. One month after surgery, visual acuity improved in PPV and PPV+IVB groups (P=0.005, P=0.006),
respectively. There was no difference between the two groups in best corrected visual acuity at baseline and after vitrectomy (P=0.71).
Intraoperative bleeding into the vitreous was recorded in 14 (63.6%) cases in the PPV group and in 7 (31.8%) cases in the PPV+IVB
group. The first month, intravitreal hemorrhage was recorded in six patients in the PPV group and in two patients in the PPV+IVB
group (P=0.03). The mean pre-postoperative central macular thickness was similar in both groups. Intravitreal injection of IVB before
vitrectomy decreased the rate of VH at the time of surgery and at the first postoperative month in patients with PDR.
Keywords: intravitreal bevacizumab, intravitreal hemorrhage, proliferative diabetic retinopathy, vitrectomy
Ophthalmology and Eye Diseases 2013:5 1115
doi: 10.4137/OED.S12352
This article is available from http://www.la-press.com.
the author(s), publisher and licensee Libertas Academica Ltd.
This is an open access article published under the Creative Commons CC-BY-NC 3.0 license.
Ophthalmology and Eye Diseases 2013:5
11
Demir et al
Introduction
Intravitreal hemorrhage (VH) during vitrectomy and
postoperative rehemorrhage into the vitreous are common complications in patients with proliferative diabetic retinopathy (PDR). Intravitreal hemorrhage,
preretinal fibrovascular membranes, and tractional
retinal detachment are the major causes of decreases in
vision in patients with PDR.1 Pars plana vitrectomy is
used to remove VH, preretinal membranes, and relieve
vitreoretinal tractions.2 Bevacizumab is a recombinant monoclonal antibody against vascular endothelial growth factor (VEGF) and was approved by the
US food and Drug Administration (FDA) for treating
colorectal cancer. Intravitreal bevacizumab (IVB) has
been used for choroidal neovascularization secondary
to age-related macular degeneration (AMD),3 proliferative diabetic retinopaty (PDR),4,5 rubeosis iridis (RI),6,7
and macular edema (ME) secondary to diabetic retinopathy (DR) or retinal vein occlusion (RVO).813 The
aim of this study was to examine the effect of IVB
before vitrectomy on VH during and after vitrectomy in
pseudophakic patients with PDR.
Methods
Data for patients who underwent pars plana vitrectomy (PPV) and PPV with IVB injection 3 days
before vitrectomy were reviewed. Preoperative values for best corrected visual acuity (BCVA, decimal),
intraocular pressure (IOP), and records of intraoperative VH and postoperative BCVA (decimal), IOP, VH,
retinal detachment, and endopthalmitis at 1 month
were analyzed.
This study included pseudophakic diabetic patients
who had preretinal fibrovascular membranes involving
or threatening the macula, PDR associated rubeosis
iridis, massive preretinal bleeding covering the posterior pole, and BCVA of #0.1. Patients with pregnancy,
phakic, history of hemodialysis, retinal vein occlusion,
history of IVB injection, optic atrophy, behcet disease,
trauma, and history of vitrectomy, break/s of retina, use
of gas, silicon oil or air the end of vitrectomy, preoperative BCVA of $0.1 were excluded.
Patients were divided into 2 groups. The PPV
group included 22 eyes of 22 patients (8 male, 14
female); the PPV + IVB group included 22 eyes of
22 patients (10 male, 12 female) undergoing PPV
from January 2008 to December 2012. The mean
age was 58.8 9.0 years in the PPV group and the
12
mean age was 60.7 7.8 years in the PPV + IVB
group (Table 1). All patients had type 2 diabetes
mellitus and had no treatment with panretinal
photocoagulation. However, panretinal photocoagulation was performed intraoperatively or during the
first month after surgery.
Bevacizumab was injected 3days before PPV at a
dose of 1.25mg/0.05 ML (Avastin; South San Francisco,
CA, USA) injected into the vitreous body using a
27-gauge (g) needle 3.5mm posterior of the limbus at
the inferotemporal area in the operating room.
Central macular thickness (CMT) was measured by
optical coherence tomography (OCT) pre- and postoperatively at one month in patients who had no VH.
Standard three port PPV was performed using
23-gauge (g) vitrectomy systems (Alcon Lab, Inc., Fort
Worth, TX, USA) in all patients. Preretinal membranes
were peeled using scissors, a pick, or the vacuum mode
of vitrectomy systems. Triamcinolone acetonide was
used in all cases for visualization of the vitreous. The
internal limiting membrane was not peeled.
Patients were examined before surgery and at 1,
7 days and 1 month after surgery. Values for the two
groups were compared used their data of preoperative,
intraoperative, and postoperative at 1 day and 1 month.
The study was approved by the local ethics committee. The study performed according to the tenets of the
Declaration of Helsinki. All patients gave their written
informed consent before participating in the study.
Mean measurements were expressed as the mean
standard deviation (SD). Mean BCVA (baseline and
at 1 month), IOP (at baseline and at 1 month), and
VH (at 1day and at 1month) were compared. SPSS
10.0software was used for evaluation. The 2-sample
Table 1. Demographic characteristics, preoperative fasting glucose level, HbA1c, and follow-up time.
Parameters
PPV (n=22;
mean SD)
PPV + IVB
(n=22;
mean SD)
P*
Age (years)
Male/female
HbA1c%
Preoperative fasting
glucose level
Follow-up time (day)
58.89.03
8/14
8.21.0
14920.4
60.77.80
10/12
8.01.4
15521.9
0.44
0.55
0.60
0.69
30.22.5
30.62.4
0.62
Note: *Statistical value P , 0.05 was considered statistically significant.
Abbreviations: PPV, pars plana vitrectomy; IVB, intravitreal
bevacizumab; HbA1c, glycosylated hemoglobin; SD, standard deviation.
Ophthalmology and Eye Diseases 2013:5
PDR/ 23 gauge PPV/IVB
t-test was used to compare data between groups.
P,0.05 was considered statistically significant.
Results
In the PPV group; final BCVA showed improvement in 15 eyes (68.2%), stabilized in 4 (18.2%)
eyes and decreased in 3 (13.6%) eyes after surgery at
one month. The mean baseline BCVA was 0.050.03
and mean postoperative BCVA was 0.120.09 at one
month (P,0.05). The BCVA was $0.1in 10 eyes
at one month.
Intraoperative VH occurred in 14 eyes, with postoperative VH recorded in 11 eyes on the first postoperative day; VH was recorded in six eyes at 1month.
In five eyes, VH was cleared spontaneously during
the first postoperative month. Iatrogenic retinal breaks
during surgery were recorded in 3 eyes.
In the PPV + IVB group, final BCVA showed
improvement in 19 eyes (86.4%), no change in one
(4.5%) eye, and decrease in two (9.1%) eyes. The mean
baseline BCVA was 0.050.04 and mean postoperative BCVA was 0.130.11 at 1month. Intraoperative
VH occurred seven eyes. VH was recorded in 4 eyes
on the first day and in 2 eyes at 1 month. During
the first month after surgery, VH was cleared spontaneously in 2 eyes. Iatrogenic retinal break/s was/
were recorded in one eye during surgery. The BCVA
was $0.1in 14 eyes at one month.
Patients who received retinal tamponade (silicon
oil, gas or air) were excluded, so the level of BCVA
was not affected by the tamponade. Elevated IOP
(.21mmHg) was recorded in 4 eyes in the PPV and
in 3 eyes in the PPV + VB group (P=0.68).
Pre- and postoperative values in mean BCVA
and IOP were similar in both groups (Table 2).
Mean preoperative CMT values were 385113 and
373138 m (P=0.97) in the PPV and PPV + IVB
groups, respectively. Postoperative CMT values were
30545 and 29434 m (P=0.51) in the PPV and
PPV + IVB groups at one month, respectively.
Discussion
VEGF has been shown to contribute significantly to
PDR. Increased production of VEGF produced by
retinal pigment epithelium (RPE) cells, pericytes,
and endothelial cells secondary to ischemia can be
blocked by retinal laser photocoagulation by decreasing the ischemic area. IVB blocks the effect of VEGF
on receptors and inhibits retinal new vessels and
cells in neovascular membranes.1416 IVB has potent
anti-angiogenic effects and has been shown to cause
regression of neovascularization.17
The effects of IVB in patients with neovascularization elsewhere in the retina secondary to PDR have
been evaluated in a number of studies. Fluorescein
angiography revealed a reduction of leakage from
the foci of neovascularization elsewhere in the retina secondary to PDR or neovascularization of the
optic disc.18 A study reported regression of neovascularization in eyes with active progressive PDR.19
Table 2. Data for BCVA, IOP, and complications in both groups.
Parameters
PPV (n=22; mean SD)
PPV + IVB (n=22; mean SD)
P*
BCVA (baseline, decimal)
BCVA (at 1month, decimal)
IOP (baseline)
IOP (at 1month)
Preop. CMT (m)
Postop. CMT (m, at 1month)
VH during PPV
VH 1st day
VH at 1month
Iatrogenic retinal breaks during surgery
IOP elevation (need antiglaucoma drug)
Endopthalmitis
Systemic side events
Retinal detachment
0.050.03
0.120.09
17.71.8
19.53.4
385113
30545
14
11
6
3
4
0
0
0
0.050.04
0.130.11
17.52.1
20.25.1
373138
29434
7
4
2
1
3
0
0
0
0.92
0.71
0.75
0.83
0.97
0.51
0.03
0.02
0.03
0.06
0.68
Abbreviations: PPV, pars plana vitrectomy; IVB, intravitreal bevacizumab; VH, vitreous hemorrhage; IOP, intraocular pressure; BCVA, best corrected
visual acuity; SD, standard deviation.
Note: *Statistical value P,0.05 was considered statistically significant.
Ophthalmology and Eye Diseases 2013:5
13
Demir et al
reoperative IVB made the surgery much easier
P
by decreasing the activity of new vessels and causing less bleeding during removal of the proliferative
membrane.20
This study revealed that IVB reduces the rate of
VH during and after PPV in patients with PDR. This
study showed that IVB is helpful for limiting fibrovascular proliferation before vitrectomy, making surgery easier.
Injection of IVB before vitrectomy also decreased
surgical time.21 Intraoperative VH is an important
complication associated with PDR in PPV.22 We determined VH by direct observation during surgery and
found VH in 14 eyes in the PPV group. Removal of
the hemorrhage may not only create iatrogenic breaks
but also extend the breaks, resulting in significantly
more bleeding. In some instances, surgery cannot continue due to the hemorrhage and a second surgery is
required. Often, surgery with intraoperative bleeding
shows an increased risk of postoperative hemorrhage.
It has been suggested that IVB is useful for avoiding hemorrhage. VH occurred less frequently in the
PPV + IVB group than in the PPV group. The use of
IVB reduced intraoperative hemorrhage and made
the surgery technically easier.18,23,24 A previous study
found no effect of IVB before vitrectomy.25
Recently, two studies found excellent clinical outcomes with IVB pretreatment in vitrectomy in patients
with severe diabetic retinopathy.26,27
IVB was found to be safe and effective for reducing the incidence of recurrent postoperative VH.28
This study showed that preoperative IVB caused less
intraoperative and postoperative VH. Preoperative
IVB injection was found to be a good strategy for
the after-surgery period.29 IVB injection before vitrectomy for PDR facilitates the surgery and decrease
postoperative VH.30 IVB injection 1 week before surgery reduced the incidence of postvitrectomy VH in
diabetic patients.31 In this study IVB injection was
performed 3 days before surgery. Postoperative VH
was reported in 6 eyes in the PPV group and in 2 eyes
in the PPV + IVB group at one month. The sources of
hemorrhage are often difficult to locate at the time of
surgery. The results of this study showed that the ratio
of re-hemorrhage into the vitreous was low in the PPV
+ IVB group. IVB prevented recurrence of VH in the
early postoperative period. Injection of IVB into the
14
vitreous decreased VH by blocking VEGF activity for
4 weeks, although some studies showed better visual
results than this study. This study did not include eyes
with preoperative cataract or lenticular opacification.
Several studies included patients that had undergone
phacoemulsification with PPV, in which a consequent
increase in BCVA was expected. No observed systemic or ophthalmologic side effect/s of IVB in either
group.
The limitations of this study were its retrospective design, small sample size, and lack of comparison of fluorescein angiography for baseline and after
vitrectomy.
In summary, preoperative IVB injection was helpful for reducing intraoperative VH and postoperative
VH complications in patients with PDR.
Author Contributions
Analyzed the data: MD, OK. Wrote the first draft of
the manuscript: MD, EC. Contributed to the writing
of the manuscript: EC, OK. Agree with manuscript
results and conclusions: All authors. Jointly developed
the structure and arguments for the paper: All authors.
Made critical revisions and approved final version:
All authors. All authors reviewed and approved of the
final manuscript.
Funding
Author(s) disclose no funding sources.
Competing Interests
Author(s) disclose no potential conflicts of interest.
Disclosures and Ethics
As a requirement of publication the authors have
provided signed confirmation of their compliance
with ethical and legal obligations including but not
limited to compliance with ICMJE authorship and
competing interests guidelines, that the article is neither under consideration for publication nor published
elsewhere, of their compliance with legal and ethical
guidelines concerning human and animal research participants (if applicable), and that permission has been
obtained for reproduction of any copyrighted material. This article was subject to blind, independent,
expert peer review. The reviewers reported no competing interests.
Ophthalmology and Eye Diseases 2013:5
PDR/ 23 gauge PPV/IVB
References
1. Patel JI, Hykin PG, Gregor ZJ, Boulton M, Cree IA. Angiopoietin concentrations in diabetic retinopathy.Br J Ophthalmol. 2005;89(4):4803.
2. Ishikawa K, Honda S, Tsukahara Y, Negi A. Preferable use of intravitreal
bevacizumab as a pretreatment of vitrectomy for severe proliferative diabetic retinopathy.Eye (Lond).2009;23(1):10811.
3. Aslan L, Aslankurt M, Aksoy A, Ozdemir M, Yksel E. Comparison of wide
conjunctival flap and conjunctival autografting techniques in pterygium
surgery. J Ophthalmol.2013;2013:209401.
4. Yang CS, Hung KC, Huang YM, Hsu WM. Intravitreal bevacizumab
(Avastin) and panretinal photocoagulation in the treatment of high-risk
proliferative diabetic retinopathy. J Ocul Pharmacol Ther. Mar 15, 2013.
[Epub ahead of print.]
5. Pokroy R, Desai UR, Du E, Li Y, Edwards P. Bevacizumab prior to vitrectomy
for diabetic traction retinal detachment. Eye (Lond).2011;25(8):98997.
6. Davidorf FH, Mouser JG, Derick RJ. Rapid improvement of rubeosis
iridis from a single bevacizumab (Avastin) injection. Retina. 2006;26(3):
3546.
7. Wolf A, von Jagow B, Ulbig M, Haritoglou C. Intracameral injection of
bevacizumab for the treatment of neovascular glaucoma. Ophthalmologica.
2011;226(2):516.
8. Ahmadieh H, Moradian S, Malihi M. Rapid regression of extensive retinovitreal neovascularization secondary to branch retinal vein occlusion after a
single intravitreal injection of bevacizumab. Int Ophthalmol. 2005;26(45):
1913.
9. Jorge R, Costa RA, Calucci D, Cintra LP, Scott IU. Intravitreal bevacizumab (Avastin) for persistent new vessels in diabetic retinopathy (IBEPE
study).Retina.2006;26(9):100613.
10. Demir M, Dirim B, Acar Z, Sendul Y, Oba E. Comparison of the effects
of intravitreal bevacizumab and triamcinolone acetonide in the treatment
of macular edema secondary to central retinal vein occlusion. Indian J
Ophthalmol. Apr 10, 2013. [Epub ahead of print.]
11. Yunoki T, Mitarai K, Yanagisawa S, Kato T, Ishida N, Hayashi A. Effects
of vitrectomy on recurrent macular edema due to branch retinal vein occlusion after intravitreal injection of bevacizumab. J Ophthalmol. 2013;2013:
415974.
12. Zhang Y,Ma J, Meng N,Li H,Qu Y. Comparison of intravitreal triamcinolone acetonide with intravitreal bevacizumab for treatment of diabetic
macular edema: a meta-analysis. Curr Eye Res.2013;38(5):57887.
13. Shimura M, Yasuda K, Yasuda M, Nakazawa T. Visual outcome after intravitreal bevacizumab depends on the optical coherence tomographic patterns of patients with diffuse diabetic macular edema. Retina.2013;33(4):
7407.
14. Giammaria D, Cinque B, Di Lodovico D, Savastano MC, Cifone MG,
Spadea L. Anti-vascular endothelial growth factor activity in the bevacizumab and triamcinolone acetonide combination for intravitreal use.Eur J
Ophthalmol.2009;19(5):8427.
15. Baeteman C, Hoffart L, Galland F, Ridings B, Conrath J. Subretinal hemorrhage after intravitreal injection of anti-VEGF for age-related macular
degeneration: a retrospective study.J Fr Ophtalmol. 2009;32(5):30913.
16. Han XX,Guo CM,LiY,Hui YN. Effects of bevacizumab on the neovascular membrane of proliferative diabetic retinopathy: reduction of endothelial
cells and expressions of VEGF and HIF-1. Mol Vis.2012;18:19.
Ophthalmology and Eye Diseases 2013:5
17. Yeoh J, Williams C, Allen P,etal. Avastin as an adjunct to vitrectomy in the
management of severe proliferative diabetic retinopathy: a prospective case
series. Clin Experiment Ophthalmol.2008;36(5):44954.
18. Avery RL, Pearlman J, Pieramici DJ, etal. Intravitreal bevacizumab (Avastin)
in the treatment of proliferative diabetic retinopathy. Ophthalmology.
2006;113(10):16956.
19. Moradian S, Ahmadieh H, Malihi M, Soheilian M, Dehghan MH,
Azarmina M. Intravitreal bevacizumab in active progressive proliferative
diabetic retinopathy. Graefes Arch Clin Exp Ophthalmol. 2008; 246(12):
1699705.
20. Ushida H, Kachi S, Asami T, Ishikawa K, Kondo M, Terasaki H. Influence
of preoperative intravitreal bevacizumab on visual function in eyes with
proliferative diabetic retinopathy. Ophthalmic Res.2013;49(1):306.
21. Rizzo S, Genovesi-Ebert F, Di Bartolo E, Vento A, Miniaci S,
Williams G. Injection of intravitreal bevacizumab (Avastin) as a preoperative adjunct before vitrectomy surgery in the treatment of severe proliferative diabetic retinopathy (PDR).Graefes Arch Clin Exp Ophthalmol.
2008;246(6):83742.
22. Oshima Y, Shima C, Wakabayashi T, etal. Microincision vitrectomy surgery
and intravitreal bevacizumab as a surgical adjunct to treat diabetic traction
retinal detachment.Ophthalmology.2009;116(5):92738.
23. Chen E, Park CH. Use of intravitreal bevacizumab as a preoperative adjunct
for tractional retinal detachment repair in severe proliferative diabetic
retinopathy.Retina.2006;26(6):699700.
24. Jirawison C, Ittipunkul N. Intravitreal bevacizumab at the end of diabetic vitrectomy for prevention of postoperative vitreous hemorrhage:
a comparative study. J Med Assoc Thai.2012;95 Suppl 4:S13642.
25. Ahn J,Woo SJ, Chung H, Park KH. The effect of adjunctive intravitreal
bevacizumab for preventing postvitrectomy hemorrhage in proliferative
diabetic retinopathy. Ophthalmology.2011;118(11):221826.
26. Couzinat A, Auriol S, Lequeux L, Arn JL, Pagot-Mathis V. Intravitreal
bevacizumab pretreatment in vitrectomy for severe diabetic retinopathy:
a series of six cases. J Fr Ophthalmol. 2012;35(4):265.
27. Zhao LQ, Zhu H, Zhao PQ, Hu YQ. A systematic review and meta-analysis
of clinical outcomes of vitrectomy with or without intravitreal bevacizumab
pretreatment for severe diabetic retinopathy. Br J Ophthalmol. 2011;95(9):
121622.
28. Cheema RA, Mushtaq J, Al-Khars W, Al-Askar E, Cheema MA. Role of
intravitreal bevacizumab (Avastin) injected at the end of diabetic vitrectomy in preventing postoperative recurrent vitreous hemorrhage. Retina.
2010;30(10):164650.
29. di LauroR,De Ruggiero P,di LauroR,di LauroMT, Romano MR. Intravitreal
bevacizumab for surgical treatment of severe proliferative diabetic
retinopathy. Graefes Arch Clin Exp Ophthalmol.2010;248(6):78591.
30. Modarres M, Nazari H, Falavarjani KG, Naseripour M, Hashemi M,
Parvaresh MM. Intravitreal injection of bevacizumab before vitrectomy for
proliferative diabetic retinopathy. Eur J Ophthalmol.2009;19(5):84852.
31. Ahmadieh H, Shoeibi N, Entezari M, Monshizadeh R. Intravitreal bevacizumab for prevention of early postvitrectomy hemorrhage in diabetic patients:
a randomized clinical trial. Ophthalmology.2009;116(10):19438.
15
Das könnte Ihnen auch gefallen
- MCQsDokument14 SeitenMCQsMudassar Saeed100% (1)
- Manual - Facoemulsificador Los DosDokument36 SeitenManual - Facoemulsificador Los DosSoporte Técnico ElectronitechNoch keine Bewertungen
- Asrs Common Retina CPT CodesDokument3 SeitenAsrs Common Retina CPT Codesapi-405859281Noch keine Bewertungen
- tmpA9F9 TMPDokument5 SeitentmpA9F9 TMPFrontiersNoch keine Bewertungen
- Retina 39 426Dokument9 SeitenRetina 39 426ryaalwiNoch keine Bewertungen
- IBEPE StudyDokument8 SeitenIBEPE StudyKaran KumarswamyNoch keine Bewertungen
- Intravitreal Conbercept Kh902 For Surgical.12Dokument6 SeitenIntravitreal Conbercept Kh902 For Surgical.12Gioco Armas HerreraNoch keine Bewertungen
- Francisco Trincão, João Feijão, Vítor Maduro, Nuno Alves, Carlos Batalha, Pedro Candelária, José Pita-NegrãoDokument1 SeiteFrancisco Trincão, João Feijão, Vítor Maduro, Nuno Alves, Carlos Batalha, Pedro Candelária, José Pita-NegrãoVitor MaduroNoch keine Bewertungen
- None 3Dokument11 SeitenNone 3Yehiel FlaviusNoch keine Bewertungen
- Tugas Akademik 13-Journal Reading 4-Glaukoma-Galuh Yulieta - 240215 - 072026Dokument8 SeitenTugas Akademik 13-Journal Reading 4-Glaukoma-Galuh Yulieta - 240215 - 072026Arina SetyaningrumNoch keine Bewertungen
- Analysis of Intraoperative and Postoperative Complications in Pseudoexfoliation Eyes Undergoing Cataract SurgeryDokument4 SeitenAnalysis of Intraoperative and Postoperative Complications in Pseudoexfoliation Eyes Undergoing Cataract SurgerymathyasthanamaNoch keine Bewertungen
- Vitrectomy Results in Proliferative Diabetic RetinopathyDokument3 SeitenVitrectomy Results in Proliferative Diabetic RetinopathyRohamonangan TheresiaNoch keine Bewertungen
- Cataract Formation and Progression in Patients Less Than 50 Years of Age After VitrectomyDokument5 SeitenCataract Formation and Progression in Patients Less Than 50 Years of Age After VitrectomyridwanNoch keine Bewertungen
- Presentación Edema Macular DiabéticoDokument26 SeitenPresentación Edema Macular Diabéticomauricio bayramNoch keine Bewertungen
- Combined Intravitreal Ranibizumab and Verteporfin Photodynamic Therapy Versus Ranibizumab Alone For The Treatment of Age-Related Macular DegenerationDokument5 SeitenCombined Intravitreal Ranibizumab and Verteporfin Photodynamic Therapy Versus Ranibizumab Alone For The Treatment of Age-Related Macular Degeneration568563Noch keine Bewertungen
- MiddleEastAfrJOphthalmol204332-3509353 094453Dokument4 SeitenMiddleEastAfrJOphthalmol204332-3509353 094453Yayu PujiNoch keine Bewertungen
- Jurnal 4Dokument8 SeitenJurnal 4Putri kartiniNoch keine Bewertungen
- tmp1BE0 TMPDokument4 Seitentmp1BE0 TMPFrontiersNoch keine Bewertungen
- Comparison of Intravitreal Bevacizumab (Avastin) With Triamcinolone For Treatment of Diffused Diabetic Macular Edema: A Prospective Randomized StudyDokument9 SeitenComparison of Intravitreal Bevacizumab (Avastin) With Triamcinolone For Treatment of Diffused Diabetic Macular Edema: A Prospective Randomized StudyBaru Chandrasekhar RaoNoch keine Bewertungen
- MainDokument7 SeitenMainiSee ClinicNoch keine Bewertungen
- Art 3A10.1007 2Fs40123 015 0033 3Dokument9 SeitenArt 3A10.1007 2Fs40123 015 0033 3Bernadin RexyNoch keine Bewertungen
- Intravitreal Injection of Bevacizumab: Review of Our Previous ExperienceDokument6 SeitenIntravitreal Injection of Bevacizumab: Review of Our Previous ExperienceShintya DewiNoch keine Bewertungen
- MataDokument16 SeitenMataIslah NadilaNoch keine Bewertungen
- Presentation 1Dokument24 SeitenPresentation 1-Yohanes Firmansyah-Noch keine Bewertungen
- PIIS0002939422003890Dokument9 SeitenPIIS0002939422003890Anca Florina GaceaNoch keine Bewertungen
- Original Article: Virendra K. Pal, Ajai Agrawal, Suwarna Suman, V. B. PratapDokument4 SeitenOriginal Article: Virendra K. Pal, Ajai Agrawal, Suwarna Suman, V. B. PratapAris BayuNoch keine Bewertungen
- Jurnal Mata 5 KEVIN PDFDokument10 SeitenJurnal Mata 5 KEVIN PDFKevinNoch keine Bewertungen
- Pi Is 0161642022006923Dokument12 SeitenPi Is 0161642022006923Anca Florina GaceaNoch keine Bewertungen
- Timing of Quiescence and Uveitis Recurrences AfterDokument10 SeitenTiming of Quiescence and Uveitis Recurrences AfterFlor ArenasNoch keine Bewertungen
- Retina 2012 Sep 32 (Suppl 2) S225-31Dokument7 SeitenRetina 2012 Sep 32 (Suppl 2) S225-31roro207Noch keine Bewertungen
- OJOph 2016062717483031Dokument8 SeitenOJOph 2016062717483031dechastraNoch keine Bewertungen
- 16 Nigwekar Etal.Dokument4 Seiten16 Nigwekar Etal.editorijmrhsNoch keine Bewertungen
- Rhegmatogenous Retinal DetachmentDokument6 SeitenRhegmatogenous Retinal DetachmentPutri kartiniNoch keine Bewertungen
- Rhegmatogenous Retinal DetachmentDokument6 SeitenRhegmatogenous Retinal DetachmentPutri kartiniNoch keine Bewertungen
- 2015 6 jns1546Dokument7 Seiten2015 6 jns1546ROHITNoch keine Bewertungen
- Piis0161642014000712 PDFDokument8 SeitenPiis0161642014000712 PDFZhakiAlAsrorNoch keine Bewertungen
- 34 67 1 SMDokument5 Seiten34 67 1 SMLutfiAnny Rahman HakimNoch keine Bewertungen
- ABSTRACT - BOOK - 10th IcgsDokument135 SeitenABSTRACT - BOOK - 10th Icgsd_kourkoutasNoch keine Bewertungen
- BMC OphthalmologyDokument7 SeitenBMC OphthalmologyRizki Yuniar WNoch keine Bewertungen
- 694-701 Yoeruek LoDokument8 Seiten694-701 Yoeruek LoMeirinda HidayantiNoch keine Bewertungen
- Pars Plana VitrekDokument8 SeitenPars Plana VitrekAnggisari Danastri DharmaNoch keine Bewertungen
- The Effect of Trabeculectomy On Astigmatism .99150Dokument5 SeitenThe Effect of Trabeculectomy On Astigmatism .99150Yulias YoweiNoch keine Bewertungen
- Adminku Journal Manager ErlaniDokument7 SeitenAdminku Journal Manager Erlanirm suryaubungNoch keine Bewertungen
- Anti-VEGF Treatment Is The Key Strategy For Neovascular Glaucoma Management in The Short TermDokument8 SeitenAnti-VEGF Treatment Is The Key Strategy For Neovascular Glaucoma Management in The Short TermhellowNoch keine Bewertungen
- 2023 Article 740Dokument13 Seiten2023 Article 740francescoNoch keine Bewertungen
- Journal ReadingDokument21 SeitenJournal ReadingRettyNoch keine Bewertungen
- Surgical Outcomes of Rhegmatogenous Retinal Detachment Associated With Ocular ToxoplasmosisDokument5 SeitenSurgical Outcomes of Rhegmatogenous Retinal Detachment Associated With Ocular Toxoplasmosisketrin capanemaNoch keine Bewertungen
- BR J Ophthalmol-2014-Chan-79-81 PDFDokument4 SeitenBR J Ophthalmol-2014-Chan-79-81 PDFRomi Mauliza FauziNoch keine Bewertungen
- Modern Capabilities of Surgical Management of Patients With Open-Angle Glaucoma Combined With CataractDokument5 SeitenModern Capabilities of Surgical Management of Patients With Open-Angle Glaucoma Combined With CataractTyasBanggaPribadieNoch keine Bewertungen
- 317694Dokument16 Seiten317694Indra PudlianNoch keine Bewertungen
- Clinical StudyDokument6 SeitenClinical StudyKarina Mega WNoch keine Bewertungen
- A Collaborative Retrospective Study On The Efficacy and Safety of Intravitreal Dexamethasone Implant (Ozurdex) in Patients With Diabetic Macular EdemaDokument17 SeitenA Collaborative Retrospective Study On The Efficacy and Safety of Intravitreal Dexamethasone Implant (Ozurdex) in Patients With Diabetic Macular EdemaJosé Díaz OficialNoch keine Bewertungen
- Jurnal Mata 5Dokument6 SeitenJurnal Mata 5Dahru KinanggaNoch keine Bewertungen
- LimitedDokument2 SeitenLimitedlfathiyahNoch keine Bewertungen
- Comparison of The Outcomes of Phacoemulsification and Manual Small-IncisionDokument5 SeitenComparison of The Outcomes of Phacoemulsification and Manual Small-Incisionkoas mr14Noch keine Bewertungen
- Ahmadieh 2007Dokument7 SeitenAhmadieh 2007Ruby KumarNoch keine Bewertungen
- Optical Coherence Tomography Angiography of Pathological Myopia Sourced and Idiopathic Choroidal Neovascularization With Follow-UpDokument7 SeitenOptical Coherence Tomography Angiography of Pathological Myopia Sourced and Idiopathic Choroidal Neovascularization With Follow-UpVlady BordaNoch keine Bewertungen
- 2016 Article 256Dokument5 Seiten2016 Article 256Yosephine SantosoNoch keine Bewertungen
- Jurnal Anti VEFGDokument9 SeitenJurnal Anti VEFGFitria Sirr Mu'thiarohmahNoch keine Bewertungen
- Five-Year Results of ViscotrabeculotomyDokument10 SeitenFive-Year Results of ViscotrabeculotomyChintya Redina HapsariNoch keine Bewertungen
- 17 - 2016-11-083 - DR Sumayya Khan PDFDokument6 Seiten17 - 2016-11-083 - DR Sumayya Khan PDFArsalan BukhariNoch keine Bewertungen
- The Effect of Bevacizumab Versus Ranibizumab in The Treatment of Corneal NeovascularizationDokument8 SeitenThe Effect of Bevacizumab Versus Ranibizumab in The Treatment of Corneal NeovascularizationmestevezfNoch keine Bewertungen
- Choroidal NeovascularizationVon EverandChoroidal NeovascularizationJay ChhablaniNoch keine Bewertungen
- Ibuprofen and Acetaminophen (Tylenol)Dokument2 SeitenIbuprofen and Acetaminophen (Tylenol)vikrizkaNoch keine Bewertungen
- 357 PDFDokument5 Seiten357 PDFvikrizkaNoch keine Bewertungen
- Primary Isoniazid Prophylaxis Against Tuberculosis in HIV-Exposed ChildrenDokument11 SeitenPrimary Isoniazid Prophylaxis Against Tuberculosis in HIV-Exposed ChildrenvikrizkaNoch keine Bewertungen
- PIN2247 Developmental Dysplasia Management With A Pavlik HarnessDokument3 SeitenPIN2247 Developmental Dysplasia Management With A Pavlik HarnessvikrizkaNoch keine Bewertungen
- Prevalence of Primary Open Angle Glaucoma in General Ophthalmic Practice in The United KingdomDokument3 SeitenPrevalence of Primary Open Angle Glaucoma in General Ophthalmic Practice in The United KingdomvikrizkaNoch keine Bewertungen
- Early Diagnosis of Developmental Hip Dysplasia in The District of Pirot, SerbiaDokument5 SeitenEarly Diagnosis of Developmental Hip Dysplasia in The District of Pirot, SerbiavikrizkaNoch keine Bewertungen
- BPPV 3Dokument5 SeitenBPPV 3vikrizkaNoch keine Bewertungen
- Comparison of A New, Minimally Invasive Strabismus Surgery Technique With The Usual Limbal Approach For Rectus Muscle Recession and PlicationDokument7 SeitenComparison of A New, Minimally Invasive Strabismus Surgery Technique With The Usual Limbal Approach For Rectus Muscle Recession and PlicationvikrizkaNoch keine Bewertungen
- Ijo 07 05 855Dokument5 SeitenIjo 07 05 855vikrizkaNoch keine Bewertungen
- Pneumatic RetinopexyDokument36 SeitenPneumatic RetinopexyMartínJiménezNoch keine Bewertungen
- Eyesi Surgical BrochureDokument16 SeitenEyesi Surgical BrochureHaag-Streit UK (HS-UK)Noch keine Bewertungen
- Medicure Instruments Delhi IndiaDokument10 SeitenMedicure Instruments Delhi IndiaMedicure InstrumentsNoch keine Bewertungen
- RetinaDokument42 SeitenRetinaAhmed Omara100% (2)
- Retina: Product CatalogDokument60 SeitenRetina: Product CatalogMohamed GamalNoch keine Bewertungen
- New Management Strategies For Ectopia LentisDokument14 SeitenNew Management Strategies For Ectopia LentisximoNoch keine Bewertungen
- Ablasi RetinaDokument38 SeitenAblasi RetinaTama RomaNoch keine Bewertungen
- 09 Pulsar2 PDFDokument7 Seiten09 Pulsar2 PDFhelpurusNoch keine Bewertungen
- Optic Disc Abnormalities - Cheat SheetDokument6 SeitenOptic Disc Abnormalities - Cheat SheetPaula EmyNoch keine Bewertungen
- 0417RT CodingDokument5 Seiten0417RT CodingcmirceaNoch keine Bewertungen
- Vitreous Gel Eye Retinal Detachment OphthalmologistDokument12 SeitenVitreous Gel Eye Retinal Detachment OphthalmologistLesTrechSaNoch keine Bewertungen
- Gui ListedTherapies PDFDokument263 SeitenGui ListedTherapies PDFSampath KumarNoch keine Bewertungen
- Fluidics in Modern VitrectomyDokument16 SeitenFluidics in Modern VitrectomyMohammad Abdullah Bawtag100% (1)
- Treatment of Macular EdemaDokument48 SeitenTreatment of Macular EdemaPushpanjali RamtekeNoch keine Bewertungen
- Machular HoleDokument14 SeitenMachular HoleRaymond FrazierNoch keine Bewertungen
- Jurnal EndoftalmitisDokument5 SeitenJurnal EndoftalmitisQuin ShaNoch keine Bewertungen
- Dos CatalogueDokument13 SeitenDos CatalogueLumbini ChowdharyNoch keine Bewertungen
- Karakteristik Dan Penanganan Penderita Sindrom Rubella Kongenital Di Pusat Mata Nasional Rumah Sakit Mata CicendoDokument7 SeitenKarakteristik Dan Penanganan Penderita Sindrom Rubella Kongenital Di Pusat Mata Nasional Rumah Sakit Mata CicendoRyuuzoraNoch keine Bewertungen
- FAIR SHIPPING CORP. v. JOSELITO T. MEDELDokument15 SeitenFAIR SHIPPING CORP. v. JOSELITO T. MEDELkhate alonzoNoch keine Bewertungen
- AAOSub2017 - RET SyllabusDokument217 SeitenAAOSub2017 - RET SyllabusYasminSolbergNoch keine Bewertungen
- Macular Buckle in Myopia: Pradeep Susvar and S. Vinay KumarDokument4 SeitenMacular Buckle in Myopia: Pradeep Susvar and S. Vinay KumarMohammad A. BawtagNoch keine Bewertungen
- List of Surgeries: AbdomenDokument35 SeitenList of Surgeries: AbdomenSaurav SaikiaNoch keine Bewertungen
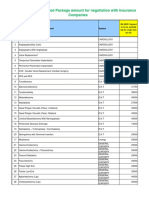
- IMA NHB Suggested Package Amount For Negotiation With Insurance CompaniesDokument5 SeitenIMA NHB Suggested Package Amount For Negotiation With Insurance Companiesmonikparmar1Noch keine Bewertungen
- Healthcare Coding Billing Reimbursement OverviewDokument130 SeitenHealthcare Coding Billing Reimbursement Overviewsvuhari100% (3)
- FIQ - Proliferative Diabetic RetinopathyDokument35 SeitenFIQ - Proliferative Diabetic RetinopathyHikban FiqhiNoch keine Bewertungen
- Clinical Patterns and Risk Factors For Rhegmatogenous Retinal Detachment at A Tertiary Eye Care Centre of Northern IndiaDokument6 SeitenClinical Patterns and Risk Factors For Rhegmatogenous Retinal Detachment at A Tertiary Eye Care Centre of Northern Indiarumaisyah alkatiriNoch keine Bewertungen
- Final Therapy PricesDokument133 SeitenFinal Therapy PriceskandukurisrimanNoch keine Bewertungen