Beruflich Dokumente
Kultur Dokumente
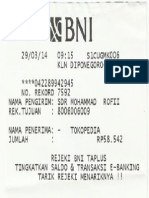
RULATIKAHBINTIABDGHANI2013
Hochgeladen von
Mohammad RofiiCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
RULATIKAHBINTIABDGHANI2013
Hochgeladen von
Mohammad RofiiCopyright:
Verfügbare Formate
PSZ 19:16 (Pind.
1/07)
UNIVERSITI TEKNOLOGI MALAYSIA
DECLARATION OF THESIS / UNDERGRADUATE PROJECT PAPER AND
COPYRIGHT
Authors full name :
NURUL ATIKAH BINTI ABD GHANI
Date of birth
16TH DECEMBER 1988
Title
BILIRUBIN LEVEL DETECTOR USING LABVIEW FOR JAUNDICE
TREATMENT
Academic Session :
2012/2013
I declare that this thesis is classified as :
CONFIDENTIAL
(Contains confidential information under the
Official Secret Act 1972)*
RESTRICTED
(Contains restricted information as specified by
the organization where research was done)*
OPEN ACCESS
I agree that my thesis to be published as online
open access (full text)
I acknowledged that Universiti Teknologi Malaysia reserves the right as follows:
1. The thesis is the property of Universiti Teknologi Malaysia.
2. The Library of Universiti Teknologi Malaysia has the right to make copies
for the purpose of research only.
3. The Library has the right to make copies of the thesis for academic
exchange.
Certified by
SIGNATURE
SIGNATURE OF SUPERVISOR
881216-05-5020
(NEW IC NO. /PASSPORT NO.)
PUAN MITRA BINTI MOHD ADDI
NAME OF SUPERVISOR
Date : 25th JUNE 2013
Date : 25th JUNE 2012
NOTES :
If the thesis is CONFIDENTIAL or RESTRICTED, please attach with the
letter from the organization with period and reasons for
confidentiality or restriction.
I hereby declare that I have read this thesis and in my
opinion this thesis is sufficient in terms of scope and quality for the
award of the degree of Bachelor of Engineering
(Electrical-Medical Electronic Engineering)
Signature
Name of Supervisor : PUAN MITRA BINTI MOHD ADDI
Date
: 25th JUNE 2013
BILIRUBIN LEVEL DETECTOR USING LABVIEW FOR JAUNDICE
TREATMENT
NURUL ATIKAH BINTI ABD GHANI
A report submitted in partial fulfillment of the
requirements for the award of the degree of
Bachelor of Engineering
(Electrical-Medical Electronic Engineering)
Faculty of Electrical Engineering
Universiti Teknologi Malaysia
JUNE 2013
ii
I declare that this report entitled Bilirubin Level Detector Using Labview For
Jaundice Treatment is the results of my own research except as cited in the
references. The report has not been accepted for any degree and is not currently
submitted in candidature of any other degree.
Signature
Name
: NURUL ATIKAH BINTI ABD GHANI
Date
: 25th JUNE 2013
iii
Blessing and peace be upon Prophet Muhammad S.A.W
This thesis is special dedicated to my beloved ibu and ayah
iv
ACKNOWLEDGMENT
Alhamdulillah. Thanks to Allah S.W.T for His blessing that has given me a
good health and strength and the opportunity to complete my final year project along
with the thesis. Throughout the journey from the beginning until my final war, I have
been through sweet and bitter memories to be remembered. But of course I am not
facing this war alone by myself because I have people who have always supported
me from behind.
First of all I would like to express my special thanks to my supervisor, Puan
Mitra Mohd Addi. Thank you for the supervision, support, guidance and
encouragement that really helped me a lot in my journey to complete my final year
project.
My great appreciation is dedicated to all my friends especially to all SEPs,
thanks for the support and friendship. My deepest gratitude to my ibu and ayah and
also my kakaks and abang for their endless love, advice, and encouragement
throughout my final year project.
Not to forget to my rowing team, thank you for being my second family in
UTM, whoever supported me directly or indirectly, may ALLAH bless all of you.
Thank you.
ABSTRACT
Phototherapy is a form of treatment for skin conditions using light and
commonly used to treat jaundice. Common light source used in phototherapy
devices include fluorescent lamp, halogen lamp, fiberoptic system and also LEDs.
Blue LEDs have been used as one of the light sources in phototherapy devices for
jaundice treatment. This is due to its unique characteristics which includes emission
of high intensity narrow band of blue light, power efficient, light in weight, less
heat production, low in cost and a longer lifetime. Previously, the Automated
Phototherapy Vest (APV) for infants was designed as an alternative device to
reduce bilirubin level jaundice babies. A bilirubin level detector is designed to
measure bilirubin level and several experiment were conducted to compare the
efficiency of blue LEDs in reducing bilirubin level in infants compared to
fluorescent light.
vi
ABSTRAK
Fototerapi adalah merupakan perubatan untuk keadaan kulit
menggunakan cahaya dan kebiasaannya digunakan untuk mengubati jaundis. Cahaya
yang biasa digunakan pada mesin fototerapi termasuk lampu kalimantang, lampu
halogen, system fiberoptik dan juga LED. LED biru telah digunakan sebagai salah
satu daripada punca cahaya dalam mesin fototerapi untuk mengubati jaundis. Ini
berikutan cirri-cirinya yang unik yang mana termasuklah pancaran intensiti yang
tinggi pada cahaya biru, kuasa yang efisien, ringan, penghasilan haba yang kurang,
murah dan mempunyai jangka hayat yang panjang. Sebelum ini, Automated
Phototherapy Vest (APV) untuk bayi telah direka sebagai satu langkah alternative
untuk mengurangkan paras bilirubin pada bayi jaundis,Pengesan paras bilirubin
direka untuk mengukur paras bilirubin dan beberapa eksperimen dijalankan untuk
membandingkan kecekapan LED biru dalam mengurangkan paras bilirubin pada bayi
berbanding dengan lampu kalimantang.
vii
TABLE OF CONTENTS
CHAPTER
TITLE
PAGE
DECLARATION
ii
DEDICATION
iii
ACKNOWLEDGEMENT
iv
ABSTRACT
ABSTRAK
vi
TABLE OF CONTENT
vii
LIST OF TABLES
LIST OF FIGURES
xi
LIST OF ABBREVIATION
xiii
LIST OF APPENDICES
xiv
INTRODUCTION
1.1 Background of study
1.2 Problem statement
1.3 Objectives
1.4 Scope
1.5 Thesis overview
viii
LITERATURE REVIEW
2.1 Hyperbilirubinemia (Jaundice)
2.2 Bilirubin
2.2.1 Metabolism
2.2.2 Measuring tools & devices
2.3 Phototherapy
11
2.3.1 Light sources of phototherapy devices
12
2.3.2 Efficacy of phototherapy lights
16
2.4 Phototherapy treatment in vitro and in vivo
19
research studies
2.5 Automated Phototherapy Vest (APV)
3
24
METHODOLOGY
3.1 Project Overview
26
3.2 Experimental Preparation
27
3.2.1 Bilirubin Solution Preparation and Detection
28
using Spectrophotometer
3.2.1.1 Spectrophotometer Wavelength
30
Determination
3.3.1.2 Bilirubin Calibration Curve
3.2.2 Light Exposure
31
32
3.2.2.1 Blue LEDs
32
3.2.2.2 LEDs Arrangement and Design
33
Considerations
3.2.2.3 Fluorescent Light
3.3 Software Development
3.3.1 Importing Data into LabView from
35
36
36
Spectrophotometer
3.3.2 Bilirubin Reading using LabView
3.4 Flow Chart
4
39
40
RESULT AND DISCUSSION
4.1 Determination of Optimum Wavelength
42
4.2 Relationship between Absorbance and Bilirubin
43
Concentration
ix
4.3 Bilirubin Degradation Experiment A
45
Comparison between Different Light Sources
4.3.1 LEDs Circuit Design
45
4.3.2 Bilirubin Degradation Experiments
46
4.4 Bilirubin Level Detector using LabView
48
4.5 Discussion
50
4.5.1 Interference during Experiments
5
51
CONCLUSION AND RECOMMENDATIONS
5.1 Conclusions
52
5.2 Recommendation for future work
53
REFERENCES
54
APPENDICES
56
LIST OF TABLES
TABLE NO.
TITLE
PAGE
2.1
Comparison of phototherapy devices
15
2.2
Practice consideration for optimal administrative of
18
phototherapy
3.1
Different bilirubin concentration
29
4.1
Wavelength determination
43
4.2
4.3
Relationship between absorbance and
concentration
Results for the light exposure experiment
4.4
Comparison of both light sources
bilirubin
44
47
47
xi
LIST OF FIGURES
FIGURE
TITLE
PAGE
NO.
2.1
Bilirubin metabolism
2.2
Babys blood sample taken from the heel
2.3
Urine strip reagent
2.4
Bilirubin level measurement using bilirubinometer
10
2.5
Visible range of lights
11
2.6
Fluorescent tube in Olympib BiliLite
12
2.7
Halogen spotlight
13
2.8
BiliSoft LED
14
2.9
Natus neoBLUE LED
14
2.10
Important factors in the efficacy of phototherapy
17
2.11
19
2.12
Comparison of both in vitro and in vivo efficacy of
bilirubin degradation between the blue LED and
conventional phototherapy unit
Efficacy comparison between LEDs
2.13
Comparison of efficacy between different light sources
21
2.14
Comparison of in vitro efficacy
phototherapy device
Absorbance spectrum of light exposure
22
2.15
of
existing
20
23
23
2.17
Bilirubin degradation percentage using sunlight and
conventional phototherapy
APV Full set-up
3.1
Block diagram of the project
26
3.2
Absorbance determination
29
3.3
Absorbance color chart
30
3.4
Example of calibration curve
31
3.5
Blue LED
33
3.6
AAP guidelines for all gestational ages
34
2.16
24
xii
3.7
Fluorescent tube
35
3.8
Block diagram
36
3.9
37
3.10
(a) Input port detection
(b) Read input data
Output data from spectrophotometer
3.11
Elimination process
38
3.12
Result after elimination process
38
3.13
Bilirubin level detection
39
3.14
Spectrophotometer sample racks
40
3.15
Flowchart of the experiment
41
4.1
Preparation of different bilirubin concentrations
43
4.2
44
4.3
Calibration curve of absorbance vs concentration for
bilirubin solution
LEDs circuit
4.4
Bilirubin degradation experiments
46
4.5
48
4.6
Comparison of bilirubin degradation in blue LED and
fluorescent light (in percentage difference)
User interface of bilirubin level detector
4.7
Exporting data into Excel
50
37
45
49
xiii
LIST OF SYMBOLS & ABBREVIATION
LabVIEW
Laboratory Virtual Instrumentation Engineering Workbench
AAP
American Academy of Pediatric
APV
Automated Phototherapy Vest
LED
Light-emitting diode
BSA
Body Surface Area
nm
nanometer
W/cm2/nm
microwatt per centimeter square per nanometer
cm2
Centimeter square
mg/dL
Milligram per deciliter
mol/L
Micromol per liter
DC
Direct Current
xiv
LIST OF APPENDICES
APPENDIX
TITLE
PAGE
NO.
A
UV-Visible Spectrophotometer
56
RS 232 Port Line
59
Completed Block Diagram
61
LabView User Interface for Blirubin Level
Detection Using LabView for Jaundice Treatment
62
CHAPTER 1
INTRODUCTION
1.1
Background of Study
Jaundice or hyperbilirubinemia is the yellow discoloration of the skin, sclera
(white of the eyes) and other tissues due to excessive bilirubin in the blood. It is
common disease in newborn infants, where 60% of term and 80% of preterm
neonates develop jaundice in the first week of life. It was also found that at one
month of age, these newborns are still jaundiced for 10% of breastfeed babies [1].
Most of the infant happened to have some mild jaundice and the condition.
Normally, most infants happened to have a mild jaundice which is temporary and
not too dangerous. However, these infants must be monitored closely as it can
cause the development of a more serious condition for the baby such as kernicterus.
Kernicterus happens due to excessive jaundice which can cause damage to the
infantss brain [2]. The condition can also cause loss of hearing, late development
in growth and yellow staining of the basal ganglio which can lead a baby to death
[1].
Bilirubin is actually a normal part of the red blood cells. When the body
breaks down the red blood cells, the old red blood cells will be removed by the liver
from the system. Extra bilirubin will then be stored in the skin and when this
happens, it causes the babys skin to become yellow. A normal infant should have a
bilirubin level of less than 35mol/L or 2mg/dL [2]. When the bilirubin reading is
more than the normal reading, treatment is required to reduce the bilirubin level.
In the early 1950s, sunlight was recognized as a treatment to reduce
jaundice in infants. The treatment was found by a nurse in England who observed
that jaundiced infants became less yellow after a certain period of exposure under
the sun [3]. The observation has led the future researchers to conduct an experiment
using blue fluorescent tubes as light sources to treat jaundice. The result showed
that bilirubin level in infants declined when they were exposed to the blue
fluorescent tubes, which led to the introduction of phototherapy.
Until now, phototherapy has been widely used as a jaundice treatment for
more than four decades [4]. Design of devices had been developing throughout the
years, with the aim of reducing bilirubin level efficiently at shorter exposure
duration. The available light sources used in phototherapy devices include
fluorescent tubes, halogen spotlights, fiberoptic systems and LEDs. There are
advantages and disadvantages of using these light sources depending on their own
specifications and requirement. There are several factors that determine the
efficiency of these phototherapy lights; spectral qualities, irradiance (light
intensity), exposed body surface area, duration of exposure, skin thickness and
pigmentation, and the amount of bilirubin degradation [5]. Suitable wavelength
used is 400nm to 520nm 2ith a peak of 460 10nm, which is in the range of blue
spectrum [5]. Bilirubin is found to be more sensitive to blue and blue-green regions
of the visible spectrum as it is closer to the bilirubin absorbance spectrum [6].
1.2
Problem Statement
Phototherapy treatments are commonly conducted in hospitals which may
taje several days. Most hospitals have sufficient numbers of phototherapy devices
to treat jaundice patients. However, in some developing countries and third-world
countries, there are limited numbers of these devices which may cause a longer
waiting period between patients. Due to this condition, a portable phototherapy
device was introduced to make phototherapy treatment available everywhere.
A design of an Automated Phototherapy Vest (APV) was proposed as an
alternative device to help reduce bilirubin level in infants. The APV which used UV
LEDs as the light source was found to be low in cost. This is a positive indicator
that it may be affordable to be used by patients in rural areas, especially those in the
third-world countries. However, there were several limitations of the current APV
which includes uneven LED brightness.
Thus, the type of LED was changed to blue LED as previous researches has
found that it is he most efficient in reducing bilirubin level of infants with jaundice.
However, the efficiency of the blue LEDs to be used on the APV are yet to be
proved.
1.3
Objectives
The main objective of this project is to verify that blue LEDs that are to be
used on the Automated Phototherapy Vest is able to reduce bilirubin level
effectively compared to other conventional phototherapy light sources. in vitro
experiments using bilirubin solution will be conducted to verify this. A bilirubin
level detector will also be designed using LabView as a measuring instrument for
the in vitro experiments.
1.4
Scope
The scope of this project includes:
Preparing bilirubin solution in accurate measurement
Developing a calibration curve which explains the relationship between
absorbance and concentration of bilirubin level in bilirubin solution.
Conducting in vitro experiments using bilirubin solution which are exposed
to blue LED and fluorescent lights.
Designing a user interface to analyze bilirubin degradation of bilirubin
samples and displaying the result in LabView
1.5
Thesis Overview
The thesis is organized into five main chapters.
Chapter 1 briefly explains the overview of the project, problem statements,
objectives and also scopes of the project.
Chapter 2 discusses about the basic concept of jaundice, bilirubin
mechanism, jaundice treatment and bilirubin measuring tools. The literauter review
discuss on this chapter are based on previous studies conducted by researchers that
covers the comparison between the efficiency of LED with other light sources used
in jaundice treatment.
Chapter 3 focuses on the methodology used in the project which explains on
the sequence of the experiment conducted and also description of the software and
hardware used in the project.
Results and analysis of the experiments are discussed in Chapter 4. The
overall functions of the bilirubin level detector are also explained in this chapter.
The last chapter provides a conclusion from the in vitro experiments
including future work and recommendations of the project.
CHAPTER 2
LITERATURE REVIEW
2.1
Hyperbilirubinemia (Jaundice)
Hyperbilirubinemia or jaundice is a common disease encountered by
infants. Over 60% of newborn develop jaundice by 48 to 72 hours of age in the
early weeks of birth [7]. Jaundice happens when the amount of bilirubin in blood is
higher than the normal rate which is less than 2mg/dL. Hight bilirubin level in
blood causes a yellowing discoloration effect which is mostly noticeable on the skin
and whites of the eyes. Early stage of jaundice, termed as physiological jaundice is
generally harmless [1]. However, the condition may get serious and worsen infants
health. Prolong jaundice develop kercniterus which is a disease that cause brain
damage when bilirubin is spread to the brain. infants may also loss their hearing,
delay in growth development, suffer sequalae like athetoid cerebral palsy, paralysis
of ipward gaze and dental dysplasia [8]. Traditionally, sunlight used as a jaundice
treatment to cure jaundice infants. Infants will be exposed to sunlight everyday for
about 20 to 30 minutes and bilirubin were monitored once is complete. Since
sunlight can be hazardous to infants, phototherapy technology has been improved to
make the treatment easier and faster.
2.2
Bilirubin
2.2.1 Metabolism
Figure 2.1: Bilirubin metabolism
Bilirubin is a part of the red blood cells. For an adult, the life span of the red
blood cells is 120 days and will be excreted through urine or stool after that period.
As the red blood cells breakdown, the hemoglobin will degrade into globin and
heme. The heme molecule will break apart and convert into bilirubin, an orangeyellow pigment. The process occurs in the reticuloendothelial cells which include the
liver, spleen and bone marrow. Bilirubin starts out as unconjugated bilirubin which is
not water soluble. The unconjugated bilirubin reacts with glucoric acid once it is
transported to the liver. After biochemical alteration in the liver, the unconjugated
bilirubin becomes conjugated bilirubin which is more soluble. It is then excreted into
the bile and goes through the gall bladder into the gut. At this stage, there is a variety
of pigments created when the bilirubin changes. 80% of the pigments which are
called stercobilin will be excreted in the feces and the other 20% called uribilinogen
will be reabsorbed to the liver and back into the blood. About 90% of uribilinogen in
the liver will be re-excreted into the bile and the other 10% goes into the blood to be
transported to the kidneys.
Compared to an adult, the liver of a newborn baby is immature and is not able
to remove extra bilirubin efficiently. Besides that, their red blood cells have a shorter
life span compared to an adult [1]. This is because the quantity of unconjugated
bilirubin to be converted into conjugated bilirubin has exceeds the capacity of the
liver [9]. When this happens, the bilirubin is stored in the skin giving it a yellow
discoloration which is known as jaundice. Besides that, incompatibility between
motjers and infants blood group may also lead to the development of jaundice.
Furthermore, infants of diabetic mothers, premature infants and also infants who a
born with a lot of bruising to their scalp or face may also have a high risk of getting
jaundice [10, 11].
2.2.2 Measurement Tools & Devices
Bilirubin measurement tools and devices are used to measure the level of
bilirubin in infants blood to evaluate the liver function. These tools and devices
utilized to diagnose the circulation level of bilirubin of the infants liver whether it is
normal or abnormal and to determine if jaundice is still present [12]. It helps doctor
to diagnose jaundiced infants whether on-going phototherapy treatment is needed.
Bilirubin measurements can be conducted in two ways, invasive or non-invasive. It
includes blood test, urine test and also bilirubinometer.
a)
Blood Test
Figure 2.2: Blood sample taken from an infant's heel
Blood test is the most common method used in hospitals to measure bilirubin
level. Blood sample is taken from the infant by puncturing the heels with a small
needle rather than from their veins. This is because an infants vein is very small and
it can be easily damaged. The blood sample is taken to the laboratory for diagnoses.
However, this method is invasive, painful, costly and may be risk the infants to
infection. Moreover, it can cause significant blood loss which is a concern in preterm
infants when repeated blood sampling is conducted [13].
b)
Urine Test
Figure 2.3: Urine strip reagent
10
The procedure is done by dipping the reagent strip into the urine sample and
removing it immediately to avoid dissolving of the reagent pads. The color change
on the reagent strip is compared to the corresponding color chart on the bottle label.
How ever, the result from this measurement method is unreliable due to color
interference and interpretation. Sample of urine should not be exposed to light since
bilirubin is very sensitive to light and will lead to inaccurate test results.
c)
Transcutaneous Bilirubinometry
Figure 2.4: Bilirubin level measurement using bilirubinometer [14]
The latest
technology in
bilirubin
measurement is
transcutaneous
bilirubinometry. It is preferable as it is a non-invasive method and is able to provide
accurate measurements instantaneously. It works by directing the light into the skin
and measureing the intensity of specific wavelength that is reflected from the
newborns tissues. These optical signals are converted into electrical signal by a
photocell. The signal are analyzed by a microprocessor to generate a serum bilirubin
value in mol/L or mg/dL [14]. The commonly used site to measure bilirubin level is
on the forehead and upper end of sternum.
11
2.3
Phototherapy
In the early 1950s, a nurse, Jean Ward from Rochford General Hospital in
Essex, England had recognized that when jaundiced infants were exposed to the sun
they become less yellow. The observation has led a pediatric resident, R.J. Cremer to
conduct an experiment. The first experiment was to expose the naked infants to
direct sunlight alternating with shades for 15 to 20 minutes. The experiment resulted
in the decreasing of bilirubin level. This further led Cremer and his team to design a
phototherapy apparatus using blue fluorescent tubes. The lamps emitted light in a
spectral range of 420nm 480nm and the treatment was given interrupted
intermittently [15]. Bilirubin level was found to drop using these blue fluorescent
tubes and this is how phototherapy was first introduced. The findings had led many
more researchers to conduct research on different phototherapy treatment [3].
Figure 2.5: Visible range of lights
12
2.3.1 Light Sources for Phototherapy Devices
Phototherapy is a form of treatment for jaundice. There are several
phototherapy devices that are available to be used for jaundice treatment includes
Olympic BiliLIte, BiliSoft LED and etc. Each of these light sources has their own
specifications, advantages, disadvantages and usage requirement [11].
a)
Fluorescent Tubes
Figure 2.6: Fluorescent tubes in Olympic BiliLite [16]
Fluorescent tube is the commonly used light source in phototherapy as it is
available in most hospitals. Figure 6 displays a phototherapy unit by Olympic
BiliLite that uses special blue fluorescent tubes as the light source. The standard
distance for light exposure is 40cm which is able to deliver an irradiance of
11W/cm2/nm while for special blue tubes it can deliver the irradiance up to
24W/cm2/nm but at the distance of 14cm [5]. Even though fluorescent tubes are
inexpensive and can be easily get, its light intensity reduces with time and need to be
replaced after every 1,000 to 2,000 hours of usage [6].
13
a)
Halogen spotlights
Figure 2.7: Halogen Spotlight
The examples of phototherapy unit that used halogen spotlight is Ohmeda
BiliBlanket Plus, Datex-Ohmeda Spot Phototherapy Lamp and Hill-Rom Microlight
Phototherapy. Ohmeda BiliBlanket Plus can be applied directly to neonates because
there is no heat produced whereas the other two phototherapy units must be placed
about 50cm from neonates. Halogen spotlight is able to provide fairly high irradiance
exceeding 20W/cm2/nm [5]. This light source should not be applied too closely and
borne in mind when used for treatment because it tend to generate considerable heat
that will cause thermal injury to infant [5, 6]. It is also must be properly shielded
because it can emit ultraviolet radiation and some other clinical responses.
b)
Fiberoptic System
Fiberoptic system has been intoduced for jaundiced treatment since late
1980s that consist of a light that delivered to halogen bulb from a tungsten through a
fiberoptic cable and emitted from the sides and end of the fibers inside a plastic pad
[3]. It can be used directly to the infants and can deliver the irradiance up to
35W/cm2/nm and able to determines the uniformity of light emission. Fiberoptic
14
system has an advantages over conventional phototherapy since it does not need an
eye patches for covering infants eyes and infant can be held during the phototherapy
treatment [5]. However, this phototherapy can only cover small body surface area
and it led to decreasing the spectral power of fiberoptic systems. Figure 2.8 shows
the example of fiberoptic system.
Figure 2.8: BiliSoft LED
c)
LEDs
Figure 2.9: Natus neoBLUE LED, courtesy of Natus Medical Incorporated
The latest technology phototherapy devices using high intensity blue LEDs
that has many advantages over the other conventional light sources. It has been used
15
as the prototype of phototherapy devices since 1990s [6]. Blue LED has been widely
used nowadays in medical devices because of its unique characteristics. LED
produce less heat so it can be use directly to infants without cause any injury and it
can deliver output energy up to 100W/cm2/nm [11]. LED have longer lifetime
which it can be used for more than 20,000 hours, emit high intensity (250mW/cm2)
with narrow-band light in the spectrum (470 60nm or 470 15nm FWHM)[5] and
it resulting in shorter treatment times [4]. Besides that, it is also power efficient, low
in cost, light in weight, low energy requirement and emit little infrared with no
ultraviolet radiation [4, 5, 17]. A research has found that LED can be effective as
conventinal phototherapy when it is used at a low irradiance of 5 to 8W/cm2/nm
[3].The examples of phototherapy devices that using blue LEDs technology is Natus
neoBlue as in Figure 2.9.
Table 2.1: Comparison of phototherapy devices[11]
Minimum
Device
Lamp source
recommended
Is the
treatment distance
effective
(mW.cm-2)
light field
>700cm2
Draeger Photo-
Folded fluorescent
Therapy 4000 Unit
3.39 (4 blue tubes and
Yes
2 white tubes) 4.07 (6
blue tubes)
Draeger Heraeus
Gas discharge bulb
5.03
Yes
Halogen bulb
4.83
No
Natus neoBLUE LED
LEDs 852 Blue
2.29
Yes
Phototherapy
320 Yellow
System
13 Red
Phototherapy Lamp
Ohmeda BiliBlanket
Plus
16
2.3.2 Efficacy of Phototherapy Lights
Since phototherapy was first evaluated in 1990s, during this period of time,
methods for reporting and measuring phototherapy doses are not standardized [18].
Phototherapy generally used according to the guidelines published by the Americans
Academy Pediatrics in 2004 [19]. Phototherapy is well known as the standard
treatment for jaundiced infants. Many researchers had conducted a research to
determine the efficacy of phototherapy for jaundice treatment. Since it first invented
in 1950s, there is a lot of research has been done in order to improve the applications
of phototherapy units with higher efficacy and safe to be used
The efficacy of phototherapy is depends on the following factors:
i.
Wavelength range and peak
ii.
Light intensity (irradiance)
iii.
Body surface area (BSA) exposure
iv.
Skin thickness and pigmentation
v.
Duration of exposure
vi.
Decreasing of total bilirubin concentration
Bilirubin is a yellow coloring pigment that very sensitive to light. Bilirubin
absorption spectrum is used as the basic to design a phototherapy light sources [5].
Blue light is most effective for phototherapy because increasing of wavelength cause
transmittance of skin increased. The best wavelength to be use is 400nm to 520nm
with the peak centered around 460nm 10nm because at this range it is most closely
to the bilirubin absorption spectrum [5, 19]. This result has been proven in both in
vitro and in vivo experiments in order to determine the degradation of bilirubin. To
maximize the area exposed to light, change the infants posture for every 2 to 3 hours
so that when the area of exposure is greater, the greater the decreasing of bilirubin
total rate [18].
17
Skin thickness and pigmentation has been reported to obstruct the
phototherapy efficacy. Besides that, the longer time taken for phototherapy exposure
to infants resulting in increasing rate of decline in total bilirubin levels [5]. For an
effective treatment, within 4 to 6 hours initiation treatment it should be able to
decrease more than 2mg/dL (34mol/L) in serum bilirubin concentration. Figure
2.10 shows important factors in the efficacy of phototherapy that should be taken
into account. The important factors that need to be considers as shown in Table 2.2.
Figure 2.10: Important Factors in the Efficacy of Phototherapy[19]
18
Table 1.2: Practice Considerations for Optimal Administration of Phototherapy[18]
Checklist
Recommendation
Implementation
Light source (nm)
Wavelength spectrum in
Know the spectral
460- 490nm blue-green light
output of the light
region
source
Light irradiance
Use optimal irradiance:
Ensure uniformity
(W/cm2/nm)
30W/cm2/nm within the
over the light
460 to 490nm waveband
footprint area
Expose maximal skin area
Reduce blocking of
Body surface area (cm2)
light
Timeliness of
Urgent or crash-cart
May conduct
Implementation
intervention for excessive
procedures while
hyperbilirubinemia
infant is on
phototherapy
Continuity of therapy
Briefly interrupt for feeding,
After confirmation
parental
of adequate
bonding, nursing care
bilirubin
concentration
decrease
Efficacy of intervention
Periodically measure rate of
Degree of total
response in bilirubin load
serum/ plasma
reduction
bilirubin
concentration
decrease
Duration of therapy
Discontinue
at
desired Serial
bilirubin
bilirubin threshold; be aware measurements
of possible
based on rate of
rebound increase
decrease
19
2.4
Comparison of Phototherapy Research Studies
Several researches were conducted to identify the best and effective light
source for jaundice treatment. Many researchers have found that the use of blue LED
for phototherapy treatment is more efficient compared to the other light source.
These researches were carried out by comparing the percentage of bilirubin
degradation when the solution exposed to the LEDs and other phototherapy light
source. They were also conducted an experiment by comparing the effectiveness of
existing phototherapy available in market. Below are the results from the study
conducted:-
a)
LEDs vs Halogen Bulb [4]
In vitro and in vivo Efficacy of New Blue Light Emitting Diode Phototherapy
Compared to Conventional Halogen Quartz Phototherapy for Neonatal
Jaundice
Figure 2.11: Comparison of both in vitro and in vivo efficacy of bilirubin
degradation between the blue LED and conventional phototherapy unit [4]
A research conducted by Korean Team entitled as stated above compared the
percentage of bilirubin degradation for in vitro and in vivo experiment using LED
20
and Halogen Bulb as the photoherapy light source. For in vitro experiment, bilirubin
solution was exposed to this light source for 5 hours at room temperature at 45 cm
distance. While for in vivo experiment, twenty of 8-day old jaundiced Gunn rats
were used and exposed to each light source for 5 hours at room temperature at 45 cm
distance. Based on the result in Figure 2.11, the researcher has found that the
percentage of bilirubin degradation is higher when using blue LED compared to the
conventional phototherapy. It is proven in both in vitro and in vivo experiment. After
the exposure time, the percentage of bilirubin degradation when using blue LED
increased to 44% for in vitro and 30% for in vivo meanwhile when using
conventional light source the percentage of bilirubin is 35% and 16% for both in
vitro and in vivo respectively. It can be concluded that the study conducted shows
that LED light source is more efficient than conventional light source for degradation
of bilirubin. The efficacy is determining by two major factors which is the
wavelength and the intensity of the light emitted during phototherapy.
b)
Blue LED vs different color of LED and other light sources [17].
Light-Emitting Diodes: A Novel Light Source for Phototherapy
Figure 2.12: Efficacy comparison between LEDs [17]
21
Another research is by Vreman and his team. They has conducted an
experiment by comparing the efficiency between different colors of the LEDs and
also compared the efficiency of phototherapy light sources (Mini Bili Lite,
BiliBlanket, Photo-Spot, and Bili Lite). Based on the result in Figure 2.12, blue LED
has proven to be able reduced the bilirubin level by 28% followed by blue-green
LED, white light and green LED with the percentage of bilirubin degradation is 18%,
14% and 11% respectively. The in vitro efficacy of bilirubin degradation was then
compared blue LEDs with several conventional phototherapy devices and the result
as in Figure 2.13.
Figure 2.13: Comparison of efficacy between different light sources
Based on the result, the greatest irradiance and the most effective light source
for bilirubin degradation are when using blue LED. The other light source has
significantly different in their ability for bilirubin degradation except for Mini BiliLite and BiliBlanket where both of them had almost the same result [17].
22
c)
LED vs Existing Phototherapy Devices [20].
In Vitro Efficacy Measurements Of Led-Based Phototherapy Devices
Compared To Traditional Light Sources In A Model System
Figure 2.14: Comparison of in vitro efficacy of existing phototherapy devices [20]
This research was conducted by Vreman and his team during EASL
International Bilirubin Workshop in 2004. This experiment is comparing the existing
phototherapy product in market. They use the same bilirubin solution but different
type of phototherapy. Based on the time taken to reduce bilirubin level, PortaBed and
neoBlue which using blue LEDs is shorter than the other phototherapy devices. The
most efficient phototherapy devices is PortaBed which is it has higher irradiance and
can reduced bilirubin level in shorter time. Irradiance is not the primary factor to
determine the efficacy for both preterm and term neonates eventhough the maximum
irradiance levels between phototherapy devices vary widely [20]. The important
factors to determine the potential efficacy of a device such as the quality of the light,
size of the subject, mean irradiance of the treatable BSA, and percentage treatable
BSA [20].
23
d)
Sunlight vs Conventional Phototherapy [9].
Can sunlight replace phototherapy units in the treatment of neonatal jaundice?
An in vitro study
Figure 2.15: Absorbance spectrum of light exposure [9]
Figure 2.16: Bilirubin degradation percentage using sunlight and conventional
phototherapy [9]
24
Some researcher found that sunlight can be an alternative to replaced
phototherapy in jaundice treatment. In his research, Fadhil M. Salih reported that the
absorbance of bilirubin is higher when sunlight is used compared to phototherapy
unit for the same time interval. The percentage of bilirubin degradation is close when
using sunlight and phototherapy unit. Sunlight can well be suggested as an
alternative source of light in the treatment of neonatal jaundice in circumstances
where phototherapy units are not available such as at third world countries or at
developing countries [9]
However, the time of sunlight exposure must be monitored very carefully and
should be in short time. This is because sunlight could impose biological hazard as it
contains a considerable amount of ultraviolet radiation [9].
2.5
Automated Phototherapy Vest (APV)
Figure 7: APV Full Set-up [11]
25
The Automated Phototherapy Vest (APV) was designed as an alternative
phototherapy device to help in reducing bilirubin level, by exposing infants under
UV LED lights [11]. The device is able to monitor an infants body temperature. It
will automatically turn OFF once the infants body temperature exceeds the set
temperature. Addition to that, the APV requires a low power which is 7.5V, it easy to
use and can be comfortably operated either in hospitals or at home. With the
Breastfeeding mothers can feed their babies easily while treatment is still in progress.
The APV also has some safety features as one of its advantages. It will send an
alarm to indicate that the treatment time is over and will also turn off automatically
once the treatment session ended. This is a precautious action to prevent babies from
being exposed to excessive UV light.
However, there are several limitations on this first APV prototype. One of the
limitation is the brightness of the UV lights are uneven. When this happens, the
lights that are exposed to the baby will have produce different irradiance. This may
due to the type of LEDs that are not able to provide a uniform light ignition. The use
of Blue LED is proposed to overcome this limitation. The UV-LED has a wavelength
of 385nm 395nm while blue LED has a wavelength in the range of 460nm
480nm. UV-LED may be able to reduce bilirubin level in infants body but not as
efficient as blue LED. This is because bilirubin has a peak absorption in the range of
450nm 470nm and it matches better with the wavelength of blue LED. Besides
that, UV-LED has a low power emission which is 80mW. The power emission for
the blue LED is much higher, which is 180mW. In addition to that, the difference in
sizes between blue LED (10mm in diameter) and UV-LED (5mm in diameter) may
cause the blue LED to be able provide higher luminous intensity compared to UVLED.
CHAPTER 3
METHODOLOGY
3.1
Project Overview
Figure 3.1: Block diagram of the project
Figure 3.1 illustrates the block diagram of the project. First of all, bilirubin
solution will be prepared before conducting the experiment. Solution of bilirubin will
be prepared by dissolving it in a buffer solution which contain Sodium Hydroxide
27
(NaOH) and saline for further dilution and filled into clear cuvette. The clear cuvette
containing bilirubin concentration will be exposed to different light sources which
are the blue LEDs and fluorescent light at certain distance for a certain period of
time.
The absorbance value for the bilirubin concentration will be recorded before
and after the light exposure using a UV-Spectrophotometer. The spectrophotometer
measures the light absorbed by the solution and the output produced was in term of
absorbance and transmittance. Sample solutions placed into the spectrophotometer
represent the bilirubin concentration before the light exposure, and sample after the
light exposure for blue LED and fluorescent light. Spectrophotometer will measure
the absorbance of the bilirubin concentration one sample at each time. Then, the
absorbance value will convert the data into concentration. This output will be linked
into the LabView programming by using RS232 to calculate the bilirubin
concentration. The value of concentration will be displayed in Graphical User
Interface (GUI) for comparison purpose.
3.2
Experimental Preparation
The experimental part for this project can be divided into two parts which is
bilirubin detection using UV-Spectrophotometer and light exposure for bilirubin
level degradation. We need to do the preparation for both experiment and the
specification will be explained below.
28
3.2.1 Bilirubin Solution Preparation and Detection using Spectrophotometer
For the first part of the experiment, we need to prepare 17 samples of
bilirubin concentration. There is a specification needed for the preparation to be
followed. First, 5 mg of bilirubin was dissolved in 10 ml of 0.05 M Sodium
Hydroxide (NaOH). This mixture will be used as the stock solution for the next
dilution preparation. This stock solution stored in a brown glass container and we
need to prepare the fresh solution for every experiment. Then, make several dilution
of bilirubin standard solution from 50 mg/dl to 500 mg/dl by dilute the stock solution
with saline. Table 3.1 shows the different bilirubin concentration and the amount
needed for the mixture.
After each of the different concentration are prepared, bilirubin solution filled
into the clean clear cuvette. The cuvette must be clean and not scratched to ensure
that the reading obtain is accurate. Then, the cuvette will be placed inside the sample
rack of the spectrophotometer. The absorbance value for each concentration was
measured and recorded. Before that, we need to pre-heating the spectrophotometer
for about 30 minutes so that the spectrophotometer reading is in stable condition and
will give the accurate value.
Figure 3.2 shows the basic routine operations of the spectrophotometer. Preheating is required for the lamp and the electronic parts to reach heat balance. The
wavelength is set to the desired value. 100%T adjustment and zero adjustment are
done in order to get the accurate measuring status. The scale is then set to
Absorbance and the sample is put into the light path. . The data will be displayed at
the LED display window.
29
Figure 3.2: Absorbance determination
Table 3.2: Different bilirubin concentration
Bilirubin concentration
Stock solution (mL)
Saline (mL)
(mg/dL)
50
0.30
5.70
100
0.60
5.40
150
0.90
5.10
200
1.20
4.80
250
1.50
4.50
300
1.80
4.20
350
2.10
3.90
400
2.40
3.60
450
2.70
3.30
500
3.00
3.00
30
3.2.1.1 Spectrophotometer Wavelength Determination
A spectrophotometer was used to measure the amount of light that passes
through the solution and measure the light absorbed by the solution to determine the
concentration of solutes at certain wavelength. The working principle follows the
Beer Lamberts Law which relates the absorption of light travelling through the
properties of the material. Beer and Lambert also found out that the relationship of
the absorbance of the solution is linear to the concentration of an absorbing solute.
Before the analysis or conducting the experiment, we need to identify the wavelength
at which will give the maximum absorbance value. This is because the wavelength
determined will be used for the next analysis or experiment. The unit of the
wavelength is in nm.
Determination of the wavelength was done by choosing one of the solution
prepared; in this experiment 500 mg/dl concentration was used. Note that bilirubin is
in yellow color which will absorb blue-violet light which at the wavelength from
560nm to 600nm. As stated in Figure 2.10 in Chapter 2, blue light was found to be
the most effective light absorbed to reduce bilirubin level. Thus, the maximum
absorbance value can be determined and will be used for the whole experiment.
Figure 3.3 can be a reference for the color absorbed and its observed color.
Figure 3.3: Absorbance color chart
31
3.2.1.2 Bilirubin Calibration Curve
The purpose of measuring the absorbance value for each of the different
concentration is to obtain the calibration curve of the bilirubin. We can determine the
concentration of the bilirubin by using a calibration curve where it will translate the
absorbance values into concentration values.
The calibration curve, Figure 3.4 was constructed by plotting a graph of
absorbance versus bilirubin concentration. Then, a straight line curve is created.
From the calibration curve, we can determine the linear equation for the solution.
Equation 3.1 is a linear equation, y = mx + c, where m is the slope and c is the yintercept. We can also calculate the concentration value manually by draw a
horizontal line to the calibration curve line once we identify the absorbance value at
y-axis. Then, draw a vertical line from the intersection to the x-axis to determine the
concentration value.
Ralationship between Absorbance and
Concentration
0.25
Absorbance
0.2
0.15
0.1
0.05
0
-100
-0.05
100
300
500
700
Concentration (mg/dl)
Figure 8: Example of calibration curve
900
32
y = mx + c
(Eq. 3.1)
y: Absorbance value
m: Slope
x: Bilirubin concentration
3.2.2 Light Exposure
The second part of the experiment is the light exposure to the bilirubin
concentration. There are two types of light used in this experiment which is blue
LEDs and fluorescent light. This experiment was conducted to determine the
efficiency of blue LEDs compared to fluorescent light by comparing the level of
bilirubin degradation after the exposure. Besides, this experiment is also to determine
the relationship between absorbance values and the bilirubin level degradation with
the exposure time.
3.2.2.1 Blue LEDs
The 10mm blue LED as shown in Figure 3.5 is one of the light sources used in
the experiment. Blue LEDs was chosen because researches has found that it is able
reduce bilirubin effectively compared to other LEDs and also other phototherapy
light source [17]. This is also because of it unique characteristics which is it emit a
higher intensity, light in weight, less heat produced, and have a longer lifetime [4].
33
The most important thing is its wavelength is 465nm to 470nm which it suitable in
reducing the bilirubin.
Figure 3.5: Blue LED
3.2.2.2 LEDs Arrangement and Design Considerations
In order to design the LEDs arrangement, there are some factors that need to
be considered. The calculation for the irradiance was made to identify the optimum
light exposure. The factors need to be considered is the effective light field,
maximum power dissipation and also the light wavelength. The calculations to
determine the positions and the distance of the LEDs are as follows:
From the datasheet, we can obtain the LED Peak Wavelength and the Maximum
Power Dissipation
LED Peak Wavelength = 465nm 470nm
Maximum Power Dissipation = 180mW
34
Effective light field = (Length x Width) of LED exposure area
= 3cm x 3cm
= 9cm2
By using these data, we can calculate the irradiance of the LEDs.
Irradiance = (Max Power Dissipation / Effective light field) / Peak Wavelength
= (180mW /9cm)/(467.5nm)
= 42.78 W/cm/nm
The calculated irradiance obtained is higher than the required irradiance
determined by the American Academy of Pediatric (AAP) guideline as in Figure 3.6.
The AAP guideline requires that the blue light should be used if the intensive
phototherapy is required. The irradiance deliver to the infants should be at least
30W/cm2/nm to the greatest surface area available.
Figure 3.6: AAP guidelines for all gestational ages [21]
35
3.2.2.3 Fluorescent Light
Figure 3.7: Fluorescent tube
Fluorescent light is the commonly used light source in phototherapy device as
we can see in most of hospital. Olympic Bililite is one of the phototherapy device
that using fluorescent tube as the light source. The fluorescent tube used in this
project is Philips TL/52 20W where TL represents the type of the lamp and 52 is its
color which is blue lamp. The wavelength for this light source is 400nm to 500nm
but the maximum wavelength is at 450nm. However care must be taken to ensure the
effective light irradiance delivery is maximize to the body surface area (BSA) and
provide eye protection during the exposure [22].
The distance from the light source should be closer to the infant as possible to
get the maximum spectral irradiance on the body surface. Usually the distance from
light source to the infant is 45cm to 50 cm[9, 20] and this will give the irradiance for
the light to be 10 15W/cm2/nm [23]. However, researches found that these light
sources are less effective and has a number of disadvantages including heat
production and the exposure to the surface area is limited.
In this project, one tube of fluorescent light will used for the experiment and
it using electronic ballast to turn it on. The distance between the light source to the
cuvette contains bilirubin concentration is adjusted to 45cm.
36
3.3
Software Development
LabView software is for visual programming language developed by National
Instruments. It is commonly used for industrial automation, instrument control and
for data acquisition. Basically, LabView program or subroutine is called virtual
instruments (VIs) consist of block diagram, a front panel and a connector panel.
Controls and indicators built in the front panel. Control is the inputs that allow the
information to the VI from the user while indicator is the output which indicate or
display the result given from the input. The block diagram contains the source code
for the graphical programming. It contains the structures and functions to perform the
operation on controls and send the data to indicators.
3.3.1 Importing data into LabView from Spectrophotometer
Figure 3.8: Block diagram
37
LabView programming can read the data from the spectrophotometer by
using RS 232. Before that we must installed DAQ-mx software into the computer
used and set the port to COM1. The block diagram for the LabView system shows as
in Figure 3.8. The system operates in stacked sequence where it consist one or more
sub-diagrams that execute sequentially. It works by allows the process proceed to the
next executions when the first sub-diagram finish its process.
Figure 3.9: (a) Input port detection (b) Read input data
VISA Resource Name used to specify the resource to which a VISA session
will be opened while VISA serial is to determine the instance to use by manually
select the instance. As in Figure 3.9 (a), this part will detect the input port from
spectrophotometer by using RS 232. Then, VISA Read Figure 3.9 (b) will read the
input data from the spectrophotometer which specify by VISA Resource Name and
return the data in Read Buffer. The output from spectrophotometer contains in Read
Buffer will be displayed at front panel as shown in Figure 3.10.
Figure 3.10: Output data from spectrophotometer
38
However, for the mathematical operation, symbol A= must be eliminate for the
calculation purpose. This system will be connected to the equation to determine the
relationship between absorbance and bilirubin concentration. Figure 3.11 shows how
the elimination process was done.
Figure 3.11: Elimination process
Figure 3.12: Result after elimination process
39
3.3.2 Bilirubin reading using LabView
Linear equation obtained for relationship between absorbance and bilirubin
concentration from the first experiment was inserted into the mathematical operation
in LabView system. This equation will be used to convert the absorbance value to
concentration. The While Loop function will repeat the process until the STOP
button pressed.
Figure 3.13: Bilirubin level detection
However, the system design is not suitable for the project because it cannot
display all the data simultaneously. This is because spectrophotometer has four
sample racks but it cannot measure the absorbance for all samples simultaneously.
The experiment requires the system to read all the data and display it in one graph for
comparison purpose. To fix this problem, stacked sequence was used as explained
earlier and the system is also use Wait (ms) function and Shift Register. Wait (ms)
function will not complete the execution until the specified time has elapsed. Since
40
the systems need to display the data simultaneously, Shift Register was used to pass
the value to the next iteration. So, the previous measured value will remain in the
graph.
Figure 3.9: Spectrophotometer sample racks
3.4
Flow Chart
The flowchart in Figure 3.15 presents the flow of the data measurement from
spectrophotometer into LabView.
The operation of the system starts by place the bilirubin concentration into the
spectrophotometer sample rack. Sample A represent the bilirubin concentration
before the light exposure while sample B and sample C represent the bilirubin
concentration after the light exposure for both blue LEDs and fluorescent light. Next,
41
the absorbance value was measured and then the value is converted to concentration
value. After one measurement, the process will stop until we push the Next button it
will continue the process until 4 reading has been measured. After the 4th
measurement or we discontinue the measurement, the system will stop and all the
data will be displayed.
Figure 3.15: Flowchart of the experiment
CHAPTER 4
RESULTS AND DISCUSSIONS
This section will discuss on the results and data analysis obtained throughout
the project.
4.1
Determination of Optimum Wavelength
Bilirubin solutions with different concentration (as shown in Figure 4.1) were
prepared and the absorbance for each different concentration was measured using a
spectrophotometer. Prior to this, the optimum absorbance wavelength for bilirubin
need to be determined as there is only one optimal wavelength for each chemical
element or chemical compound.
Table 4.1 displays the results of absorbance reading when 500mg/dL of
bilirubin solution was tested using different wavelength settings (560nm 600nm).
The results show that the highest absorbance value is 0.150, which occured at
560nm. Thus, 560nm was fixed as the optimum absorbance wavelength to be used
throughout the experiment.
43
Figure 4.1: Preparation of different bilirubin concentrations
Table 4.3: Determination of optimum absorbance wavelength
4.2
Wavelength (nm)
Absorbance
560
0.150
570
0.116
580
0.095
590
0.079
600
0.067
Relationship between Absorbance and Bilirubin Concentration
The relationship between bilirubin absorbance and concentration was
determined by measuring the absorbance for different bilirubin concentration at a
fixed wavelength using a spectrophotometer. The results are illustrated in Table 4.2.
Generally, bilirubin absorbance is directly proportional to bilirubin concentration.
From the results, a calibration curve (as shown in Figure 4.2) was plotted to
determine the mathematical equation that relates bilirubin absorbance and
concentration.
44
Table 4.4: Measurement of absorbance for different bilirubin concentrations
Concentration (mg/dL)
Absorbance
50
-0.011
100
0.065
150
0.094
200
0.153
250
0.206
300
0.304
350
0.420
400
0.432
450
0.532
500
0.599
Relationship between Absorbance and
Concentration
0.6
Absorbance
0.5
y = 1.1512x - 0.0751
0.4
R = 0.9962
0.3
0.2
0.1
0
-0.1 0
0.1
0.2
0.3
0.4
0.5
0.6
Concentration (mg/dl)
Figure 4.2: Calibration curve of absorbance vs concentration for bilirubin solution
From the calibration curve, a linear equation (Equation 4.1) is obtained.
y = 1.151x 0.075
2
R = 0.996
(Eq. 4.1)
45
The value of the correlation is closely approaching 1, which indicates that
there is a strong positive linear relationship between X (concentration) and Y
(absorbance). It also means that bilirubin absorbance and bilirubin concentration
tends to increase and decrease proportionally. The linear equation obtained was used
in the concentration calculation in LabView.
4.3
Bilirubin Degradation Experiment A Comparison between Different
Light Sources
4.3.1 LEDs Circuit Design
The calculation for irradiance and optimum light exposure which was
conducted in Chapter 3 resulted in the design of the LEDs circuit. 18 super bright
blue LEDs were arranged as in Figure 4.3. The supplied direct current (DC) voltage
was 9.5V and resistors with resistance values of 39 were arranged in series with
each LED.
Figure 4.3: LEDs circuit
46
4.3.2 Bilirubin Degradation Experiments
Two sets of five samples of 100mg/dL bilirubin solution were prepared. Both
sets of bilirubin solutions were exposed to blue LEDs and fluorescent light at five
time intervals; 10 minutes, 30 minutes, 60 minutes, 120 minutes and 180 minutes.
The absorbance value for each sample was measured before and after the light
exposure.
(a)
(b)
Figure 4.4: Bilirubin degradation experiments (a) Blue LEDs exposure (b)
Fluorescent light exposure
Table 4.3 exhibits the absorbance measurements, before and after light
exposure at each time intervals while Table 4.4 displays the degradation of bilirubin
47
concentrations in mg/dl and in percentage difference. Based on the results in Figure
4.5, the percentage difference of bilirubin degradation for blue LEDs is higher than
the fluorescent light. the experimental findings proved that blue LEDs more efficient
in redusing bilirubin level compared to fluorescent light.
Table 4.5: Results (in absorbance) of bilirubin degradation experiment
Absorbance
Time
Blue LEDs
(minutes)
Fluorescent Light
Before
After
Before
After
10
0.059
0.058
0.062
0.062
30
0.057
0.043
0.060
0.059
60
0.055
0.038
0.056
0.054
120
0.055
0.034
0.053
0.047
180
0.048
0.024
0.041
0.031
Table 6.4: Results (in concentration & percentage difference) of bilirubin
degradation experiment
Concentration (mg/dl)
Blue LEDs
Time
(minutes)
Fluorescent light
Before
After
Difference
(%)
Before
After
Difference
(%)
10
0.117
0.116
0.85
0.119
0.119
30
0.115
0.103
10.43
0.117
0.116
0.87
60
0.113
0.098
13.27
0.114
0.112
1.75
120
0.113
0.095
15.92
0.111
0.106
4.39
180
0.107
0.086
19.63
0.101
0.092
8.91
48
Percentage Difference of Bilirubin
Degradation
% bilirubin degradation
25
20
15
10
Blue LEDs
Fluorescent light
5
0
10
30
60
120
180
Time (minutes)
Figure 4.5: Comparison of bilirubin degradation in blue LED and fluorescent light
(in percentage difference)
The percentage difference of bilirubin degradation was calculated using
equation 4.2:
100
(Eq. 4.2)
4.4
Bilirubin Level Detector using LabView
LabView was used as the platform to measure bilirubin level in samples of
bilirubin solutions. Figure 4.6 displays the user interface of the bilirubin level
detector. Initially, user will need to select the input port from the instrument that
interfaces with the computer. The port detection for this project is at COM1, as had
been set before the experiment. As mentioned earlier, the spectrophotometer has four
slots on the sample rack. The first slot was used for the blank/empty cuvette for
49
instrument calibration purpose, while the other three slots were used for bilirubin
solution samples.
Figure 4.6: User interface of bilirubin level detector
Once the absorbance reading is obtained from the spectrophotometer,
the ABSORBANCE VALUE tab will display the value of absorbance for a
specific sample. The system runs the calculation automatically and converts the
absorbance data into concentration. The converted bilirubin concentration value is
displayed graphically and in the numeric form.. Once the measurement is completed,
the system will wait until the user pushes the NEXT MEASUREMENT button to
analyze the next measurement. Before that, the user will need to push the push-pull
rod to the next position.
50
The measurement process will start again for the next sample while the data
from the first measurement remains in the waveform graph for comparison purpose.
The system will stop once it reach l the fourth measurement or at anytime when the
user pushes the STOP button. The final results will display all four measurements
simultaneously on the waveform graph, making it easier for the user to make any
comparison between several data. The data from the waveform graph can be saved in
Excel by right-clicking at the waveform graph and exporting the data into Excel, as
shown in Figure 4.7. User can either print or save the data for future reference.
Figure4.7: Exporting data into Excel
4.5
Discussion
In the earlier experiment to determine the optimum absorbance
wavelength, the spectrophotometer was used to measure the bilirubin solution
concentration based on the principle of color absorbance. Different bilirubin
51
solutions were used to determine the absorbance- concentration relationship and also
to test the reliability of the bilirubin detector system in displaying measured data. In
relation with real applications, blood or urine samples can be used to test the
bilirubin level in an infants body.
In the bilirubin degradation experiment, several samples of similar bilirubin
concentration were used to identify the efficacy of blue LEDs and fluorescent light.
It is proven that blue LEDs is more efficient in reducing bilirubin level compared to
fluorescent light. Results from the bilirubin samples that were exposed to blue LEDs
gave a higher concentration difference, before and after light exposure. These
samples also showed a higher percentage difference in bilirubin degradation
compared to the sample which was exposed to the fluorescent light.
4.5.1
Interference during Experiments
It is suspected that, there might be some interference that occurred during the
experiments. This might be the cause that resulted in negative absorbance values for
a few samples of bilirubin concentration. All measurement values should be positive.
Another possible reason might be due to the inaccuracy of measurement during the
bilirubin solution preparation. During the bilirubin degradation experiment, light
interference may also occur, which will affect the bilirubins absorbance, as the
substance is very sensitive to light.
Besides that, another factor which may lead to inaccuracy of data is the
condition of the spectrophotometer. It should be fully warmed up before use and
should not be ON for a long period of time.
CHAPTER 5
CONCLUSIONS AND RECOMMENDATIONS
5.1
Conclusions
Bilirubin level detector using LabView for jaundice treatment is continuity
from the Automated Phototherapy Vest (APV) project. A simple spectrophotometric
method using spectrophotometer has been found to be the cheapest way to measure
the degradation of bilirubin level. This is because the spectrophotometric method is
simple, easy to operate, highly sensitive and is widely used for data analyzing in
industrial applications.
The main objective of the project is to verify that blue LEDs which are
proposed to be used as the light source in the APV is able to reduce bilirubin level in
infants efficiently and effectively compared to conventional phototherapy device,
such as fluorescent light. An experiment was conducted to determine the efficacy of
blue LEDs compared to fluorescent light. Samples of bilirubin solution were
prepared and exposed to each light source. Based on the experimental results, it is
proven that blue LEDs were more efficient in reducing bilirubin concentration
compared to fluorescent light.
53
The bilirubin level detector system was developed to measure bilirubin
concentration using LabView by translating absorbance value into bilirubin
concentration before displaying the data. The graphical user interface enables user to
compare bilirubin measurements of several samples which can be saved into Excel
for future reference.
5.2
Recommendation for future work
There are several recommendations that can be used to improve the current
limitations of the project. The recommendations include:
Implementing a suitable LEDs arrangement for the APV and verifying that
the blue LED on the APV is able to reduce bilirubin efficiently.
Comparing the efficiency of blue LEDs on the APV with other portable
phototherapy device such as the BiliBlanket and neoBLUE blanket LED.
Designing a system which is able to automatically identify the required time
exposure depending on the bilirubin concentration level.
54
REFERENCES
1.
Health, N.C.C.f.W.s.a.C.s., Neonatal Jaundice2010: Royal College of
Obstetricians and Gynaecologists.
2.
Jaundice in newborn babies. BMJ Publishing Group Limited 2012.
3.
M. Jeffrey Maisels, M., BCh, Phototherapy - Traditional and Nontraditional.
J. Perinatol 2001; 21:S93-S97.
4.
YS Chang, J.H., et al. , In vitro and in vivo Efficacy of New Blue Light
Emitting Diode Phototherapy Compared to Conventional Halogen Quartz
Phototherapy for Neonatal Jaundice. J Korean Med Sci 2005; 20:61-4.
5.
HJ Vreman, R.W., DK Stevenson, Phototherapy: Current Methods and
Future Directions. Semin Perinatol 2004; 28:326-333.
6.
Wentworth, S.D.P., Neonatal phototherapy - today's lights, lamps and
devices 2005. 6:14-19.
7.
Ramesh Agarwal, R.A., Ashok Deorari, Vinod K Paul, Jaundice in the
newborn. All India Institute of Medical Sciences.
8.
Malaysia, M.o.H., Management Of Jaundice In Healthy Term Newborn.
Academy of Medicine, February 2003.
9.
Salih, F.M., Can sunlight replace phototherapy unit in the treatment of
neonatal jaundice?An in vitro study. Photomed 2001; 17:272-277.
10.
Newborn jaundice (Hyperbilirubinemia), N.C.W.s. Hospital, Editor 2002.
11.
Daud, S.A., Automatic Phototherapy Vast (APV), in Faculty of Electrical
Engineering2012, University Teknologi Malaysia.
12.
Bilirubin Test. 2012.
13.
Tanja Karen, H.U.B.a.J.-C.F., Comparison of a new transcutaneous
bilirubinometer (Bilimed) with serum bilirubin measurements in preterm
and full-term infants. BMC Pediatr., 2009.
14.
Krishnasamy, M., Non-Invasive, Hand Held Transcutaneous Bilirubinometer,
H.T.A.S.M.D. Division, Editor 2009, Ministry of Health Malaysia.
55
15.
Bruzell, E.M., Phototherapy of newborns suffering from hyperbilirubinaemia.
An experimental study. Doctor Scientarium Thesis 2003.
16.
Phototherapy
in
Clinical
Applications.
Available
from:
http://www.sytledepartment.com/phototherapy-in-clinical-applications-2/.
17.
Hendrik J. Vreman, R.J.W., David K. Stevenson, et al., Light-Emitting
Diodes: A Novel Light Source for Phototherapy. Pediatr. Res; 44: 804-9,
1998.
18.
Bhutani, V.K., Phototherapy to Prevent Severe Neonatal Hyperbilirubinemia
in the Newborn Infant 35 or More Weeks of Gestation. American Academy of
Pediatrics, 2011.
19.
M. Jeffrey Maisels, A.F.M., Phototherapy for Neonatal Jaundice. N Engl J
Med; 358:920-8, 2008.
20.
Hendrik J. Vreman, R.J.W., David K. Stevenson, et al., In vitro Efficacy
Measurement of LED-Based Phototherapy Devices Compared to Traditional
Light Sources In a Model System. EASL International Bilirubin Workshop,
2004: p. 51-56.
21.
Management of Hyperbilirubinemia in the Newborn Infant 35 or more weeks
of gestation. Pediatr 2004; 114 (1),297-316.
22.
Light sources for phototherapy, 2009, Koninklijke Philips Electronics N V.
23.
Belma Saygili Karagol, O.E., Begum Atasay, Saadet Arsan, Efficacy of Light
Emitting Diode Phototherapy In Comparison To Conventional Phototherapy
In Neonatal Jaundice. Med sci 2007;31-34.
56
APPENDIX A
UV-VISIBLE SPECTROPHOTOMETER
10
Spectrumlab 752s
TRANS.
ABS.
UV VIS Spectrophotometer
MODE FUNC. 0%ADJ. 100%ADJ.
FACT.
CONC.
3
4
15
16
17
Figure 1
14
11
12
Figure 2
13
57
Instrument Appearance and Operation Keys
1. /100% button: It is used to automatically adjust 100%T when the
transmittance indicating lamp is lit. It can be pushed
once more as the end position is not reached yet.
Display- - - - is appeared to indicate the adjustment is
undergoing. This button is used to automatically adjust
0 absorbance when the absorbance indicating lamp is
lit. It can be pushed once more as the end position is
not reached yet. Display- - - - is appeared to indicate
the adjustment is undergoing. It is used to increase
concentration factor setting when conc. factor
indicating lamp is lit. One action for one push. The
concentration factor increases rapidly when the button
is kept pressing for more than 1 second. Setting value is
automatically confirmed after entered into rapid
increasing by pressing Mode button.
2. /0% button:
It is used for automatically adjusting 0%T (adjusting
range <10%T) when transmittance indicating lamp is
lit.
* This button is not used when absorbance indicating
lamp is lit. Overload will be occurred if this button is
pressing at that time.
This button is used for decreasing the concentration
factor setting when the concentration factor
indicating lamp is lit. Operation of this button is
same as /100% button.
3. Func. button:
For extending the predetermined function.
The present display value will be transmitted via
RS232C port. This value can be received by personal
computer or by printer.
4. Mode button:
It is used for selecting display scale.
The indicating lamps are ignited on the following
sequence: transmittance, absorbance and
concentration factor. The sequence is advanced
one step by pressing the button once a time and is
cycled by pressing operation.
58
5. Sample rack push-pull rod: For changing sample trough positionfour
positions
6. Four digit LED display window: For display readings and error message.
7. Transmittanceindicating lamp: Indicating that the window is displaying
transmittance data.
8. Absorbanceindicating lamp: Indicating that the window is displaying
absorbance data.
9. Concentration factorindicating lamp: Indicating that the window is
displaying concentration factor data.
10. Conc. direct read-outindicating lamp: Indicating that the window is
displaying concentration direct read-out data.
11. Power source socket:
For connecting power cord.
12. Fuse socket:
For setting fuses.
13. Main switch:
ONOFF power source
14. RS232C serial port:
For connecting RS232C serial cord
15. Sample compartment:
For sample testing
16. Wavelength display window:
For wavelength display
17. Wavelength adjusting knob:
For wavelength adjustment
59
APPENDIX B
(A) RS 232 PORT LINES
60
(B) RS 232 IMAGE
61
APPENDIX C
COMPLETED BLOCK DIAGRAM
First page
Second page
62
APPENDIX D
LABVIEW USER INTERFACE FOR BILIRUBIN LEVEL DETECTION
USING LABVIEW FOR JAUNDICE TREATMENT
Das könnte Ihnen auch gefallen
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- Lightning ProtectionDokument20 SeitenLightning Protectionsofyan_shah50% (2)
- Rework, Modification and Repair of Electronic Assemblies: IPC-7711B/7721B Change 1 November 1, 2011Dokument20 SeitenRework, Modification and Repair of Electronic Assemblies: IPC-7711B/7721B Change 1 November 1, 2011Daniel Martinez100% (1)
- Introduction To Bio Medical Instrumentation The Technology of Patient CareDokument245 SeitenIntroduction To Bio Medical Instrumentation The Technology of Patient CareAtziri Miranda88% (8)
- 8.8A 2.0 EXPLAIN STEMscopedia EnglishDokument9 Seiten8.8A 2.0 EXPLAIN STEMscopedia Englishabdur2011Noch keine Bewertungen
- Scale Up ArticleDokument8 SeitenScale Up ArticleAndrek QueckNoch keine Bewertungen
- Bab2 Mode AddressingDokument29 SeitenBab2 Mode AddressingMohammad RofiiNoch keine Bewertungen
- Texture Analysis of Aggressive and Nonaggressive Lung Tumor CE CT Images PDFDokument9 SeitenTexture Analysis of Aggressive and Nonaggressive Lung Tumor CE CT Images PDFMohammad RofiiNoch keine Bewertungen
- Kementerian Agama Republik Indonesia: Jadwal Shalat Propinsi: JAWA TENGAH Daerah: SEMARANGDokument1 SeiteKementerian Agama Republik Indonesia: Jadwal Shalat Propinsi: JAWA TENGAH Daerah: SEMARANGMohammad RofiiNoch keine Bewertungen
- WekaManual 3 7 8 PDFDokument327 SeitenWekaManual 3 7 8 PDFEduardoMendozaNoch keine Bewertungen
- IcaDokument1 SeiteIcaMohammad RofiiNoch keine Bewertungen
- BrosurgDokument4 SeitenBrosurgMohammad RofiiNoch keine Bewertungen
- RangkaianDokument1 SeiteRangkaianMohammad RofiiNoch keine Bewertungen
- ReadmedDokument1 SeiteReadmedMohammad RofiiNoch keine Bewertungen
- User Manual1 2Dokument56 SeitenUser Manual1 2Mohammad Rofii100% (1)
- Learn MATLABDokument61 SeitenLearn MATLABsayyanNoch keine Bewertungen
- Bok Mark FirefoxsDokument2 SeitenBok Mark FirefoxsMohammad RofiiNoch keine Bewertungen
- Icml TutorialDokument85 SeitenIcml TutorialMohammad RofiiNoch keine Bewertungen
- Bab3 - ElectriccircuitreviewDokument5 SeitenBab3 - ElectriccircuitreviewDefika FiantiNoch keine Bewertungen
- IEEE Outline FormatDokument3 SeitenIEEE Outline FormatAlex HerrmannNoch keine Bewertungen
- Bab3 - ElectriccircuitreviewDokument5 SeitenBab3 - ElectriccircuitreviewDefika FiantiNoch keine Bewertungen
- Instrumentasi Sistem HayatiDokument21 SeitenInstrumentasi Sistem HayatiMohammad Rofii100% (1)
- Icml TutorialDokument85 SeitenIcml TutorialMohammad RofiiNoch keine Bewertungen
- Instrumentasi Sistem Hayati: Kode MK: TM216 2 (Dua) SKSDokument26 SeitenInstrumentasi Sistem Hayati: Kode MK: TM216 2 (Dua) SKSMohammad RofiiNoch keine Bewertungen
- Bab 3 Slide 1Dokument11 SeitenBab 3 Slide 1Mohammad Rofii100% (1)
- Nota TransferDokument1 SeiteNota TransferMohammad RofiiNoch keine Bewertungen
- F 1Dokument10 SeitenF 1Srinivas AmbalaNoch keine Bewertungen
- IEEE Outline FormatDokument3 SeitenIEEE Outline FormatAlex HerrmannNoch keine Bewertungen
- 2009-IJRTE Analysis of Foveal Avascular Zone in Color Fundus Image For Grading of DRDokument4 Seiten2009-IJRTE Analysis of Foveal Avascular Zone in Color Fundus Image For Grading of DRMohammad RofiiNoch keine Bewertungen
- Intro Sci LabDokument87 SeitenIntro Sci LabandysarmientoNoch keine Bewertungen
- Computers in Biology and Medicine: B. Nayebifar, H. Abrishami MoghaddamDokument8 SeitenComputers in Biology and Medicine: B. Nayebifar, H. Abrishami MoghaddamMohammad RofiiNoch keine Bewertungen
- Invoice-G3bawDokument1 SeiteInvoice-G3bawMohammad RofiiNoch keine Bewertungen
- DCT Theory and ApplicationDokument32 SeitenDCT Theory and ApplicationAhmed SoulimanNoch keine Bewertungen
- Au in C - HutchingsDokument8 SeitenAu in C - HutchingsLuis TolentinoNoch keine Bewertungen
- Sumitomo PDFDokument20 SeitenSumitomo PDF何家銘Noch keine Bewertungen
- Chapter 5: Analytic Techniques: by Julia C. Drees, Matthew S. Petrie, Alan H.B. WuDokument15 SeitenChapter 5: Analytic Techniques: by Julia C. Drees, Matthew S. Petrie, Alan H.B. WuTanveerNoch keine Bewertungen
- Schultz 1987Dokument18 SeitenSchultz 1987Ruiz ManuelNoch keine Bewertungen
- Lettre MotivationDokument2 SeitenLettre MotivationSalhi SiwarNoch keine Bewertungen
- A Physical Absorption Process For The Capture of Co From Co - Rich Natural Gas StreamsDokument6 SeitenA Physical Absorption Process For The Capture of Co From Co - Rich Natural Gas StreamssinhleprovietNoch keine Bewertungen
- CGR 18650cgDokument2 SeitenCGR 18650cgKonstantinos GoniadisNoch keine Bewertungen
- Manual CAT4000Dokument36 SeitenManual CAT4000windrider56Noch keine Bewertungen
- ASTM A193: GradesDokument1 SeiteASTM A193: GradesRamon MendozaNoch keine Bewertungen
- Properties of Gelatins From Skins of Fish - Black Tilapia (Oreochromis Mossambicus) and Red Tilapia (Oreochromis Nilotica)Dokument4 SeitenProperties of Gelatins From Skins of Fish - Black Tilapia (Oreochromis Mossambicus) and Red Tilapia (Oreochromis Nilotica)Rizky Febrian SatrianiNoch keine Bewertungen
- L2472 Rev 9Dokument4 SeitenL2472 Rev 9Ignacio León CornejoNoch keine Bewertungen
- Docu Tips-24972ukqualsgcebiologyas804224972Dokument52 SeitenDocu Tips-24972ukqualsgcebiologyas804224972Rafid HaqNoch keine Bewertungen
- AQA GCSE NOV2020 Combined Science Trilogy Chemistry Paper 1H QPDokument24 SeitenAQA GCSE NOV2020 Combined Science Trilogy Chemistry Paper 1H QPmakintolu7Noch keine Bewertungen
- PG 91Dokument1 SeitePG 91Shahruzi MahadzirNoch keine Bewertungen
- 150ah C20Dokument2 Seiten150ah C20movick.25Noch keine Bewertungen
- Physico-Chemical Standardization and Phytochemical Screening of Potential Medicinal Herb: Vetiveria Zizanioides (Roots)Dokument6 SeitenPhysico-Chemical Standardization and Phytochemical Screening of Potential Medicinal Herb: Vetiveria Zizanioides (Roots)xiuhtlaltzinNoch keine Bewertungen
- Model Questions ElasticityDokument3 SeitenModel Questions Elasticityrameshbabu_1979Noch keine Bewertungen
- Benzene Hydrogenation Over Ni/Al O Catalysts Prepared by Conventional and Sol-Gel TechniquesDokument9 SeitenBenzene Hydrogenation Over Ni/Al O Catalysts Prepared by Conventional and Sol-Gel TechniquesHarun AydınNoch keine Bewertungen
- Thin CylinderDokument5 SeitenThin CylinderAngshuman BhardwajNoch keine Bewertungen
- The Philippine Chemical Industry ProfileDokument7 SeitenThe Philippine Chemical Industry ProfileEddie Resurreccion Jr.Noch keine Bewertungen
- Monel K500 PDFDokument6 SeitenMonel K500 PDFOZAIRTRADELINKNoch keine Bewertungen
- Fuelless GeneratorDokument20 SeitenFuelless GeneratorazoubraNoch keine Bewertungen
- Zinc Chloride Sol Msds PDFDokument6 SeitenZinc Chloride Sol Msds PDFJunia Alfa NessaNoch keine Bewertungen
- BEIKE - Tripod Catalogue 2014Dokument30 SeitenBEIKE - Tripod Catalogue 2014BaliNoch keine Bewertungen
- Bongsuwan D 2008Dokument7 SeitenBongsuwan D 2008Liona MargaritaNoch keine Bewertungen
- SDS - Vinyguard Silvergrey 88 - Marine - Protective - English (Uk) - SingaporeDokument6 SeitenSDS - Vinyguard Silvergrey 88 - Marine - Protective - English (Uk) - SingaporeAmi Terecef Gamboa MirandaNoch keine Bewertungen