Beruflich Dokumente
Kultur Dokumente
IM Hematology 6 With Oncology
Hochgeladen von
LucyellowOttemoesoeCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
IM Hematology 6 With Oncology
Hochgeladen von
LucyellowOttemoesoeCopyright:
Verfügbare Formate
IM
HEMATOLOGY 6 WITH ONCOLOGY 1
HEMATOLOGY 6
Dr. Tuy
012309
Common dse
associations
ACQUIRED HEMOLYTIC ANEMIA
*Warm reactive active type of AIHA
*Primary/Idiophatic most cases
*some are associated with common diseases
IMMUNE HEMOLYTIC ANEMIA (AIHA)
Erythrocytes destroyed prematurely by
immune mediated mechanism
Hemolysis resultd from ab or completements or
both, attached to RBC membrane comfirmed
by a positive direct antigloublin test (Coombs
test)
Pathophysiology
Cause intravascular hemolysis/extravascular
hemolysis
Intra: a able to actvate complement sys
prodn of membrane attack complex (can
directly attack the cell)
o IgM can readily activate complent
o IgG can sometimes activate
complement sys
Extra: reticuloendothelial system, ab in spleen
express the MPC phagocytosis
o Fragmentation of membrane
spherocytes
Coombs test
Direct coombs test binds to complement or
ab and makes the agglutination visible to the
naked eye
o Detects the presence of ab that is
attached to the cell
Indirect coombs test detects the presence of
ab that is present in the serum
Positive presence of agglutinins
Mark of AIHA positive coombs test
Classification
1. Alloimmune HA
a. Ab are alloab / made in response to
presence of foreign ag
i. Ex: ABO
ii. Major cross-matched reaction
2. Autoimmune HA
a. Derangement in self tolerance
b. Ab directed to the whole RBC age sp
RH antigen
i. Ex. With AIHA there is major
cross matching reaction
3. Drug-induced HA
a. Secondary to ab initially directed to the
bld which cross-react to the patients
RBC
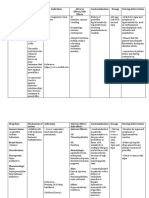
TYPE OF AIHA
characteristics
Ab isotype
DAT
Ag specificity
Hemolysis
Warm
reactive
Cold
agglutinin
dse
igG, rare IgA,
IgM
Igg, rare C3
Multiple esp
Rh
Extravas
Igm
Paroxysmal
cold
hemoglobinu
ria
Igg
C3
i/I, Pr
C3
P
Extra
Intra
b-cell
neoplasia,
collagenvascular
Viral,
neoplasia
Syphilis, viral
*positive Coombs test and presence of spherocytes
*Tx: 1st line: use of steroids
WHITE
-
BLOOD CELL DISORDERS
Granulocytes
Lymphocytes
Monocytes
The Normal Leukocyte Count
Cell type
Percent
Leukocytes
Neutrophils
45-75%
Stabs
0-5
Monocytes
5-10
Eosinophils
0-5
Basophils
0-1
Lymphocytes
10-45
Absolute count
5-11x109/L
4-6
0.5-1
<.45
<0.05
2-5
Absolute Neutrophil Count
Segmental + Stab x Total WBC count
Ex. TWBC = 10,000, ___= 90%
*AN COUNT = >5000
Normal Myeloppoiesis
DO of granulocytes and monocytes
Myeloid Differentiation
Granulocytes and monocytes have a common
progenitor cell
Derived from more primitive myeloid stem cell
line
From pluripotent stem cells in bone marrow
G-CSF: necessary to activate neutrophil to be
able to perform its action like phagocytosis
IL-3: colony-stimulating factor
Myeloid Function
Able to move from bone marrow, to circulation
to tissues (one way), follows the interleukins to
determine the site of location
o From circulation to tissue diapedesis
Mobilized during time of inflammation
Can phagocytose microorganism
Can exocytose
N stays in the circ from 6-7hrs
Sequence of Neutrophil Maturation
Can determine through the presence of
granules
Myeloblast
Promyelocytes primary granules
(myeloperoxidase)
Myelocytes - eccentric nucleus
Metamyelocytes (band) segmented nucleus
Polymorphonuclear neutrophils mature
IM
Histochemical stains for myeloid cells
Cell type
MPO
Specific
Nonspeci
esterase fic
esterase
Neutrophil 4+
3+
1+
s
Monocyte
2+
1+
3+
s
Lymphocy +/te
Periodic
acid
Schif
4+
2+
+/-
CD34 marker for pluripotent stem cells
Lymphocytes no specific immunologic markers
3 compartments:
1. BM comp 90%
2. Peripheral bld 2-3%
a. Circulating pool
b. Marginated pool attached to
endothelium
i. Decrease - leukocytosis
3. Extravascular space remaining %
*Quantitative DO due to defect in the storage
compartments
*infection BM inc granulocyte prodn, more granulocte
enter circ leukopenia
Neutropenia
Absolute Neutrophil
Count
>1500/mm3
1000-1500
500-1000
<500
<200
Clinical Significance
Normal
No significant risk for infxn
Some risk for infxn
Significant risk for infxn
Absence of inflammatory
response
Acute neutropenia more dangerous than chronic type
-
Leukemoid rxn 15-30K, mostly mature cells,
any infxn can trigger (cancer), no blast cells
Shift to the left presence of immature cells
Eosinophilia - >500
Basophilia rare
Abnormalities in lymphoid cells
IINTRODUCTION TO LEUKEMIAS
Leukemia presence of totally derived leukemic cells
(abnormal cells), displacing normal hematopoiesis
Presence of immature cells in the peripheral
blood
Leukemic cells are frequently present in:
Periph bld
Invade reticuloendothelial tissue
o Spleen, liver, LN
May invade other tissues
Untreated eventually causes death
HEMATOLOGY 6 WITH ONCOLOGY 2
Classification
Classified accdg to cell type with regards to both:
Cell maturity used to distinguish bet acute
and chronic leukemia
o If malignant cells are immature acute
Rapidly progressive
o If predominantly mature chronic
Slow and indolent
-
Cell lineage
o Myeloid
o Lymphoid
Classification:
Acute Lymphoid Leukemia
Acute Myeloid Leukemia or Acute Non-myeloid
Leukemia
Chronic Lymphocytic Leukemia
Acute Lymphocytic Leukemia
Etiology/Risk Factors
Heredity
o Congenital chromosomal abnormalities
o Hereditary immunodeficiency states
Chronic marrow dysfunction
o Aplastic 20%
o PNH
Drugs anticancer drugs
Ionizing radiation
Chemicals - benzene
Viruses
o HTLV-1 causative agent of adult T-cell
leukemia/lymphoma
Seen in Japan
Comparison of Acute and Chronic
Acute
Age
All ages
Clinical onset
Sudden
Course
<6mo
(untreated)
Leukemic cells
Immature
Anemia
Mild to severe
Thrombocytopen Mild to severe
ia
White cell count
Variable
Organomegaly
Mild
Leukemia
Chronic
Adults
Insidious
2-6yrs
Mature
Mild
Mild
Increased
Prominent
*cardinal feature: presence of blasts acute
Pathogenesis
BM failure
Anemia
Thrombocytopenia
Granulocytopenia
Organ Infiltration
Marrow expansion
Spleen
Liver
LN
CNS
Gums, mouth
*Acute form: rapidly progressive
*adults - sternum
Clin mani
Fatigue, malaise, pallor
Bruising, bleeding
Fever, infections
Bone or joint pain
Splenomegaly
Hepatomegaly
Lympadenopathy
Neurologic symptoms
Gingival hypertrophy, oral
lesions
IM
*<4y/o difficulty in walking
*testes, brain, anterior chamber of eye privilege sites,
absence of lymphnodes
Periodic acidSchif
HEMATOLOGY 6 WITH ONCOLOGY 3
Glycogen and
related
substances
Lymphocytes,
granulocytes,
megakaryocytes
Helpful in
supporting
diagnosis of
erythroleukemia
Immunologic Markers
Laboratory Evaluation of Acute Leukemia
Purpose: confirm the dx and distinguish AML
from ALL
Preliminary evaluation:
o CBC and peripheral bld examn
o BM studies
Morphologic examination
subjective exam
Cytochemical staining
Immunologic markers
Cytogenetic studies
Molecular genetic studies
Electron microscopy
Morphologic Approach to Classification (book)
Feature
AML
ALL
Blast size
Larger, usually
Variable, small
uniform
to medium size
Nucleoli
1-4, often
Absent or 1-2,
prominent
often indistinct
Auer rods
Present in 60Not present
70% of cases
Nuclear
Usually finely
Coarse to fine
chromatin
dispersed
Cytoplasm
Moderate,
Scant, coarse
abundant, fine
granules,
granules present sometimes
present ~7%
Others
Often dysplastic
Myeloid cells not
changes in
dysplastic
maturing
myeloid cells
*pathognomonic findings that distinguish AML/ALL: (+)
Auer rods
Cytochemical reactions useful in the dx of acute
leukemia
Special Stain
Site of Action
Cells Stained
Comment
Myeloperoxida
se
Mainly primary
granules; Auer
rods
Late myeloblasts, Separates AML (+)
granulocytes;
from
monocytes less
ALL (-)
intensely
Sudan black B
Phospholipids;
sterols, neutral
fats
Late myeloblast,
granulocytes;
monocytes less
intensely
Parallels
peroxidase, but
smears do not need
to fresh
Specific
esterase
(Naphthol AS-D
chloroacetate
Cytoplasm
Neutrophilic
granulocytes;
mast cells
Parallels
peroxidase, but less
sensitive;
Non-specific
esterase
(alphanapththyl
acetate and
butyrate)
Cytoplasm
Monocytes; focal Useful for
staining in T cells determining degree
of monocytic
diferentiation;
separates mono (+)
from myelo
(-) blasts
Lineage
Antigen
B cell
CD19, CD20, CD21, CD22, CD23, D24
T cell
CD1, CD2, CD3, CD4, CD5, CD7, CD8
Lymphoid
TdT
Myeloid
(granulocytic)
CD13, CD33, CD11b, CD15
Monocytic
CD14, CD11b
Erythroid
Glycophorin A
Megakaryocytic
CD41, CD42b, CD61
Lineage Independent
Antigens
HLA-DR
HLA class II
CD45
Leukocyte common antigen
CD34
Stem cell antigen
CD10
Common ALL antigen (CALLA)
ACUTE MYELOID LEUKEMIA / ACUTE
NONLYMPHOID LEUKEMIA
Definition
AML are clonal malignancies that are
characterized by the appearance of increased
numbers of immature myeloid cells in the
marrow and blood.
AML is a clonal, malignant disease of the
hematopoietic tissue that is characterized by
accumulation of abnormal (leukemic)
blast cells, principally in the marrow
impaired production of normal blood
cells.
Etiopathogenesis
Risk factors
Environmental
o radiation
o benzenes
o alkylating agents and other
cytotoxic drugs therapyrelated AML
Evolution from a chronic clonal
hemopathy
Inherited syndromes
Epidemiology
AML is the predominant form of leukemia
during the neonatal period and
accounts for 15 to 20 percent of acute
leukemia in children and
80 percent of acute leukemia in adults.
IM
HEMATOLOGY 6 WITH ONCOLOGY 4
(c) Diagnosis of M4 confirmed if > 20 percent of
marrow precursors are monocytes (confirmed by
special stains).
M4 with eosinophilia
1.
Revised Criteria for the Classification of AML
(FAB)
M0 with minimal differentiation
Large, agranular blasts (resemble ALL L2, rarely L1).
Myeloperoxidase negative or<3 percent positive; B-, T
lineage markers negative; CD13 and/or CD33 positive;
myeloperoxidase positive by immunochemistry or
electron microscopy; TdT may be positive.
M1 with minimal maturation
1.
2.
Blast cells, agranular and granular types (type I
and type II) >90 percent of non erythroid cells.
At least 3 percent of these are myeloperoxidase
or Sudan black positive.
Remaining 10 percent (or less) of cells are
maturing granulocytes or monocytes
M2 with maturation
1.
2.
3.
Sum of agranular and granular blasts (types I
and II) is from 30 to 89 percent of non-erythroid
cells.
Monocytic cells, <20 percent.
Granulocytes from promyelocytes to mature
polymorphs, > 10 percent.
M3 Promyelocytic
1.
Majority of cells are abnormal promyelocytes
with heavy granulation.
2. Characteristic cells containing bundles of Auer
rods (faggots) invariably present.
Note: Microgranular variant (M3v) also occurs.
Promyelocytes have marked nuclear irregularity that
includes reniform, lobulated and monocyte-like
indented nuclei. The cytoplasm contains fine or
indistinct granules in contrast to the coarse azurophilic
granules in typical M3.
M4 Myelomonocytic
1.
In the marrow, blasts >30 percent of nonerythroid cells.
2. Sum of myeloblasts, promyelocytes,
myelocytes and later granulocytes is between
30 and 80 percent of non-erythroid cells.
3. > 20 percent of non-erythroid cells are
monocyte lineage.
4. If monocytic cells exceed 80 percent, diagnosis
is M5
Note: (a) If marrow findings as above and
peripheral blood monocytes (all types) are > 5.0 x
109/L, diagnosis is M4
(b) If monocyte count < 5 x 109/L, M4 can be
confirmed on basis of serum lysozyme, combined
esterase, etc.
2.
3.
Eosinophils > 5 percent of non-erythroid cells in
marrow.
Eosinophils are abnormal.
Eosinophilis are chloroacetate and PAS positive.
M5 Monocytic
1.
2.
3.
80 percent of marrow non-erythroid cells are
monoblasts, promonocytes or monocytes.
M5a, 80 percent of monocytic cells are
monoblasts.
M5b, < 80 percent of monocytic cells are
monoblasts, remainder are predominantly
promonocytes and monocytes.
M6 Erythroleukemia
1.
The erythroid component of the marrow
exceeds 50 percent of all nucleated cells.
2. 30 of the remaining non-erythroid cells are
agranular or granular blasts ( types I and II).
Note: If > 50 percent erythroid cells but < 30
percent blasts, diagnosis becomes myelodysplastic
syndromes.
A rare form of erythoird neoplasia, erythremic
myelosis, involves only the red blood cell precursors.
The erythroblasts, primarily pronormoblasts and
basophilic normoblasts, constitute 90% or more of the
marrow cells.
M7 Megakaryocytic
1.
2.
3.
30 percent at least of nucleated cells are blasts.
Blasts identified by platelet peroxidase on
electron microscopy, or by monoclonal
antibodies.
Increased reticulin is common.
M0 all cells primitive
M1 Maturing granulocytes
M2 Pro-mature segmenters
M3 Unique disease, most abundant #of auer rods,
best prognosis (50% cure), spontaneous remission,
associated with DIC (usual complication), treatment is
diferent
M4 confused type; with eso: good prognostic sign
M5 infiltrates the gums and cns
M6 confused with megaloblastic anemia
M7 with fibroblastic tissue, difficult to aspirate during
BM studies
All trans retinoic acid (ATRA) M3
Same treatment for all except M3
Common Cytogenetic Abnormalities Associated
with AML
Chromosome
Abnormality
Associated Disorder
IM
t(8;21)
AML (M2)
t(15;17)
Unique to APL (M3)
16q
abnormalities:
inv (16) and del
(16)
AML with abnormal eosinophilia
(M4E)
t9;22)
t(9;11)
CML Philadelphia chromosome
Treatment
Remission-induction therapy
Post-remission maintenance therapy
Stem cell transplant
HEMATOLOGY 6 WITH ONCOLOGY 5
L1: best prognosis, commonly seen in children
L2: Poor prognosis, same appearance as myeloid
leukemia
L3: Worst prognosis, mature B-cell type, cytoplasmic
vacuolation, basophilia, heavy tumor burden, large
adenopathy, organomegaly
Acute Leukemia
A heterogeneous group of neoplasms afecting
uncommitted or partially committed
hematopoietic stem cells.
The retained capacity of some diferentiation is
the basis for the phenotypic classification.
Broadly divided into (based on cell origin)
Non-lymphoid (Myeloid) leukemia
Lymphoid leukemia
ACUTE LYMPHOID LEUKEMIA
(Acute Lymphoblastic leukemia, Acute Lymphocytic
Leukemia)
Definition
ALL is a neoplastic disease that results from
multistep somatic mutations in a single
lymphoid progenitor at one of several discrete
stages of development.
The immunophenotype of leukemic cells at
diagnosis reflects the level of diferentiation
achieved by the dominant clones.
Etiopathogenesis
Risk Factors
Genetic syndromes
Environmental factors
Host pharmocogenetics
In utero development of ALL
FAB Classification of ALL
Morphologi
c
Features
L1
L2
L3
Cell size
Small
Large
Large
Nuclear
chromatin
Fine or clumped Fine
Fine
Nuclear
shape
Regular, may
have cleft of
indentation
Regular, oval to
round
Nucleoli
Indistinct or not 1 or more per
visible
cell; large
prominent
1 or more per
cell; large
prominent
Amount of
cytoplasm
Scanty
Moderately
abundant
Moderately
abundand
Cytoplasmic
basophilia
Slight
Slight
Prominent
Cytoplasmic
vacuoles
Variable
Variable
variable
Irregular, may
have cleft or
indentation
Classification of Leukemia
Acute Myeloid (FAB classification)
Acute myeloblastic leukemia
without diferentiation (M0)
without maturation (M1)
with maturation (M2)
Acute promyelocytic leukemia (M3)
APL
Acute myelomonocytic leukemia (M4)
AMML
Acute monocytic leukemia (M5) AMoL
Erythroleukemia (M6) Di Guglielmos
syndrome
Acute megakaryoblastic leukemia (M7)
Acute Lymphoblastic
Precursor B-cell ALL
Early-Pre-B-cell ALL
Pre-B-cell ALL
B-cell ALL
T-cell ALL
Chronic Myeloid
Chronic myelogenous leukemia (CML)
Chronic eosinophilic leukemia (CEL)
Chronic basophilic leukemia (CBL)
Chronic Lymphoid
Chronic lymphocytic leukemia (CLL)
B-cell CLL
T-cell CLL
Prolymphocytic leukemia
Hairy cell leukemia
Plasma cell leukemia
Szary syndrome
Etiology and Risk Factors
Host Factors
Heredity
Congenital chromosomal abnormalities
Immunodeficiency
Chronic marrow dysfunction
Environmental Factors
IM
Ionizing radiation
Chemicals and drugs
Viruses
HEMATOLOGY 6 WITH ONCOLOGY 6
3 separate phases
Chronic phase 2-5years
Accelerated phase intractable anemia
and splenomegaly
Blastic (acute) leukemia phase 34months
AML
acute lymphoid leukemia
Clinical features
Sx of hypermetabolism wt loss anorexia or
night sweats
Splenomegaly
Features of anemia
Signs of bleeding inspite of elevated platelet ct
Rare sx: visual disturbance, priapism
Asymptomatic
Laboratory findings
Leukocytosis >50000
Inc circling basophils
Nomocytic normochromic
Neutrophil alkaline phosphatase low
CHRONIC MYELOPROLIFERATIVE DISORDERS
(CMPDs)
Definition
Clonal dos in multipotent hematopoietic
progenitor cell characterized by:
Overprodn of one or more of the
formed elements if the bld withut
significant dysplasia
BM hypercellular
Predilection to extramedullary
hematopoiesis
Splenomegaly
Myelofibrosis
WHO classification of CMPDs
CML behaves as a malignant neoplasm (Ph
chromosome)
Chronic neutrophilic
Chronic esosinophilic
Polycythemia vera
Chronic idiopathic myelofibrosis
Essential thrombocythemia
Common clinical features of CMPDs
Afects middle-aged and o.der grps
Insidious, sometimes silent, asymp onset
Panhyperplasia of BM
Freq transitions between DO
Large numner of megakaryocytes
Elevation of plt ct
Hemorrhagic and thrombotic complications
Cytogenetic abnormalities (Ph chromosome)
CHRONIC MYELOID LEUKEMIA
Clonal do of a pluripotent stem cell
May occur at any age
Characterized by presence of Philadelphia
chromosome (t9:22)
With tyrosine kinase activity necessary for signal
transduction
Clinical course
Treatment chronic phase
Tyrosine kinase inhibitors
Imatinib mesylate
Stem cell transplantation only curative tx
Age <70
1st degree relative
Chemotherapy
Hydroxyurea
Busulfan
a-interferon
CHRONIC LYMPHOPROLIFERATIVE DISORDERS
Definition
accumulation in the blood of mature
lymphocytes of either b or t cell type
features may overlap lymphoma
distinction bet CLL and lymphoma may
be difficult
generally incurable but may have a chronic and
fluctuating course
Classification of Chronic Lymphoproliferative
Disorders
B-cell
T-cell
Chronic lymphoid leukemia
Chronic lymphoctyic
Large granular
leukemia (CLL)
lymphocytic
leukemia
Prolymphocytic
T-cell
leukemia (PLL)
prolymphocytic
leukemia (T-PLL)
Hairy cell leukemia (HCL)
Plasma cell leukemia
Leukemia/lymphoma
syndromes
Splenic lymphoma with
Sezary syndrome
villous lymphocytes
Follicular lymphoma
Adult T-cell
leukemia/
IM
Mantle cell lymphoma
Lymphoma
Large cell
lymphoma
Lymphoplasmacytic
lymphoma
Large cell lymphoma
Diagnosis
chronic persistent lymphocytosis
subtypes:
morphology
immunophenotype
cytogenetics
DNA analysis showing a monoclonal
rearrangement of either Ig or T-cell
receptor genes
Chronic Lymphocytic Leukemia
B-cell
MC leukemia in the western worlds
Definition
Clonal do of b cell lymphocyte characterized
by:
Peripheral blood and BM lymphocytosis
Morphologically the lympghocytes have
a relatively mature, well-diferentiated
appearance
Presence of basket cells/smudge cells
Clinical features
Older adults
MF 2:1
Discovered incidentally
Some may have enlarged lymph nodes; signs
and symptoms of anemia; bleeding secondary
to thrombocytopenia
Spleen palpable in half of cases
Immunosuppression from
hypogammaglobulinemia and cellular immune
dysfunction may occur
Laboratory findings
Absolute lymphocytosis > 5 x 109/L
Normocytic normochromic anemia
Lymphocytic replacement of normal marrow
elements
Hypogammaglobulinemia
Autoimmune phenomena
Immune hemolytic anemia
Immune thrombocytopenia or neutropenia
*Coombs positive
Immunophenotype
CD markers include : 19, 20. HLA-DR(Ia)
Express weakly Ig M or D
CD5 and CD23 positive
Staging of CLL-RAI Classification
Determine the survival of the
Stage
Clinical features
0
Ab
lymphocytosis
I
Stage 0 +
patient
Survival (year)
>12.5
8.5
II
III
IV
HEMATOLOGY 6 WITH ONCOLOGY 7
enlarged LN
Stage 0 +
enlarged liver
/spleen +
lymphadenopath
y
0 + anemia
0+
thrombocytopen
ia
1.5
1.5
Stages 0 and 1 = observation
Staging Binet (Europeans)
Stage
Organ
Hemoglobin
enlargemen
t
A
012 areas
B
345 areas
>10
C
Not
<10
considered
Stages A and B = watchful waiting
Stage C = needs treatment
Treatment
Chrlorambucil DOC Phils
Purine analogs
fludarabine
Monoclonal antibodies
Campath-1H (anti-CD52)
Corticosteroids
Platelets
>100
And/or
<100
Das könnte Ihnen auch gefallen
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Chelators and Heavy MetalsDokument3 SeitenChelators and Heavy MetalsLucyellowOttemoesoeNoch keine Bewertungen
- IM Clinics History 2Dokument4 SeitenIM Clinics History 2LucyellowOttemoesoeNoch keine Bewertungen
- Tubulointerstitial DiseaseDokument94 SeitenTubulointerstitial DiseaseLucyellowOttemoesoeNoch keine Bewertungen
- Dr. N. Collantes - Learning To CommunicateDokument11 SeitenDr. N. Collantes - Learning To CommunicateLucyellowOttemoesoeNoch keine Bewertungen
- White Blood Cell DisordersDokument18 SeitenWhite Blood Cell DisordersLucyellowOttemoesoeNoch keine Bewertungen
- Introduction To LeukemiaDokument51 SeitenIntroduction To LeukemiaLucyellowOttemoesoeNoch keine Bewertungen
- Ventricular Action Potential: Cardiac CycleDokument1 SeiteVentricular Action Potential: Cardiac CycleLucyellowOttemoesoeNoch keine Bewertungen
- ENT Benign Laryngeal DisordersDokument6 SeitenENT Benign Laryngeal DisordersLucyellowOttemoesoeNoch keine Bewertungen
- IM IBD IBsDokument1 SeiteIM IBD IBsLucyellowOttemoesoeNoch keine Bewertungen
- ENT Benign Neck MassesDokument2 SeitenENT Benign Neck MassesLucyellowOttemoesoeNoch keine Bewertungen
- Cystic Fibrosis: Navigation SearchDokument15 SeitenCystic Fibrosis: Navigation SearchLucyellowOttemoesoeNoch keine Bewertungen
- ENT Diseases of Paranasal SinusesDokument3 SeitenENT Diseases of Paranasal SinusesLucyellowOttemoesoeNoch keine Bewertungen
- ENT Anatomy and Physiology of The Esophagus and Tracheobronchial TreeDokument1 SeiteENT Anatomy and Physiology of The Esophagus and Tracheobronchial TreeLucyellowOttemoesoeNoch keine Bewertungen
- Respiratory Volumes and CapacitiesDokument1 SeiteRespiratory Volumes and CapacitiesLucyellowOttemoesoeNoch keine Bewertungen
- Bowman's Capsule Proximal Tubule Distal TubuleDokument1 SeiteBowman's Capsule Proximal Tubule Distal TubuleLucyellowOttemoesoeNoch keine Bewertungen
- Principles of GeneticsDokument4 SeitenPrinciples of GeneticsLucyellowOttemoesoeNoch keine Bewertungen
- Body Mass Index (BMI), The Waist Circumference and The Waist/hip Ratio. Although Not ADokument2 SeitenBody Mass Index (BMI), The Waist Circumference and The Waist/hip Ratio. Although Not ALucyellowOttemoesoeNoch keine Bewertungen
- IM Infective Endocarditis Pericardial DiseaseDokument4 SeitenIM Infective Endocarditis Pericardial DiseaseLucyellowOttemoesoeNoch keine Bewertungen
- 2 PneumoniaDokument53 Seiten2 PneumoniaLucyellowOttemoesoeNoch keine Bewertungen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Effect of Inositol Sterioisomers at Different Dosages in Gestational DiabetesDokument8 SeitenEffect of Inositol Sterioisomers at Different Dosages in Gestational DiabetesMohsin HassamNoch keine Bewertungen
- Pedodontic Lect 20-21Dokument8 SeitenPedodontic Lect 20-21كوثر علي عدنان حسينNoch keine Bewertungen
- The Health Belief ModelDokument5 SeitenThe Health Belief ModelYerichu JNoch keine Bewertungen
- Potential of rDNA Technology in Revolutionizing FutureDokument23 SeitenPotential of rDNA Technology in Revolutionizing FutureNusra FaizNoch keine Bewertungen
- Buccal Midazolam CEWT Pi MidazDokument2 SeitenBuccal Midazolam CEWT Pi MidazAgnieszka WaligóraNoch keine Bewertungen
- Bacteria Cell CalloDokument16 SeitenBacteria Cell CalloAngelo CalloNoch keine Bewertungen
- ITLSAdvancedPre TestDokument8 SeitenITLSAdvancedPre TestMuhammad AsifNoch keine Bewertungen
- Checklist & Algoritma ACLSDokument16 SeitenChecklist & Algoritma ACLSNadhif JovaldyNoch keine Bewertungen
- HirsutismDokument19 SeitenHirsutismCita KresnandaNoch keine Bewertungen
- The Learning Curve For Laparoscopic Cholecystectomy PDFDokument5 SeitenThe Learning Curve For Laparoscopic Cholecystectomy PDFIgor CemortanNoch keine Bewertungen
- Emi Tesalonika - Rahametwau Askep Bahasa InggrisDokument7 SeitenEmi Tesalonika - Rahametwau Askep Bahasa InggrisSiva PutriNoch keine Bewertungen
- Reynold Dilag ResumeDokument3 SeitenReynold Dilag Resumeapi-283388869Noch keine Bewertungen
- UGIB Prob Sec To BPUD Vs Gastric Mass Alzheimer's DiseaseDokument7 SeitenUGIB Prob Sec To BPUD Vs Gastric Mass Alzheimer's DiseaseMonique Angela Turingan GanganNoch keine Bewertungen
- Toronto Notes Nephrology 2015 10Dokument1 SeiteToronto Notes Nephrology 2015 10JUSASBNoch keine Bewertungen
- Science 5 DLP 3 - PubertyDokument8 SeitenScience 5 DLP 3 - PubertyMark Cua100% (4)
- Influenza Virus Research and Funding Opportunities by John StambasDokument10 SeitenInfluenza Virus Research and Funding Opportunities by John StambasGCEIDNoch keine Bewertungen
- Multiple Questions SocDokument2 SeitenMultiple Questions SocbrinardNoch keine Bewertungen
- Nitrogen NarcosisDokument30 SeitenNitrogen NarcosisNancy Dalla DarsonoNoch keine Bewertungen
- Evidenced-Based Nursing I. Clinical QuestionDokument3 SeitenEvidenced-Based Nursing I. Clinical QuestionLemuel Glenn BautistaNoch keine Bewertungen
- Welcome AddressDokument55 SeitenWelcome AddressDiego RodriguesNoch keine Bewertungen
- OET Speaking Criteria ChecklistDokument4 SeitenOET Speaking Criteria ChecklistNobomita GhoshNoch keine Bewertungen
- OB Test 2 Study GuideDokument21 SeitenOB Test 2 Study GuideJaclyn FugateNoch keine Bewertungen
- Making The Best Clinical Decision DCNADokument18 SeitenMaking The Best Clinical Decision DCNAJohnNoch keine Bewertungen
- Management of Shock in TraumaDokument4 SeitenManagement of Shock in TraumaVictor Manuel Gutierrez AraujoNoch keine Bewertungen
- Drug Study SARAHDokument2 SeitenDrug Study SARAHirene Joy DigaoNoch keine Bewertungen
- HydrotherapyDokument25 SeitenHydrotherapyleilanurse100% (1)
- NCM 107 - RleDokument23 SeitenNCM 107 - RleMaxinne Allyssa Cancino RoseñoNoch keine Bewertungen
- Appendicitis NCPDokument5 SeitenAppendicitis NCPEarl Joseph DezaNoch keine Bewertungen
- BookBalkanMedicalWeek FINALDokument48 SeitenBookBalkanMedicalWeek FINALsome bodyNoch keine Bewertungen
- A Colour Atlas of FundosDokument132 SeitenA Colour Atlas of FundosMohammed HosenNoch keine Bewertungen