Beruflich Dokumente
Kultur Dokumente
Liver Cirrhosis: (Alterations in Metabolic and Endocrine Functions)
Hochgeladen von
Jorie RocoOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Liver Cirrhosis: (Alterations in Metabolic and Endocrine Functions)
Hochgeladen von
Jorie RocoCopyright:
Verfügbare Formate
[Alterations in Metabolic and Endocrine Functions]
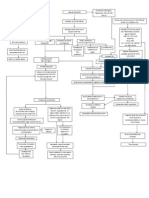
LIVER CIRRHOSIS
Precipitating Factors:
Predisposing Factor:
- Excessive alcohol - LAENNECS CIRRHOSIS
- Complication of viral, toxic / idiopathic hepatitis
- POSTNECROTIC CIRRHOSIS
- Chronic biliary obstruction and infection - BILIARY CIRRHOSIS
- Severe right-sided heart failure
- Biliary Atresia
- Genetic digestive disorder
- Autoimmune hepatitis
Liver Cell Injury
Increased
Pain
Inflammation
Fatigue
Nausea & Vomiting
Fever
Anorexi
Activation of Hepatic Stellate cells
Expansion of Myofibroblasts-Pool
Fibrosis/Scarring of the Liver
Obstruction of Blood Flow
Increased pressure in the venous and sinusoidal
channels
Portal Hypertension ( 10mmHg)
Formation of collateral circulation
pressure to nearest
susceptible organ/s
organs
Splanchnic vascular and Peripheral
arterial vasodilation
Increased circulating
bilirubin
Caput medusae
Jaundice
Hemorrhoids
Esophageal varices
Hypersplenism
Thrombocytopenia
Anemia
Leukopenia
Prolonged bleeding
weakness
infection
Splanchnic Lymph
production
Hepatorenal Syndrome
Effective blood volume decreased
Cardiac output decreased
SNS
Renal Arterial
Vasoconstriction
ADH
RAAS
*Oliguria
*Increased BUN and Creatinine levels - azotemia
*Increased osmolality and urine specific gravity
*Low blood sodium
*Low urine sodium concentration
Renal blood flow
Na+ & Water
Retention
Ascites formation
A
SOURCES:
Gressner, O., Weiskirchen, R., & Gressner, A. (2007). Medscape Nurses: Evolving Concepts of Liver Fibrogenesis Provide New
Diagnostic and Therapeutic Options. Retrieved March 2015, from http://www.medscape.com/viewarticle/573027.
Lewis, S. and et.al. (2008). Medical Surgical Nursing: Assessment and Management of Clinical Problems. Singapore: Mosby
Elsevier Inc.
Mayo Foundation for Medical Education and Research. (2015). Cirrhosis. Retrieved March 2015, from
http://www.mayoclinic.org/diseases-conditions/cirrhosis/basics/causes/con-20031617.
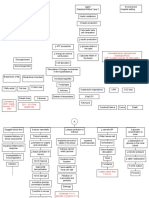
[Alterations in Metabolic and Endocrine Functions]
Udan, J. (2002). Medical Surgical: Concepts and Clinical Application (First Edition). Philippines: Guiani Prints House.
Wolf, D. (2014, December 10). Medscape: Cirrhosis. Retrieved March 2015, from
http://emedicine.medscape.com/article/185856-overview.
A
Arterial
underfilling
Activation of
vasoconstrictors
Decreased bile in Gastrointestinal
tract and increase urobilinogen
Release of endothelin-1 and
combines to capillary cells
Nitric oxide secreted causing to
vasodilate and increased blood flow
Clay-colored stools
and dark urine
Increased RBC causing insufficient O2 supply and different
pressure d/t different pressure in capillary and alveolus
Hepatic Pulmonary
Syndrome
*Exhaustion
*Fatigue
Poor Vitamin
K absorption
Decreased
emulsification of
Bleeding
tendencies
Hypoglycemia
Malnutrition
Inability to metabolize
ammonia to urea
Ammonia levels
in the blood
Brain edema
Astrocyte swelling
Neurotransmitter and receptor alteration
Altered brain glucose metabolism
Decrease androgen and
estrogen detoxification
Decrease metabolism of
protein and carbohydrates
Osmotic
pressure
* Palmar erythema
* Testicular atrophy
* Gynecomastia
* Spider Angiomas
* Loss of body hair
* Menstrual changes
Ascites
Decrease ADH &
aldosterone detoxification
Edema
Bacterial
Peritonitis
Sepsis
Hepatic Encephalopathy
* Inability to concentrate
* Loss of memory
* Confusion
* Depressed level of consciousness
* Asterixis
* Foul breath
* Respiratory acidosis
* Alteration in sleep
Hepatic Coma
Death
Gressner, O., Weiskirchen, R., & Gressner, A. (2007). Medscape Nurses: Evolving Concepts of Liver Fibrogenesis Provide New
Diagnostic and Therapeutic Options. Retrieved March 2015, from http://www.medscape.com/viewarticle/573027.
Lewis, S. and et.al. (2008). Medical Surgical Nursing: Assessment and Management of Clinical Problems. Singapore: Mosby
Elsevier Inc.
Mayo Foundation for Medical Education and Research. (2015). Cirrhosis. Retrieved March 2015, from
http://www.mayoclinic.org/diseases-conditions/cirrhosis/basics/causes/con-20031617.
[Alterations in Metabolic and Endocrine Functions]
Udan, J. (2002). Medical Surgical: Concepts and Clinical Application (First Edition). Philippines: Guiani Prints House.
Wolf, D. (2014, December 10). Medscape: Cirrhosis. Retrieved March 2015, from
http://emedicine.medscape.com/article/185856-overview.
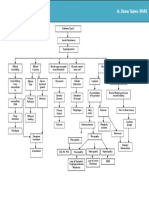
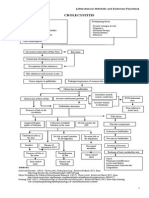
LIVER CIRRHOSIS
Cirrhosis is the final stage attained by various chronic liver diseases after years or
decades of slow progression. The liver cells attempt to regenerate, but the regenerative process is
disorganized, resulting in abnormal blood vessel and bile duct architecture. The overgrowth of
new and fibrous connective tissue distorts the livers normal lobular structure, resulting in
lobules of irregular size and shape with impeded blood flow. Eventually, irregular, disorganized
regeneration; poor cellular nutrition; and hypoxia caused by inadequate blood flow and scar
tissue result in decreased functioning of the liver. Cirrhosis may be having an insidious,
prolonged course.[1]
ETIOLOGY
Excessive alcohol (Laennecs Cirrhosis) the first change in the liver from excessive
alcohol intake is an accumulation of fat in the liver cells. Uncomplicated fatty changes in
the liver are potentially reversible if the person stops drinking alcohol. If the alcohol
abuse continues, widespread scar formation occurs throughout the liver.
Complication of viral, toxic or idiopathic hepatitis (Postnecrotic Cirrhosis) called as
post necrotic cirrhosis.
Chronic biliary obstruction and infection due to gallstones, inflammation of bile ducts,
trauma, biliary strictures (abnormal narrowing of the ducts), cysts, enlarged lymph nodes,
pancreatitis, and injury related to gallbladder or liver surgery, tumors of bile ducts or
pancreas, hepatitis, or parasites. (Biliary Cirrhosis)
Severe right-sided heart failure in patients with cor pulmonale, constrictive pericarditis,
and tricuspid insufficiency.[2]
Biliary Atresia
Genetic digestive disorder
Autoimmune hepatitis[3]
Wolf, D. (2014, December 10). Medscape: Cirrhosis. Retrieved March 2015, from
[Alterations in Metabolic and Endocrine Functions]
http://emedicine.medscape.com/article/185856-overview
2
Udan, J. (2002). Medical Surgical: Concepts and Clinical Application (First Edition). Philippines: Guiani Prints House.
Lewis, S. and et.al. (2008). Medical Surgical Nursing: Assessment and Management of Clinical Problems. Singapore: Mosby
Elsevier Inc.
PATHOPHYSIOLOGY
In cirrhosis, continuous liver damage can result to cell destruction and fibrosis of hepatic
tissues. Fibrosis within the cirrhotic liver obstructs the flow of blood through the liver and to the
liver cells. As a result of the obstruction to the flow of blood through the liver, blood backs-up in
the portal vein, and the pressure in the portal vein increases, a condition called portal
hypertension. Because of the obstruction to flow and high pressures in the portal vein, blood in
the portal vein seeks other veins in which to return to the heart, veins with lower pressures that
bypass the liver. Unfortunately, the liver is unable to add or remove substances from blood that
bypasses it. It is a combination of reduced numbers of liver cells, loss of the normal contact
between blood passing through the liver and the liver cells, and blood bypassing the liver that
leads to many of the manifestations of cirrhosis. In an attempt to reduce the high portal pressure
and to reduce the increased plasma volume and lymphatic flow, collateral circulation develops.
The common area for collateral circulation includes the veins in the esophagus, anterior
abdominal wall, parietal peritoneum and the mesenteric veins in the intestines specifically in the
rectum. Varicosities develop in the collateral areas, resulting to esophageal and gastric varices,
caput medusa and haemorrhoids. These varices can lead to massive haemorrhage if the varices
are being ruptured because of some factors such as acid regurgitation from the stomach,
ingestion of coarse food, swallowing of poorly masticated food, and increased abdominal
pressure.[1]
The spleen normally acts as a filter to remove older red blood cells, white blood cells,
and platelets. The blood that drains from the spleen joins the blood in the portal vein from the
intestines. As the pressure in the portal vein rises in cirrhosis, it increasingly blocks the flow of
blood from the spleen. The blood turns back accumulating in the spleen, and the spleen swells in
size, a condition referred to as hypersplenism.[2] Sometimes, the spleen is so enlarged that it
causes abdominal pain. As the spleen enlarges, it filters out more and more of the blood cells and
platelets until their numbers in the blood are reduced called as thrombocytopenia, leukopenia,
anemia and coagulation disorders. The anemia can cause weakness, the leukopenia can lead to
infections, and the thrombocytopenia can impair the clotting of blood and result in prolonged
bleeding.[3]
[Alterations in Metabolic and Endocrine Functions]
Lewis, S. and et.al. (2008). Medical Surgical Nursing: Assessment and Management of Clinical Problems. Singapore: Mosby
Elsevier Inc.
Mayo Foundation for Medical Education and Research. (2015). Cirrhosis. Retrieved March 2015, from
http://www.mayoclinic.org/diseases-conditions/cirrhosis/basics/causes/con-20031617.
Wolf, D. (2014, December 10). Medscape: Cirrhosis. Retrieved March 2015, from
http://emedicine.medscape.com/article/185856-overview.
Some of the protein in food that escapes digestion and absorption is used by bacteria
that are normally present in the intestine. While using the protein for their own purposes, the
bacteria make substances that they release into the intestine. These substances then can be
absorbed into the body. Some of these substances, for example, ammonia, can have toxic
effects on the brain. Ordinarily, these toxic substances are carried from the intestine in the
portal vein to the liver where they are removed from the blood and detoxified. When cirrhosis
is present, blood are not detoxified and ammonia and other substances are present in the
systemic circulation. When the toxic substances accumulate sufficiently in the blood, the
function of the brain is impaired, a condition called hepatic encephalopathy. Symptoms
include
irritability,
inability
to
concentrate
or
perform
calculations,
loss
of
memory, confusion, or depressed levels of consciousness, asterixis, foul breath, respiratory
acidosis, and alteration in sleep. Hepatic encephalopathy will further complicate to hepatic
coma if not well managed that will lead to death.[1]
Rarely, some patients with advanced cirrhosis can develop hepatopulmonary syndrome.
These patients can experience difficulty breathing because certain hormones specifically the
endothelin-1, a portent vasoconstrictor, released in advanced cirrhosis cause the lungs to function
abnormally. The basic problem in the lung is that not enough blood flows through the small
blood vessels in the lungs that are in contact with the alveoli of the lungs. Blood flowing through
the lungs is shunted around the alveoli and cannot pick up enough oxygen from the air in the
alveoli. As a result the patient experiences shortness of breath, particularly with exertion.[2]
In uncontrolled multiplication of liver cells for recovery of lost cells, cancer of the liver
develops. The most common symptoms and signs of primary liver cancer are abdominal pain and
swelling, hepatomegaly, weight loss, and fever.[3]
The liver cells and the channels through which bile flows are also affected in cirrhosis.
Bile is a fluid produced by liver cells that has two important functions: to aid in digestion and to
remove and eliminate toxic substances from the body. The bile that is produced by liver cells is
secreted into very tiny channels that run between the liver cells that line the sinusoids, called
canaliculi. The canaliculi empty into small ducts which then join together to common bile duct.[5]
[Alterations in Metabolic and Endocrine Functions]
Gressner, O., Weiskirchen, R., & Gressner, A. (2007). Medscape Nurses: Evolving Concepts of Liver Fibrogenesis Provide New
Diagnostic and Therapeutic Options. Retrieved March 2015, from http://www.medscape.com/viewarticle/573027.
Lewis, S. and et.al. (2008). Medical Surgical Nursing: Assessment and Management of Clinical Problems. Singapore: Mosby
Elsevier Inc.
Mayo Foundation for Medical Education and Research. (2015). Cirrhosis. Retrieved March 2015, from
http://www.mayoclinic.org/diseases-conditions/cirrhosis/basics/causes/con-20031617.
Wolf, D. (2014, December 10). Medscape: Cirrhosis. Retrieved March 2015, from
http://emedicine.medscape.com/article/185856-overview.
Ultimately, all of the ducts combine into one duct that enters the small intestine. In this way, bile
gets to the intestine where it can help with the digestion of food. At the same time, toxic
substances contained in the bile enter the intestine and then are eliminated in the stool. In
cirrhosis, the canaliculi are abnormal and the relationship between liver cells and canaliculi is
destroyed, just like the relationship between the liver cells and blood in the sinusoids. As a result,
obstructive jaundice may also occur and is usually accompanied by pruritus, an accumulation of
bile salts underneath the skin. The liver is not able to eliminate toxic substances normally, and
they can accumulate in the body. To a minor extent, digestion in the intestine also is reduced.
Jaundice occurs as a result of decreased ability to conjugate and excrete bilirubin. If obstruction
of the biliary tracts occurs, obstructive jaundice may also occur and is usually accompanied by
pruritus, an accumulation of bile salts underneath the skin.[1]
Patients with worsening cirrhosis can develop hepatorenal syndrome. This syndrome is a
serious complication in which the function of the kidneys is reduced. It is a functional problem
in the kidneys, meaning there is no physical damage to the kidneys. Instead, the reduced function
is due to changes in the way the blood flows through the kidneys themselves. Due to the portal
hypertension along with liver decompensation results in splanchnic and systemic vasodilation
and decreased arterial blood volume, renal vasoconstriction occurs and renal failures occur. This
syndrome consists of progressive oliguria and azotemia in the absence of structural damage to
the kidney. There will be an increase BUN and Creatinine levels in the urinalysis result. There
will be also an increase osmolality and urine specific gravity, low blood sodium and low urine
sodium concentration due to sodium reabsorption.[2]
As cirrhosis of the liver becomes severe, signals are sent to the kidneys to retain salt and
water in the body. The excess salt and water first accumulates in the tissue beneath the skin of
the ankles and legs because of the effect of gravity when standing or sitting. This accumulation
of fluid is called edema or pitting edema. Fluid also may accumulate in the abdominal cavity
between the abdominal wall and the abdominal organs. This accumulation of fluid, called ascites
causes swelling of the abdomen, abdominal discomfort, and increased weight. When BP is
elevated in the liver, proteins move from the blood vessels via the large pores of sinusoids into
6
[Alterations in Metabolic and Endocrine Functions]
the lymph space. When the lymphatic system is unable to carry off the excess proteins and water,
they leak through the liver capsule into the peritoneal cavity. The osmotic pressure of the
proteins pulls additional fluid into the peritoneal cavity. Another mechanism is hypoalbuminemia
resulting from inability of the liver to synthesize albumin.[3] The hypoalbuminemia results in
Wolf, D. (2014, December 10). Medscape: Cirrhosis. Retrieved March 2015, from
http://emedicine.medscape.com/article/185856-overview.
Gressner, O., Weiskirchen, R., & Gressner, A. (2007). Medscape Nurses: Evolving Concepts of Liver Fibrogenesis Provide New
Diagnostic and Therapeutic Options. Retrieved March 2015, from http://www.medscape.com/viewarticle/573027.
Lewis, S. and et.al. (2008). Medical Surgical Nursing: Assessment and Management of Clinical Problems. Singapore: Mosby
Elsevier Inc.
decreased colloidal oncotic pressure. Another mechanism is hyperaldosteronism which occurs
when aldosterone is not metabolized by damaged hepatocytes. The increased level of aldosterone
causes increased sodium reabsorption by the renal tubules. This retention of sodium as well as
the increased in antidiuretic hormone, causes additional water retention. When this ascites will
rupture, usually at the abdominal part, this may lead to bacterial peritonitis, sepsis and may
progress and lead to death.[1]
Several signs and symptoms relating to the metabolism and inactivation of adrenocortical
hormones, estrogen and testosterone occur in cirrhosis. When the liver is unable to metabolize
the hormones, various manifestations occur. In men, gynecomastia, loss of axillary and pubic
hair, testicular atrophy, and impotence with loss of libido may occur as a result of increased
estrogen levels. In younger women, amenorrhea may occur, and in older women there may be
vaginal bleeding. The liver fails to metabolize aldosterone adequately, resulting in
hyperaldosteronism with subsequent sodium and water retention and potassium loss.[2]
Jaclyn Mae T. Alviola, RN
[Alterations in Metabolic and Endocrine Functions]
_____________________________________________________________________________
_
1
Lewis, S. and et.al. (2008). Medical Surgical Nursing: Assessment and Management of Clinical Problems. Singapore: Mosby
Elsevier Inc.
Wolf, D. (2014, December 10). Medscape: Cirrhosis. Retrieved March 2015, from
http://emedicine.medscape.com/article/185856-overview.
Das könnte Ihnen auch gefallen
- Pahtophysiology of EsrdDokument5 SeitenPahtophysiology of EsrdCarl JardelezaNoch keine Bewertungen
- Pathophysiology of DMDokument4 SeitenPathophysiology of DMNicole Louise N. VillanuevaNoch keine Bewertungen
- Acute Renal Failure DiagramDokument3 SeitenAcute Renal Failure DiagramMichelle BarojaNoch keine Bewertungen
- BEDS AND BED MAKING ContentDokument12 SeitenBEDS AND BED MAKING ContentSneha80% (5)
- EpidemiologyDokument86 SeitenEpidemiologySainab Moohamoud83% (6)
- Elderly PrimigravidaDokument5 SeitenElderly PrimigravidaDeepti Kukreti100% (5)
- Liver Cirrhosis: Precipitating Factors: Predisposing FactorDokument22 SeitenLiver Cirrhosis: Precipitating Factors: Predisposing FactorJorie RocoNoch keine Bewertungen
- Pathophysio Chronic GlomerulonephritisDokument1 SeitePathophysio Chronic GlomerulonephritisRan Ma100% (1)
- Pathophysiology of Portal HYPERTENSION PDFDokument11 SeitenPathophysiology of Portal HYPERTENSION PDFCamilo VidalNoch keine Bewertungen
- DB31 - Pathophysiology of Diabetes Mellitus and HypoglycemiaDokument5 SeitenDB31 - Pathophysiology of Diabetes Mellitus and HypoglycemiaNeil Alcazaren かわいいNoch keine Bewertungen
- IV. The PATIENTS ILLNESS (Nephrolithiasis) Pathophysiology (Book-Based)Dokument3 SeitenIV. The PATIENTS ILLNESS (Nephrolithiasis) Pathophysiology (Book-Based)wapakalypseNoch keine Bewertungen
- Path o PhysiologyDokument9 SeitenPath o PhysiologyKyle Ü D. CunanersNoch keine Bewertungen
- BPH Pathophysio 4CDokument2 SeitenBPH Pathophysio 4CPatricia Camille Ponce JonghunNoch keine Bewertungen
- PATHOPHYDokument3 SeitenPATHOPHYArlly Faena AbadNoch keine Bewertungen
- Bladder CancerDokument1 SeiteBladder CancerCarmina AguilarNoch keine Bewertungen
- Multiple Physical Injuries Secondary To Vehicular AccidentDokument31 SeitenMultiple Physical Injuries Secondary To Vehicular AccidentJane Arian BerzabalNoch keine Bewertungen
- Pathophysiology of Alcoholic Liver DiseaseDokument4 SeitenPathophysiology of Alcoholic Liver Diseaseshailendra tripathiNoch keine Bewertungen
- Pathophysio CRF RevisedDokument2 SeitenPathophysio CRF Revisedroseanne18Noch keine Bewertungen
- Age Greater Than 60 Y/o Hereditary Precipitating Factors: Hypertension Increase Protein and Fat IntakeDokument3 SeitenAge Greater Than 60 Y/o Hereditary Precipitating Factors: Hypertension Increase Protein and Fat Intakenursing concept mapsNoch keine Bewertungen
- Diabetes Mellitus: Hyperglycemia (304 MG/DL, 13.2 MG/DL)Dokument3 SeitenDiabetes Mellitus: Hyperglycemia (304 MG/DL, 13.2 MG/DL)John Henry ValenciaNoch keine Bewertungen
- PathoDokument7 SeitenPathoAnonymous 87fNoO2fhVNoch keine Bewertungen
- Anatomy and Physiology of The GallbladderDokument1 SeiteAnatomy and Physiology of The GallbladderRojanisa Baculi RomathoNoch keine Bewertungen
- Pathophysiology of DiarrheaDokument3 SeitenPathophysiology of DiarrheaFathur RahmatNoch keine Bewertungen
- Presentation PathophysiologyDokument11 SeitenPresentation PathophysiologyJade DeopidoNoch keine Bewertungen
- Pathophysiology of Hypertension, Diabetes, Ubm, BPHDokument3 SeitenPathophysiology of Hypertension, Diabetes, Ubm, BPHCarly Beth Caparida LangerasNoch keine Bewertungen
- Anemia IntroductionDokument15 SeitenAnemia IntroductionNitesh Kotian100% (1)
- Upper Gastrointestinal BleedingDokument69 SeitenUpper Gastrointestinal Bleedingeliza luisNoch keine Bewertungen
- Pathway - Urethral StrictureDokument1 SeitePathway - Urethral StrictureCiptaningrum Marisa PNoch keine Bewertungen
- Pathophysiology of Liver CirrhosisDokument2 SeitenPathophysiology of Liver Cirrhosisgaelty100% (4)
- CKD - For Concept MappingDokument7 SeitenCKD - For Concept MappingKennette Lim0% (1)
- Esrd Diagram PathophysiologyDokument3 SeitenEsrd Diagram PathophysiologySTEPHANIE JOSUE100% (1)
- Osteosarcoma-Ana and PhysiologyDokument4 SeitenOsteosarcoma-Ana and PhysiologyNeirfla WassabiNoch keine Bewertungen
- CholelithiasisDokument3 SeitenCholelithiasisMIlanSagittarius0% (1)
- Serum ElectrolytesDokument2 SeitenSerum ElectrolytesKervin CablaidaNoch keine Bewertungen
- Increased Serum Glucose Level (Hyperglycemia) 278.14 MG/DL (Normal: 70-100 MG/DL)Dokument3 SeitenIncreased Serum Glucose Level (Hyperglycemia) 278.14 MG/DL (Normal: 70-100 MG/DL)Angel FiloteoNoch keine Bewertungen
- Pathophy - Nephrotic SyndromeedDokument1 SeitePathophy - Nephrotic Syndromeedianecunar100% (1)
- Pathophysiology of Hyperthyroidism and Thyroid StormDokument3 SeitenPathophysiology of Hyperthyroidism and Thyroid StormPen MontanteNoch keine Bewertungen
- DB13 - Pathophysiology of AtherosclerosisDokument2 SeitenDB13 - Pathophysiology of Atherosclerosisi_vhie03Noch keine Bewertungen
- Liver Cirrhosis PathophysiologyDokument1 SeiteLiver Cirrhosis PathophysiologyCaren ReyesNoch keine Bewertungen
- Electrolyte Imbalance 1Dokument3 SeitenElectrolyte Imbalance 1Marius Clifford BilledoNoch keine Bewertungen
- Nephrolithiasis PDFDokument16 SeitenNephrolithiasis PDFApriany Cordias Arlita SilalahiNoch keine Bewertungen
- Phosphate Imbalances PDFDokument1 SeitePhosphate Imbalances PDFKaye RicoNoch keine Bewertungen
- Anal Canal: Fissure in Ano HaemorrhoidsDokument37 SeitenAnal Canal: Fissure in Ano Haemorrhoidsyash shrivastavaNoch keine Bewertungen
- Pathophysiology ErDokument3 SeitenPathophysiology ErAlexa A. AldayNoch keine Bewertungen
- Patof DMDokument1 SeitePatof DMxerwaneNoch keine Bewertungen
- Summary Case Peptic Ulcer and PeritonitisDokument8 SeitenSummary Case Peptic Ulcer and PeritonitissyududNoch keine Bewertungen
- Modified Radical MastectomyDokument6 SeitenModified Radical Mastectomymetch isulatNoch keine Bewertungen
- Liver Cirrhosis: A Case Study OnDokument31 SeitenLiver Cirrhosis: A Case Study OnCharmaine del RosarioNoch keine Bewertungen
- Schematic Diagram of Alcoholic Cirrhosis: Liver Steatosis/ Fatty LiverDokument2 SeitenSchematic Diagram of Alcoholic Cirrhosis: Liver Steatosis/ Fatty LiverCarmelli Mariae CalugayNoch keine Bewertungen
- Disease Spotlight: Diabetes Mellitus: Insulin Insulin Is A Drug That Is Used To ControlDokument7 SeitenDisease Spotlight: Diabetes Mellitus: Insulin Insulin Is A Drug That Is Used To ControlMIR SARTAJNoch keine Bewertungen
- Addison'sDokument4 SeitenAddison'sKoRnflakesNoch keine Bewertungen
- Pathophysiology-Kni Ns PLZZZDokument8 SeitenPathophysiology-Kni Ns PLZZZAnna Lira Manluyang MungcalNoch keine Bewertungen
- Pathophysiology of UrolithiasisDokument3 SeitenPathophysiology of UrolithiasisNavjot Brar100% (2)
- Systemic Lupus Erythematosus (SLE) : Genetic Factors Environmental FactorsDokument5 SeitenSystemic Lupus Erythematosus (SLE) : Genetic Factors Environmental Factorsjoyrena ochondraNoch keine Bewertungen
- Management of OliguriaDokument14 SeitenManagement of OliguriaAhmed El-MalkyNoch keine Bewertungen
- Pa Tho Physiology of Open FractureDokument2 SeitenPa Tho Physiology of Open FracturegiffersonbNoch keine Bewertungen
- Diabetes PathophysiologyDokument2 SeitenDiabetes PathophysiologyShelly_Ann_Del_9959Noch keine Bewertungen
- The Pathophysiology of Peptic UlcerDokument15 SeitenThe Pathophysiology of Peptic UlcerKike Meneses100% (1)
- Presentation Liver CirrhosisDokument26 SeitenPresentation Liver CirrhosisFaye Dominique Roxas PalmaresNoch keine Bewertungen
- Cirrhosis of LiverDokument35 SeitenCirrhosis of LiverShazia Parveen100% (1)
- Viruses Genetic Autoimmune Liver Disease Immune System: Mallory-Weiss Tears Peptic Ulcer DiseaseDokument3 SeitenViruses Genetic Autoimmune Liver Disease Immune System: Mallory-Weiss Tears Peptic Ulcer DiseasecpublicoNoch keine Bewertungen
- Cirrhosis: Petrus J. HasibuanDokument17 SeitenCirrhosis: Petrus J. HasibuanAgustinus VincentNoch keine Bewertungen
- Liver, Biliary Tract and Pancreas ProblemsDokument95 SeitenLiver, Biliary Tract and Pancreas ProblemsBav VAansoqnuaetzNoch keine Bewertungen
- Nursing TheoriesDokument51 SeitenNursing TheoriesJorie RocoNoch keine Bewertungen
- BioethicsDokument31 SeitenBioethicsJorie RocoNoch keine Bewertungen
- Chapter 1Dokument5 SeitenChapter 1Jorie RocoNoch keine Bewertungen
- Case Study ProposalDokument4 SeitenCase Study ProposalJorie RocoNoch keine Bewertungen
- Transpersonal CaringDokument46 SeitenTranspersonal CaringJorie Roco100% (1)
- Critical Thinking PointersDokument40 SeitenCritical Thinking PointersJorie RocoNoch keine Bewertungen
- Measures of LocationDokument9 SeitenMeasures of LocationJorie RocoNoch keine Bewertungen
- Table of ContentsDokument2 SeitenTable of ContentsJorie RocoNoch keine Bewertungen
- Approval Sheet SampleDokument1 SeiteApproval Sheet SampleJorie RocoNoch keine Bewertungen
- Measures of SkewnessDokument15 SeitenMeasures of SkewnessJorie Roco100% (1)
- Theoretical Foundation in NursingDokument24 SeitenTheoretical Foundation in NursingJorie RocoNoch keine Bewertungen
- StaffingDokument50 SeitenStaffingPradeep PandaNoch keine Bewertungen
- Cover Page Nursing ManualDokument1 SeiteCover Page Nursing ManualJorie RocoNoch keine Bewertungen
- Kinds of Data PresentationDokument18 SeitenKinds of Data PresentationJorie RocoNoch keine Bewertungen
- SurveyDokument38 SeitenSurveyJorie RocoNoch keine Bewertungen
- Overview of SpssDokument49 SeitenOverview of SpssJorie RocoNoch keine Bewertungen
- Hypos TestingDokument192 SeitenHypos TestingJorie RocoNoch keine Bewertungen
- Summary StatisticsDokument28 SeitenSummary StatisticsJorie RocoNoch keine Bewertungen
- Advanced Statistics ReviewDokument21 SeitenAdvanced Statistics ReviewJorie RocoNoch keine Bewertungen
- Measures of LocationDokument9 SeitenMeasures of LocationJorie RocoNoch keine Bewertungen
- J1 Lecture 1 A Stimulus To DefineDokument6 SeitenJ1 Lecture 1 A Stimulus To DefineJorie RocoNoch keine Bewertungen
- Nursing Administration PowepointDokument27 SeitenNursing Administration PowepointJorie RocoNoch keine Bewertungen
- Survey Hema OncoDokument1 SeiteSurvey Hema OncoJorie RocoNoch keine Bewertungen
- Kinds of Data PresentationDokument18 SeitenKinds of Data PresentationJorie RocoNoch keine Bewertungen
- Pancreatitis: (Alterations in Metabolic and Endocrine Functions)Dokument7 SeitenPancreatitis: (Alterations in Metabolic and Endocrine Functions)Jorie Roco0% (1)
- Cholecystitis: (Alterations in Metabolic and Endocrine Functions)Dokument4 SeitenCholecystitis: (Alterations in Metabolic and Endocrine Functions)Jorie RocoNoch keine Bewertungen
- Saint Paul University Dumaguete Graduate School: Master of Science in NursingDokument5 SeitenSaint Paul University Dumaguete Graduate School: Master of Science in NursingJorie RocoNoch keine Bewertungen
- The Teacher and His Profession Written ReportDokument7 SeitenThe Teacher and His Profession Written ReportJorie RocoNoch keine Bewertungen
- Objectives For Hospital ExperienceDokument5 SeitenObjectives For Hospital ExperienceJorie RocoNoch keine Bewertungen
- Patient Details Ref No: Date & Time:: Dr. Nikita Mohana MbbsDokument1 SeitePatient Details Ref No: Date & Time:: Dr. Nikita Mohana MbbsVishwaja satish virbhaktNoch keine Bewertungen
- Article With BhajanDokument4 SeitenArticle With BhajanBibek SutradharNoch keine Bewertungen
- Bizarre Foreign Objects in The Genital Tract-Our Experience and Review of LiteratureDokument5 SeitenBizarre Foreign Objects in The Genital Tract-Our Experience and Review of LiteratureLidwina ApyakaNoch keine Bewertungen
- Discharge Planning Bleeding Peptic Ulcer DiseaseDokument5 SeitenDischarge Planning Bleeding Peptic Ulcer DiseaseAlexandrea MayNoch keine Bewertungen
- PBL PrintDokument4 SeitenPBL PrintShereen OngNoch keine Bewertungen
- Jurnal Nausea and VomitingDokument15 SeitenJurnal Nausea and VomitingRisa KarmeylithaNoch keine Bewertungen
- NycoCard Brochure 01Dokument2 SeitenNycoCard Brochure 01TimNoch keine Bewertungen
- Edwards' SyndromeDokument2 SeitenEdwards' Syndromeمحمود محمد0% (1)
- Catheter Care and MaintenanceDokument4 SeitenCatheter Care and MaintenanceSha BtstaNoch keine Bewertungen
- Gestational Diabetes MellitusDokument16 SeitenGestational Diabetes Mellitusarjunr19910% (1)
- Chronic Rhinosinusitis With Nasal Polyps: Clinical PracticeDokument9 SeitenChronic Rhinosinusitis With Nasal Polyps: Clinical PracticeAnabel SagasteguiNoch keine Bewertungen
- Tricuspid AtresiaDokument5 SeitenTricuspid AtresiaCassyDelaRosaNoch keine Bewertungen
- How To Stop SmokingDokument48 SeitenHow To Stop SmokingAditya KumarNoch keine Bewertungen
- Sirka Health OfficeDokument30 SeitenSirka Health OfficeWogen GenaNoch keine Bewertungen
- Hospt Treat Outcome Time Acutet Age GenderDokument3 SeitenHospt Treat Outcome Time Acutet Age Genderbats_robynNoch keine Bewertungen
- (Pharma-TRANS) 2.09 Geriatric Pharmacology: D. Protein BindingDokument2 Seiten(Pharma-TRANS) 2.09 Geriatric Pharmacology: D. Protein BindingStudy ReviewersNoch keine Bewertungen
- Gallbladder DiseasesDokument6 SeitenGallbladder DiseasesJoharaNoch keine Bewertungen
- Fluids, Electrolytes, Acid-Base Disorders, and Nutrition SupportDokument56 SeitenFluids, Electrolytes, Acid-Base Disorders, and Nutrition SupportFarryrazaNoch keine Bewertungen
- ETS & CapillaryDokument6 SeitenETS & CapillaryRoela Marie AlbaniaNoch keine Bewertungen
- Dip RCP FP 2000-2004Dokument6 SeitenDip RCP FP 2000-2004Akash Deep AggarwalNoch keine Bewertungen
- HPV and Related Diseases Report HPV Informacion CentreDokument303 SeitenHPV and Related Diseases Report HPV Informacion CentreRenée Elizade Martinez-PeñuelaNoch keine Bewertungen
- ANATOM 128 Brochure-ReDokument8 SeitenANATOM 128 Brochure-ReAli MirzaNoch keine Bewertungen
- Effectiveness of The Motor Relearning ApproachDokument5 SeitenEffectiveness of The Motor Relearning ApproachZahid MehmoodNoch keine Bewertungen
- Congenital CataractDokument20 SeitenCongenital CataractYouhengNoch keine Bewertungen
- Aceclofenac 100 MG Film-Coated Tablets - Summary of Product Characteristics (SMPC) - Print Friendly - (eMC) PDFDokument9 SeitenAceclofenac 100 MG Film-Coated Tablets - Summary of Product Characteristics (SMPC) - Print Friendly - (eMC) PDFHabibNoch keine Bewertungen
- TUMOR MARKERS (Hand-Out) EDITDokument36 SeitenTUMOR MARKERS (Hand-Out) EDITAliza Dewi FortuaNoch keine Bewertungen
- Guided Notes 7Dokument9 SeitenGuided Notes 7Desiree Denise Valle-DearNoch keine Bewertungen